Published online Feb 18, 2024. doi: 10.5312/wjo.v15.i2.163
Peer-review started: October 19, 2023
First decision: November 23, 2023
Revised: December 19, 2023
Accepted: January 16, 2024
Article in press: January 16, 2024
Published online: February 18, 2024
Processing time: 110 Days and 8.9 Hours
Tourniquets are commonly used in elective extremity orthopaedic surgery to reduce blood loss, improve visualization in the surgical field, and to potentially reduce surgical time. There is a lack of consensus in existing guidelines regarding the optimal tourniquet pressure, placement site, and duration of use. There is a paucity of data on the relationship between the site of a tourniquet and postope
To explore the relationship between tourniquet site and intensity of post-operative pain scores in patients undergoing elective foot and ankle surgery.
Retrospective analysis of prospectively collected data on 201 patients who underwent foot and ankle surgery in a single institution was undertaken. Intraoperative tourniquet duration, tourniquet pressure and site, and postoperative pain scores using Visual Analogue Score were collected in immediate recovery, at six hours and at 24 h post-op. Scatter plots were used to analyse the data and to assess for the statistical correlation between tourniquet pressure, duration, site, and pain scores using Pearson correlation coefficient.
All patients who underwent foot and ankle surgery had tourniquet pressure of 250 mmHg for ankle tourniquet and 300 mmHg for thigh. There was no correlation between the site of the tourniquet and pain scores in recovery, at six hours and after 24 h. There was a weak correlation between tourniquet time and Visual Analogue Score immediately post-op (r = 0.14, P = 0.04) but not at six or 24 h post-operatively.
This study shows that there was no statistically significant correlation between tourniquet pressure, site and post-op pain in patients undergoing foot and ankle surgery. The choice of using a tourniquet is based on the surgeon's preference, with the goal of minimizing the duration of its application at the operative site.
Core Tip: Tourniquets are standard in orthopedic extremity surgery, aiding blood loss control and surgical efficiency. However, varying guidelines and a lack of consensus on tourniquet parameters exist. This study prospectively examines tourniquet site and duration effects on post-operative pain scores using data from 201 patients undergoing foot and ankle surgery.
- Citation: Mishra A, Barakat A, Mangwani J, Kazda J, Tiwatane S, Shaikh SMA, Houchen-Wolloff L, Kaushik V. Effect of ankle versus thigh tourniquets on post-operative pain in foot and ankle surgery. World J Orthop 2024; 15(2): 163-169
- URL: https://www.wjgnet.com/2218-5836/full/v15/i2/163.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i2.163
Tourniquets are frequently employed in orthopaedic procedures involving lower extremities[1]. Their primary purpose is to minimize blood loss, enhance surgical visibility, and streamline the surgical process[2]. Due to their ubiquity within the sphere of lower limb surgery, particularly foot and ankle, their use has been an interest of study to establish protocols and guidelines for their application. Nevertheless, the utilization of tourniquets has been linked to numerous local and systemic complications, one of which is postoperative pain[3].
The choice of tourniquet site and duration can significantly affect post-operative pain, and striking the right balance is essential[4]. The incidence of complications associated with tourniquet usage increases proportionally with the duration of tourniquet application. This is linked to the hypoxic conditions induced by tourniquet inflation, thereby increasing the likelihood of consequential hypoxic and reperfusion damage to soft tissues[3].
In foot and ankle surgery, the usual placement of a tourniquet is at the thigh, calf, or ankle. While thigh tourniquets are effective in minimizing intraoperative blood loss and maintaining a clear surgical field, they have been associated with a slightly higher risk of post-operative pain compared to ankle tourniquets[5]. The duration for which a tourniquet is inflated during surgery is another critical consideration. Prolonged tourniquet application has been associated with ischemic complications, muscle damage, and post-operative pain[6]. The challenge lies in finding the delicate balance between achieving adequate surgical conditions and minimizing tourniquet-associated complications. Other than minimizing tourniquet duration and optimizing occlusion pressure, the aim is to reduce the column of blood confined by the tourniquet use during surgery by utilizing an effective, well-tolerated and distal as possible.
We present the results of a comparative study investigating thigh vs ankle tourniquets applied for elective foot and ankle surgery in terms of effect on post-operative pain scores at different time points up to 24 h post-procedure. In addition, patient demographics such as age, gender, relevant medical conditions, and tourniquet time correlation to pain scores at those time points was also evaluated.
The study was performed at the University Hospitals Leicester, United Kingdom. The study protocol was reviewed and accepted by University Hospitals Leicester as a service evaluation project ensuring compliance with regulatory and ethical guidance.
201 consecutive patients who had elective foot or ankle surgery under tourniquet (ankle and thigh) were included. The recruitment was performed as per the pre-set inclusion and exclusion criteria outlined in the study protocol. The inclusion criteria included patients who had their foot or ankle procedures under thigh or ankle tourniquets. All trauma/fracture procedures were excluded as well as those with peripheral neuropathy or generalized pain disorders (e.g., fibromyalgia rheumatica). Patient demographics such as age, gender, and relevant pre-existing medical conditions such as peripheral vascular disease, cardiac disease, severe hypertension, coagulopathies, diabetes, and smoking status were collected. Patients were assigned to either ankle or thigh tourniquet groups in accordance with the surgeon's discretion. Recruited patients’ operative details such as tourniquet site, occlusion pressure, and length of the operative procedure were recorded in the patient’s operative records.
A standardized ankle tourniquet (Anetic Aid Ltd, Baildon, United Kingdom) was applied 5-10 cm above the ankle joint (586 mm length × 106 mm width) and thigh tourniquets (Anetic Aid Ltd, Baildon, United Kingdom) at mid-thigh (1074 mm length × 129 mm width). The tourniquet site was well padded in all patients with 3 rolls of 150 mm width cotton roll (Softban Ltd, United Kingdom) and tourniquet site occluded with an impervious U-drape. All limbs were either exsanguinated or elevated before tourniquet inflation; a tourniquet pressure of 250 mmHg for ankle tourniquet and 300 mmHg for thigh was applied. Local anaesthetic depending on the length of the incision and procedure performed (10-20 mLs of 0.5% Levobupivacaine) was injected into the incision site before dressings were applied. Whilst in the recovery bay and as soon as the patient was fully awake and co-operative, visual analogue score (VAS) was recorded in the immediate post-operative, six hours, and 24 h after the operative procedure. Any tourniquet related complications (skin burn and post-tourniquet syndrome) were recorded. The analgesic plan for all the included patients in the first 24 h was standardized with Paracetamol 500 mg and Dihydrocodeine 30 mg prescribed per-orally every 4-6 h and Oromorph 10-20 ug prescribed as required unless patient’s specific medical conditions or allergies precludes that.
Statistical analysis was performed using IBM SPSS software package version 20.0 (Armonk, NY: IBM Corp). The normality of variable distribution was assessed using the Kolmogorov-Smirnov test with mean, standard deviation (SD) and range used to describe normally distributed data. A Kruskal-Wallis test was employed in this study to assess whether there is a statistically significant relationship between the placement of tourniquets at different sites (thigh or ankle) and the reported pain scores at immediate, six-hour, and 24-h post-operative time points. Scatter plots were used to analyse the data and to assess the statistical correlation between tourniquet pressure, duration, site, and pain scores using Pearson correlation coefficient. The significance of the obtained results was established at the 5% level (P ≤ 0.05) and strong correlation considered for r values > 0.7 while weak correlation for those < 0.3[7].
A total of 201 patients were included in our analysis. There were 116 (57%) males while the remainder 85 (43%) were females. The mean age was 59.4 years (range = 23–95 years, SD = 15.6) with no statistically significant difference between the ankle and the thigh tourniquet groups (P = 0.4). The medical records and conditions were available for all patients, with 89 (44%) having a relevant pre-existing medical condition presenting a potential risk factor influencing the outcomes of tourniquet use. The distribution of patient’s demographics for the ankle and the thigh tourniquet groups is tabulated in Table 1.
| Group | No. of patients | Mean age (yr, SD) | Gender (Male/Female) | Pre-existing medical conditions |
| Ankle tourniquet | 87 | 58.3 (SD = 14.3) | 51/36 | 49 |
| Thigh tourniquet | 114 | 60.2 (SD = 15.8) | 65/49 | 40 |
| Total | 201 | 59.4 (SD = 15.6) | 116/85 | 89 |
A total of 87 patients (43%) had an ankle tourniquet while 114 patients (57%) had a thigh tourniquet. The average tourniquet time was 73.7 min (range = 10–149 min, SD = 28.7) with no statistical difference between the ankle and the thigh tourniquet groups (P = 0.12). There were two occurrences of tourniquet interruption after 120 min due to exceeding the recommended tourniquet time. Both of which happened in the thigh tourniquet group.
The mean immediate postoperative VAS was 3.9 (SD = 3.2, range = 0–10), mean six-hour VAS was 3.6 (SD = 2.6, range = 0-10), and mean 24-hour post-operative VAS was 5.8 (SD = 3.2, range = 0-10). Those patients who had a VAS of 10 at any time point were managed with elevation and escalated analgesia with resolution of their pain. None had any signs of compartment syndrome or concerning clinical findings. There were no reported tourniquet related complications for any of the included patients. Subsequent subgroup analysis showed no statistically significant relationship between the 24 h VAS and the patient’s age, gender or pre-existing medical conditions using multivariate regression analysis (P = 0.35, P = 0.18 and P = 0.25 respectively).
A paired t-test showed that there was a significantly higher mean VAS after 24 h as compared to the immediate post-operative (t = 61.2, P < 0.0001). We postulate that this is due to weaning of the local anaesthetic effect, post-operative oedema, increasing patient activity level and peaking of the inflammatory response[8].
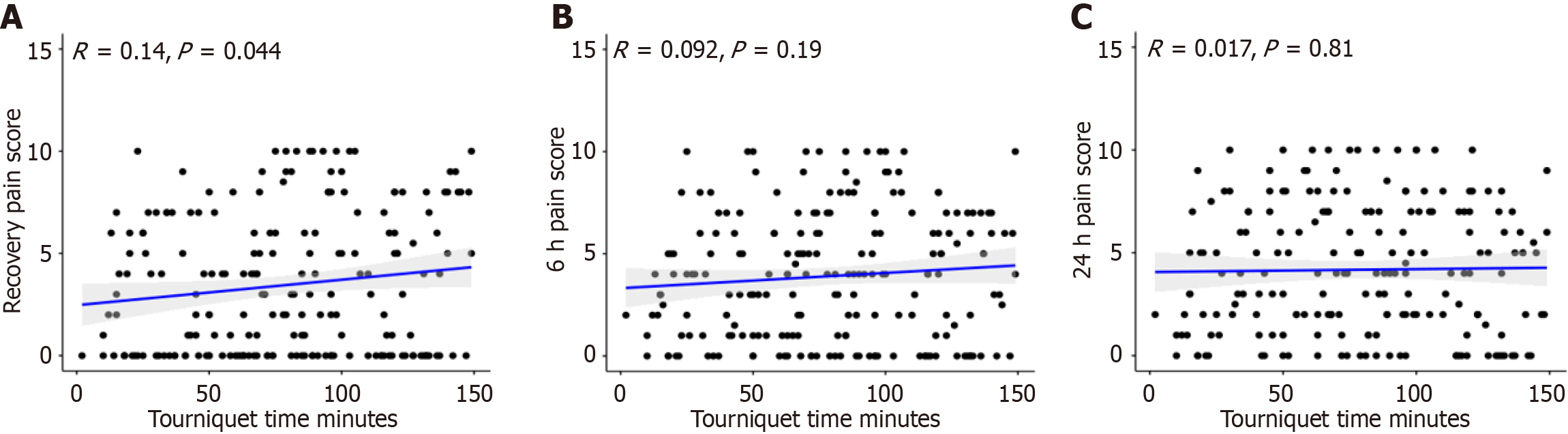
There was a very weak correlation between tourniquet time and recovery pain score (P = 0.04). However, the size of the correlation coefficient is rather small (r = 0.14). On the other hand, there was no statistically significant correlation between tourniquet time and the six-hour pain score (r = 0.09, P = 0.19) or the 24-h pain score (r = 0.01, P = 0.81) (Figure 1).
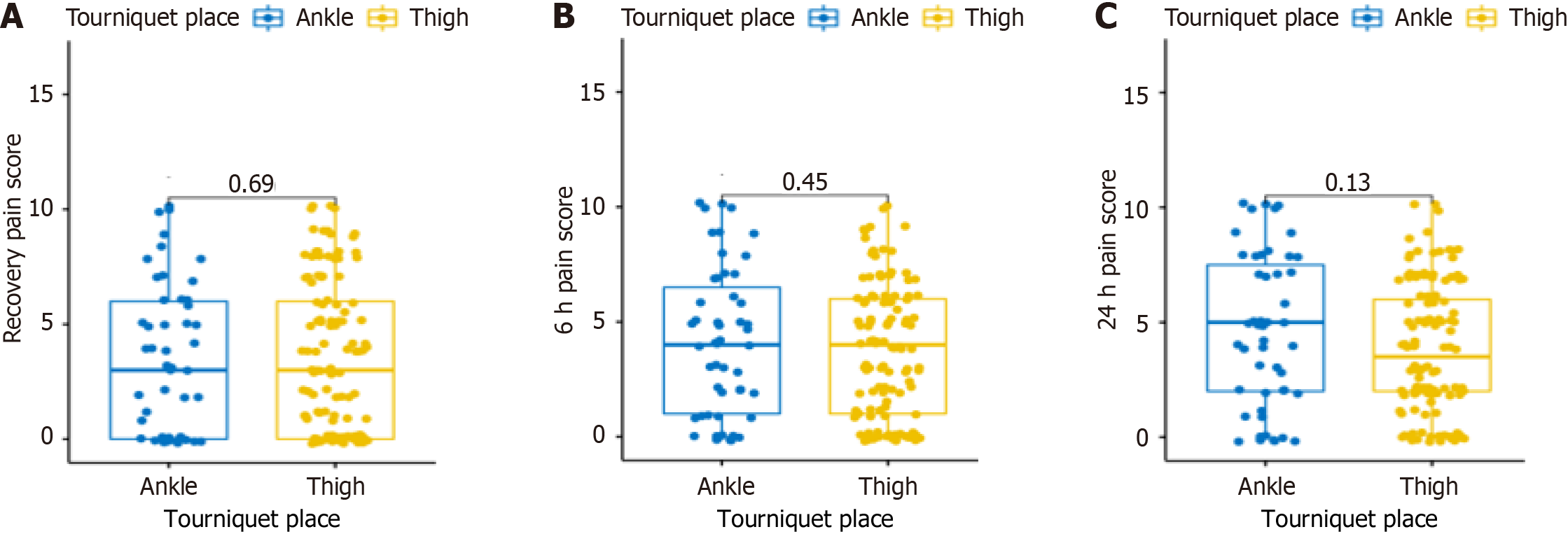
As for the tourniquet site, Kruskal-Wallis analysis demonstrated no significant difference between immediate post-operative (P = 0.69), six-hour (P = 0.45) and 24 h (P = 0.13) pain scores as opposed to the tourniquet site (thigh vs ankle) (Figure 2).
The use of tourniquet offers several potential benefits during foot and ankle surgery, including reducing operative time, minimizing blood loss, and thus improving visualization. However, tourniquet use is associated with well-documented drawbacks, which encompass muscle ischemia, wound complications, neurovascular injuries, deep venous thrombosis[9-11]. The most common side effect remains to be post-operative pain at the tourniquet site[12]. Exploring the effect of tourniquet site and duration on post-operative pain has been investigated in our prospective study.
Mitigating tourniquet related post-operative pain can improve patient rehabilitation and engagement with physiotherapy as well as reducing morbidity and hospital stay. As for tourniquet duration, it has been recommended that tourniquet time should not exceed 120 min for foot and ankle surgery[13,14]. It has been demonstrated that tourniquet-related complications increase as tourniquet time increases attributed to the hypoxic conditions and tissue ischaemia[15,16].
Although we observed no complications directly related to tourniquet use, we did identify a weak correlation between tourniquet duration and immediate post-operative pain scores, this correlation did not extend to the pain scores at six- or 24-hours post-operation. Other studies have observed a similar relationship between tourniquet duration and post-operative pain with even better pain scores when not using a tourniquet. In a randomized trial by Dimnjaković et al[17] assessing tourniquet vs no tourniquet in 50 consecutive ankle arthroscopy patients, they found less post-operative pain scores in the no tourniquet group. A systematic review encompassing four studies that investigated tourniquet usage in lower limb surgery yielded consistent results. The findings supported the notion that surgical procedures performed without the use of a tourniquet resulted in a notably shorter hospital stay. Furthermore, these tourniquet-free surgeries were associated with reduced post-operative pain and complication rates, as compared to surgeries where tourniquets were utilized[18].
On the other hand, and contrary to other studies, there was no significant correlation between the choice of tourniquet site—whether at the thigh or the ankle—and the post-operative pain scores at the various time points we assessed. While extensive research exists regarding the immediate consequences of applying a tourniquet at a particular site, there is a notable paucity of high-quality data elucidating the comparative risk profiles associated with tourniquet use at one location vs another with only three comparative studies concerned with foot and ankle surgery available. For instance, a comparative study evaluated the impact of calf and ankle tourniquets on pain scores immediately and 30 min after de
There are limitations to our study as we did not assess foot and ankle functional scores due to the heterogenicity in the operative procedures included. Furthermore, the allocation of both groups was according to surgeon’s preference and not randomized. However, despite these limitation, the authors believe that the findings of this study contribute to the current knowledge on this subject.
In conclusion, the use of tourniquet, both at ankle and thigh location, serves to meet the requirement of surgical field in foot and ankle procedures. Tourniquet location does not have a significant bearing on post-operative pain levels but minimizing tourniquet duration does. Future high quality randomized trials are warranted to derive conclusions more reliably about the value of using tourniquets in foot and ankle surgery.
Tourniquet utilization in orthopedic surgery is widespread for its benefits in blood loss reduction and enhanced surgical visibility, yet guidelines lack consensus on optimal pressure, placement, and duration. Despite its common use, there is limited understanding of how tourniquet site relates to postoperative pain in foot and ankle surgeries, highlighting a significant gap in existing knowledge.
The motivation behind this study stems from the existing ambiguity in guidelines regarding tourniquet practices in foot and ankle surgeries and the dearth of data on the connection between tourniquet site and postoperative pain. Understanding this relationship could not only improve patient outcomes but also guide surgical practices by providing evidence-based recommendations.
The primary objective of this study was to investigate the potential correlation between the tourniquet site and the intensity and duration of postoperative pain in patients undergoing foot and ankle surgery.
The study analyzed prospectively collected data from 201 patients who underwent foot and ankle surgery in a single institution. Key variables included intra-operative tourniquet duration, pressure, site, and postoperative pain scores assessed through Visual Analogue Score at immediate recovery, six hours, and 24 h post-operation. Data analysis involved scatter plots and statistical testing using Pearson correlation.
There was no correlation between tourniquet pressure, site, and postoperative pain in foot and ankle surgery patients. All patients had standardized tourniquet pressures, and the weak correlation found between tourniquet time and immediate postoperative pain did not persist at six or 24 h post-operatively.
The study demonstrates that tourniquet pressure and site do not significantly influence postoperative pain in foot and ankle surgery.
The absence of a correlation suggests that the surgeon's preference in choosing a tourniquet is not necessarily tied to minimizing postoperative pain.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: British Orthopedic Association, 38006.
Specialty type: Surgery
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Ewers A, Austria; Vaheb S, Iran S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Younger AS, Kalla TP, McEwen JA, Inkpen K. Survey of tourniquet use in orthopaedic foot and ankle surgery. Foot Ankle Int. 2005;26:208-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Lau B, Kothari V, Trowbridge S, Lewis TL, Ray R. Tourniquet use in ankle arthroscopy: A systematic review. Foot Ankle Surg. 2024;30:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Jensen J, Hicks RW, Labovitz J. Understanding and Optimizing Tourniquet Use During Extremity Surgery. AORN J. 2019;109:171-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Wilson AG. Current Insights and Recommendations For Tourniquet Use In Foot And Ankle Surgery–Part 3: Recommendations. Podiatry Today. 2021;34. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Hamad F, Rossiter N. Tourniquet use in trauma and orthopaedics, how and when: current evidence. Surgery (Oxford). 2023;. [DOI] [Full Text] |
| 6. | Gangadharan R, Roslee C, Kelsall N, Taylor H. Retrospective review of complications following long tourniquet time in foot and ankle surgery. J Clin Orthop Trauma. 2021;16:189-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:69-71. [PubMed] |
| 8. | Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287-2298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 405] [Cited by in RCA: 785] [Article Influence: 98.1] [Reference Citation Analysis (0)] |
| 9. | Kim YH, Kim JS, Kim DY. Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Joint Surg Br. 2007;89:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Huang HT, Su JY, Chang JK, Chen CH, Wang GJ. The early clinical outcome of minimally invasive quadriceps-sparing total knee arthroplasty: report of a 2-year follow-up. J Arthroplasty. 2007;22:1007-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33:1263-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Farhan-Alanie MM, Dhaif F, Trompeter A, Underwood M, Yeung J, Parsons N, Metcalfe A, Wall PDH. The risks associated with tourniquet use in lower limb trauma surgery: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2021;31:967-979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Dosani S, Devarakonda S. 104 Audit on Adherence to the BOAST Guidelines on the Safe Use of Intraoperative Tourniquets. Br J Surg. 2023;110 Suppl 7:znad258-648. [DOI] [Full Text] |
| 14. | Fitzgibbons PG, Digiovanni C, Hares S, Akelman E. Safe tourniquet use: a review of the evidence. J Am Acad Orthop Surg. 2012;20:310-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Noordin S, McEwen JA, Kragh JF Jr, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91:2958-2967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 16. | Altin R, Yesil M, Ozcan O, Karaca C, Sen S, Firat F. An investigation into the cellular-level adverse effects of tourniquet use on the infrapatellar fat pad in primary total knee arthroplasty: A prospective randomized study. Acta Orthop Traumatol Turc. 2023;57:283-288. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Dimnjaković D, Hrabač P, Bojanić I. Value of Tourniquet Use in Anterior Ankle Arthroscopy: A Randomized Controlled Trial. Foot Ankle Int. 2017;38:716-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 18. | Smith TO, Hing CB. The efficacy of the tourniquet in foot and ankle surgery? A systematic review and meta-analysis. Foot Ankle Surg. 2010;16:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Piyavunno C, Mahaisavariya B. Tourniquet pain: calf versus ankle tourniquet. J Med Assoc Thai. 2012;95 Suppl 9:S110-S113. [PubMed] |
| 20. | Xu FL, Yao Y, Zhang Y, Zhou LY, Shi TT, Fan J, Yu GR. Analysis of curative effect of low position tourniquet in calcaneal fracture surgery. [DOI] [Full Text] |
| 21. | Finsen V, Kasseth AM. Tourniquets in forefoot surgery: less pain when placed at the ankle. J Bone Joint Surg Br. 1997;79:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |