Published online Jan 18, 2024. doi: 10.5312/wjo.v15.i1.30
Peer-review started: September 26, 2023
First decision: November 14, 2023
Revised: November 26, 2023
Accepted: December 19, 2023
Article in press: December 19, 2023
Published online: January 18, 2024
Processing time: 111 Days and 7.1 Hours
Hip fracture is a common musculoskeletal injury in the elderly requiring surgery worldwide. The operative mainstay of intra-capsular hip fractures is arthroplasty with a smaller proportion for fixation.
To determine the most beneficial method of fixation for patients with intra-capsular hip fractures.
A registered audit from 2012-2018 was conducted on all intra-capsular hip fractures treated with 2 commonly used fixation methods. Patient notes, electronic records and clinical codes for cost benefit were evaluated. A validated quality of life measure was collected at least 1 year after surgery.
A total of 83 patients were identified with intra-capsular fractures undergoing fixation during the retrospective period. There were 47 cannulated cancellous screw and 36 sliding hip screw fixations with the case mix comparable for age, gender, co-morbidities and fracture configuration. There was no significant difference in blood loss, tip apex distance, radiation exposure, length of stay, radiological union time, collapse, avascular necrosis or re-operation between fixation methods. Logistic regression analysis demonstrated displaced intracap
No significant advantage was identified with differing fixation type, but irrespective there were a high number of patients requiring re-operation. This was predicted by initial fracture displacement and patient age. Arthroplasty may need to be carefully considered for health economics and patient benefit.
Core Tip: Both sliding and cannulated hip screws had undesirable outcomes in older patients with displaced fractures. More predictable methods of treatment such as hip arthroplasty should be considered for older patients with displaced fractures.
- Citation: Wiik A, Ashdown T, Holloway I. Health economics for intra-capsular hip fractures undertaking fixation. World J Orthop 2024; 15(1): 30-38
- URL: https://www.wjgnet.com/2218-5836/full/v15/i1/30.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i1.30
Hip fracture is the commonest musculoskeletal injury requiring surgery in the United Kingdom[1,2]. In 2017 alone, the national hip fracture database reported 65958 admissions with a 1 mo mortality of 6.9% and the disability leaving only half of patients returning to their premorbid state[3]. The total cost and burden to health and social services is over £1 billion per year along with 1.5 million National Health Service beds occupied annually[3-5]. A number that is set to rise with an aging population making health resource and provision allocation more important than ever[6].
Almost all hip fractures are managed surgically to enable early mobilisation, reducing complications associated with prolonged recumbency[7-9]. Surgical management is primarily dictated by fracture configuration and level, whilst also considering patient-specific factors such as physiological age, co-morbidities and pre-morbid function[10,11]. Specifically, operative management of intra-capsular fractures, which accounts for roughly 60% of all hip fractures, include a range of fixation and arthroplasty procedures[3,12]. Hip fixation whilst less successful than arthroplasty still comes as an attraction in order to maintain native anatomy and hip geometry whilst always having arthroplasty as a backup if it fails[12-14]. The evidence to date is equivocal for which fixation type is superior but a recent international multi-centre randomised controlled trial (FAITH) comparing standard cancellous and sliding hip screws found trends favouring sliding hip screws in certain subgroups of patients for reoperation rate[15]. With the cost implication to society of these fractures, health economics may play an important role in the decision making of fixation type to best manage them. This study therefore set out to determine the best fixation method routinely used for intra-capsular neck of femur fractures incorporating patient, surgeon and hospital metrics. The primary aim of this clinical practice study is to determine the most effective and beneficial way of treating these patients. The secondary aim is to determine which factors predispose to an undesirable fixation result. The null hypothesis was that no difference would be determined between fixation methods.
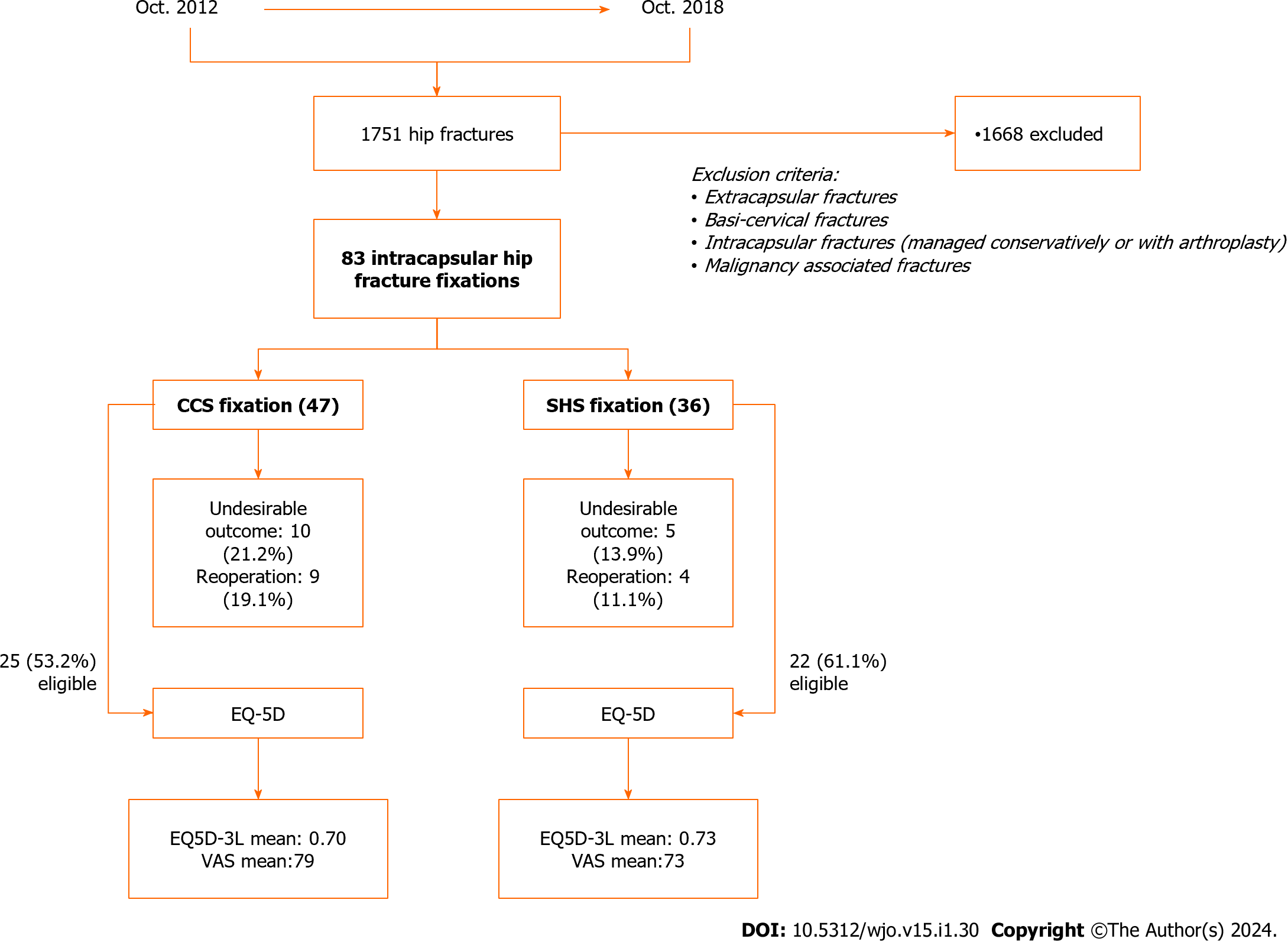
A retrospective analysis was conducted on all skeletally mature patients who sustained a closed intra-capsular hip fracture treated with either cannulated cancellous screws (CCS) or 2-hole sliding hip screw (SHS) fixation during the period from October 2012 to October 2018 (Figure 1). The study was conducted at a single district general hospital which regularly treats hip fractures using both fixation types and having no preference for either, with the requirement to proceed having achieved good-closed reduction in all planes intraoperatively. Patients with malignancy associated, basi-cervical or intertrochanteric fractures were excluded. The service improvement project was registered locally to follow good clinical governance practice guidelines.
Over the audit period, 1751 patients were admitted with a hip fracture, of which 83 had intra-capsular hip fracture fixation (Table 1) which met the study criteria. Fixation was achieved with either three partially threaded cancellous screws (6.5 mm diameter with 16 mm thread length) arranged in a reverse triangular configuration or with a single 13 mm sliding hip screw with a 47 mm barrelled two hole side plate affixed with two 4.5 mm cortical screws +/- 6.5 mm anti-rotational screw. The time of surgery was defined as time from admission to the emergency department to the time of surgery in theatres. All procedures were conducted by specialty trainee registrars with minimum 3 years’ experience under the supervision of a consultant. The patient setup was identical for both using a standard hip traction table using routine manoeuvres such as gentle traction with internal rotation. All patients before having closed reduction with fixation under fluoroscopy guidance had a single dose of intravenous antibiotic. All patients had hospital guided prophylaxis low molecular weight heparin peri-operatively unless contra-indicated. Patients were all seen by physiotherapy department day 1 post-operatively with a standardised protocol encouraging early mobilisation.
| Cannulated cancellous screw fixation | 2-hole sliding hip screw fixation | |
| Fixation group | 47 (56.6) | 36 (43.4) |
| Laterality | ||
| Left | 25 (53.2) | 18 (50) |
| Right | 22 (46.8) | 18 (50) |
| Garden classification | ||
| I | 24 (51.1) | 13 (36.1) |
| II | 8 (17) | 11 (30.6) |
| III | 10 (21.3) | 7 (19.4) |
| IV | 5 (10.6) | 5 (13.9) |
| Pauwels classification | ||
| I | 7 (14.9) | 1 (2.8) |
| II | 32 (68.1) | 24 (66.7) |
| III | 8 (17) | 11 (30.6) |
All clinical records were reviewed to determine age, sex, date of injury, date of surgery, pre-to-post operative haemoglobin count, post-operative weight bearing status and length of stay. Pre-operative imaging studies were reviewed to assess fracture configuration and displacement, classified according to the Pauwel and Garden classification systems, respectively with a simple modification (undisplaced or displaced) to the Garden classification for improved reliability[16,17]. Intra-operative imaging studies were reviewed to assess fixation type, reduction adequacy, fixation accuracy on the centre of the femoral head (tip-apex index) along with the radiation exposure time report, a surrogate for procedural complexity and radiation exposure. All available post-operative patient imaging studies were reviewed to assess fracture union time and the event of an undesirable outcome including significant collapse (> 5 mm), non-union, avascular necrosis (AVN) or implant failure. All images were accessed through the hospital electronic picture archiving and communication system and were reviewed by a senior surgeon. Follow up clinic letters were accessed using the electronic clinic letter system and reviewed further for an undesirable outcome.
Patients not flagged as deceased by hospital records were contacted by a trauma coordinator a minimum of 1 year after surgery. Patients were asked if they were satisfied with their outcome and if further operations following hip fixation was required. A validated quality of life measure, the EuroQol-5 dimensions 3-level (EQ-5D- 3L) index score and visual analogue scale score were collected to provide a single index value for health status[18].
Clinical coding data corresponding to the patients hip fracture hospital spell was obtained from the hospital clinical coding department. Data included international classification disease (ICD- version 10) diagnostic codes, OPCS-4 procedural codes and health resource group (HRG) coding records. Patient co-morbidity data was extracted and recorded based on number of chronic end-organ co-morbidities. HRG Codes were then converted into monetary tariffs based on service level agreements.
The current standard implants used for CCS and SHS fixation are the Stryker Asnis III and Omega 3 systems respectively (Mahwah, NJ, United States). The implant cost price for each procedure was obtained from the local procurement officer.
Statistical analysis was performed using SPSS (IBM SPSS Statistics, version 21) software. Normality was assessed using a Kolmogorov-Smirnov test. A Student-t and Mann-Whitney U test were used for parametric and non-parametric data. Fisher’s exact test was used for categorical variables. Logistical regression analysis was conducted to analyse factors affecting an undesirable result. Significance was set at 0.05 throughout. Results are reported as mean (range) and number (percentage).
Ethical approval was not sought nor required as it was part of a service evaluation project for the trauma and orthopaedic department. The service evaluation was registered (SUR.NP.19.003) with the local clinical governance team before the audit commencement to ensure hospital standard operating procedure adherence.
A total of 83 patients meeting the inclusion/exclusion criteria were evaluated. CCS fixation was utilised in 47 (57%) patients with 36 (43%) patients undergoing 2-hole SHS fixation. Fracture configuration was comparable between CCS and SHS groups, with undisplaced fractures (Garden I/II) 68.1% vs 66.7%, respectively and Pauwel type II the most common type representing 68.1% and 66.7% respectively. Fracture configuration for each fixation group is detailed in Table 1. The case mix was similar for age (65.7 vs 70.9 year), gender (66% vs 58.3% female) and end-organ co-morbidities (1.47 vs 1.42 mean). Patient demographics are summarised in Table 2.
| Cannulated cancellous screw fixation | 2-hole sliding hip screw fixation | |
| Mean age, yr (range) | 66 (18-91) | 71 (28-100) |
| Group by age | ||
| < 50 | 7 | 6 |
| > 50 | 40 | 30 |
| Gender | ||
| Male | 16 (34) | 15 (41.7) |
| Female | 31 (66) | 21 (58.3) |
| Number of organ co-morbidities | ||
| 0 | 13 (27.7) | 11 (30.6) |
| 1 | 13 (27.7) | 9 (25) |
| 2 | 11 (23.4) | 8 (22.2) |
| 3 | 6 (12.8) | 6 (16.7) |
| 4 | 4 (8.5) | 2 (5.6) |
| Mean | 1.5 | 1.4 |
There was no significant difference in blood loss (1.8 vs 1.5 g/dL), blood transfusions (2 in each group), tip apex distance (20 mm vs 23 mm, length of stay (15 vs 17 d), total radiation exposure time (53 vs 47 sec.) or union time (5.1 vs 5.8 mo) respectively for CCS and SHS (Table 3). There was a clear difference in post operative weight bearing instructions following the fixation types (Table 3). Partial weight bearing was most common advice, 45% of the time, in CCS fixation and fully weight bearing, 44% of the time for the SHS fixation.
| Cannulated cancellous screw fixation | 2-hole sliding hip screw fixation | |
| Time to surgery, h (range) | 39 (6-168) | 43 (7-408) |
| Tip-apex, mm (range) | 20 (10-45) | 23 (15-35) |
| Hb drop pre-op to post op, g/dL (range) | 1.8 (0.1-5.0) | 1.4 (0.3-4.2) |
| Radiation time, sec (range) | 53 (7-127) | 47 (35-75) |
| Length of stay, d (range) | 15 (3-69) | 17 (4-62) |
| Weight bearing status | ||
| NWB | 5 (10) | 2 (6) |
| PWB | 21 (45) | 7 (19) |
| FWB | 3 (6) | 16 (44) |
| Unclear | 18 (39) | 11 (31) |
| Union time, mo (range) | 5.1 (1-16) | 5.8 (1-12) |
| Health resource group, £ (range) | 5979 (517-11117) | 6862 (639-14323) |
In total there were 15 undesirable events with no statistical difference between groups for avascular necrosis, significant collapse, non-union, and cut-out (Table 4). Furthermore there was no statistical difference in re-operation rate between the groups with 9 (19.1%) and 4 (11.1%) for the CCS and SHS groups respectively. Most reoperations were metal work removal due to significant collapse causing soft tissue irritation. Each group had 3 patients having undergone revision total hip replacement.
| Undesirable outcomes | Cannulated cancellous screw fixation | 2-hole SHS fixation |
| Avascular necrosis | 1 (2.1) | 3 (8.3) |
| Significant collapse | 5 (10.6) | 1 (2.7) |
| Non-union | 3 (6.4) | 0 (0) |
| Cut-out | 1 (2.1) | 1 (2.7) |
| Reoperation | 9 (19.1) | 4 (11.1) |
In total there were 56 patients with undisplaced fractures and 27 with displaced fractures. With the undisplaced fractures only 9% (n = 5) resulted in an unsatisfactory outcome in comparison to 37% (n = 10) in the displaced group. When subdividing the patient by age, there were a total of 13 patients under the age of 50 with 5 having an undisplaced fracture and 8 having a displaced fracture. There were zero unsatisfactory results in the less than 50 years undisplaced fracture patients but 25% (n = 2) in the displaced fractures. When analysing patients over the age of 50 years, there were in total 70 patients with 51 undisplaced and 19 displaced fractures. Of the greater than 50 group with an undisplaced fracture, only 10% (n = 5) resulted in an unsatisfactory outcome as compared to 42% (n = 8) in the displaced group.
Binary logistic regression analysis of all characterisable variables showed that only a displaced (Garden 1-2 vs Garden 3-4) intracapsular hip fracture was a significant (P = 0.016) independent predictor of an unsatisfactory result. Hosmer-Lemeshow goodness of fit was P = 0.566 for the model and Nagelkerke R-Square was 0.287 with a classification accuracy of 82% and an odds ratio of 7.25 (CI: 1.45-36.31).
Of the 83 patients having undergone fixation only 47 (57%) were contactable or able to coherently converse for psychometric analysis. A breakdown of those included and reasons for exclusion are detailed in Table 5. Fixation groups were similar for the proportion valid to be included (74% vs 79%). There was no significant difference in EQ 5D-3L or VAS scores between fixation groups (0.70 vs 0.73 and 79 vs 73, respectively). Sub-analysis of all requiring revision total hip arthroplasty demonstrated a score of 0.62 and 69.
| Cannulated cancellous screw fixation | 2-hole sliding hip screw fixation | |
| Successfully contacted patients, n (%) | 25 (53.2) | 22 (61.1) |
| Deceased | 12 (25.5) | 4 (11.1) |
| Moved abroad | 2 (4.3) | 1 (2.8) |
| Dementia | 1 (2.1) | 4 (11.1) |
| Unable to contact | 7 (14.8) | 5 (13.9) |
| Time from surgery to PROM, months (range) | 42 (12-78) | 46 (12-98) |
| Valid (n) to answer questionnaire | 25/34 (74%) | 22/28 (79%) |
| EQ 5D 3 level (range) | 0.70 (0.07-1) | 0.73 (0.22-1) |
| EQ 5D visual analogue score (range) | 79 (40-100) | 73 (10-100) |
Clinical coding demonstrated no significant difference in the actual tariff received with a mean value of £5979 and £6862 respectively. Total CCS implant cost was £259.35 incorporating Asnis III 6.5 mm cannulated cancellous screws (×3), washers (×3), guidewire and drill bit. Total SHS implant cost was £146.13 assimilating SHS plate, 13 mm lag screw, cortex screws (×2), guidewire and drill bit.
Whilst much research has focused on the clinical outcomes of intra-capsular hip fracture fixation considerably less work has examined the health economics on the quality of life and financial effect of differing fixation methods[19,20]. This retrospective study found no significant cost-saving difference between CCS and SHS fixation methods. Both groups had similar lengths of stay and intra-operative radiation exposure, a surrogate for the cost of time. The mean HRG, which is the currency that each patient event attracts, were not statistically dissimilar but favouring the SHS with a mean of £6862 when compared to the CCS with a mean of £5979. Additionally both fixation types had comparative quality of life indices with a mean EQ-5D score of 0.70 and 0.73 and EQ-VAS of 79 and 73for CCS and SHS respectively. These quality of life findings for economical appraisal terms signifies reasonable return of everyday health and function considering the average index and visual analogue score without injury in the United Kingdom is 0.78 and 77for individuals greater that 65[21].
In terms of the health impact to the patient, both methods had relatively high rates of undesirable outcomes (21.2% CCS vs 13.9% SHS group) resulting in reoperation rates of 19.1% and 11.1% respectively. With greater failures predicted by fracture displacement and patient age over 50 years which is consistent with a recent study looking at displaced fractures treated with fixation[22]. The reoperation rates, demonstrating a non-significant trend favouring SHS, are comparable with those demonstrated in the FAITH study, a multi-centre randomised controlled trial comparing CCS and SHS fixation in an elderly with low impact fractures[15]. As found in the FAITH trial, the rates of AVN also appear to be more frequent in the SHS group. This is contrary to a previous systematic review which suggested CCS were more likely to develop AVN than SHS[23]. Non-union on the contrary was found to be more common for the CCS group but not statistically dissimilar and were identical to the FAITH trial at 6%[15]. The latter observation may be accounted by a recent biomechanical cadaveric study that found significant superiority for prevention of implant migration, varus tilt, femoral neck and leg shortening with a SHS when compared to CCS[24].
Yet, the most compelling finding in this study was the significant correlation of the degree of fracture displacement with the risk of an undesirable outcome following any fixation procedure, which is not unsurprising biomechanically and has been previously reported[25-28]. Previous trials have indicated poor outcomes with internal fixation in displaced hip fractures with one study reporting fixation failure rates as high as 44%[29], which was marginally higher than the 42% found in this study for the greater than 50 age group. A meta-analysis comparing internal fixation and arthroplasty in displaced hip fractures found arthroplasty significantly reduces the need for further revision surgery at the expense of greater operative blood loss and surgery time[30]. A subsequent national registry study in patients with displaced hip fractures found that those treated with arthroplasty had significantly less reoperations, reported less pain and had a better quality of life[25,31]. Most literature to date suggest that arthroplasty should be more readily considered in those with displaced fractures, particularly in the elderly[12,32-34].
This study is limited by a variety of factors. The basic retrospective analysis intrinsically suffers bias and lends to a fall out rate for data collection. This was seen, as near 20% of patients had deceased before patient reported outcome measures were collected. Surprisingly, this was higher in the CCS group despite being 10% younger. There was also a noticeable difference in the post-operative weight bearing instructions between the two fixations in our study, which is consistent with a multi-national survey studying surgeon preferences for managing femoral neck fractures[35]. In this study, operating surgeons preferred partial or non-weight bearing following CCS fixation whereas SHS fixation was associated with more full weight bearing status. There is evidence to suggest that a restriction in weight bearing status can compromise functional levels up to a year following surgery[36]. In this respect arthroplasty has been shown to be advantageous given the lack of restriction and improved mobility[37]. Finally, the small nature of this series can lead to statistical errors, particularly false negatives, which limit the conclusion, so caution must be taken with these results.
In conclusion, no significant benefit was seen with differing fixation types for intra-capsular hip fractures. Nonetheless, younger patients and undisplaced fractures fared better. The significant rates of undesirable outcomes seen in displaced fractures for patients over the age of 50 years suggest hip arthroplasty should be considered.
Hip fractures are common injuries requiring surgery.
Determining if there is an advantage between two common procedures for hip fracture fixation.
Identifying the best fixation method and identifying any patient factors which put them of a less desirable outcome.
An audit was conducted to identify patients who had hip fracture fixation during a 6 year period followed by a quality of life questionnaire along with cost analysis of patient having undergone hip fracture fixation.
Older patients (> 50 years) and displaced fractures were risk factors for undesirable outcomes in hip fracture fixation.
Alternatives from hip fracture fixation should be considered in displaced hip fractures and older patients requiring surgery.
Further research should look into fixation constructs along with patient metabolomics.
We thank Mohammad Hindawi, Claudette Christine, Jim Ramos and Ramil Taligatos for their contribution of data collection.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Willis-Owen C, Australia S-Editor: Liu JH L-Editor: A P-Editor: Chen YX
| 1. | Curtis EM, van der Velde R, Moon RJ, van den Bergh JP, Geusens P, de Vries F, van Staa TP, Cooper C, Harvey NC. Epidemiology of fractures in the United Kingdom 1988-2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone. 2016;87:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 301] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 2. | Johansen A, Boulton C, Hertz K, Ellis M, Burgon V, Rai S, Wakeman R. The National Hip Fracture Database (NHFD) - Using a national clinical audit to raise standards of nursing care. Int J Orthop Trauma Nurs. 2017;26:3-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | NHFD (2018) National Hip Fracture Database annual report 2018. 32. Available from: https://www.nhfd.co.uk/2018report. |
| 4. | Centre NCG The Management of Hip Fractures in Adults. Available from: https://www.nice.org.uk/guidance/cg124/evidence/full-guideline-pdf-183081997. |
| 5. | Ftouh S, Morga A, Swift C; Guideline Development Group. Management of hip fracture in adults: summary of NICE guidance. BMJ. 2011;342:d3304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Metcalfe D, Zogg CK, Judge A, Perry DC, Gabbe B, Willett K, Costa ML. Pay for performance and hip fracture outcomes: an interrupted time series and difference-in-differences analysis in England and Scotland. Bone Joint J. 2019;101-B:1015-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 7. | Hay D, Parker MJ. Hip fracture in the immobile patient. J Bone Joint Surg Br. 2003;85:1037-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Parker MJ, Handoll HH, Bhargara A. Conservative vs operative treatment for hip fractures. Cochrane Database Syst Rev. 2000;CD000337. [RCA] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Parker MJ, Lewis SJ, Mountain J, Christie J, Currie CT. Hip fracture rehabilitation -- a comparison of two centres. Injury. 2002;33:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Lu Y, Uppal HS. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr Orthop Surg Rehabil. 2019;10:2151459319859139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 11. | Turesson E, Ivarsson K, Thorngren KG, Hommel A. Hip fractures - Treatment and functional outcome. The development over 25 years. Injury. 2018;49:2209-2215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: a long-term follow-up of a randomised trial. Injury. 2010;41:370-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 13. | Lehtonen EJI, Stibolt RD Jr, Smith W, Wills B, Pinto MC, McGwin G Jr, Shah A, Godoy-Santos AL, Naranje S. Trends in surgical treatment of femoral neck fractures in the elderly. Einstein (Sao Paulo). 2018;16:eAO4351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Shah AK, Eissler J, Radomisli T. Algorithms for the treatment of femoral neck fractures. Clin Orthop Relat Res. 2002;28-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH) Investigators. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet. 2017;389:1519-1527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 218] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 16. | Van Embden D, Rhemrev SJ, Genelin F, Meylaerts SA, Roukema GR. The reliability of a simplified Garden classification for intracapsular hip fractures. Orthop Traumatol Surg Res. 2012;98:405-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | van Embden D, Roukema GR, Rhemrev SJ, Genelin F, Meylaerts SA. The Pauwels classification for intracapsular hip fractures: is it reliable? Injury. 2011;42:1238-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3986] [Cited by in RCA: 4412] [Article Influence: 152.1] [Reference Citation Analysis (0)] |
| 19. | Alolabi B, Bajammal S, Shirali J, Karanicolas PJ, Gafni A, Bhandari M. Treatment of displaced femoral neck fractures in the elderly: a cost-benefit analysis. J Orthop Trauma. 2009;23:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Haentjens P, Lamraski G, Boonen S. Costs and consequences of hip fracture occurrence in old age: an economic perspective. Disabil Rehabil. 2005;27:1129-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 21. | Janssen MF, Szende A, Cabases J, Ramos-Goñi JM, Vilagut G, König HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ. 2019;20:205-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 229] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 22. | Chang CH, Tsai SW, Wu PK, Chen CM, Chang MC, Chen WM, Chen CF. Suboptimal outcomes after internal fixation for displaced intracapsular femoral neck fractures in 50- to 60-year-old patients. Hip Int. 2020;30:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Parker MJ, Stockton G. Internal fixation implants for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2001;2001:CD001467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, Oswald M, Gueorguiev B. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J Orthop Trauma. 2017;31:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 184] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 25. | Gjertsen JE, Fevang JM, Matre K, Vinje T, Engesæter LB. Clinical outcome after undisplaced femoral neck fractures. Acta Orthop. 2011;82:268-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 26. | Parker M, Cawley S, Palial V. Internal fixation of intracapsular fractures of the hip using a dynamic locking plate: Two-year follow-up of 320 patients. Bone Joint J. 2013;95-B:1402-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46:484-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 257] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 28. | Sprague S, Schemitsch EH, Swiontkowski M, Della Rocca GJ, Jeray KJ, Liew S, Slobogean GP, Bzovsky S, Heels-Ansdell D, Zhou Q, Bhandari M; FAITH Investigators. Factors Associated With Revision Surgery After Internal Fixation of Hip Fractures. J Orthop Trauma. 2018;32:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Wang CT, Chen JW, Wu K, Chen CS, Chen WC, Pao JL, Chang CH, Lan TY. Suboptimal outcomes after closed reduction and internal fixation of displaced femoral neck fractures in middle-aged patients: is internal fixation adequate in this age group? BMC Musculoskelet Disord. 2018;19:190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 30. | Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85:1673-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 379] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 31. | Bartels S, Gjertsen JE, Frihagen F, Rogmark C, Utvåg SE. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop. 2018;89:53-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 32. | Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87:2122-2130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 272] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 33. | Jiang J, Yang CH, Lin Q, Yun XD, Xia YY. Does Arthroplasty Provide Better Outcomes Than Internal Fixation At Mid- and Long-term Followup? A Meta-analysis. Clin Orthop Relat Res. 2015;473:2672-2679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Parker MJ. Hemiarthroplasty versus internal fixation for displaced intracapsular fractures of the hip in elderly men: a pilot randomised trial. Bone Joint J. 2015;97-B:992-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Kakar S, Tornetta P 3rd, Schemitsch EH, Swiontkowski MF, Koval K, Hanson BP, Jönsson A, Bhandari M; International Hip Fracture Research Collaborative. Technical considerations in the operative management of femoral neck fractures in elderly patients: a multinational survey. J Trauma. 2007;63:641-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT. Non-weight-bearing status compromises the functional level up to 1 yr after hip fracture surgery. Am J Phys Med Rehabil. 2014;93:641-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 37. | Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, Hoelsbrekken SE, Utvåg SE. Screw Fixation Versus Hemiarthroplasty for Nondisplaced Femoral Neck Fractures in Elderly Patients: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am. 2019;101:136-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |