Published online May 18, 2023. doi: 10.5312/wjo.v14.i5.312
Peer-review started: March 2, 2023
First decision: March 24, 2023
Revised: March 27, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: May 18, 2023
Processing time: 77 Days and 9.1 Hours
Diabetic foot is a clinical manifestation of diabetes with a wide range of symp
Core Tip: Making a decision regarding amputation for diabetic foot patients is not as simple as following guidelines, such as scoring systems. There are many influential factors that come from different perspectives and are sometimes contradictory. Decision-making should consider other clinical and sociocultural factors, with the improvement of patient quality of life as the main goal.
- Citation: Primadhi RA, Septrina R, Hapsari P, Kusumawati M. Amputation in diabetic foot ulcer: A treatment dilemma. World J Orthop 2023; 14(5): 312-318
- URL: https://www.wjgnet.com/2218-5836/full/v14/i5/312.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i5.312
The rising prevalence of diabetes represents a major public health and socioeconomic burden on society. Diabetes presents relatively mild symptoms that generally go unnoticed at early stages. Patients commonly seek medical treatment in later stages when complications occur. Diabetic complications are associated with poor glycemic control[1].
Diabetic foot is one clinical manifestation of diabetes with a wide range of symptoms, including ulceration, osteomyelitis, osteoarticular destruction, and gangrene, as a consequence of advanced disease (Figure 1). Some diabetic foot cases present general indications for amputation, including dead limb, threat to the patient’s life, pain, loss of function, or nuisance[2]. Various scoring systems are applicable for clinicians to determine whether the indication for amputation is present, such as the mangled extremity severity score or diabetic ulcer severity score[3,4]. However, clinicians must address various factors that are not resolvable by these scoring systems in many cases. Therefore, decision-making is complicated. This article reviewed the contributing factors that are often encountered during decision-making in diabetic foot management, especially when it is related to amputation.
The etiology of diabetic foot ulcer is multifactorial. Poor glycemic control is the major underlying cause of advanced glycation end product (AGE) accumulation circulating in the body, which affects various organs. AGE formation is one of the main mechanisms responsible for vascular damage in diabetes patients, and it alters the angiogenic reaction[5]. Angiopathy indicates a vascular defect that is associated with angiogenic abnormalities. Angiogenesis itself results from the balanced functions of pro- and antiangiogenic molecules. Defects in this angiogenic balance may result in excessive or antiangiogenesis[6]. The activity of various regulators determine this angiogenesis switch. Vascular endothelial growth factor (VEGF) is a signal protein responsible for blood vessel formation. Hypoxia-inducible factors (HIFs) are transcription factors that respond to decreases in cellular hypoxia. Exposure to high glucose inhibits HIF and VEGF expression in normal cells[6].
Peripheral artery disease (PAD) may be described as atherosclerotic occlusive disease of the lower extremities. Chronic hyperglycemia, dyslipidemia, and insulin resistance in diabetes mellitus patients are responsible for vascular wall derangements via promotion of vascular inflammation, endothelial cell dysfunction, abnormalities in blood cells, and factors affecting hemostasis[7]. AGEs contribute to impaired angiogenesis via a reduction in collateral vessel development. AGEs also participate in the modification of extracellular matrix molecules, which promote atherosclerotic lesion development[8,9].
Macroangiopathy or microangiopathy has a tendency to inhibit nutrient/oxygen supply. These conditions put the foot at risk for ulceration and hinder the wound-healing process[6]. These vascular problems in combination with increased plantar pressure due to fibrosis-related Achilles tendon contracture and loss of protective sensory function result in recalcitrant complicated foot ulceration[10]. The involvement of infrapopliteal vessels is commonly found in diabetes patients with PAD. When ischemia is established, the restoration of pulsatile blood flow by revascularization is paramount for limb salvage. The treatment options are angioplasty, surgical bypass, or subintimal recanalization with varied results[11,12].
Infection is a common complication in diabetes, and it is particularly attributable to hyperglycemia-related immunosuppression in which polymorphonuclear lymphocyte activity is hindered. Infection results in prolonged inflammation that prevents wound healing and keeps the microorganism portal of entry open, which eventually causes further infections[13]. Diabetic foot infection is difficult to manage. Timely diagnosis and appropriate intervention are essential in management strategies. Diabetic foot osteomyelitis (DFO) is the consequence of a soft tissue infection that spreads into the bone, and it involves the cortex first then the marrow. DFO showed an increase in multidrug-resistant organisms, primarily methicillin-resistant Staphylococcus aureus or extended-spectrum beta-lactamase-producing bacteria[14,15]. The presence of osteomyelitis impedes infection control and raises the further need for medical treatment and surgeries[16]. Osteomyelitis requires surgery to remove portions of bone that are infected or dead. Although an aggressive surgical approach may be mandatory, retrospective studies showed that conservative treatment effectively promoted wound healing and reduced the risk of major amputations[14,17]. Recurrent ulcers are a significant cause of hospitalization and amputation[18].
Although diabetic foot ulcer is generally painless, it is viewed as the main reason for ulcer formation due to the loss of protective sensory function, and as many as 27% of patients experience painful diabetic peripheral neuropathy (DPN) to various degrees[19]. However, severe neuropathy is not the only cause of pain because there are other causes precipitating pain, including ischemia, infection, and oxidative stress-related mechanisms. Other than clinical findings, DPN may be diagnosed using several adjunct examination tools, such as nerve conduction studies. One of the newest tools is the assessment of transcutaneous oxygen pressure (TcPO2), in which the sitting-supine position difference in TcPO2 is higher in DPN patients than control subjects[20]. Various drugs have been introduced to address this problem, including selective serotonin and norepinephrine reuptake inhibitors, anticonvulsant agents, and opioid receptor agonists, but pain relief remains poor for most patients[21].
Longstanding diabetic foot, particularly when treated insufficiently, may produce some disabling deformities. The wound may be healed in this condition, but functional gait or ambulation is hindered. When physical activity is decreased, static positioning with fibrotic changes within the muscle will lead to contracture formation. Considering the muscle imbalance between the anterior and posterior groups, equinus contracture will likely develop[10]. Combined with muscle atrophy resulting from disuse and neuropathy, deformity and function loss may occur and result in a condition called damned nuisance, in which the limb is functionless, and amputation followed by prosthesis application would be a better solution. The deformity can also occur from osteoarticular destruction or prior autoamputation.
Amputation is generally the last choice for the treatment of non-salvageable limbs[22]. The main indications for amputation include various conditions, such as posing a threat to the body, such as the spreading of infection or tumors, the presence of necrotic tissue that constitutes a medium for pathological microorganism growth and a functionless limb, and some situations in which the patient and clinician believe that amputation will yield better results in overall function and quality of life in the absence of dead or dangerous limbs. Clinical decision-making on whether to amputate or to determine the amputation level frequently deviates from the factors that the patient and surgeon initially considered when the patient first presented with diabetes.
Amputation is divided into major or minor, according to its level. Major amputation is defined by any ankle disarticulation, transfemoral amputation, or transtibial amputation, and minor amputation is defined as a toe or transmetatarsal amputation[23]. Determining the amputation level is critical to the efficacy of management. Amputation should be performed at a level with sufficient blood supply for wound healing. Arterial angiography, Doppler ultrasonography, and perfusion pressure are acceptable methods. The latest advanced examination tools, such as transcutaneous oxygen pressure measurement, are reliable in predicting wound healing in diabetic foot[24]. Soft tissue coverage should also be considered in deciding the amputation level. For great toe gangrenes, ray amputation is preferred over metatarsophalangeal joint disarticulation despite good blood supply and biomechanical advantages of the latter. Less soft tissue bulk and higher pressure at the distal part result in eventual wound breakdown. Exposed cartilage following disarticulation may be a source of infection via necrotic tissue formation[22]. In addition to local vascular status, systemic condition will also determine the result. Lower albumin and higher glycated hemoglobin, C-reactive protein, white blood count, and creatinine levels are determinants of failed amputations that need subsequent reamputation[25]. Amputation is contraindicated in these situations and delayed until systemic improvement is achieved, except in emergency situations.
Despite the clear clinical findings prompting amputation, the negative perception of amputation remains, which results in hesitation to undergo amputation[22]. The ability to cope with an amputation is affected by clinical measurements, cosmesis, cultural issues, social support, and the patients’ pre-amputation coping style[26]. Although many patients refuse amputation and are discharged against medical advice, they often request that the surgeon perform amputation as distally as possible without understanding the indications. The fact that amputation may be perceived as a taboo makes discussion with patients and their relatives difficult[27].
Leg amputation is related to increased dependence. In addition to the medical benefit obtained from well-indicated amputation, function may be restored using proper prosthetics to regain the patient’s independence. However, the recovery of function is not solely based on prosthetics. Older age, poor balance, previously low function level, and higher amputation level are some determinants of disability status[26]. Considering the physical demands, amputee patients spend more energy during walking than able-bodied persons. The energy expenditure of transfemoral amputees is higher than transtibial amputation[28]. Therefore, choosing the amputation level should also be in concordance with further postoperative rehabilitation plans.
In regard to decision-making for amputation, various factors may be determinants. Choosing the level of amputation is the mainstay of treatment, but the timing of surgery is also important.
While establishing the indication is paramount, its contraindication is also critical. The general contraindication for amputation is the patient’s inability to tolerate anesthesia or the surgery itself, such as the accompanying systemic problems. Amputation at a particular level is contraindicated when inadequate blood supply for wound healing is encountered, when the infarcted area is undetermined, or when malnutrition occurs that hinders wound healing. Therefore, amputation is contraindicated when the quality of life is reduced afterward.
PAD and infections are the main causes of lower-leg amputations. Limb salvage in diabetic patients with PAD requires comprehensive management, including medical therapies. Other than glucose-lowering and lipid-lowering drugs, these patients need medications that aim to improve vascular functions, including antiplatelet therapy, protease-activated receptor-1 antagonists, anticoagulants, or vasodilators[29]. Due to ischemic and neuropathic pain, many diabetic foot patients continually consume analgesics, including several anticonvulsants[21]. Antihypertensive and antithrombotics are the major medications related to polypharmacy management for the elderly population, which increase the risk of adverse drug reactions (ADRs)[30]. Chronic kidney disease occurs as a diabetic complication via renal fibrosis. Therefore, longstanding drug administration in limb preservation should be monitored carefully. Deprescription should be considered to avoid ADRs. PAD is difficult to treat in diabetes patients due to various comorbidities. Atherosclerotic lesions are multilevel with a high prevalence of long occlusions. New techniques and technologies have been introduced for addressing PAD with various results that were likely related to the individual patient conditions[31,32].
Revascularization is a procedure to restore blood supply to the tissue by addressing the blocked blood vessels. The aim is to salvage the limb by healing the trophic disorder. The indications included critical ischemia with some suggestive vascular examination findings (arterial pressure < 50 mmHg or TcPO2 < 30 mmHg). However, prerequisite conditions must be met, including a satisfactory support bed, a distal artery of a good caliber, and the presence of a plantar arch[11]. Vascular surgeons generally choose between endovascular procedures (transluminal or subintimal), bypasses, or hybrid techniques that include both procedures. The choice of revascularization technique depends on the type of lesion, the presence or absence of stenosis, and thrombosis and their length[11]. Iatrogenic injuries were reported but were mostly self-limited and of minimal clinical significance. Some life-threatening complications may occur, including ruptures, perforations, and pseudoaneurysms. Patient subpopulation selection is important to avoid unpredicted complications[33]. The main objective of revascularization is wound healing and limb salvage. At the one-year follow-up, 60% or more ulcers had healed with endovascular procedures or open bypass surgery. However, the overall results demonstrate improved rates of revascularization compared to conservative treatment[31].
Revascularization is mandatory in ischemic limbs for wound healing and as a prerequisite for further surgical procedures, including debridement and amputation. Otherwise, re-amputation will likely be needed[22]. Many patients presented contraindications for minor or major amputation, systemic or local, including unfeasible revascularization. Autolytic debridement may be an option in this setting, or major amputation at the safe level. Autolytic debridement itself is safe because it uses the natural ability of the body’s own enzymes to remove dead tissues. To achieve autolytic debridement, the maintenance of a moist local wound environment is paramount[34].
Regarding limb salvage options, wound bed preparation via serial debridement is important, initially to limit the spread of infection. There are various advanced treatment options for recalcitrant diabetic foot wounds, such as hyperbaric oxygen therapy and platelet-rich gel treatment. Hyperbaric oxygen therapy involves the patient entering a pressurized room and breathing almost pure oxygen, which increases the amount of oxygen in the bloodstream and eventually boosting oxygen flow to the wound. Hyperbaric oxygen therapy offers great benefit in diabetic foot ulcer treatment and the reduction of amputation[35,36]. Autologous platelet-rich gel therapy is another option that effectively improves the healing of diabetic foot ulcers by increasing the concentration of platelets and growth factors in the wound and improving the surrounding microenvironment[37]. When the infection is controlled and granulation induces healing, limb reconstruction can proceed. Therefore, vascular flow is predominant. Thorough evaluation and approaches are needed to ensure this reconstructive procedure. Small, vascularized areas with no bone exposed may be grafted for nonbearing areas or local flaps in weight-bearing areas. Complex wounds are considerable for limb reconstructive procedures. Either decision must be made by the team and family[38].
Other than clinical measurements, patients’ quality of life is an important factor to evaluate. Diabetic foot has a negative impact on patient quality of life. Pain from ischemia, dependent status, daily ulcer dressing, and unemployment stress were some the major causes of decreased quality of life[39]. Considering the frustrating circumstances and physical deconditioning caused by prolonged immobilization, early major amputation may be a viable option. With early major amputation followed by appropriate prosthesis use, particularly in patients who had lower possibility of successful limb salvage, deconditioning may be avoided, and quality of life is preserved or even improved. Cost analysis must also be considered. Earlier amputation may decrease the costs from the length of hospital stay, repeated surgery, medications, and daily expense. However, patients undergoing major amputation will need proper rehabilitation exercise and prostheses that may be costly as well[40]. Therefore, decisions should be made carefully and promptly.
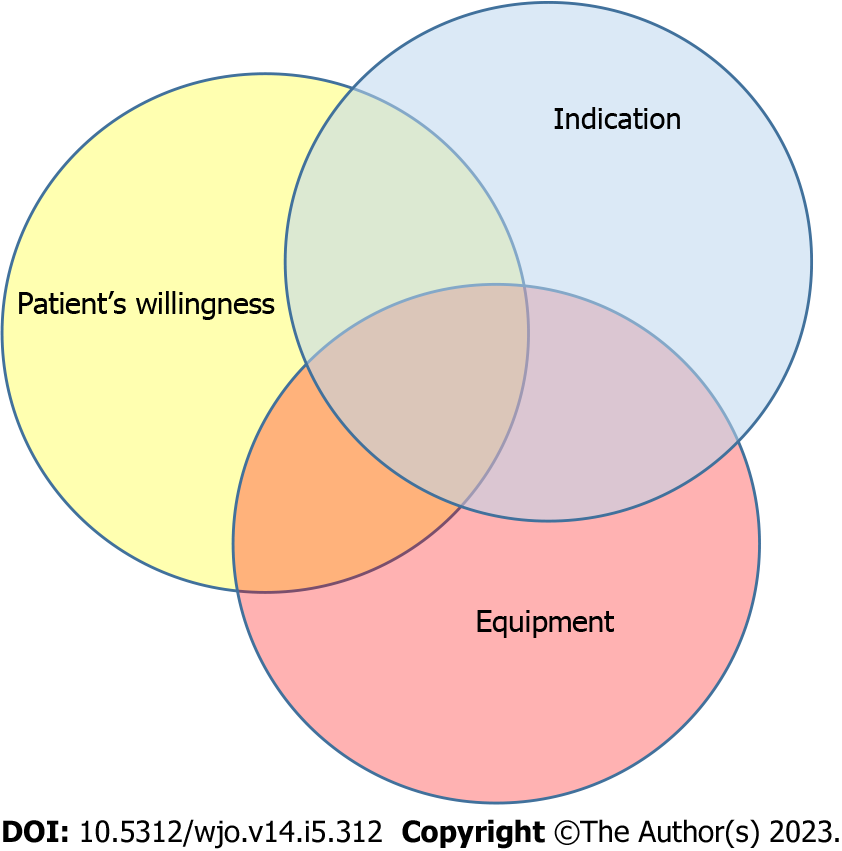
Amputation is an option for patients with diabetic foot ulcers. Although there are absolute or relative indications for amputation, there is also a clinical decision algorithm to determine whether a limb can be salvaged. However, various influencing factors should also be considered (Figure 2). The objective is to reach an immediate optimum state for the patient and increase their quality of life. In contrast to clinical discussion, cultural values also played a role in patients’ willingness to undergo amputation, as suggested. Surgeons should not be autocratic in these circumstances and should be aware of beneficence and maleficence when considering the decision of whether to amputate.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: LI L, China; Wu QN, China S-Editor: Li L L-Editor: A P-Editor: Zhao S
| 1. | Smith LL, Burnet SP, McNeil JD. Musculoskeletal manifestations of diabetes mellitus. Br J Sports Med. 2003;37:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Agu TC, Ojiaku ME. The indications for major limb amputations: 8 years retrospective study in a private orthopaedic and trauma centre in the south-east Nigeria. J Clin Orthop Trauma. 2016;7:242-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Slauterbeck JR, Britton C, Moneim MS, Clevenger FW. Mangled extremity severity score: an accurate guide to treatment of the severely injured upper extremity. J Orthop Trauma. 1994;8:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 68] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Beckert S, Witte M, Wicke C, Königsrainer A, Coerper S. A new wound-based severity score for diabetic foot ulcers: A prospective analysis of 1,000 patients. Diabetes Care. 2006;29:988-992. [PubMed] [DOI] [Full Text] |
| 5. | Silvestre JS, Lévy BI. Molecular basis of angiopathy in diabetes mellitus. Circ Res. 2006;98:4-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Xu L, Kanasaki K, Kitada M, Koya D. Diabetic angiopathy and angiogenic defects. Fibrogenesis Tissue Repair. 2012;5:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes. 2015;6:961-969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 216] [Cited by in RCA: 246] [Article Influence: 24.6] [Reference Citation Analysis (4)] |
| 8. | Poznyak A, Grechko AV, Poggio P, Myasoedova VA, Alfieri V, Orekhov AN. The Diabetes Mellitus-Atherosclerosis Connection: The Role of Lipid and Glucose Metabolism and Chronic Inflammation. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 636] [Article Influence: 127.2] [Reference Citation Analysis (0)] |
| 9. | Katakami N. Mechanism of Development of Atherosclerosis and Cardiovascular Disease in Diabetes Mellitus. J Atheroscler Thromb. 2018;25:27-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 306] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 10. | Primadhi RA, Herman H. Diabetic foot: Which one comes first, the ulcer or the contracture? World J Orthop. 2021;12:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Kota SK, Kota SK, Meher LK, Sahoo S, Mohapatra S, Modi KD. Surgical revascularization techniques for diabetic foot. J Cardiovasc Dis Res. 2013;4:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Meloni M, Morosetti D, Giurato L, Stefanini M, Loreni G, Doddi M, Panunzi A, Bellia A, Gandini R, Brocco E, Lazaro-Martinez JL, Lauro D, Uccioli L. Foot Revascularization Avoids Major Amputation in Persons with Diabetes and Ischaemic Foot Ulcers. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 13. | Dryden M, Baguneid M, Eckmann C, Corman S, Stephens J, Solem C, Li J, Charbonneau C, Baillon-Plot N, Haider S. Pathophysiology and burden of infection in patients with diabetes mellitus and peripheral vascular disease: focus on skin and soft-tissue infections. Clin Microbiol Infect. 2015;21 Suppl 2:S27-S32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 14. | Giurato L, Meloni M, Izzo V, Uccioli L. Osteomyelitis in diabetic foot: A comprehensive overview. World J Diabetes. 2017;8:135-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 104] [Cited by in RCA: 107] [Article Influence: 13.4] [Reference Citation Analysis (2)] |
| 15. | Eleftheriadou I, Tentolouris N, Argiana V, Jude E, Boulton AJ. Methicillin-resistant Staphylococcus aureus in diabetic foot infections. Drugs. 2010;70:1785-1797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Pitocco D, Spanu T, Di Leo M, Vitiello R, Rizzi A, Tartaglione L, Fiori B, Caputo S, Tinelli G, Zaccardi F, Flex A, Galli M, Pontecorvi A, Sanguinetti M. Diabetic foot infections: a comprehensive overview. Eur Rev Med Pharmacol Sci. 2019;23:26-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 39] [Reference Citation Analysis (0)] |
| 17. | Aragón-Sánchez FJ, Cabrera-Galván JJ, Quintana-Marrero Y, Hernández-Herrero MJ, Lázaro-Martínez JL, García-Morales E, Beneit-Montesinos JV, Armstrong DG. Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. Diabetologia. 2008;51:1962-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 155] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 18. | Andrews KL, Houdek MT, Kiemele LJ. Wound management of chronic diabetic foot ulcers: from the basics to regenerative medicine. Prosthet Orthot Int. 2015;39:29-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Yunus YM, Rajbhandari SM. Insensate foot of diabetic foot ulcer can have underlying silent neuropathic pain. Int Wound J. 2011;8:301-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Deng W, Dong X, Zhang Y, Jiang Y, Lu D, Wu Q, Liang Z, Yang G, Chen B. Transcutaneous oxygen pressure (TcPO₂): a novel diagnostic tool for peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract. 2014;105:336-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Schreiber AK, Nones CF, Reis RC, Chichorro JG, Cunha JM. Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes. 2015;6:432-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 241] [Cited by in RCA: 286] [Article Influence: 28.6] [Reference Citation Analysis (9)] |
| 22. | Primadhi RA. Susceptibility Factors for Early Reamputation in Diabetic Great Toe Gangrene. Curr Diabetes Rev. 2021;17:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Long CA, Mulder H, Fowkes FGR, Baumgartner I, Berger JS, Katona BG, Mahaffey KW, Norgren L, Blomster JI, Rockhold FW, Hiatt WR, Patel MR, Jones WS, Nehler MR. Incidence and Factors Associated With Major Amputation in Patients With Peripheral Artery Disease: Insights From the EUCLID Trial. Circ Cardiovasc Qual Outcomes. 2020;13:e006399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Yang C, Weng H, Chen L, Yang H, Luo G, Mai L, Jin G, Yan L. Transcutaneous oxygen pressure measurement in diabetic foot ulcers: mean values and cut-point for wound healing. J Wound Ostomy Continence Nurs. 2013;40:585-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Gülcü A, Etli M, Karahan O, Aslan A. Analysis of routine blood markers for predicting amputation/re-amputation risk in diabetic foot. Int Wound J. 2020;17:1996-2004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Bhuvaneswar CG, Epstein LA, Stern TA. Reactions to amputation: recognition and treatment. Prim Care Companion J Clin Psychiatry. 2007;9:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Kragh Nielsen M, Bergenholtz H, Madsen UR. Thoughts and experiences on leg amputation among patients with diabetic foot ulcers. Int J Qual Stud Health Well-being. 2022;17:2009202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Göktepe AS, Cakir B, Yilmaz B, Yazicioglu K. Energy expenditure of walking with prostheses: comparison of three amputation levels. Prosthet Orthot Int. 2010;34:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 29. | Atturu G, Homer-Vanniasinkam S, Russell DA. Pharmacology in peripheral arterial disease: what the interventional radiologist needs to know. Semin Intervent Radiol. 2014;31:330-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Roux-Marson C, Baranski JB, Fafin C, Exterman G, Vigneau C, Couchoud C, Moranne O, Investigators PSPA. Medication burden and inappropriate prescription risk among elderly with advanced chronic kidney disease. BMC Geriatr. 2020;20:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 31. | Hinchliffe RJ, Brownrigg JR, Andros G, Apelqvist J, Boyko EJ, Fitridge R, Mills JL, Reekers J, Shearman CP, Zierler RE, Schaper NC; International Working Group on the Diabetic Foot. Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev. 2016;32 Suppl 1:136-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 32. | Graziani L, Silvestro A, Bertone V, Manara E, Andreini R, Sigala A, Mingardi R, De Giglio R. Vascular involvement in diabetic subjects with ischemic foot ulcer: a new morphologic categorization of disease severity. Eur J Vasc Endovasc Surg. 2007;33:453-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 228] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 33. | Ge BH, Copelan A, Scola D, Watts MM. Iatrogenic percutaneous vascular injuries: clinical presentation, imaging, and management. Semin Intervent Radiol. 2015;32:108-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 34. | Nuutila K, Eriksson E. Moist Wound Healing with Commonly Available Dressings. Adv Wound Care (New Rochelle). 2021;10:685-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 221] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 35. | Zhang Z, Zhang W, Xu Y, Liu D. Efficacy of hyperbaric oxygen therapy for diabetic foot ulcers: An updated systematic review and meta-analysis. Asian J Surg. 2022;45:68-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 36. | Sharma R, Sharma SK, Mudgal SK, Jelly P, Thakur K. Efficacy of hyperbaric oxygen therapy for diabetic foot ulcer, a systematic review and meta-analysis of controlled clinical trials. Sci Rep. 2021;11:2189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 37. | Pu D, Lei X, Leng W, Zheng Y, Chen L, Liang Z, Chen B, Wu Q. Lower limb arterial intervention or autologous platelet-rich gel treatment of diabetic lower extremity arterial disease patients with foot ulcers. Ann Transl Med. 2019;7:485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 38. | Suh HP, Park CJ, Hong JP. Special Considerations for Diabetic Foot Reconstruction. J Reconstr Microsurg. 2021;37:12-16. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 39. | Sothornwit J, Srisawasdi G, Suwannakin A, Sriwijitkamol A. Decreased health-related quality of life in patients with diabetic foot problems. Diabetes Metab Syndr Obes. 2018;11:35-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 40. | Gil J, Schiff AP, Pinzur MS. Cost comparison: limb salvage versus amputation in diabetic patients with charcot foot. Foot Ankle Int. 2013;34:1097-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |