CLINICAL MANIFESTATIONS OF ESSEX-LOPRESTI INJURY
The typical clinical manifestations of Essex-Lopresti injury include limited flexion and extension of the elbow joint, significant lateral swelling and tenderness, restricted forearm rotation, and tenderness at the distal radioulnar joint, which worsens with forearm rotation. In severe cases, the dorsal process of the ulna can cause dislocation of the distal radioulnar joint. X-ray imaging is essential for diagnosing fractures. However, children's ability to express symptoms is limited due to their underdeveloped cartilage structures and biomechanical properties, such as unclosed epiphyses and lower bone density. These factors make children more susceptible to fractures from longitudinal forces rather than complete ligament or joint capsule ruptures. The strength of children's bones, particularly in the growth plate area, is weaker compared to that of ligaments and joint capsules[5]. Landin[5] analyzed that fractures in children frequently involve the epiphyseal plate, while ligament injuries are rare, confirming that bones, especially the epiphyseal plate, are the weak link in pediatric trauma. Therefore, it is crucial to combine imaging studies to analyze the pattern of forearm injuries in children. The forearm ring comprises the radius, ulna, proximal radioulnar joint, and distal radioulnar joint, stabilized by the annular ligament, IOM, and TFCC.
The integrity of the IOM can be evaluated using the C-finger crush test. IOM injuries can be diagnosed through magnetic resonance imaging (MRI) or ultrasound imaging. On T2-weighted MRI images, a normal IOM appears as a clear and continuous black line. Disruption of this line with surrounding signal enhancement indicates IOM damage. Ultrasound examination reveals a continuous hyperechoic "white line" between the ulna and radius; interruption of this line suggests IOM injury[6]. Fester et al[7] found no statistically significant difference between MRI and ultrasound in diagnosing IOM injuries in cadaveric studies. Awan and Goitz[8] concluded that both MRI and ultrasound have similar diagnostic accuracy for IOM tears. Kachooei et al[9] validated the reliability of the intraoperative radial traction test for diagnosing IOM injuries through cadaveric studies. Lum et al[10] applied axial traction to the wrist in cadaveric models to assess the severity of longitudinal forearm instability by observing proximal radial displacement. The radial traction test is used intraoperatively to diagnose injuries to the distal radioulnar joint and the IOM[11]. If the radius cannot be reduced during intraoperative traction, it is essential to evaluate ulnar shortening from osteotomy to restore radial length, which may necessitate surgical intervention[12].
DIAGNOSIS AND TREATMENT OF ESSEX-LOPRESTI INJURY
Early diagnosis of Essex-Lopresti injury is crucial. For all forearm injuries, particularly those involving the radial head, a comprehensive physical examination should include adjacent joints, specifically the wrist, forearm, and elbow. Prompt recognition of Essex-Lopresti injury in acute settings is essential. Recent orthopaedic literature[13] highlights that acute Essex-Lopresti injuries have garnered significant attention. This suggests the existence of multiple injury patterns, emphasizing the need to evaluate IOM and ligament injuries in any forearm axial loading injury, as these may lead to longitudinal instability. The initial evaluation typically involves standard wrist and elbow radiographs to assess proximal radial displacement. While MRI and ultrasonography can be valuable in acute settings, their diagnostic findings and clinical significance remain unclear. Surgical management focuses on restoring radial length and ensuring distal radioulnar joint stability. Currently, the Edward and Jupiter classification system for Essex-Lopresti injuries is widely adopted: Type I involves radial head fractures with large displaced fragments, which can be managed with open reduction and internal fixation (ORIF); Type II includes comminuted fractures where resection of the radial head and replacement with a prosthesis may be necessary to prevent proximal radial displacement; Type III encompasses chronic cases characterized by irreducible proximal radial displacement. Clinical studies have defined forearm longitudinal instability, including IOM injury, or longitudinal radioulnar separation, with radioulnar joint injuries classified as acute (within 4 weeks) or chronic (beyond 4 weeks)[14]. However, there remains no universally accepted definition of Essex-Lopresti injury in the literature, likely due to its rarity in clinical practice.
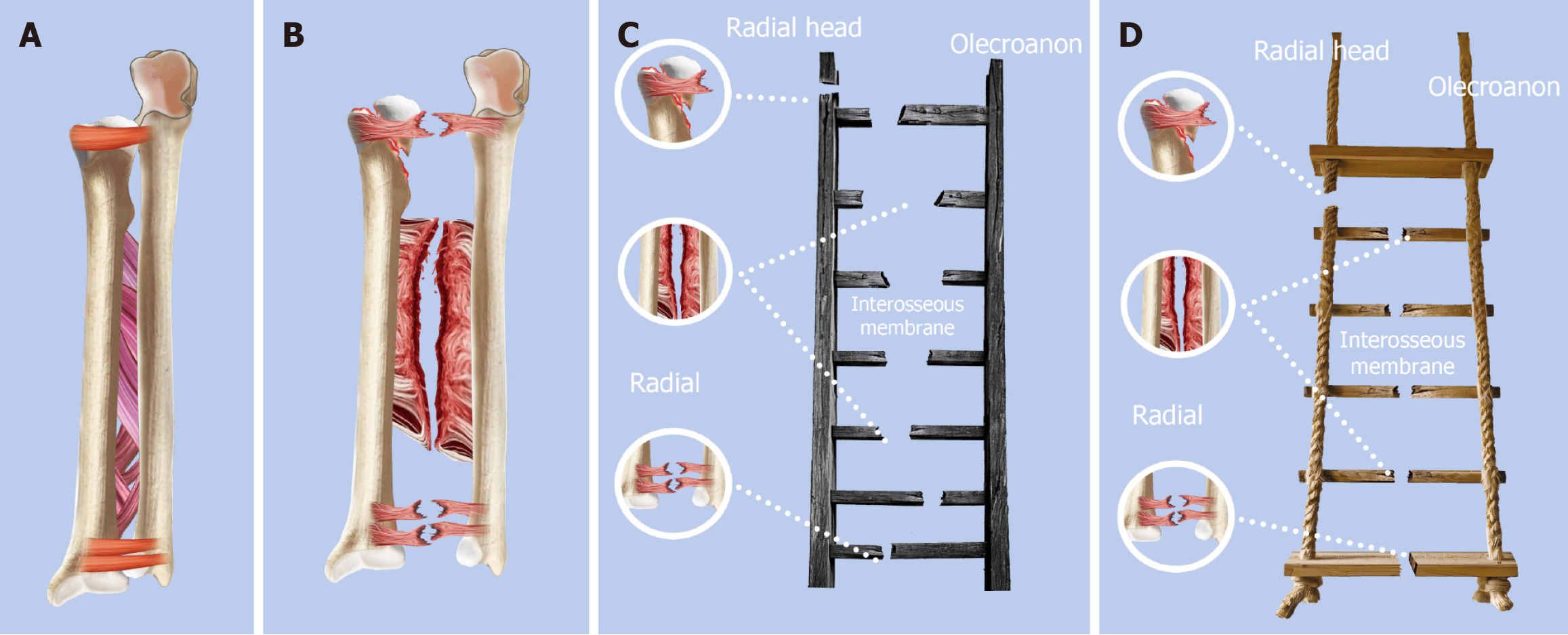
The injury to the IOM is typically caused by a high-energy longitudinal compression force, resulting in complex lesions that may originate from the transverse rupture of the central zone of the IOM[15]. Clinically, this manifests as longitudinal instability of the forearm, proximal displacement of the radius (radial shortening), secondary dislocation of both the distal and proximal radioulnar joints. If it remains undiagnosed and untreated in the early stage, it may result in chronic instability or shortening of the forearm in later stages, with clinical manifestations including limited rotational function of the forearm, and degeneration of the wrist and elbow joints due to abnormal stress, ultimately causing chronic pain. Autopsy studies of the forearm IOM have indicated that following radial head resection, the central zone of the IOM contributes 71% to longitudinal stability. Injury to this region may play a critical role in the development of proximal radius displacement after radial head resection[16] (Figure 1). In cases of longitudinal instability injuries in pediatric patients, the bone, particularly the proximal radius, is often the weak point, making fractures more common than ligament injuries. Peterson[17] highlighted that in children, longitudinal forces on the forearm are more likely to result in epiphyseal separation or metaphyseal fractures rather than ligament damage. Although the IOM comprises multiple ligaments, including the accessory fasciculus, distal oblique fasciculus, proximal oblique fasciculus, and dorsal oblique accessory fasciculus, the central fasciculus is considered the most resistant to both longitudinal and transverse radioulnar forces[11].
Figure 1 Mechanism of Essex-Lopresti injury and its difference between adults and children.
A: Normal ulna and radius structure; B: Essex-Lopresti injury structure; C: A ladder analogy illustrating an adult Essex-Lopresti injury; D: A rope ladder analogy is utilized to compare Essex-Lopresti injuries in children, as the strength of pediatric bones is generally lower than that of ligaments.
Intraoperative ultrasonography can aid in detecting IOM injuries, with the "muscle hernia sign" demonstrating a significant positive predictive value (sensitivity 88%) as reported by Loeffler et al[18]. Fontana et al[19] utilized the tilt test to diagnose distal radioulnar joint instability associated with IOM rupture. The diagnosis of IOM injury poses significant challenges. MRI and ultrasound have been demonstrated to be valuable tools for evaluating such injuries. However, the selection of the appropriate method should be individualized based on specific clinical contexts, as diagnostic errors or failures could potentially result in complications[20]. Repairing the central bundle restores longitudinal stability to the forearm and reestablishes the anatomical radioulnar relationship. However, the efficacy of one-stage repair for acute IOM injuries remains controversial, with insufficient evidence supporting its additional benefits[13]. While some researchers advocate for one-stage repair due to concerns about inadequate self-healing, others caution that surgical intervention may lead to forearm dysfunction or bone bridge formation[21]. Smith proposed based on cadaver studies that following radial head resection, a proximal displacement of 3 mm under longitudinal traction suggests interosseous membrane disruption, while a proximal displacement of 6 mm or more indicates longitudinal instability and complete disruption of all ligamentous structures in the forearm[22]. Not all MRI-diagnosed IOM injuries necessitate surgical intervention. For instance, Hausman et al[23] observed good outcomes following early mobilization in 9 out of 14 patients with partial IOM lesions and Mason type 1 radial head fractures. Conversely, Grassman et al[6] recommended treating IOM ruptures alongside radial head fractures, even in the absence of radiographic shortening, in addition to Kirschner wire stabilization of the distal radioulnar joint. In conclusion, considering the specific characteristics of Essex-Lopresti injuries and the physiological features of the IOM in children, it is advisable to avoid a single-stage repair of the IOM injury. Instead, the focus should be on restoring normal anatomical structures and ensuring a stable radioulnar relationship.
Two out of the three constraints of the forearm (proximal radioulnar joint, IOM, and distal radioulnar joint) can result in transverse radioulnar instability. If these two lesions are not adequately addressed, they can lead to a loss of forearm rotation[24]. Examples of such injuries include Galeazzi fractures, Monteggia fractures, and combined proximal and distal radioulnar joint dislocations with intact radioulnar and IOMs[25]. Post-surgical fixation of the radius in Galeazzi fractures often overlooks the instability of the distal radioulnar joint, leading to persistent pain and limited wrist movement, particularly in pediatric cases involving radial shaft fractures with distal ulna epiphysis separation[26,27]. The stability of the distal radioulnar joint is maintained by the TFCC, joint capsule, and ligaments (volar and dorsal radioulnar ligaments). The inherent instability of the distal radioulnar joint, which results in weakened forearm pronation and supination, is frequently observed in injuries to the TFCC[28]. Distal radioulnar joint instability may also present as dislocation or subluxation, weakened grip strength, and chronic wrist pain (often associated with degenerative arthritis). In the absence of instability or displaced fractures, TFCC injuries are typically managed conservatively for 3-6 months. If conservative treatment fails, arthroscopy-assisted diagnosis and repair of the TFCC injury is recommended[29].
The treatment of forearm injuries primarily aims to restore the anatomical structure and stability of the forearm ring. To prevent missed diagnoses of acute Essex-Lopresti injuries, clinicians should be vigilant for this condition in patients presenting with radial head and neck fractures accompanied by wrist and/or forearm pain. Given the rarity of Essex-Lopresti injuries in children and the challenges posed by open epiphyses and X-ray diagnosis, these cases are often misdiagnosed as simple radius fractures[30]. To reduce the risk of missed or incorrect diagnoses, comparative radiological studies and dynamic evaluations of longitudinal radioulnar stability should be conducted. Kooistra et al[31] investigated the diagnostic value of MRI and dynamic evaluation, as well as the application of axial stress tests in patients with radial head fractures and wrist pain. They also retrospectively analyzed that over half of the studies lacked a precise definition of Essex-Lopresti injury, and the majority of articles failed to address injuries to the IOM. Consequently, he concluded that to prevent missed diagnoses of acute Essex-Lopresti injury, clinicians should be vigilant about the possibility of this injury in patients with radial head fractures accompanied by wrist and/or forearm pain. Treatment of acute cases typically involves proximal radial stabilization, while indications for radial head resection have become more limited due to a better understanding of the radial head's functional importance. Specifically, rupture of the annular ligament can lead to radial head subluxation, and the radial head plays a crucial role in providing valgus, transverse, and rotational stability. Consequently, loss of the radial head can result in chronic dysfunction and instability[32,33].
In childhood, the radial head exhibits a cartilaginous structure and is safeguarded by the annular ligament. Clinically, radial neck fractures are prevalent, yet they constitute only 1% of all pediatric fractures, radial neck fractures are common and can result in displacement of the radial head. Radial neck fractures in children are uncommon, and their association with Essex-Lopresti injuries is exceedingly rare. Clinicians should remain vigilant in diagnosing such cases. Postoperative complications, including malunion, forearm rotational instability, and radioulnar fusion, must be carefully avoided in pediatric patients with radial neck fractures[34]. Restoration of normal elbow function and the brachioradial joint can be achieved through appropriate management. Changes in the proximal radioulnar joint are frequently associated with Monteggia fractures, characterized by pain, stiffness during elbow flexion-extension or rotation, and reduced pronation/supination range. Maintaining the normal anatomical position of the radial neck and head is crucial for restoring forearm rotational function. Radial head resection can compromise function and stability, particularly impacting young patients and children, potentially leading to wrist pain, relative shortening of the radius, and ulnar deformity post-resection. For severe radial head or neck deformities, resection may be necessary, and ischemic necrosis of the radial head is an indication for joint replacement. ORIF remains the treatment of choice for comminuted radial head fractures due to its ability to restore anatomical alignment and stabilize the fracture site effectively, which brings a decreasing trend in surgical resection of the radial head, with a significant increase in joint replacements[35]. In cases of IOM injury, radial head resection may be contraindicated[36]. However, Lanting et al[37] reported that, based on cadaveric studies, the tension of the interosseous membrane significantly increased during simulated forearm rotation following radial head resection. However, no significant difference in interosseous membrane tension was observed after radial head replacement. Recent attention has focused on early postoperative rehabilitation to address ulnar incarceration and longitudinal wrist instability, as prolonged immobility can lead to poor function and morbidity[38]. Zhang et al[39] argues that the radial head should not be resected in acute radial head fractures, even when the elbow joint is unstable and/or wrist pain is present. This is particularly important when the longitudinal stability of the forearm is assessed using the radial traction stress test during surgery, as it is crucial to avoid Essex-Lopresti injuries in cases of acute trauma.
Understanding the anatomy and biomechanics of the forearm joint is essential for the effective treatment of chronic Essex-Lopresti injuries. The forearm, functioning as a joint with uniaxial rotation and three locking mechanisms, ensures both mobility and stability to facilitate load transfer and full range of motion. Instability can occur longitudinally due to the loss of the relationship between the radius and ulna, and translaterally due to dislocation of the proximal and/or distal radioulnar joints; the primary surgical objective is to reestablish the proper longitudinal alignment between the radius and ulna[40]. In cases of delayed treatment, anatomical recovery of the forearm ring is typically not feasible. If the Essex-Lopresti injury is classified as type III according to the Edward and Jupiter classification, the role of the radial head in elbow joint function should be thoroughly assessed. Given that such injuries typically result in limitations of elbow joint function, radial head replacement may be necessary to restore the normal anatomical and biomechanical function of the radial head within the elbow joint. Edwards and Jupiter[41] reported two cases of chronic Essex-Lopresti lesions treated with radial head replacement and ulnar shortening osteotomy, resulting in improved grip strength and supination postoperatively compared to preoperative conditions, with no complications noted. Schnetzke et al[42] utilized prosthetic radial head replacement to address the sequelae of complex radial head fractures in the chronic stage of Essex-Lopresti injury. Jungbluth et al[43] described a case report where the Sauve-Kapandji procedure was performed alone or in combination with radial head resection and radial head prosthesis implantation after restoring the correct radioulnar relationship in patients with weak grip due to instability of the distal radioulnar joint. All patients achieved good grip strength and stable fusion of the distal radioulnar joint. Other treatments for chronic Essex-Lopresti injury include radial head resection alone or combined with ulnar shortening osteotomy, IOM reconstruction, among others.
For both acute and chronic Essex-Lopresti injuries, the primary goal is to reconstruct the anatomical position of the radial head fracture. This involves not only the functional reconstruction of the radial head but also the restoration of forearm rotation. Radial head replacement is advisable when forearm rotation and elbow flexion-extension functions are limited due to malunion of the radial head. However, radial head resection is not recommended as it may compromise overall function.