Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.108454
Revised: May 3, 2025
Accepted: May 21, 2025
Published online: June 18, 2025
Processing time: 64 Days and 24 Hours
Meniscal cysts are a relatively uncommon form of meniscus pathology and often coexist with meniscus tears or degeneration. They are typically diagnosed as intra-meniscal cysts or para-meniscal cysts. The majority of para-meniscal cysts protrude towards the joint capsule side of the meniscus, and to date, no cases have been documented at the free edge of the meniscus. The present case of free-edge medial meniscal cysts will contribute to a deeper understanding of meniscal cysts.
A 30-year-old male presented with intermittent right knee pain six months ago. Diagnostic arthroscopic examination revealed a medial meniscus tear accom
This first case of meniscal free-edge cyst exemplifies the expansion of the spectrum of morphological types of meniscal cysts.
Core Tip: Meniscal cysts represent a relatively uncommon form of meniscal pathology and are typically classified as intra-meniscal or para-meniscal cysts. Para-meniscal cysts generally arise on the side of the meniscus adjacent to the joint capsule. However, this report presents a rare case of a medial meniscus free-edge cyst, which, to the best of current knowledge, has not been previously documented. This case contributes to a broader understanding of meniscal cysts.
- Citation: Ding M, Liao BH, Shangguan L, Wang YC, Xu H. Arthroscopic management of a rare free-edge medial meniscal cyst: A case report. World J Orthop 2025; 16(6): 108454
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/108454.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.108454
Meniscal cysts, a relatively uncommon form of meniscal pathology, exhibit incidence rates ranging from 1% to 8%, as reported in the literature[1]. These cysts frequently coexist with meniscal tears[1,2] or degenerative changes; however, their underlying pathogenesis remains incompletely understood. A unidirectional valve mechanism is believed to facilitate the accumulation of synovial fluid[3]. Medial meniscal cysts are more prevalent than lateral meniscal cysts, with a reported prevalence ratio ranging from 2:1 to 4:1[4]. The most common site for these cysts is the posterior horn of the medial meniscus[4]. Meniscal cysts are typically diagnosed using magnetic resonance imaging (MRI), with approximately 5% identified as intra-meniscal cysts and 95% as para-meniscal cysts[5]. Most para-meniscal cysts protrude toward the joint capsule side of the meniscus. However, to date, no cases of para-meniscal cysts occurring at the free edge of the meniscus have been reported. This report presents a cyst located at the free edge of the medial meniscus—a very rare presentation—which contributes to a deeper understanding of meniscal cysts.
A 30-year-old male with no significant medical history presented with intermittent right knee pain that began 6 months prior.
The patient initially experienced right knee pain following running and lower limb strength training. He denied any history of direct knee trauma associated with these activities. Since onset, the pain has recurred intermittently and has not fully resolved with rest. It remains localized to the right knee, with no involvement of other joints. The pain typically worsens following physical activity. The patient occasionally reports clicking sounds during knee movement without any sensation of joint locking or dislocation. No associated systemic symptoms—such as fever, night sweats, weight loss, or loss of appetite—have been noted.
No prior knee injuries.
The patient had no significant past medical, surgical, or family history.
Examination revealed tenderness along the medial joint line of the right knee. The joint was painful on palpation, but the range of motion was preserved, with extension measured at -5° and flexion up to 130°. McMurray's test was positive, suggesting a medial meniscus tear.
Laboratory investigations revealed no abnormalities.
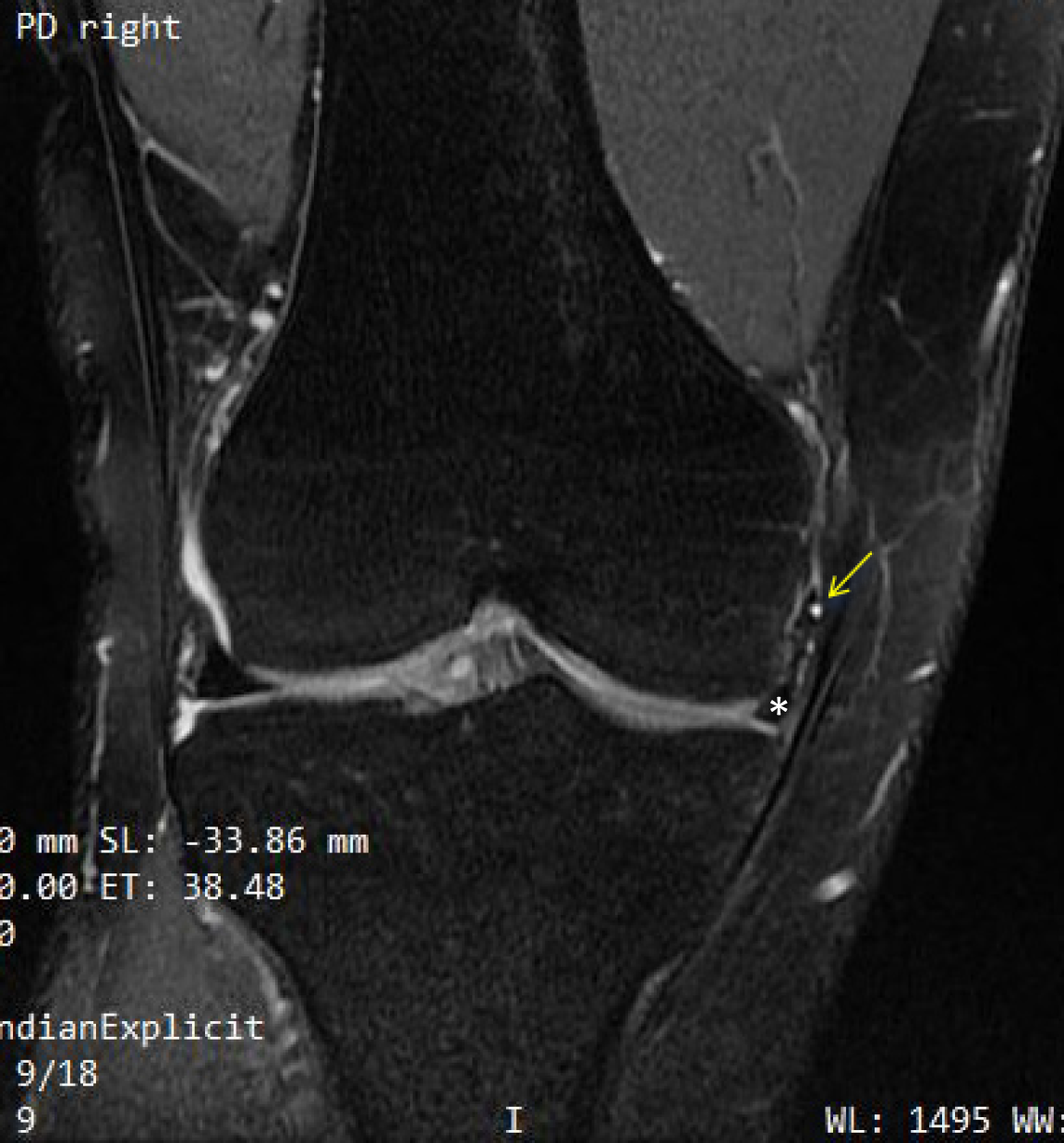
Plain radiographs of the right knee demonstrated normal bone density and joint spaces, with no evidence of fracture or dislocation (Figure 1). MRI revealed a tear of the medial meniscus with a small joint effusion. The medial meniscus was obliquely ruptured and displaced inward into the medial groove on the anteromedial aspect, located between the medial femoral condyle and the medial joint capsule. A cystic structure approximately 0.5 cm in diameter was observed at the edge of the torn meniscus. The anterior and posterior cruciate ligaments appeared continuous, with normal morphology and alignment. Both the medial and lateral collateral ligaments were intact. The articular surfaces were smooth, and no abnormalities were detected in the surrounding muscles or soft tissues (Figure 2).
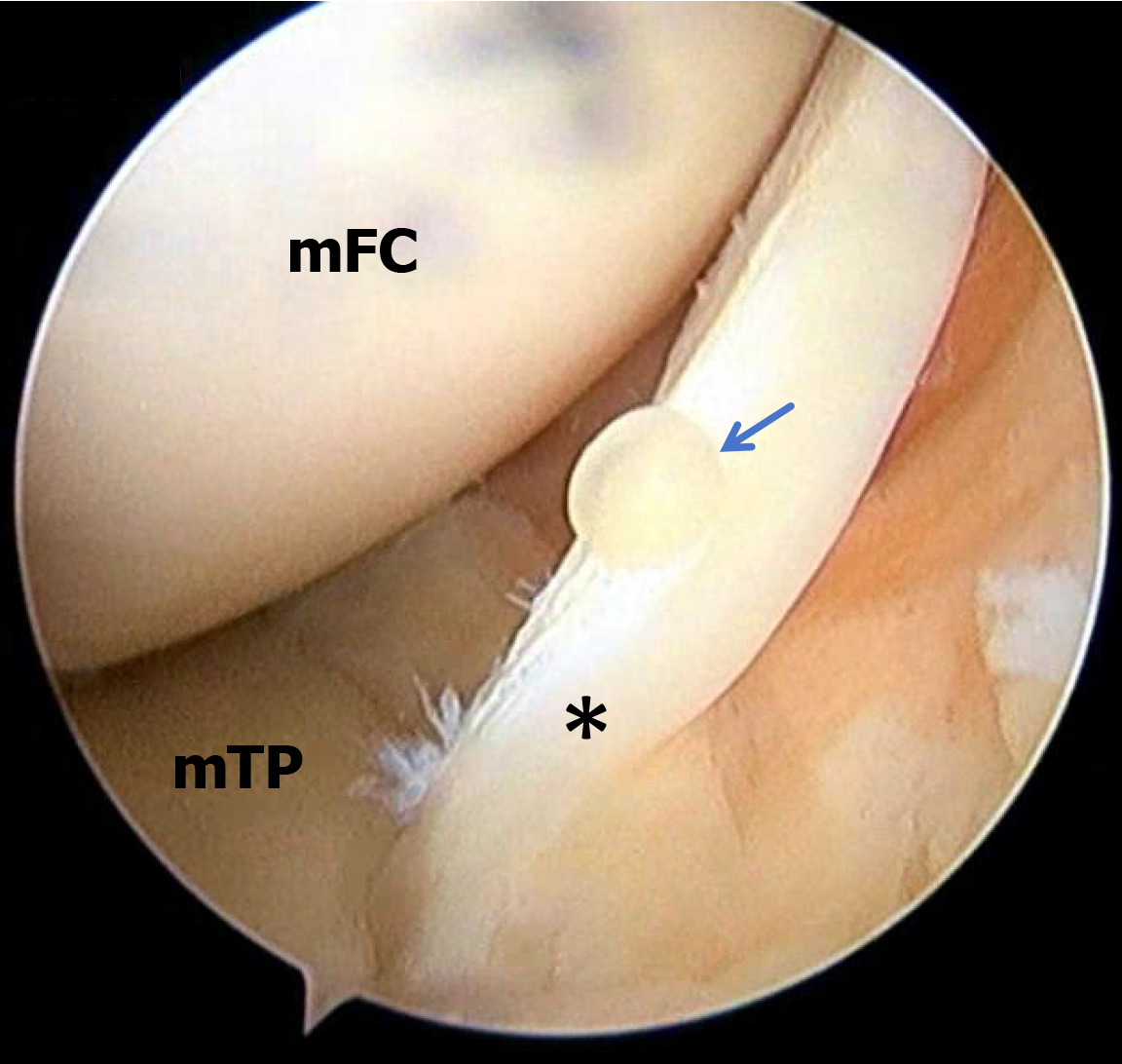
Based on the patient's history, physical examination, imaging studies, and findings from diagnostic arthroscopy, a diagnosis of a medial meniscus tear associated with a medial meniscus free-edge cyst was established (Figure 3).
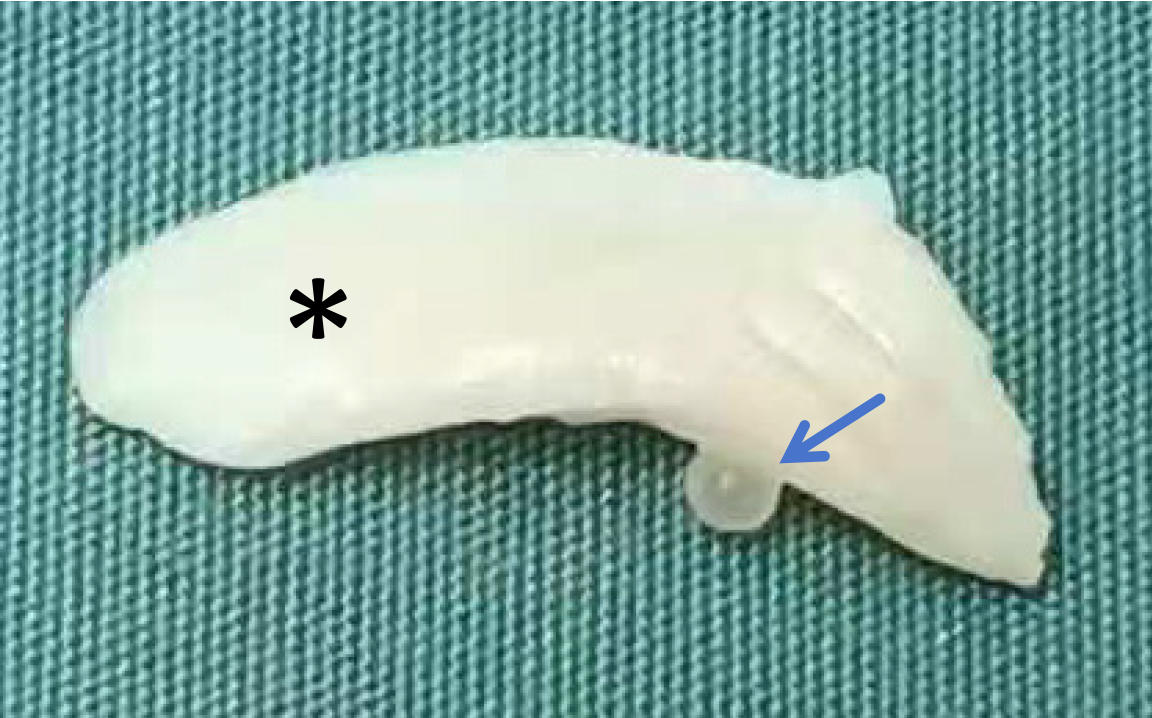
Diagnostic arthroscopy revealed an oblique tear in the body of the medial meniscus with anterior medial flipping. A cyst approximately 0.5 cm in diameter was identified at the free edge of the flipped meniscal flap. Partial resection of the oblique tear was subsequently performed (Figure 4), and the resected meniscal tissue, including the cyst, was submitted for pathological examination. The arthroscopic portals were closed using 2/0 prolene sutures following surgical excision.
On the first postoperative day, the patient commenced static quadriceps strengthening exercises and active range-of-motion training, which were continued for six weeks. Sutures from the arthroscopic portals were removed after two weeks.
Pathological examination confirmed the presence of a cyst at the free edge of the meniscus (Figure 5). At nearly two months postoperatively, the patient demonstrated marked improvement in knee function, with ongoing recovery anticipated. The clinical course remained favorable, with no recurrence of the meniscal cyst, pain, or limitations in joint mobility.
The notable finding in this case was the identification of a meniscal cyst located at the free edge of the meniscus—a phenomenon not previously documented in the literature. This observation aligns with recent studies on lateral meniscal cysts, which suggest that such cysts are commonly associated with meniscal injuries and are amenable to arthroscopic treatment. Existing literature indicates that meniscal cysts predominantly affect the lateral meniscus, with reported prevalence ratios ranging from 5:1 to 10:1 compared to the medial meniscus. These cysts are frequently linked to traumatic events. Passler et al[6] reported a 1.4% detection rate of meniscal cysts during knee arthroscopy, with a distribution of 87.5% in the lateral meniscus and 12.5% in the medial meniscus. Similarly, Seger and Woods[7] reported a lateral-to-medial meniscus cyst ratio of 10:1.
However, advances in MRI technology have led to evolving insights. In contrast to earlier findings based solely on arthroscopic or surgical data, recent imaging-based studies suggest that medial meniscal cysts are more common than previously believed[4,8]. Campbell et al[4] reported a revised ratio, indicating that medial meniscal cysts occur approximately twice as frequently as lateral cysts.
Meniscal cysts are generally categorized by their anatomical location as either para-meniscal or intra-meniscal. Para-meniscal cysts are typically located on the side of the meniscus adjacent to the joint capsule[9]. The cyst presented in this case was situated at the free edge of the meniscus, a location where para-meniscal cysts have not been previously described. This position might lead to it being mistaken for an intra-meniscal cyst while the cyst may appear intra-meniscal radiologically, however, its surgical behavior and histology support a para-meniscal classification, and the structural integrity of the surrounding meniscal tissue remained intact. To date, no cases involving a para-meniscal cyst at the free edge of the meniscus have been reported. This case broadens the spectrum of known morphological presentations of para-meniscal cysts and contributes to a more comprehensive understanding of this pathology.
Meniscal cysts are relatively rare entities encountered in meniscal surgery and are typically associated with underlying meniscal tears. The prevailing hypothesis regarding the pathogenesis of para-meniscal cysts suggests the extrusion of synovial fluid from adjacent meniscal tears[1,2,4,10]. A history of trauma is a known risk factor, with studies showing that 37.5% of patients diagnosed with meniscal cysts have a documented history of knee injury. Nevertheless, many cases may result from chronic degenerative processes, particularly among older individuals[11].
In the present case, although an oblique tear was observed in the medial meniscus, there was no apparent tear or degenerative change in the region surrounding the cyst. This raises the possibility that the cyst may have developed spontaneously. Alternatively, repetitive microtrauma or biomechanical alterations leading to mechanical irritation of the free edge may have contributed to its formation. However, as this is a single case report, further investigation is required to validate these hypotheses and confirm the authenticity of this presentation.
MRI remains the imaging modality with the highest diagnostic efficacy for meniscal cysts. Chen et al[12] reported that computed tomography can be useful in evaluating cyst size, location, internal content, and anatomical relationships with the meniscus and surrounding structures. Rutten et al[13] indicated that high-resolution ultrasonography may serve as a viable alternative to conventional MRI. Although these alternative imaging techniques can be utilized when MRI is unavailable, they are not commonly employed in routine clinical practice.
In the present case, although the meniscal cyst was visualized on MRI, its small size made detection challenging. This highlights the importance of a comprehensive MRI evaluation of the meniscus that includes both the capsular and free-edge regions to ensure accurate identification and assessment of meniscal cysts. For future cases involving free edge meniscal cysts, specific MRI protocols may enhance diagnostic sensitivity and specificity. These could include reduced slice thickness or the use of targeted signal enhancement techniques to improve visualization of small cystic structures—representing a promising direction for future research.
Regarding treatment, as most meniscal cysts are associated with underlying meniscal tears, the primary therapeutic approaches include arthroscopic meniscus repair combined with cyst excision or total meniscectomy. Cowden and Barber[14] recommend total meniscectomy for symptomatic meniscal tears accompanied by cysts. However, Kumar et al[15] reported that during midterm follow-up, patients undergoing total meniscectomy exhibited significant declines in Lysholm scores compared to preoperative levels, primarily due to postoperative joint degeneration. Pedowitz et al[16] advocated for partial meniscectomy, which targets the underlying pathology while preserving meniscal structure to prevent further degeneration.
With advancements in arthroscopic repair techniques and evolving surgical concepts, Thor et al[17] suggest that the most common horizontal meniscal tears—frequently associated with cyst formation—can now be effectively addressed through meniscal repair. Therefore, horizontal meniscal tears with concurrent cysts may be managed simultaneously using arthroscopic repair and cyst excision. However, it remains uncertain whether meniscus repair improves outcomes or reduces the recurrence rate of meniscal cysts[17]. While arthroscopy enables concurrent meniscus repair and cyst excision, the efficacy of repair alone in preventing cyst recurrence requires further investigation.
In the present case, an oblique tear of the medial meniscus had flipped into the anterior medial gutter, with a cyst located at the free edge of the torn segment. Arthroscopic partial meniscectomy was sufficient for definitive management. Notably, the flipped tear exposed the free-edge cyst, facilitating its identification and excision. In cases involving other types of meniscal tears, such cysts may remain obscured by the medial femoral condyle, potentially complicating preoperative assessment and intraoperative visualization. When MRI strongly suggests the presence of a medial meniscus free-edge cyst, modification of the standard arthroscopic approach may be warranted. Specifically, the anterolateral portal can be positioned more distally to optimize visualization of the medial meniscus. If necessary, a pie-crusting release of the medial collateral ligament may be performed to widen the medial joint space and improve access for both diagnostic and therapeutic procedures.
To the best of our knowledge, this is the first documented case report describing a rare variant of meniscal cyst located at the free edge of the meniscus. This finding expands the known morphological spectrum of meniscal cysts and highlights the importance of meticulous evaluation of the meniscal free edge on MRI to avoid overlooking this uncommon presentation. Surgeons should maintain a high index of suspicion for free-edge meniscal cysts in cases of anterior medial flipping and inconclusive imaging findings.
| 1. | Haratian A, Bolia IK, Hasan LK, Fathi A, Solaru S, Homere A, Petrigliano FA, Weber AE. Arthroscopic Management of Meniscal Cysts: A Systematic Review. Orthop Res Rev. 2021;13:123-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Ryu RK, Ting AJ. Arthroscopic treatment of meniscal cysts. Arthroscopy. 1993;9:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 47] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Howe TS, Koh JS. Arthroscopic internal marsupialization of meniscal cysts. Knee. 2007;14:408-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: incidence, location, and clinical significance. AJR Am J Roentgenol. 2001;177:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 88] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Laddha MS, Shingane D. Intrameniscal Cyst-Arthroscopic Open- and Closed-Door Repair Technique. Arthrosc Tech. 2023;12:e141-e145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Passler JM, Hofer HP, Peicha G, Wildburger R. Arthroscopic treatment of meniscal cysts. J Bone Joint Surg Br. 1993;75:303-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Seger BM, Woods GW. Arthroscopic management of lateral meniscal cysts. Am J Sports Med. 1986;14:105-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 35] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | De Smet AA, Graf BK, del Rio AM. Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. AJR Am J Roentgenol. 2011;196:W180-W186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Saraiva L, Saraiva AP, Coutinho M, Pereira da Silva JA. Parameniscal cyst: an important differential diagnosis in slow growing masses of the knee. ARP Rheumatol. 2023;2:83-84. [PubMed] |
| 10. | Choi EH, Huang J, Bryk D, Bryk E. Giant medial parameniscal cyst in an osteoarthritic knee. Orthopedics. 2009;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Rajput MI, Rafique M, Khan MW, Sahito B, Hussain N, Mohammad JG. Substantial medial para-meniscal cyst with a complex meniscal tear: A case report. Int J Surg Case Rep. 2024;125:110533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Chen WC, Wu JJ, Chang CY, Chen BF, Yang DJ. Computed tomography of a meniscal cyst. Orthopedics. 1987;10:1569-1572. [PubMed] |
| 13. | Rutten MJ, Collins JM, van Kampen A, Jager GJ. Meniscal cysts: detection with high-resolution sonography. AJR Am J Roentgenol. 1998;171:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Cowden CH 3rd, Barber FA. Meniscal cysts: treatment options and algorithm. J Knee Surg. 2014;27:105-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Kumar NS, Jakoi AM, Swanson CE, Tom JA. Is formal decompression necessary for parameniscal cysts associated with meniscal tears? Knee. 2014;21:501-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Pedowitz RA, Feagin JA, Rajagopalan S. A surgical algorithm for treatment of cystic degeneration of the Meniscus. Arthroscopy. 1996;12:209-12; discussion, 213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Thor JEH, Lim GYC, Hui JHP, Lee DYH. Do meniscal repairs with meniscus cyst do better than meniscectomy?-a systematic review of meniscal cyst treatment. Ann Jt. 2023;8:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |