Published online Jun 18, 2025. doi: 10.5312/wjo.v16.i6.105068
Revised: April 21, 2025
Accepted: May 21, 2025
Published online: June 18, 2025
Processing time: 142 Days and 15.2 Hours
The Victorian institute of sports assessment for patellar tendons questionnaire (VISA-P), a valid tool for patellar tendinopathy, has been used for patellofemoral pain (PFP).
To validate VISA-P in PFP.
Study of validity, responsiveness and feasibility following COSMIN. Inclusion criteria: Subjects with PFP, aged 18 to 55. Agreement among 10 experts on the relevance and clarity of each item using Aiken's V coefficient determined content validity. An exploratory factorial analysis established structural validity. The correlation of VISA-P with knee injury and osteoarthritis outcome score for PFP and Osteoarthritis (KOOS-PF) and Kujala patellofemoral score (KPS; specific for PFP) analyzed the construct validity. Internal consistency was calculated with Cronbach's α and test-retest reliability with the intraclass correlation coefficient (ICC). Feasibility considered the subjects' self-completion time.
The sample consisted of 103 knees from 73 subjects (47 female/26 male; aged 34.9 ± 13 SD). The items were relevant and clear, with the exception of item-8, which didn't reach an acceptable level of agreement on clarity. Exploratory factorial analysis found a 2-factor solution, which explained 63.48% of the variance. VISA-P achieved a strong and significant correlation with KOOS-PF (Spearman rho = 0.826; P < 0.001) and KPS (Spearman rho = 0.771; P < 0.001). The questionnaire showed adequate reliability (Cronbach's α: 0.752; ICC: 0.934; P < 0.0001; 95%CI: 0.902-0.955). The mean self-completion time was 232 ± 0.52 SD seconds.
VISA-P proved to be valid and reliable to functionally assess PFP and/or chondromalacia patella. VISA-P is a feasible tool in the clinical and research environment, quick and easy to complete.
Core Tip: Victorian institute of sports assessment for patellar tendons questionnaire (VISA-P) is an appropriate tool for the evaluation of patellofemoral pain and/or chondromalacia patella. This scale is useful for users who are physically active or involved in sports. VISA-P, recommended for assessing the progression of pathology in a subject, has been translated, cross-culturally adapted and validated in Spanish.
- Citation: Chamorro-Moriana G, Espuny-Ruiz F, Ridao-Fernandez C, Magni E. Validation of “Victorian institute of sports assessment for patellar tendons” in patellofemoral pain: Reliability, interpretability and feasibility study. World J Orthop 2025; 16(6): 105068
- URL: https://www.wjgnet.com/2218-5836/full/v16/i6/105068.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i6.105068
The Victorian institute of sports assessment for patellar tendons questionnaire (VISA-P) was designed and validated in 1998[1]. Although this is a functional assessment questionnaire reliable for patellar tendinopathy (PT)[2] and there are other specific ones such as Knee Injury and Osteoarthritis Outcome Score for Patellofemoral Pain (PFP) and Osteoarthritis (KOOS-PF)[3] and Kujala patellofemoral score (KPS)[4]; VISA-P has been applied with good clinical criteria in PFP[4] because of the similarity between their symptoms and their anatomical-functional relationship[5]. PT are considered overuse injuries[6], as are PFP[7]. PT begins with insidious and progressive pain[6,8], as does PFP[9], in the anterior area of the knee, identified by reference[10] in PT and by reference[11] in PFP. Load and repetitive activities that overload the knee, such as running, jumping or tasks that involve knee flexion, are influential factors in PT[6,12,13] and PFP[14,15]. In severe cases, pain and limitation in activities of daily life is associated with PT[6] and with PFP[16,17].
PFP affects one in five people[7] and the prognosis is poor. Symptoms continue 1-2 years after treatment in 50% of subjects, even up to 20 years[18]. It is associated with a progressive decline in quality of life, which may limit or prevent pain-free work and sporting life[19]; and psychological disorders such as depression, anxiety, catastrophism and fear of movement[20]. Thus, prevention and thus early assessment are essential.
Assessments by therapists or imaging tests are sometimes not enough due to the complex understanding of pain and the limitations it can entail[21]. In this sense, patient-reported outcome measures (PROMs), i.e., questionnaires are useful in initial evaluations in a quick, simple and efficient way; or to discover the effectiveness of a treatment[2,22]. They quantify patients' perception of their disease, symptoms, quality of life and functionality[23]. The high prevalence of PFP and the social impact it has, which individually affects quality of life[19] and mental health[20] suggest the need to further expand the use of useful assessment tools[24]. As the VISA-P is efficient[4] and applicable[2] in PFP, but has not yet been validated in this disorder, it would be advisable to support it scientifically for clinical and research use. Therefore, we aimed to validate VISA-P in PFP.
Validation study of VISA-P (Spanish version) in PFP using clinical measurement, undertaken at the University of Seville (Spain) with the approval of the Ethical Committee (No. C. I.0162-N-21). All participants gave informed consent. The lead author of the original questionnaire[1] approved the validation of the questionnaire in PFP.
They were recruited through convenience sampling. Inclusion criteria: (1) Symptomatic PFP; and (2) Aged 18-55 years. Exclusion criteria: (1) Severe cognitive impairment or impaired coordination; (2) Severe cardiovascular or respiratory conditions; and (3) Knee symptomatology or functional impairment due to other pathology.
Three Spanish validated questionnaires were used: VISA-P[1,25], and the specific questionnaires KOOS-PF[3,26] and KPS[4,27].
VISA-P, consisting of 8 items (item-8 is divided into 3), explores: Frequent knee flexion-extension pain in daily life (items-1-6); and its possible association with the subject's sporting activity (items-7-8). Item ranges: 0-10 (items-1-7 and 8C), 6-30 (8A) and 0-20 (8B).
KOOS-PF consists of 11 items examining: Stiffness (1 item), pain (9 items) and quality of life (1 item) related to the clinical symptoms. Item range: 0 (none/never) - 4 (extreme/always).
KPS consists of 13 items on: Pain and physical impairment (3 items), functional limitation (8 items) and difficulty in sports activities (2 items). Item ranges: 0-10 or 0-5.
All three questionnaires have a minimum score of 0 and a maximum score of 100, indicating the absence of symptomatology.
Descriptive data were collected: affiliation, sex, date of birth, weight, height, affected knee, months since onset of symptoms and Q-angle of the affected knee(s).
Subjects completed VISA-P, KOOS-PF and KPS in that order, twice, with a 7-day washout period, which would not result in substantial changes in pathology[3,4]. A researcher was present to ensure the process. Subjects with bilateral PFP completed one questionnaire per knee.
The psychometric properties of validity (content, structural, construct), reliability (test-retest reliability, internal consistency and measurement error) and interpretability were analyzed, following COSMIN[28] and the definitions of Mokkink et al[29]. Feasibility was studied[25]. It is important to highlight that this paper does not address criterion validity, as it adheres to COSMIN's recommendations for PROMs studies[30]. COSMIN addresses criterion validity in PROMs with the necessary use of gold standards. However, even in its latest 2024 version[31], it emphasizes that PROMs lack gold standards due to their subjective nature and, therefore, does not recommend studying this type of validity.
Content validity was carried out with a committee of 10 clinical experts[32] with experience in PFP. Each expert rated using Likert scales: The relevance of each item (1 = not relevant; 2 = not very relevant; 3 = relevant; 4 = very relevant); and the clarity (1 = disagree; 2 = slightly agree; 3 = agree; 4 = strongly agree). Experts were able to express their views and suggest improvements.
Structural validity entailed an exploratory factorial analysis[33] to group the items into dimensions identifying the main aspects of the pathology. Based on previous evidence from the validation of VISA-P in PT[25,34,35] researchers tested whether the pain and sport activity components were also adjusted to PFP.
In the construct validity, the results obtained in VISA-P were correlated with those of KOOS-PF and KPS.
Reliability was studied with internal consistency and test-retest reliability. The measurement error was also de
Interpretability studied ceiling or floor effects with respect to the final score and in relation to each item. These were considered if more than 15% of the subjects had the maximum or minimum final score, or if more than 75% achieved the maximum or minimum score for each item[36].
Feasibility considered the time taken by subjects to complete VISA-P and was compared with that of the other two questionnaires. The researchers noted queries, difficulties in understanding each item, ease of completion and the number of questionnaires that remained incomplete.
The sample size was calculated with G*Power 3.1.9.2. The study was based on the Spanish validation of VISA-P in PT[4]. The intraclass correlation coefficient (ICC) was used. An α error of 0.05 and a statistical power of 0.80 were established.
The sample size obtained was 103 subjects, exceeding the number recommended by COSMIN[28,37,38] (optimum ≥ 100). Our sample size included a few more subjects in case there were dropouts.
The characteristics of the participants and their VISA-P scores were described (m ± SD; Med and IQR) after testing for normality (Kolmogorov-Smirnov test).
The concordance of the experts' assessments was determined with Aiken's V coefficient (V)[39], with V ≥ 0.70 being acceptable[40].
The exploratory factorial analysis extracted the main components by applying Varimax rotation with Kaiser normalization. Prior to this, sampling adequacy was established with the Kaiser-Meyer-Olkin test (KMO) and Bartlett's test of sphericity. Values close to 1 in KMO and a significance < 0.05 in Bartlett were considered adequate. Communalities were calculated by extracting item by item, with values > 0.4 being acceptable. The factorial rotation matrix was calculated, estimating acceptable values to be > 0.5. When an item achieved factor loadings on both factors, it was assigned to the one with the highest correlation as long as the difference between the two loadings was > 0.2[41].
After checking for linearity (scatter plot) and normality (Kolmogorov-Smirnov test), the Pearson correlation coefficient or Spearman rho determined the correlation between VISA-P with KOOS-PF and KPS: Very weak, r < 0.25; weak, 0.25 < r < 0.5; moderate, 0.5 < r < 0.7; and strong, r > 0.70[42].
The internal consistency was calculated with Cronbach's α, with values between 0.70 and 0.95 being adequate[43]. The test-retest reliability was determined with ICC[44], with values > 0.70 being adequate[32,43]. Both tests assumed a 95%CI.
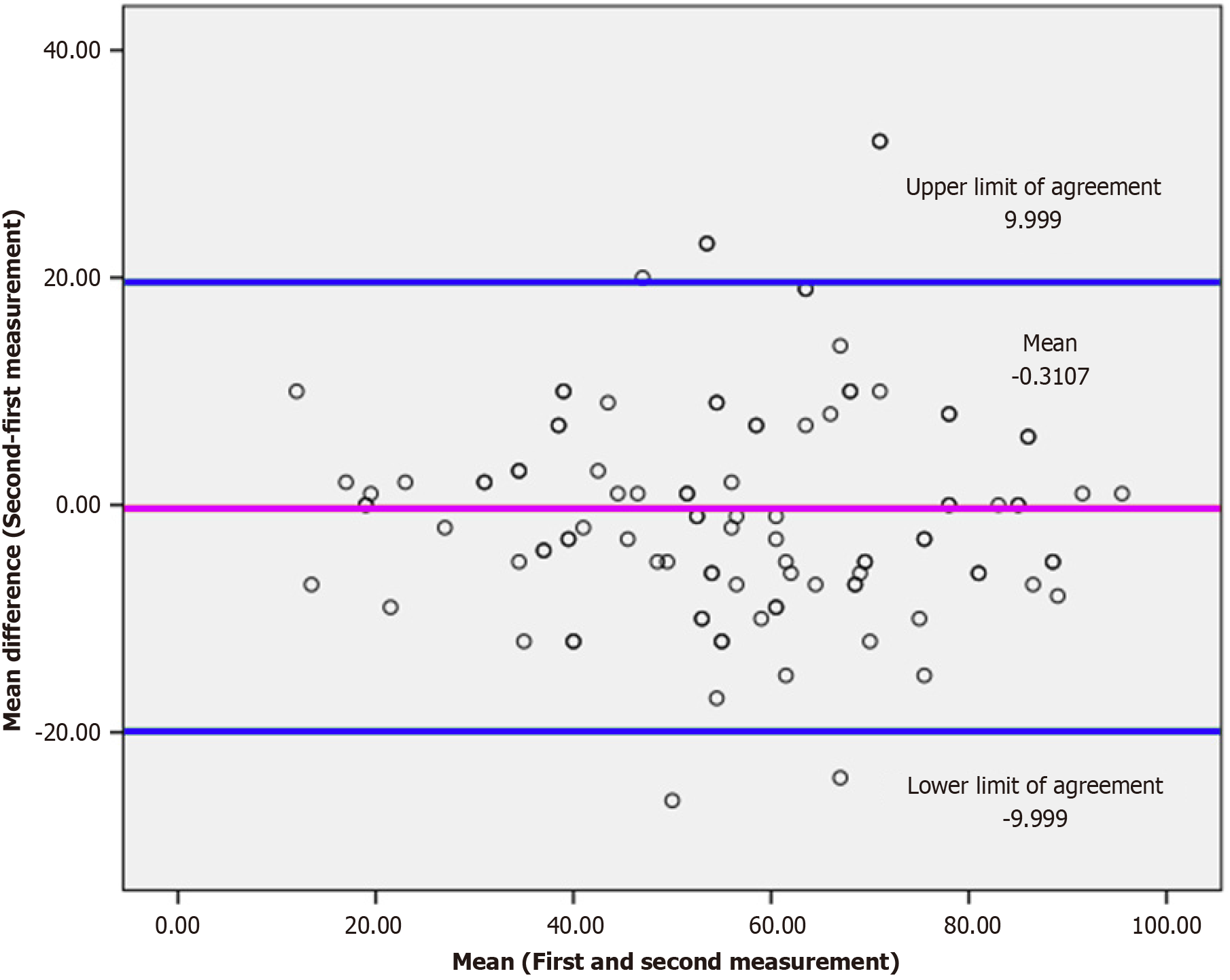
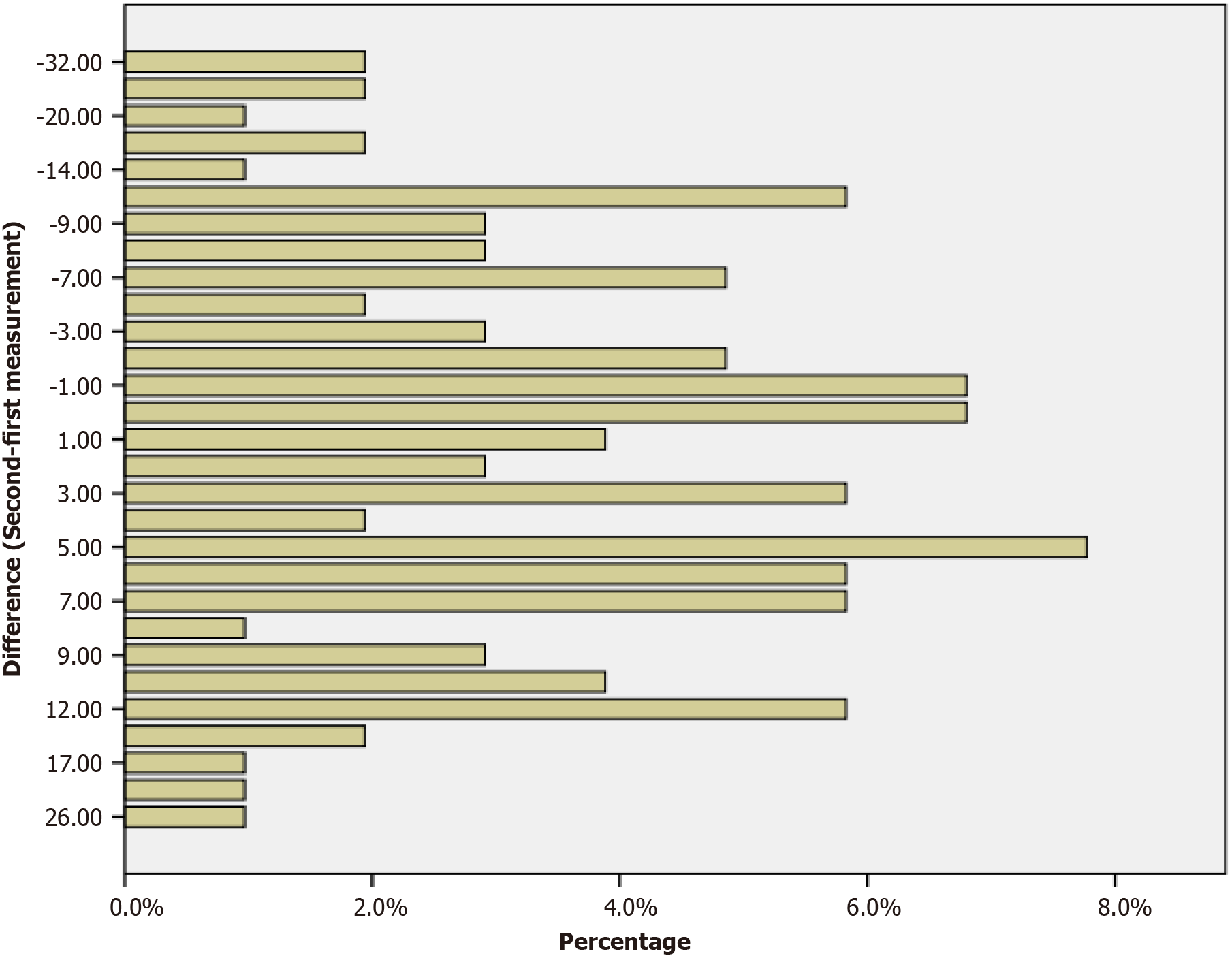
A Bland-Atman plot[43,45] showed the mean of the differences in the VISA-P scores of each subject in the two measurements. A bar chart showed the magnitude and distribution (percentages) of the differences between the two scores for each subject.
ICC was used to calculate SEM by applying the following formula[45,46]: SEM = SD × 1-test-retest reliability coefficient.
All statistical analysis were performed using SPSS Version 26 (SPSS Inc, Chicago, IL). The statistical review of the study was performed by a biomedical statistician.
The sample consisted of 103 affected knees from 73 subjects (47 female/26 male; aged 34.9 ± 13 SD; 30 bilateral/43 unilateral). The descriptions of the sample and participants are shown in Table 1.
| Women (n = 47) | Men (n = 26) | Total (n = 73) | |||
| Weight (kg) | μ | 66 | 87.59 | 73.89 | |
| SD | 11.7 | 11.20 | 15.3 | ||
| Height (cm) | μ | 165 | 181 | 171 | |
| SD | 6 | 5 | 9 | ||
| Time with pain (months) | Med | 48 | 66 | 54 | |
| IQR | 21-84 | 27-129 | 24-96 | ||
| Affected knees Q-angle (degree) | Med | 19 | 17 | 18 | |
| IQR | 18-24 | 16-18 | 16-22 | ||
| Impairment | Bilateral | n | 20 | 10 | 30 |
| % | 27.4 | 13.6 | 41.1 | ||
| Unilateral | n | 27 | 16 | 43 | |
| % | 37 | 21.9 | 58.9 |
Table 2 shows the V for inter-judge agreement on the relevance and clarity of the items.
| Item | Relevance | Clarity |
| 1 | 0.80 | 1 |
| 2 | 0.93 | 1 |
| 3 | 0.80 | 0.70 |
| 4 | 0.80 | 0.80 |
| 5 | 0.93 | 0.93 |
| 6 | 0.70 | 0.83 |
| 7 | 0.90 | 0.83 |
| 8 | 0.90 | 0.63a |
KMO obtained 0.827 and Bartlett's test of sphericity reached C2= 319.914, P < 0.0001; demonstrating the adequacy of the sample for the exploratory factorial analysis.
The analysis yielded a two-factor matrix, which explained 63.48% of the total variance (Table 3): Component 1 (items-2-3-4-5-6) and component 2 (items-1-7-8). Item-6 could have been included in both, but was included in the first because it had a higher factor loading (0.802) with a difference > 0.2 with the other loading (0.363).
| Item | Loading | |
| Component 1 | Component 2 | |
| 2 | 0.763 | |
| 3 | 0.732 | |
| 4 | 0.773 | |
| 5 | 0.848 | |
| 6 | 0.802 | 0.363 |
| 1 | 0.656 | |
| 7 | 0.736 | |
| 8 | 0.816 | |
Spearman rho between VISA-P and KOOF-PF was 0.826 for the first measurement and 0.821 for the second. Spearman rho between VISA-P and KPS was 0.752 for the first measurement and 0.771 for the second. All correlations were strong, with statistically significant differences (P < 0.001).
Cronbach α was 0.752 for the whole questionnaire, 0.865 for the component 1 and 0.559 for the component 2. ICC was 0.934 (P < 0.0001; 95%CI: 0.902-0.955).
Mean VISA-P scores were 56.23 ± 20.03 SD at the first measurement and 56.54 ± 20.01 SD at the second measurement.
The mean of the differences in the scores at the two measurement points was -0.310 ± 11.06 SD, with upper and lower agreement limits of 9.997 and -9.999, respectively. The Blad-Altman plot (Figure 1) shows that the differences between the two measurements are distributed around the 0 Line, being within the limits of agreement except for some outliers. No systematic bias was detected, i.e. the zero line was within the 95%CI.
The difference between the scores achieved at the two points in time was between 5 and -5 points in 43.7% of the cases, while in 51,4% of them it was between 6 and -6 (Figure 2). The SEM was 5.147.
No ceiling or floor effects were detected, no subject reached the maximum or minimum scores. In relation to each item, the percentage of subjects achieving the highest or lowest possible scores were: Item-1, 42.71%; item-2, 21.35%; item-3, 26.21%; item-4, 12.6%; item-5, 13.59%; item-6, 14.56%; item-7, 45.63%; item-8, 14.56%.
The mean time (seconds) to complete VISA-P was 232 ± 52 SD, KOOS, 264 ± 42 SD; and KPS, 293 ± 23 SD.
In VISA-P, no participant found it difficult to understand the content of the items, although 29 participants asked for clarification on how to answer item-8. All questionnaires were completed in full.
This study validated VISA-P in the Spanish population with PFP, being originally designed for PT in English[1] and subsequently translated, cross-culturally adapted and validated in Spanish[25]. Analysis of the psychometric properties revealed good reliability, content and construct validity.
It proved to be a feasible and user-friendly questionnaire, with high correlations with specific PFP questionnaires, i.e., construct validity, enabling its use in this pathology.
Before discussing the results, it is important to further explore the relationship between PT and PFP. The background highlighted several shared features regarding their anatomical-functional relationships, symptoms such as the characteristics of pain[7,9], and associated activities involving knee flexion—particularly when combined with load and repetition[6,12–15]. However, notable differences in their pathomechanics must also be taken into account.
PT is primarily a tendon-centric condition that can be acute/subacute and even progress to a chronic state, leading to reactive or degenerative changes in the tendon structure[6]. In contrast, PFP is generally considered a chronic condition[15] closely associated with altered joint biomechanics, such as patellar maltracking[47]. This dysfunction may result from muscular imbalances or poor motor control, which increase friction and stress on the patellofemoral joint[48,49] (pro
In line with the above, the authors of this study consider the possibility of shared joint origins for both disorders, either independently or simultaneously. Lateral or axial displacement of the patella, as well as patellar rotation or tilt—regardless of other contributing factors mentioned—can result in patellar maltracking. Similarly, a displaced patella can disrupt the alignment and tension of the patellar tendon, leading to altered biomechanics and, over time, to inflammatory and degenerative changes due to chronic stress. The laterally displaced patella may stem from muscular imbalances between the vasti muscles of the quadriceps, from lower limb misalignments, i.e., valgus knees, where the Q-angle is altered, etc. as well as the axially displaced patella could be due to weakness or retraction of the quadriceps. Likewise, anteroposterior femorotibial misalignment—such as that caused by chronic hamstring tightness—may tilt the patella forward while simultaneously redirecting the patellar tendon posteriorly at its distal insertion. Femoral-tibial rotation can also displace the patellar tendon laterally, thereby misaligning the patella. The latter example is commonly observed not only due to anatomical or acquired muscular imbalances, but also following surgical interventions[51]—for example, anterior cruciate ligament reconstructions, where the placement of the graft is not optimal.
These shared origins and the frequent co-occurrence of PT and PFP further support the relevance of the VISA-P content, as well as the objectives and findings of this study.
In relation to content validity and content relevance based on Aiken's V coefficient, all items reached “acceptable” (items-2-5-7-8) or “excellent” (items-1-3-4-6) levels of agreement among experts. The highest rated items were item-2 (pain when walking down stairs), and item-5 (pain when squatting), both being eccentric activities under load, and thus over-stressing the patellar tendon. In contrast, item-6 (pain in repeated monopodal jumps), was the least rated. This involves plyometry affecting the patellar tendon, but was possibly considered less aggressive than the others as it was assumed that the jumps were light/gentle, as observed during data collection. We understand that gentle hopping would be symptomatic only in acute or severe cases.
In terms of clarity, “acceptable” (items-3-4) and “excellent” (items-1-2-5-6-7) agreements were obtained among experts, and they were considered sufficiently understandable for users. Item-8 (duration of sporting activity due to pain), did not reach an “acceptable” level. In fact, 2 of the experts strongly indicated that it was not clear, in line with the statements of the participants. In addition, item-8 is divided into 3 sections according to levels of symptomatology, only one of which is to be answered. Since the symptomatology of PFP is variable depending on the load on the knee[14], subjects may misidentify themselves and/or answer several items incorrectly. Therefore, an improvement would be strongly recommended. Item-4 (pain in forward stride and loading) was also problematic for participants, although it reached the “acceptable” level, possibly thanks to the accompanying figure. The authors suggest, following expert opinion, clarifying figures that do not substitute the text (e. g. initial and final position of confusing actions). In item-3 (extending the knee without resting the foot on the ground), an image with the subject seated could clarify the initial position.
Structural validity found two dimensions associated with "pain" and "physical activity", as Hernandez-Sanchez et al[25]. The groupings were: Items-2-3-4-5-6, clearly associated with "pain"; and items-1-7-8, where only items-7-8 were associated with physical activity.
Initially, item-1 (time we can sit without pain) appears to be more closely associated with sedentary behavior and, therefore, with the absence of repeated loaded flexion-extension movements typically seen in individuals with PT or PFP[6,15]. Nevertheless, it addresses a significant source of patellofemoral joint stress, not only due to static compressive force (knee flexion beyond 90º)[52], but also due to the prolonged duration of this force. The combined impact of these two elements—compression and time—suggests that both dynamic friction in the patellofemoral joint during physical and sports activities, and prolonged compression in static positions, may elicit similar painful symptoms in PFP. A comparative analysis of this issue could be of scientific interest. Although theoretical reasoning would support the inclusion of item 1 within the "physical activity" dimension, the authors still consider it to be a conflictive item regarding dimensionality, understanding that it would make more clinical sense in the "pain" group as established by[25], or even consider a third dimension[34,35].
Our results could also be justified by the fact that sitting (90º knee flexion and no movement) is a position that affects PFP and PT, but at different intensities. Mild PFP could suffer pain in a short time sitting, as opposed to PT, which requires more severity.
Construct validity showed a strong correlation between VISA-P and the PFP-specific questionnaires KOOS-PF and KPS.
VISA-P was previously correlated with specific PFP questionnaires, for the Spanish validation of the KPS[27], due to the similarity of the clinical symptoms, and the fact that there was no other specific questionnaire in Spanish. This study found values similar to ours, and even lower[4]. KPS and VISA-P were also correlated previously to establish convergent validity in the Spanish validation of VISA-P in PT[25]. KPS was also used to determine the convergent validity of KOOS-PF in the translation, adaptation and validation into Spanish, again obtaining similar values[3].
All this is evidence of the association that several experts find between PT and PFP, and consequently between their methods of functional assessment.
In terms of reliability, the internal consistency and test-retest reliability analyses revealed "adequate" reproducibility of the questionnaire according to Terwee et al[43]. The values in this study were similar to those found in the cross-cultural adaptation and validation of the original VISA-P questionnaire in Spanish[25] (Cronbach α: 0.752 vs 0.88; CI: 0.934 vs 0.99; respectively).
Within the same "adequate" range, the internal consistency found in VISA-P was slightly lower than that obtained in the Spanish validation of KPS[4] (0.77 vs 0.8) and in the Spanish validation of KOOS-PF[3] (0.826 vs 0.93). Even so, the items of each of the 3 scales correlated to describe the clinical symptoms of the subjects, making VISA-P suitable for use in this pathology.
Moreover, this study found a temporal stability of VISA-P well above that of KOOS-PF (0.932 vs 0.82)[3], suggesting greater reproducibility of VISA-P in research and in the clinic. For KPS, the values were similar (0.932 vs 0.99).
The interpretability did not find ceiling and floor effects, as was the case in[25], which contributed to demonstrating the validity of the questionnaire's application in PFP.
Summarizing the analyzed advantages and disadvantages of VISA-P, it proved to be a quick self-completion questionnaire, favoring its routine use in the clinical setting to obtain an overview of clinical symptoms. Compared to KOOS-PF and KPS, VISA-P was the fastest to complete. According to Hernandez-Sanchez et al[25], it was easy to understand and consequently easy to use. However, this study detected conflicts in item-8 for participants and for expert opinion, as mentioned above.
VISA-P was advantageous, like KOOS-PF and unlike KPS, for users who are physically active or involved in sports, especially for items-7-8. However, item-8 (how long can you do the activity), makes it impossible to use VISA-P to compare active subjects doing different activities at different intensities. As these data are not specified, the times are not comparable, i.e., 10 minutes of running & 10 minutes of walking. VISA-P is useful in intrasubject comparisons, again as KOOS-PF, to assess progression during treatment, its effectiveness or the evolution of the patellofemoral degeneration itself.
Regarding the limitations of the study, responsiveness could not be measured because it did not include interventions and the sample was only of affected knees. This could be the subject of prospective studies. Furthermore, criterion validity was excluded based on COSMIN recommendations (see methods).
The strengths are associated with the fact that a questionnaire initially designed and validated in PT is now validated in PFP and/or chondromalacia patella based on scientific evidence that associates both disorders.
Unlike other studies, the validation included an exploratory factor analysis, confirming similar dimensions of the questionnaire in both pathologies. It also establishes the usefulness of separate sets of items (components) to assess specific aspects: Pain or physical activity.
VISA-P proved to be a valid and reliable tool to functionally assess PFP and/or chondromalacia patella. The findings showed that VISA-P is feasible in clinical and research settings due to its quick and easy completion. This study suggests that VISA-P is appropriate for active and/or athletic subjects, as well as for intrasubject comparisons. However, comparisons between subjects are not suggested unless they are practicing the same sport at the same intensity.
The authors would like to acknowledge the confidence of our colleague Paul Visentini, lead author of the original validation of VISA-P; all the participants in the sample and all the experts who collaborated to the construct validity of the questionnaire. We would also like to thank the Research Group “Area of Physiotherapy CTS-305” of the University of Seville for their collaboration.
| 1. | Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 312] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 2. | Chamorro-Moriana G, Perez-Cabezas V, Espuny-Ruiz F, Torres-Enamorado D, Ridao-Fernández C. Assessing knee functionality: Systematic review of validated outcome measures. Ann Phys Rehabil Med. 2022;65:101608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 3. | Martinez-Cano JP, Vernaza-Obando D, Chica J, Castro AM. Cross-cultural translation and validation of the Spanish version of the patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF). BMC Res Notes. 2021;14:220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Gil-Gámez J, Pecos-Martín D, Kujala UM, Martínez-Merinero P, Montañez-Aguilera FJ, Romero-Franco N, Gallego-Izquierdo T. Validation and cultural adaptation of "Kujala Score" in Spanish. Knee Surg Sports Traumatol Arthrosc. 2016;24:2845-2853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Sisk D, Fredericson M. Taping, Bracing, and Injection Treatment for Patellofemoral Pain and Patellar Tendinopathy. Curr Rev Musculoskelet Med. 2020;13:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Rosso F, Bonasia DE, Cottino U, Dettoni F, Bruzzone M, Rossi R. Patellar tendon: From tendinopathy to rupture. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2:99-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Smith TO, Logan P. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One. 2018;13:e0190892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 317] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 8. | Muaidi QI. Rehabilitation of patellar tendinopathy. J Musculoskelet Neuronal Interact. 2020;20:535-540. [PubMed] |
| 9. | Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM. Patellofemoral Pain. J Orthop Sports Phys Ther. 2019;49:CPG1-CPG95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 225] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 10. | Núñez-Martínez P, Hernández-Guillen D. Management of Patellar Tendinopathy Through Monitoring, Load Control, and Therapeutic Exercise: A Systematic Review. J Sport Rehabil. 2022;31:337-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Saltychev M, Dutton RA, Laimi K, Beaupré GS, Virolainen P, Fredericson M. Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis. J Rehabil Med. 2018;50:393-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Cenni MH, Silva TD, do Nascimento BF, de Andrade RC, Júnior LF, Nicolai OP. Patellar tendinopathy: late-stage results from surgical treatment. Rev Bras Ortop. 2015;50:550-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Sprague AL, Smith AH, Knox P, Pohlig RT, Grävare Silbernagel K. Modifiable risk factors for patellar tendinopathy in athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52:1575-1585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 14. | Bazett-Jones DM, Huddleston W, Cobb S, O'Connor K, Earl-Boehm JE. Acute Responses of Strength and Running Mechanics to Increasing and Decreasing Pain in Patients With Patellofemoral Pain. J Athl Train. 2017;52:411-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Collins NJ, Vicenzino B, van der Heijden RA, van Middelkoop M. Pain During Prolonged Sitting Is a Common Problem in Persons With Patellofemoral Pain. J Orthop Sports Phys Ther. 2016;46:658-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Pereira PM, Baptista JS, Conceição F, Duarte J, Ferraz J, Costa JT. Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 17. | Kim S, Mangum LC, Glaviano NR. Influence of unilateral versus bilateral patellofemoral pain on physical activity, pain self-efficacy, and disability. Musculoskelet Sci Pract. 2024;73:103167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Collins NJ, Barton CJ, van Middelkoop M, Callaghan MJ, Rathleff MS, Vicenzino BT, Davis IS, Powers CM, Macri EM, Hart HF, de Oliveira Silva D, Crossley KM. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52:1170-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 212] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 19. | Crossley KM, Callaghan MJ, van Linschoten R. Patellofemoral pain. Br J Sports Med. 2016;50:247-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 20. | Rhon DI, Roy TC, Oh RC, Young JL. Sex and Mental Health Disorder Differences Among Military Service Members With Patellofemoral Syndrome. J Am Board Fam Med. 2021;34:328-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Togashi I, Nagao M, Nishio H, Nozu S, Shiota Y, Takazawa Y. Cross-cultural adaptation, validity, reliability and responsiveness of the Japanese version of the Victorian Institute of sports assessment for patellar tendinopathy (VISA-P-J). BMC Sports Sci Med Rehabil. 2023;15:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Décary S, Frémont P, Pelletier B, Fallaha M, Belzile S, Martel-Pelletier J, Pelletier JP, Feldman D, Sylvestre MP, Vendittoli PA, Desmeules F. Validity of Combining History Elements and Physical Examination Tests to Diagnose Patellofemoral Pain. Arch Phys Med Rehabil. 2018;99:607-614.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Churruca K, Pomare C, Ellis LA, Long JC, Henderson SB, Murphy LED, Leahy CJ, Braithwaite J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect. 2021;24:1015-1024. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 353] [Article Influence: 88.3] [Reference Citation Analysis (0)] |
| 24. | Chamorro-Moriana G, Espuny-Ruiz F, Ridao-Fernández C, Magni E. Clinical value of questionnaires & physical tests for patellofemoral pain: Validity, reliability and predictive capacity. PLoS One. 2024;19:e0302215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Hernandez-Sanchez S, Hidalgo MD, Gomez A. Cross-cultural adaptation of VISA-P score for patellar tendinopathy in Spanish population. J Orthop Sports Phys Ther. 2011;41:581-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Crossley KM, Macri EM, Cowan SM, Collins NJ, Roos EM. The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br J Sports Med. 2018;52:1130-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 27. | Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 879] [Cited by in RCA: 1017] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 28. | Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, Terwee CB. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual Life Res. 2018;27:1171-1179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1083] [Cited by in RCA: 1464] [Article Influence: 209.1] [Reference Citation Analysis (0)] |
| 29. | Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63:737-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2171] [Cited by in RCA: 3004] [Article Influence: 200.3] [Reference Citation Analysis (0)] |
| 30. | Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, Bouter LM, de Vet HC. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol. 2010;10:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1110] [Cited by in RCA: 1232] [Article Influence: 82.1] [Reference Citation Analysis (0)] |
| 31. | Mokkink LB, Elsman EBM, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures version 2.0. Qual Life Res. 2024;33:2929-2939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 31] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 32. | Villarejo D, Ortega E, Gómez M, Palao J. Design, validation, and reliability of an observational instrument for ball possessions in rugby union. International Journal of Performance Analysis in Sport. 2014;14:955-967. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Pérez-Gil JA, Chacón-Moscoso S, Moreno-Rodríguez R. Validez de constructo: el uso de análisis factorial exploratorio-confirmatorio para obtener evidencias de validez. Psicothema. 2000;12:442-446. |
| 34. | Frohm A, Saartok T, Edman G, Renström P. Psychometric properties of a Swedish translation of the VISA-P outcome score for patellar tendinopathy. BMC Musculoskelet Disord. 2004;5:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Zwerver J, Kramer T, van den Akker-Scheek I. Validity and reliability of the Dutch translation of the VISA-P questionnaire for patellar tendinopathy. BMC Musculoskelet Disord. 2009;10:102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Denegar CR, Vela LI, Evans TA. Evidence-based sports medicine: outcomes instruments for active populations. Clin Sports Med. 2008;27:339-351, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147-1157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 937] [Cited by in RCA: 1941] [Article Influence: 277.3] [Reference Citation Analysis (0)] |
| 38. | Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, Bouter LM, de Vet HCW, Mokkink LB. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27:1159-1170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 976] [Cited by in RCA: 1231] [Article Influence: 175.9] [Reference Citation Analysis (0)] |
| 39. | Aiken LR. Three coefficients for analyzing the reliability and validity of ratings. Educ Psychol Meas. 1985;45:131-142. [DOI] [Full Text] |
| 40. | Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A practical guide to their development and use. 5th ed. Oxford: Oxford Academic, 2015. [DOI] [Full Text] |
| 41. | Goursuch RL. Factor Analysis. 2nd ed. New Jersey: Lawrence Erlbaum Associates, 1983. |
| 42. | Martínez-Ortega RM, Tuya-Pendás LC, Martínez-Ortega M, Pérez-Abreu A, Cánovas AM. El Coeficiente De Correlación De Los Rangos De Spearman, Caracterización. Rev Habanera Cienc Médicas. 2009;8. |
| 43. | Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5565] [Cited by in RCA: 7322] [Article Influence: 385.4] [Reference Citation Analysis (0)] |
| 44. | Martínez Pérez JA, Pérez Martin PS. [Intraclass correlation coefficient]. Semergen. 2023;49:101907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 45. | Bland JM, Altman DG. A note on the use of the intraclass correlation coefficient in the evaluation of agreement between two methods of measurement. Comput Biol Med. 1990;20:337-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 469] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 46. | Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19:231-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 1305] [Article Influence: 65.3] [Reference Citation Analysis (0)] |
| 47. | Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, Liebau C. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2014;22:2264-2274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 150] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 48. | Ismail MM, Gamaleldein MH, Hassa KA. Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. 2013;49:687-698. [PubMed] |
| 49. | Hu H, Zheng Y, Liu X, Gong D, Chen C, Wang Y, Peng M, Wu B, Wang J, Song G, Zhang J, Guo J, Dong Y, Wang X. Effects of neuromuscular training on pain intensity and self-reported functionality for patellofemoral pain syndrome in runners: study protocol for a randomized controlled clinical trial. Trials. 2019;20:409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral Pain Syndrome. Am Fam Physician. 2019;99:88-94. [PubMed] |
| 51. | Lum ZC, Saiz AM, Pereira GC, Meehan JP. Patella Baja in Total Knee Arthroplasty. J Am Acad Orthop Surg. 2020;28:316-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 52. | Besier TF, Draper CE, Gold GE, Beaupré GS, Delp SL. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J Orthop Res. 2005;23:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 162] [Article Influence: 8.1] [Reference Citation Analysis (0)] |