Published online Mar 18, 2024. doi: 10.5312/wjo.v15.i3.285
Peer-review started: December 1, 2023
First decision: December 28, 2023
Revised: January 8, 2024
Accepted: February 5, 2024
Article in press: February 5, 2024
Published online: March 18, 2024
Processing time: 104 Days and 18 Hours
The traditional Gamma3 nail is a mainstream treatment for femoral intertro
To investigate the clinical efficacy of Gamma3 and Gamma3 U-blade for intertro
A computerized search for Chinese and English literature published from 2010 to 2022 was conducted in PubMed, Cochrane, CNKI, Wanfang, and VIP databases. The search keywords were gamma 3, gamma 3 U blade, and intertrochanteric fracture. Additionally, literature tracking was performed on the references of published literature. The data were analyzed using Revman 5.3 software. Two individuals checked the inputs for accuracy. Continuous variables were described using mean difference and standard deviation, and outcome effect sizes were expressed using ratio OR and 95% confidence interval (CI). High heterogeneity was considered at (P < 0.05, I2 > 50%), moderate heterogeneity at I2 from 25% to 50%, and low heterogeneity at (P ≥ 0.05, I2 < 50%).
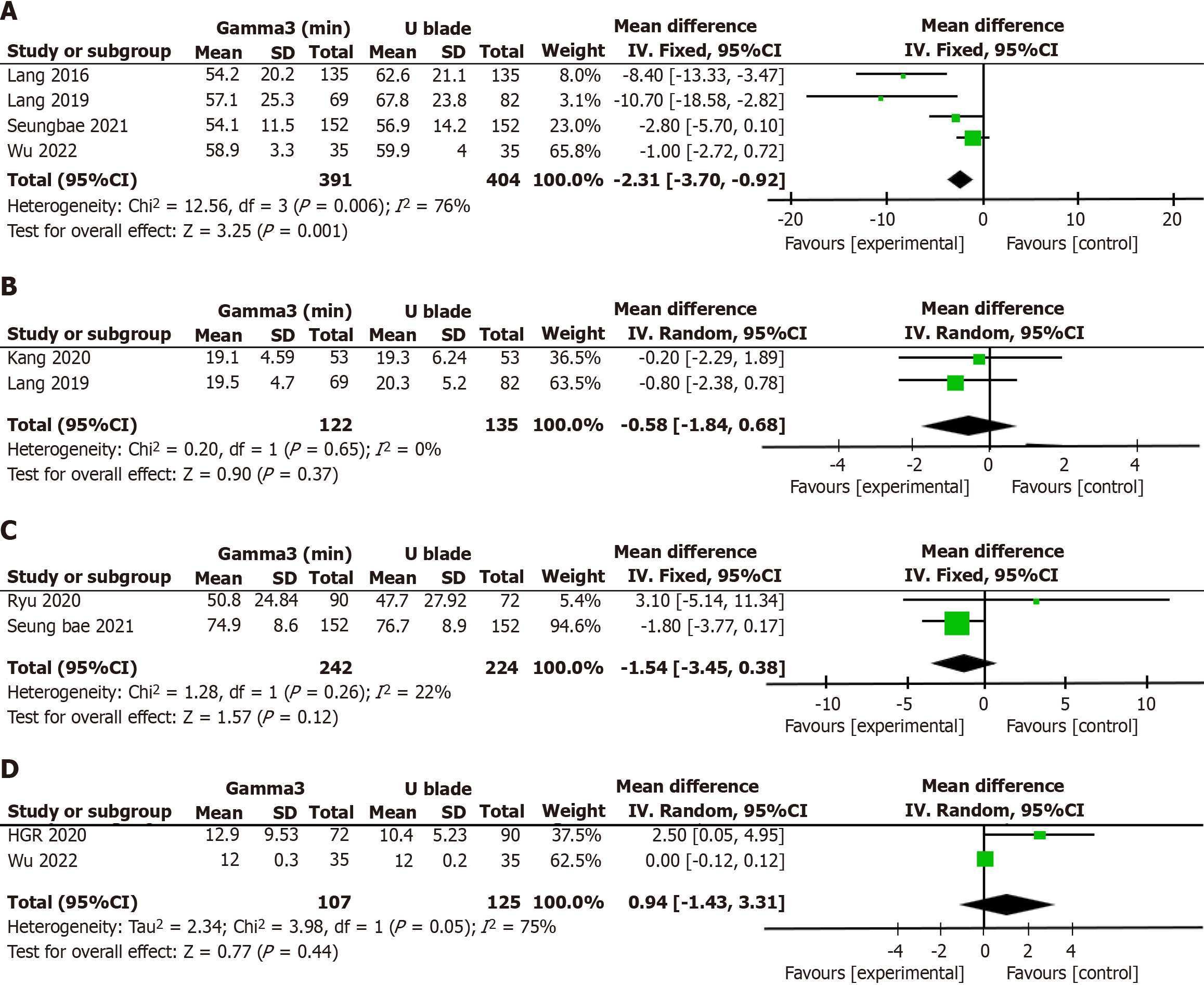
Following a comprehensive literature search, review, and analysis, six articles were selected for inclusion in this study. This selection comprised five articles in English and one in Chinese, with publication years spanning from 2016 to 2022. The study with the largest sample size, conducted by Seungbae in 2021, included a total of 304 cases. Statistical analysis: A total of 1063 patients were included in this meta-analysis. The main outcome indicators were: Surgical time: The Gamma3U blade system had a longer surgical time compared to Gamma3 nails (P = 0.006, I2 = 76%). Tip-apex distance: No statistical significance or heterogeneity was observed (P = 0.65, I2 = 0%). Harris Hip score: No statistical significance was found, and low heterogeneity was detected (P = 0.26, I2 = 22%). Union time: No statistical significance was found, and high heterogeneity was detected (P = 0.05, I2 = 75%).
Our study indicated that the Gamma3 system reduces operative time compared to the Gamma3 U-blade system in treating intertrochanteric fractures. Both surgical methods proved to be safe and effective for this patient group. These findings may offer valuable insights and guidance for future surgical protocols in hip fracture patients.
Core Tip: The Gamma3U-Blade, representing the third generation of Gamma nails, possesses several notable features: the incorporation of self-tapping tension screws enhances fixation stability and lowers the risk of cutting out. Anti-screw nails are ingeniously designed to aid in compressing the fracture end. Additionally, the option of dynamic lock or static force lock is available. Despite these advancements, comparative studies between Gamma3 and Gamma3U-blade are limited. Therefore, a meta-analysis of the existing literature was conducted to compare the clinical efficacy of these two surgical methods.
- Citation: Wu X, Gao B. Meta-analysis of the clinical efficacy of the Gamma3 nail vs Gamma3U-blade system in the treatment of intertrochanteric fractures. World J Orthop 2024; 15(3): 285-292
- URL: https://www.wjgnet.com/2218-5836/full/v15/i3/285.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i3.285
Intertrochanteric fractures are commonly seen lower limb fractures in elderly patients[1-4], with an increasing incidence[5]. Previous studies have indicated that early surgical intervention for intertrochanteric fractures can reduce mortality[6,7]. The prevalent clinical classification for these fractures includes the Evans and AO types[8,9]. Intramedullary fixation, characterized by its minimally invasive approach, reduced soft tissue damage, and high healing rate, has become the preferred surgical method for intertrochanteric fracture treatment[10].
Key representatives of this approach are the Gamma Nail, proximal femoral nail, proximal femoral nail antirotation (PFNA), TriGen InterTan hip fracture nailing system (InterTan), and trochanteric fixation nail advanced[11]. PFNA is particularly suitable for elderly patients with osteoporosis, but its usage has been extending to younger patients. During penetration, the PFNA spiral blade anchors in pressurized cancellous bone, but penetration can be challenging in patients with robust bone. PFNA surgery does not allow for pulp enlargement, and in cases of marrow cavity stenosis, there's a risk of shifting the fracture end during insertion, thus increasing operation time. The InerTAN system, with its superior anti-rotation capability, might not be appropriate for patients with small or thin bone marrow cavities. The use of two interlocking nails in InerTAN can lead to more bone loss at the femoral neck, leaving a large residual cavity post-fixation and heightening the risk of refracture. Additionally, the InerTAN system demands high technical skill and has a steep learning curve. The Gamma nail, designed by Halder in 1988, is considered a pioneering product for modern pulp nails. The Gamma3 nail, however, does not possess the robust anti-pulling effect of the PFNA spiral blade. To enhance this aspect of the Gamma3 nail, Lenich introduced the "U" type blade pull screw for Gamma nails, known as the Gamma3U-Blade system[12]. As the third-generation Gamma nail, the Gamma3U-Blade has distinctive features: it uses self-tapping tension screws to bolster fixation stability and mitigate the risk of cutting out. Its anti-screw nails are engineered to assist in compressing the fracture end, and it offers the choice between dynamic lock and static force lock[13,14].
The conventional Gamma3 nail remains the primary treatment for femoral intertrochanteric fractures. However, reports in the literature[15] suggest that the Gamma3U-blade system enhances the stability of the Gamma3 nail and lessens complication rates. Yet, comparative studies between the Gamma3U-blade and Gamma3 systems are sparse. This meta-analysis was thus conducted to investigate the clinical efficacy of these two surgical methods.
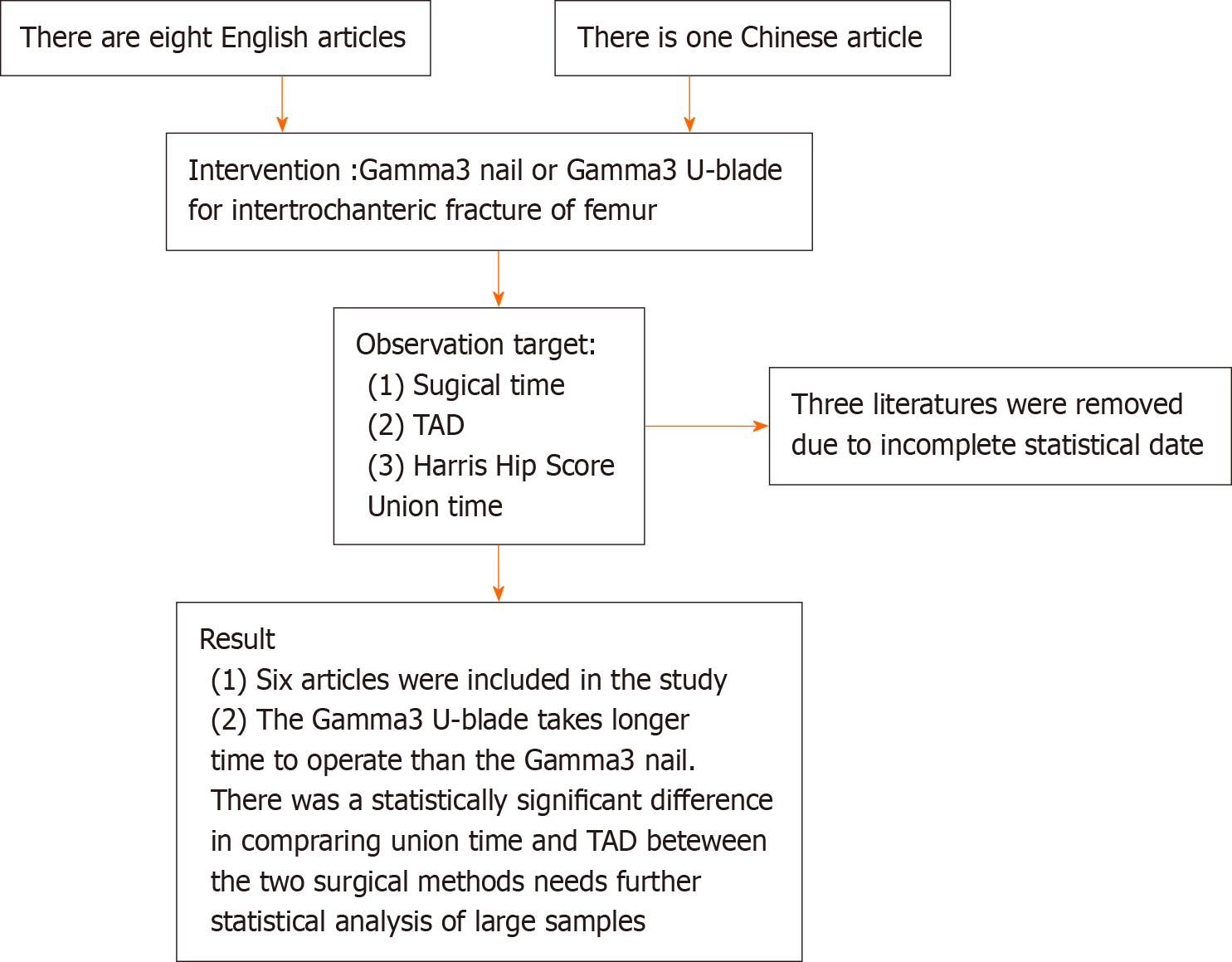
This study included Chinese and English clinical studies comparing the Gamma3 nail and Gamma3U blade in treating femoral intertrochanteric fractures, published between 2010 and 2022. The focus was on adult cases of femoral intertrochanteric fractures. The literature considered provided measurements such as operation time, intraoperative blood loss, postoperative hip function Harris score, postoperative tip-apex distance value (TAD), and functional recovery (Figure 1).
Excluded from the study were cases involving pathologic fractures, polytrauma combined with intertrochanteric fractures, treatment measures integrated with other surgical methods, repeatedly published literature, reviews, systematic evaluations, case reports, letters, basic research, and finite element analysis models.
General information: Authors, year of publication, sample size.
Main outcome indicators: Operative time, Harris hip score (HHS), TAD, and union time.
Data collection and analysis: The PRISMA statement guidelines were adhered to for conducting and reporting meta-analysis data. The data were analyzed using Revman 5.3 software. Two reviewers ensured the accuracy of data input. Continuous variables were reported using mean difference and standard deviation, and outcome effect sizes were expressed using ratio OR and 95% confidence interval (CI). High heterogeneity was defined as (P < 0.05, I2 > 50%), moderate heterogeneity as I2 ranging from 25% to 50%, and low heterogeneity as (P ≥ 0.05, I2 < 50%).
KEY (“Gamma3” or “Gamma3 nail” or “Gamma3 U-blade” or “U-blade”) and Femoral intertrochanteric fractures (“Femoral intertrochanteric fractures” or “intertrochanteric fractures”).
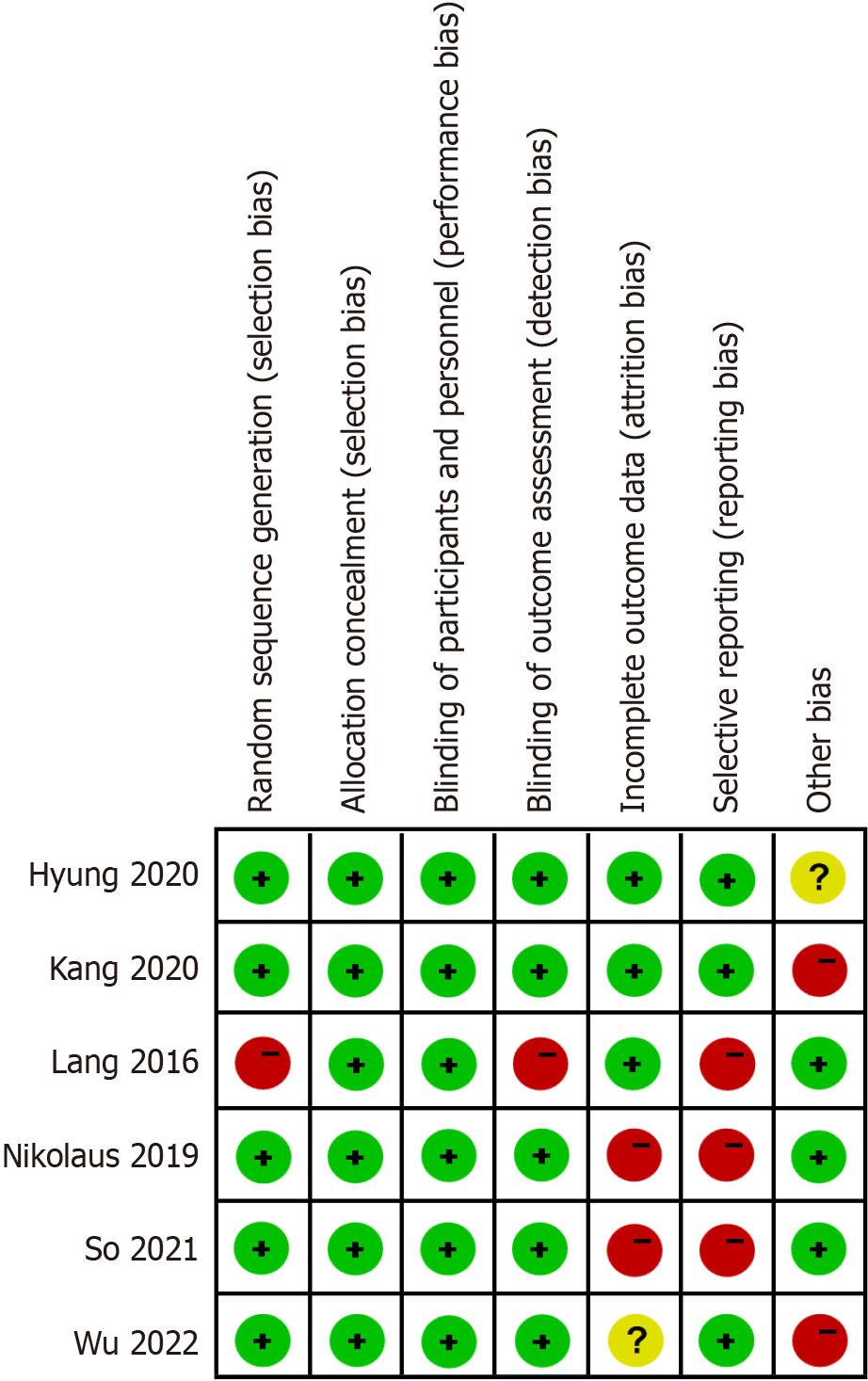
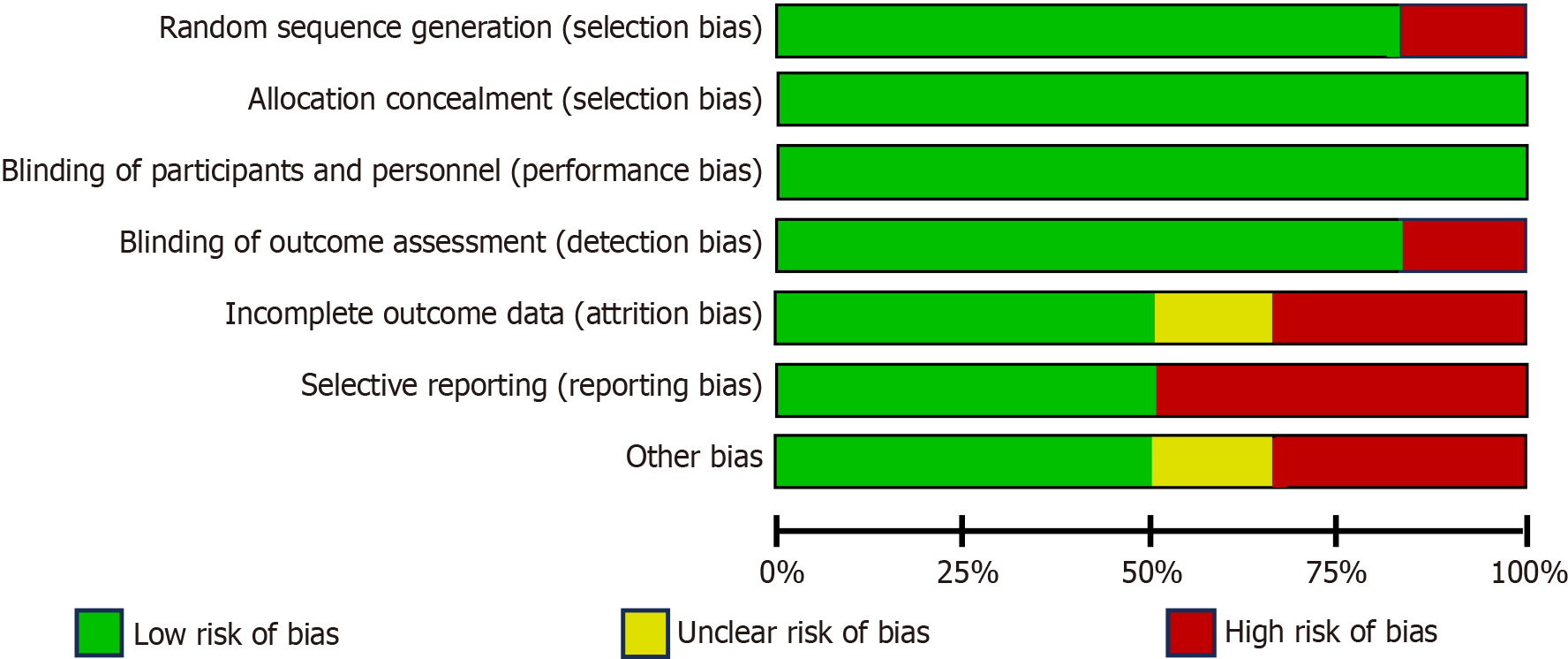
After a thorough search, review, and analysis of the literature, six articles were ultimately included in this study. These comprised five articles in English and one in Chinese, published between 2016 and 2022 (Supplementary Table 1, Figure 2). The study with the largest sample size, authored by Seungbae in 2021, encompassed a total of 304 cases (Figures 3 and 4).
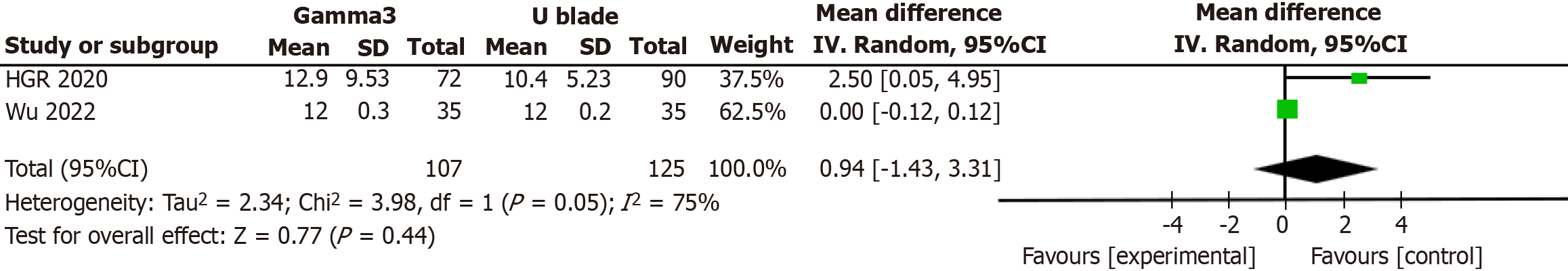
The meta-analysis included a total of 1063 patients. The primary outcome indicators were as follows: Surgical time: The surgical time for the Gamma3U blade system was longer compared to Gamma3 nails (P = 0.006, I2 = 76%). TAD: No statistical significance or heterogeneity was observed (P = 0.65, I2 = 0%). HHS: No statistical significance was found, with low heterogeneity (P = 0.26, I2 = 22%). Union time: No statistical significance was noted, accompanied by high heterogeneity (P = 0.05, I2 = 75%) (Figure 5).
The limited availability of controlled studies on Gamma3 and Gamma3 U-blade has restricted the number of comparisons in this meta-analysis. Variations in the focus of comparative follow-up across existing references also impacted the number of comparisons. Additionally, regional differences in fracture diagnosis among clinicians pose a risk of inclusion bias in the study.
Elderly patients are particularly susceptible to osteoporotic intertrochanteric fractures. Early surgical intervention for these fractures, along with hip joint functional exercises, can reduce complications like deep vein thrombosis, pressure ulcers, and joint stiffness[16]. Intramedullary fixation of intertrochanteric fractures offers effective anti-rotational stability. For unstable fractures (31-A2, 31-A3), intramedullary nailing fixation is the preferred treatment, a consensus in clinical practice[17]. Gamma3 nails, an evolution from Gamma nails for treating intertrochanteric fractures, address some limitations of the earlier design. However, some clinical studies have noted that the head nail of Gamma3 screws demonstrates poor stability and a higher risk of screw withdrawal[18]. The Gamma3 U-blade system incorporates a U-shaped blade, increasing the contact area between the femoral head, neck, and the screw, thereby enhancing head nail stability and reducing the risk of nail dislodgement. This meta-analysis revealed that the Gamma3 U-blade method required longer operative time compared to the Gamma3 nail method (I2 = 76%, P = 0.006).
The observed differences in operative time were statistically significant. However, no statistically significant difference was found in fracture healing time between the two internal fixation systems (P = 0.05). Presently, no literature conclusively states that the postoperative stability of the Gamma3 U-Blade system surpasses that of Gamma3 nails[19]. Therefore, patients undergoing intertrochanteric fracture treatment with intramedullary nailing can commence early functional exercises of the affected limb to reduce complications like joint stiffness. The literature selected for this meta-analysis did not systematically analyze when patients began functional exercises or their limb function scores, nor did it provide specific clinical analysis of functional exercise impacts. Patients with intertrochanteric femur fractures often have associated osteoporosis, necessitating further clinical analysis to determine if postoperative anti-osteoporosis treatment can expedite fracture healing and influence the timing of functional exercise commencement. This meta-analysis indicates that the Gamma3 U-blade system has a longer operative time compared to Gamma3 nails, with a statistically significant difference (P = 0.006). Gamma3 nails are preferable for frail patients with multiple underlying conditions who cannot withstand lengthy surgery. However, the Gamma3 U-blade offers superior postoperative stability and a lower risk of revision surgery due to internal fixation loosening and nail withdrawal, making it more suitable for elderly patients who can tolerate extended surgery.
Intertrochanteric fractures are susceptible to screw cutting after intramedullary nail fixation, which is closely related to three factors: the TAD, the greater trochanter, and the posterolateral wall. Literature suggests that a TAD value of 20-25 mm is safest, but debates on the optimal TAD value persist. The average TAD value in the literature included in this study ranged from 19.1-20.3 mm, with patients showing favorable clinical outcomes during follow-up. It can be inferred that an average TAD of 20 mm can yield good clinical results, but further large-scale studies are required to ascertain the precise upper and lower limits of this value.
This meta-analysis revealed no statistically significant difference in postoperative fracture healing time between the two surgical methods. Intertrochanteric fractures, primarily unstable, benefit from the abundant vascularity at the fracture ends, leading to a low rate of nonunion. The literature[20] highlights that effective reduction is key to the healing of intertrochanteric fractures. Both Gamma 3 nails and Gamma U-blade nails proficiently restore the force line at the fracture end and maintain stability of the fracture ends. Consequently, it can be inferred that both surgical methods positively impact fracture healing.
Clinical studies have determined that elderly and underweight patients, having lower bone mineral density (BMD), are more susceptible to intertrochanteric femur fractures[21]. These patients often present with preoperative anemia, while obese patients tend to experience more intraoperative blood loss. This study found no statistically significant difference in body mass index (BMI) and BMD values, possibly due to the wide age range of the patients involved, leading to non-significant differences in comparisons. Patients from different age groups exhibit varying metabolic rates, and their BMI and BMD values differ accordingly. For enhanced clinical relevance, dividing patients into age groups for comparative analysis could yield more significant insights.
The literature included in this meta-analysis indicates that operations using the U-blade tend to have longer durations compared to those with Gamma3, attributed to the additional steps required in the Gamma3U-blade procedure. Given that the Gamma3U-blade has been in use for a shorter time than Gamma3, advancements in clinical procedures and increased clinical experience may address the issue of prolonged surgical time. However, further statistical analysis regarding operation time necessitates a substantial number of clinical samples for a robust research foundation. Limitations of the Included Research Articles: While surgical intervention enhances survival quality in patients with intertrochanteric fractures, reports[22] indicate that the one-year postoperative mortality rate for these patients ranges from 11.9%-18.5%. It is plausible that long-term follow-up data may be skewed due to postoperative mortality, particularly in older patients, contributing to statistical bias in the study. Large-sample studies are required to minimize data bias related to mortality. Union time and TAD, vital scoring criteria post-intertrachanteric fracture, were accounted for in only two articles each, with no statistically significant differences observed in comparisons (P = 0.05 for Union time and P > 0.05 for TAD). Given the limited number of articles included, the data on Union Time and TAD may be biased. Currently, no prospective studies compare these two types of internal fixation methods. Therefore, the aim of this study is a meta-analysis of the efficacy of femoral trochanteric surgery, limited to clinical efficacy indicators for surgical outcome assessment. To ascertain whether significant differences exist in comparing Union Time and TAD between the two surgical methods, further statistical analysis with large samples is warranted.
Our study demonstrated that the Gamma 3 system is associated with reduced operative time in comparison to the Gamma 3 U-blade for treating intertrochanteric fractures. Both surgical approaches are safe and effective for this patient group. These insights may offer valuable recommendations and information for future surgical protocols in hip fracture patients. Nevertheless, to enhance the evidence base, further extensive multicenter prospective trials are necessary. A randomized controlled trial focusing on documented and quantified osteoporosis patients with extended follow-up periods is required.
The conventional Gamma3 nail remains the primary treatment for femoral intertrochanteric fractures. However, reports in the literature suggest that the Gamma3U-blade system enhances the stability of the Gamma3 nail and lessens complication rates. Yet, comparative studies between the Gamma3U-blade and Gamma3 systems are sparse. This meta-analysis was thus conducted to investigate the clinical efficacy of these two surgical methods.
To compare the clinical efficacy of Gamma3 and Gamma3 U-blade, and then to guide the clinical treatment.
Whether Gamma3 U-blade can replace Gamma3 nails, and whether there is room for further improvement.
The article chooses the traditional meta-analysis, and its main purpose is to analyze the existing data and guide the clinical treatment.
The Gamma3 U-blade procedure is longer than the Gamma3, but both surgical procedures are safe and effective, and further clinical studies are needed to optimize the Gamma3 U-blade procedure.
These insights may offer valuable recommendations and information for future surgical protocols in hip fracture patients. Nevertheless, to enhance the evidence base, further extensive multicenter prospective trials are necessary. A randomized controlled trial focusing on documented and quantified osteoporosis patients with extended follow-up periods is required.
Comparative surgical studies of Gamma3 U-blade and Gamma3 are missing, and numerous clinical surgery and prospective studies are needed.
We thank the professors from the School of Public Health of Southeast University for providing technical advice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mostafavinia A, Iran S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ
| 1. | Reynolds A. The fractured femur. Radiol Technol. 2013;84:273-91; quiz p.292. [PubMed] |
| 2. | Strøm Rönnquist S, Svensson HK, Jensen CM, Overgaard S, Rogmark C. Lingering challenges in everyday life for adults under age 60 with hip fractures - a qualitative study of the lived experience during the first three years. Int J Qual Stud Health Well-being. 2023;18:2191426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 3. | Refaeli E, Zarour S, Lior Y, Herut M, Rabkin V, Aharonov M, Ben-Tov T, Cohen B, Matot I. Prevalence of preoperative metabolic disturbances in elderly patients with hip fracture and their association with mortality - A retrospective cohort study. J Clin Anesth. 2023;88:111137. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Wang H, Cao X, Li B, Wu H, Ning T, Cao Y. Incidence and predictors of postoperative acute kidney injury in older adults with hip fractures. Arch Gerontol Geriatr. 2023;112:105023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Zeelenberg ML, Den Hartog D, Panneman MJM, Polinder S, Verhofstad MHJ, Van Lieshout EMM. Trends in incidence, health care consumption, and costs for proximal femoral fractures in the Netherlands between 2000 and 2019: a nationwide study. Osteoporos Int. 2023;34:1389-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 6. | Fischer H, Maleitzke T, Eder C, Ahmad S, Stöckle U, Braun KF. Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur J Med Res. 2021;26:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 92] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 7. | Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 172] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 8. | Sheehan SE, Shyu JY, Weaver MJ, Sodickson AD, Khurana B. Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know. Radiographics. 2015;35:1563-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Ricci WM. Stability of Intertrochanteric Femur Fractures. J Orthop Trauma. 2023;37:S1-S4. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Lu GL, Li SJ, Li WX. Biomechanical study of extramedullary and intramedullary fixation in the treatment of unstable intertrochanteric reversed-tilt fractures of the femur. Ann Transl Med. 2022;10:191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Maffulli N, Aicale R. Proximal Femoral Fractures in the Elderly: A Few Things to Know, and Some to Forget. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 84] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 12. | Lenich A, Vester H, Nerlich M, Mayr E, Stöckle U, Füchtmeier B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip--Blade vs screw. Injury. 2010;41:1292-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Born CT, Karich B, Bauer C, von Oldenburg G, Augat P. Hip screw migration testing: first results for hip screws and helical blades utilizing a new oscillating test method. J Orthop Res. 2011;29:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Kwak DK, Kim WH, Lee SJ, Rhyu SH, Jang CY, Yoo JH. Biomechanical Comparison of Three Different Intramedullary Nails for Fixation of Unstable Basicervical Intertrochanteric Fractures of the Proximal Femur: Experimental Studies. Biomed Res Int. 2018;2018:7618079. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Yoo J, Kim S, Choi J, Hwang J. Gamma 3 U-Blade lag screws in patients with trochanteric femur fractures: are rotation control lag screws better than others? J Orthop Surg Res. 2019;14:440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. Instr Course Lect. 2010;59:503-509. [PubMed] |
| 17. | Li J, Zhang L, Tang P. [Evolving concept in treatment of intertrochanteric fractures and development of internal fixation devices]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1-7. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Huang H, Xin J, Ma B. Analysis of complications of intertrochanteric fracture treated with Gamma 3 intramedullary nail. Int J Clin Exp Med. 2014;7:3687-3693. [PubMed] |
| 19. | Lang NW, Breuer R, Beiglboeck H, Munteanu A, Hajdu S, Windhager R, Widhalm HK. Migration of the Lag Screw after Intramedullary Treatment of AO/OTA 31.A2.1-3 Pertrochanteric Fractures Does Not Result in Higher Incidence of Cut-Outs, Regardless of Which Implant Was Used: A Comparison of Gamma Nail with and without U-Blade (RC) Lag Screw and Proximal Femur Nail Antirotation (PFNA). J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Marmor M, Guenthner G, Rezaei A, Saam M, Matityahu A. Reporting on quality of reduction and fixation of intertrochanteric fractures-A systematic review. Injury. 2021;52:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA. Nutritional Status and Nutritional Treatment Are Related to Outcomes and Mortality in Older Adults with Hip Fracture. Nutrients. 2018;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 120] [Cited by in RCA: 219] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 22. | Rui Y, Lu P, Li Y, Dai G, Ma B, Zou J, Chen H, Wang C. [Risk factors analysis for postoperative mortality of elder patients with intertrochanteric fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1538-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |