Published online Oct 18, 2023. doi: 10.5312/wjo.v14.i10.776
Peer-review started: August 1, 2023
First decision: September 4, 2023
Revised: September 5, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: October 18, 2023
Processing time: 75 Days and 13.8 Hours
Clavicle fractures can rarely be associated with brachial plexus injury. These are commonly caused by tractional injury at the time of trauma, but unfrequently can be caused by compression of the brachial plexus from excessive callus or granu
We report a rare case of an adult male who sustained a mid-shaft clavicle fracture and had a late presentation of brachial plexus palsy due to compression from excessive callus formation.
We reported a case of a rare occurrence of delayed brachial plexus palsy due to compression from excessive callus formation in a midshaft clavicle fracture. Early diagnosis and surgical decompression of the brachial plexus is critical, as when managed efficiently, a full recovery of the brachial plexus palsy can be expected in these patients.
Core Tip: Brachial plexus palsy due to compression from excessive callus formation in a midshaft clavicle fracture is a rare occurrence. We reported a case of a of delayed brachial plexus palsy due to compression from excessive callus formation in a midshaft clavicle fracture. Early diagnosis and surgical decompression of the brachial plexus is critical for improved patient outcomes.
- Citation: Alzahrani MM. Late brachial plexopathy after a mid-shaft clavicle fracture: A case report. World J Orthop 2023; 14(10): 776-783
- URL: https://www.wjgnet.com/2218-5836/full/v14/i10/776.htm
- DOI: https://dx.doi.org/10.5312/wjo.v14.i10.776
Clavicle fractures are a common injury in the adult population, accounting for 2%-3% of all fractures[1-3]. While these injuries are common, an associated brachial plexus injury is considered rare with an incidence of less than 1%, while this incidence can reach 2% in displaced fractures[4,5]. These brachial plexus injuries commonly occur due to tractional injury at the time of trauma. A rare cause of brachial plexus lesion is compression due to excessive callus or granulation tissue formation and these patients typically have a late presentation[6,7].
A 58-year-old male was involved in a frontal impact motor vehicle accident as a restrained driver. Patient had no history of loss of consciousness and was brought by ambulance to the emergency department. Primary survey was found to be normal, while on secondary survey patient was found to have tenderness over the right clavicle with obvious deformity. In addition, patient had limited right shoulder range of motion in all planes due to severe pain. Plain radiographs diagnosed multiple right sided rib fractures (which were managed conservatively) and a right mid-shaft comminuted clavicle fracture. Neurological and vascular exam was found to be normal at the time of the initial assessment and there was no sign of skin tenting or skin breakage over the clavicle fracture.
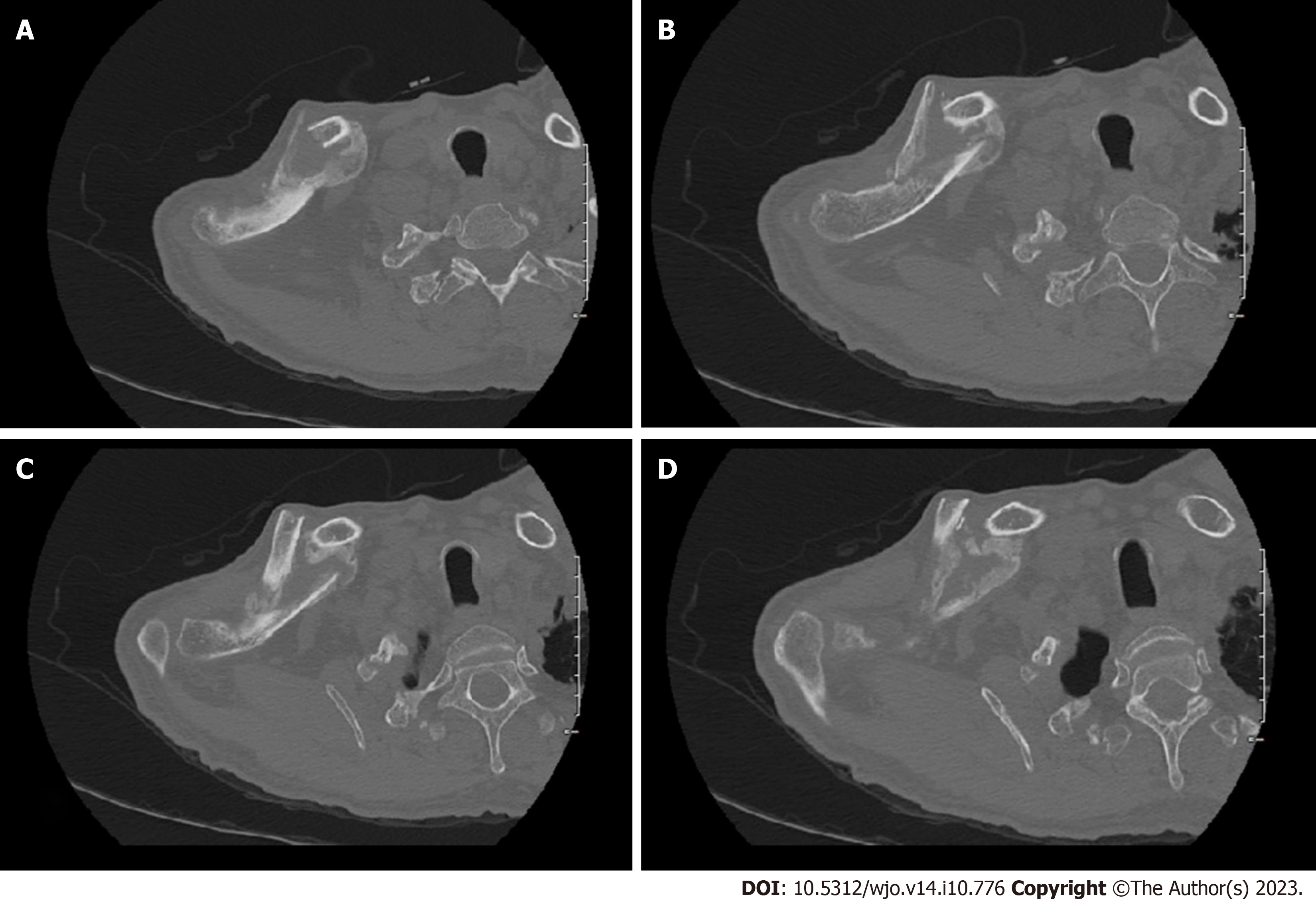
Patient was immobilized in a sling and discharged with a follow up in the orthopaedic clinic in 2 wk. At the time of the follow up 2 wk post-injury, plain radiographs were performed again and re-documented a displaced mid-shaft comminuted clavicle fracture (Figure 1A). Patient again was found to have tenderness over a deformed right clavicle with pain and limited right shoulder range of motion. The neurological and vascular exam of the right upper extremity was still found to be normal. Patient was offered open reduction and internal fixation of the clavicle fracture, but patient declined surgery and opted for conservative management and was given follow up in 4 wk.
At the time of the 4 wk follow up, patients’ tenderness over the right clavicle improved and follow up imaging showed progression of callus formation at the fracture site (Figure 1B). Interestingly, patient was complaining to intermittent right upper extremity mild to moderate shooting pain but was found to have a normal motor and sensory exam of the extremity.
There was no significant past medical illness.
There was no significant personal and family history.
At the following office visit at 3 mo post-injury, the patient’s shoulder and clavicle pain resolved, but patient was complaining of significant right upper extremity weakness, with inability to hold a cup in his hand and decreased grip strength. On further history, patient also gave history of loss of sensation in the hand and forearm region (C7, C8 and T1 distribution). On physical exam there was resolution of the localized right clavicle tenderness with a large bony deformity in the region. Motor power showed weakness in right upper extremity muscle power globally, but more pronounced in finger flexion, adduction and abduction, in addition to weakness in thumb flexion and adduction. On sensory exam, there was loss of sensation over the ulnar aspect of the hand and medial forearm. Distal pulses were present, including radial and ulnar pulses at the wrist.
There were no significant laboratory examinations.
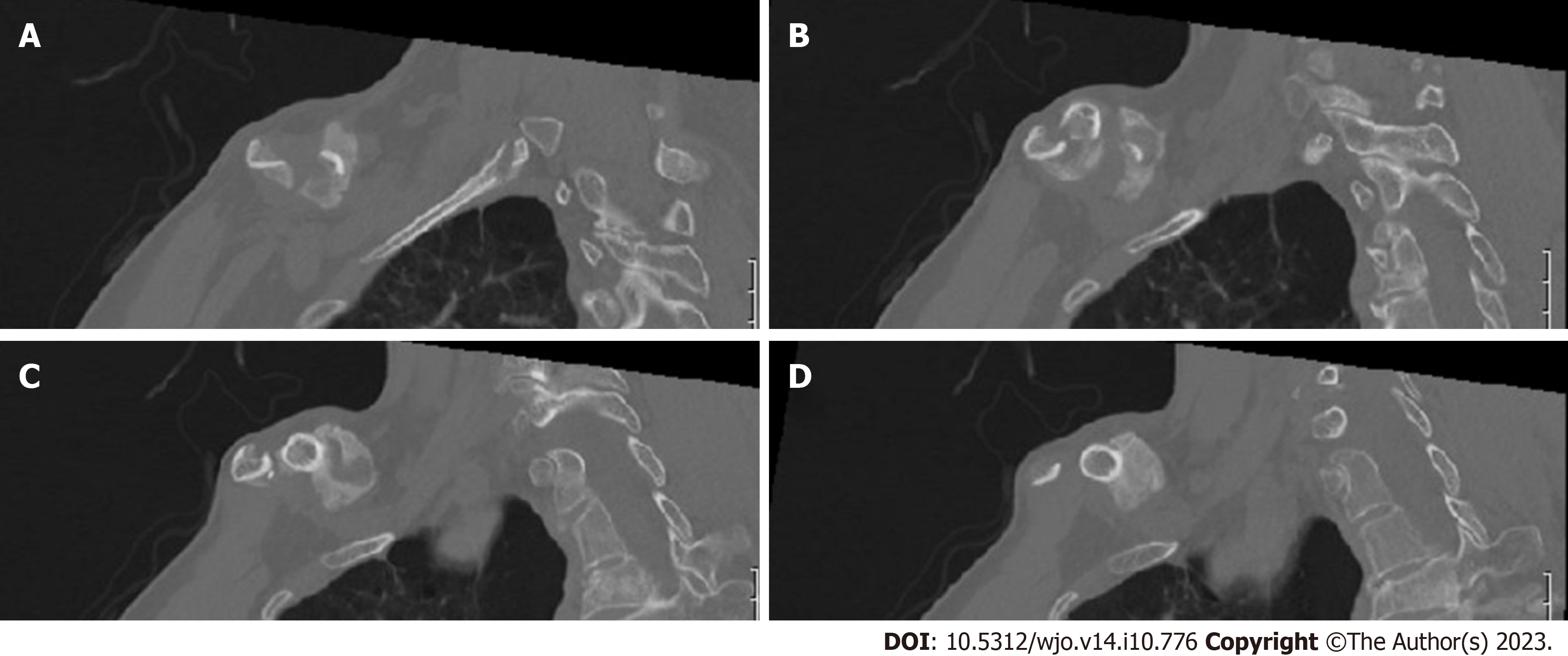
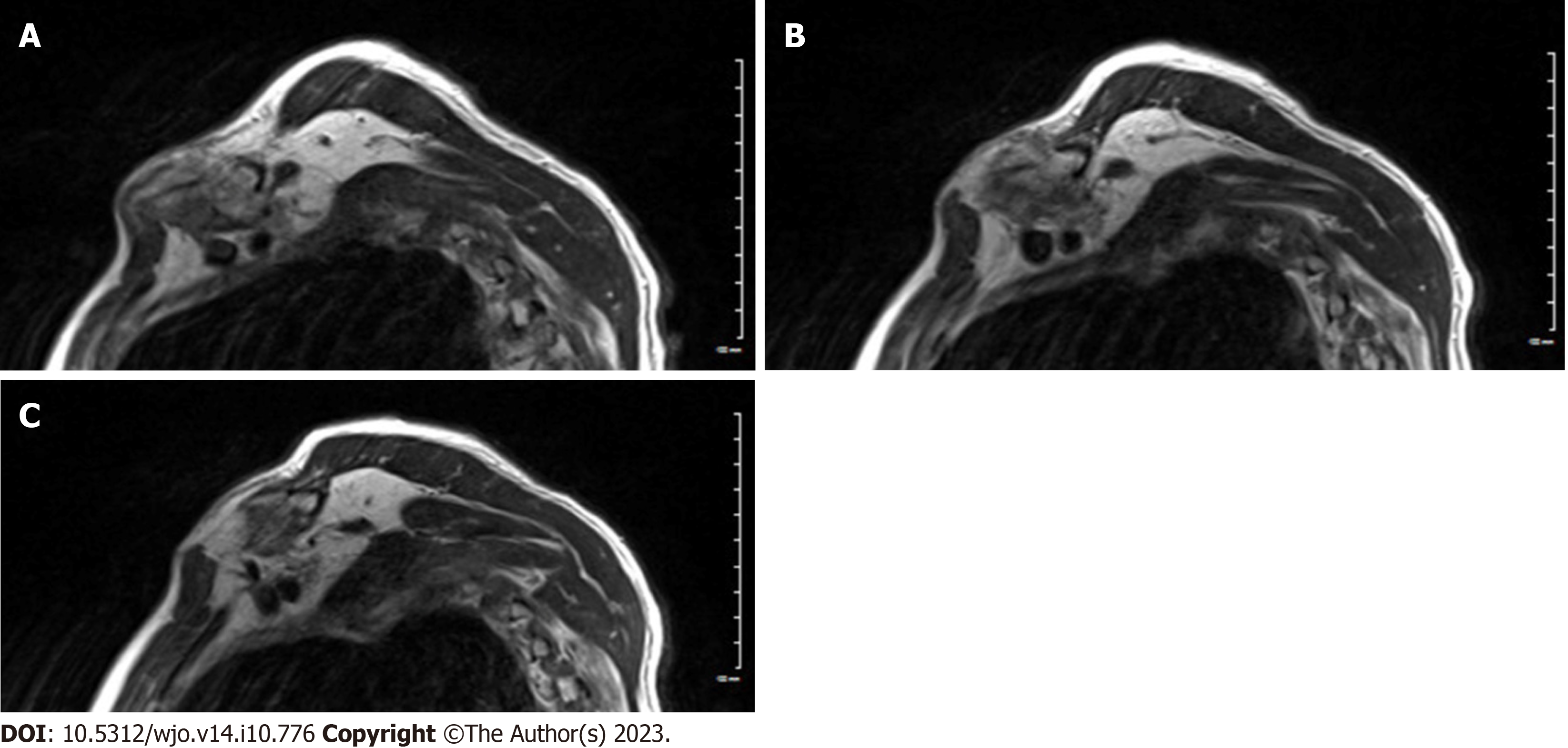
Plain radiograph of the clavicle showed large formation of callus at the fracture site (Figure 1C). A computed tomography (CT) scan was performed which confirmed the midshaft comminuted fracture with hypertrophic callus formation around the fracture site (Figures 2 and 3). Due to the patient’s neurological deficit, a magnetic resonance imaging (MRI) of the region was performed and showed that the hypertrophic callus formation was causing compression of the brachial plexus trunks in the infraclavicular region (Figure 4).
A nerve conduction study was arranged for the patient. But as the patient was exhibiting significant neurological deficits due to brachial plexus compression from the hypertrophic callus formation, an urgent surgical decompression and clavicle open reduction internal fixation was planned.
Right mid-shaft clavicle fracture with hypertrophic callus formation causing compression of the brachial plexus trunks in the infraclavicular region.
The surgery was performed under general anesthesia. After 2 g of intravenous cefazolin was administered, the patient was positioned in the supine position and the right upper extremity was sterilely prepped and draped up to the mid-sternal region. A direct surgical incision over the right clavicle was performed extending from the sternoclavicular joint medial to the distal clavicle laterally. The incision was performed through skin and subcutaneous tissue and hemostasis was obtained. Due to the mass effect of the callus formation over the fracture site, only a thin layer of muscle and fascia was identified and was sharply dissected through. Normal clavicle bone both medial and laterally to the fracture site was exposed to allow application of the internal fixation.
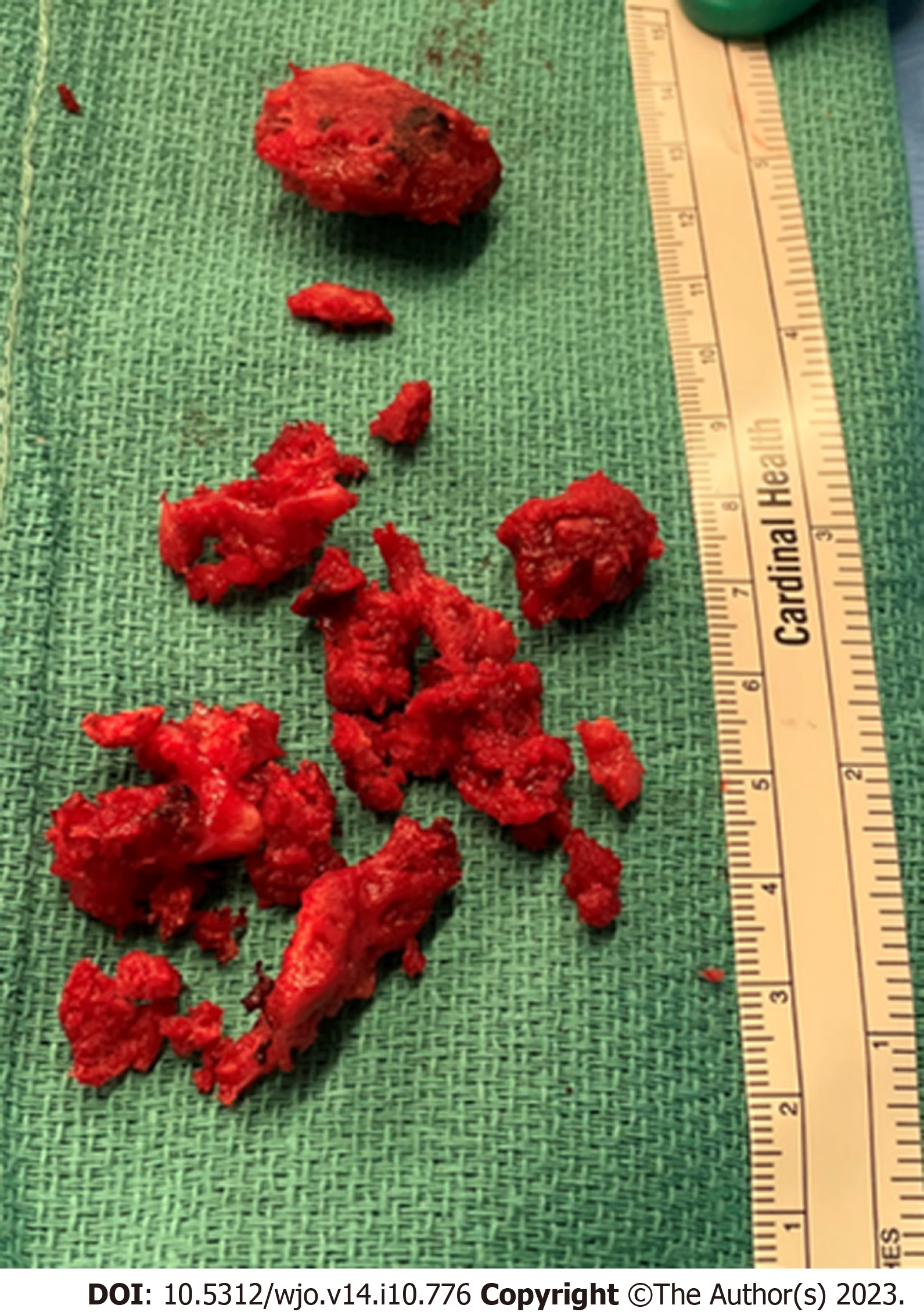
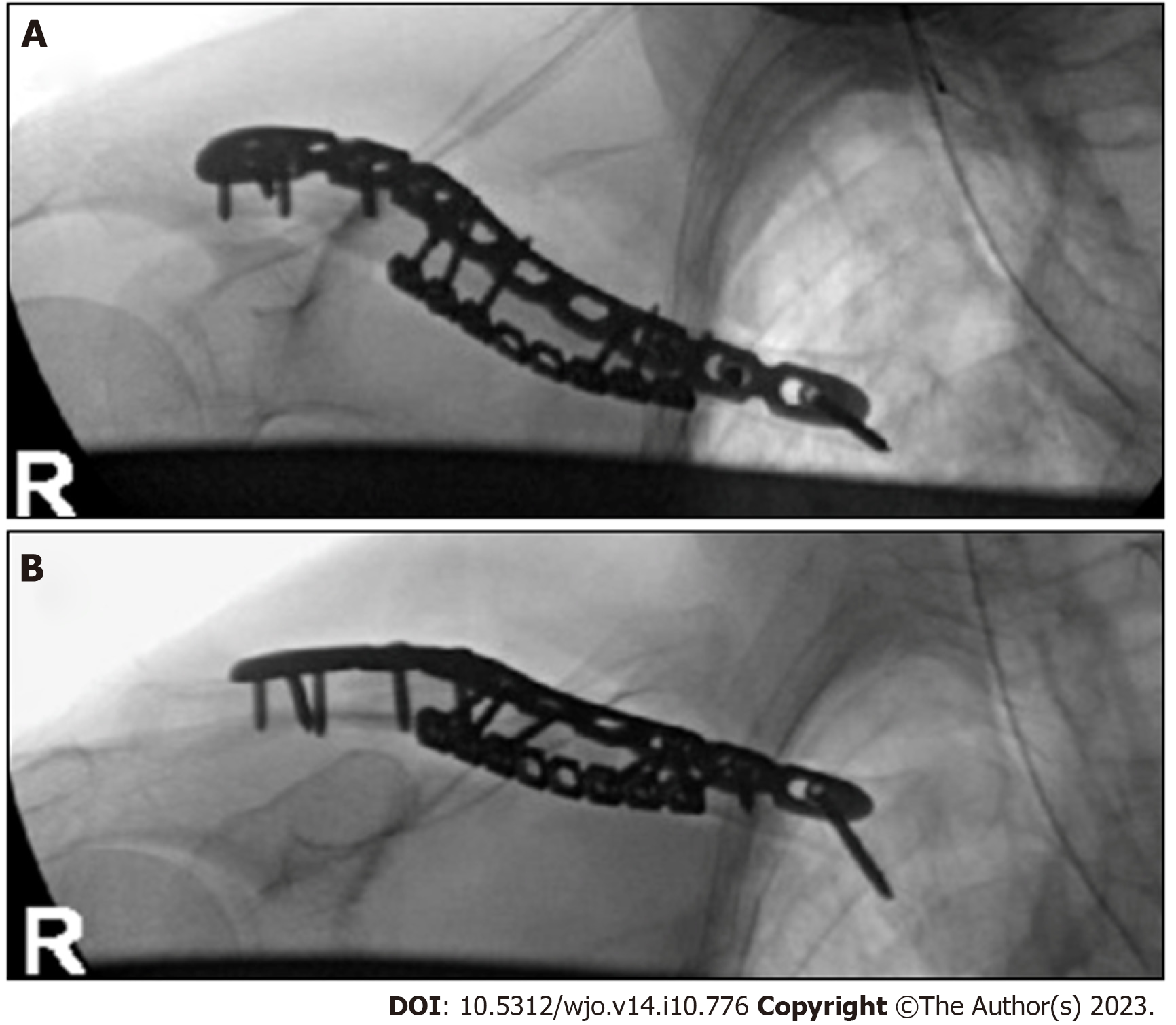
Once adequate exposure was obtained, the area of the bridging callus was carefully osteotomized using small osteotomes and a small handheld burr. The callus was then excised using the burr and small rongeur until the native fracture site was identified. After complete removal and decompression of the hypertrophic callus (Figure 5), we identified the medial and lateral end of the fracture with a small butterfly piece. We confirmed that the infra-clavicular region was decompressed, and no remanent callus or granulation tissue was still present.
The comminuted fracture was then reduced and held provisionally with pointed reduction clamps and then provisionally fixed with an anterior contoured 2.7 mm reconstruction plate and then a superior pre-contoured 3.5 mm clavicular plate was applied. Intra-operative fluoroscopic images were obtained confirming adequate fracture reduction and implant positioning (Figure 6). The wound was then copiously irrigated with normal saline. The wound was closed in layers and a sterile dressing was applied.
Patient was allowed gentle shoulder range of motion but instructed to avoid any weight bearing through the right upper extremity for the first six weeks post-operatively. In the early post-operative phase, patient noted significant improvement in his symptoms and formal physical therapy was initiated at 6 wk post-operatively.
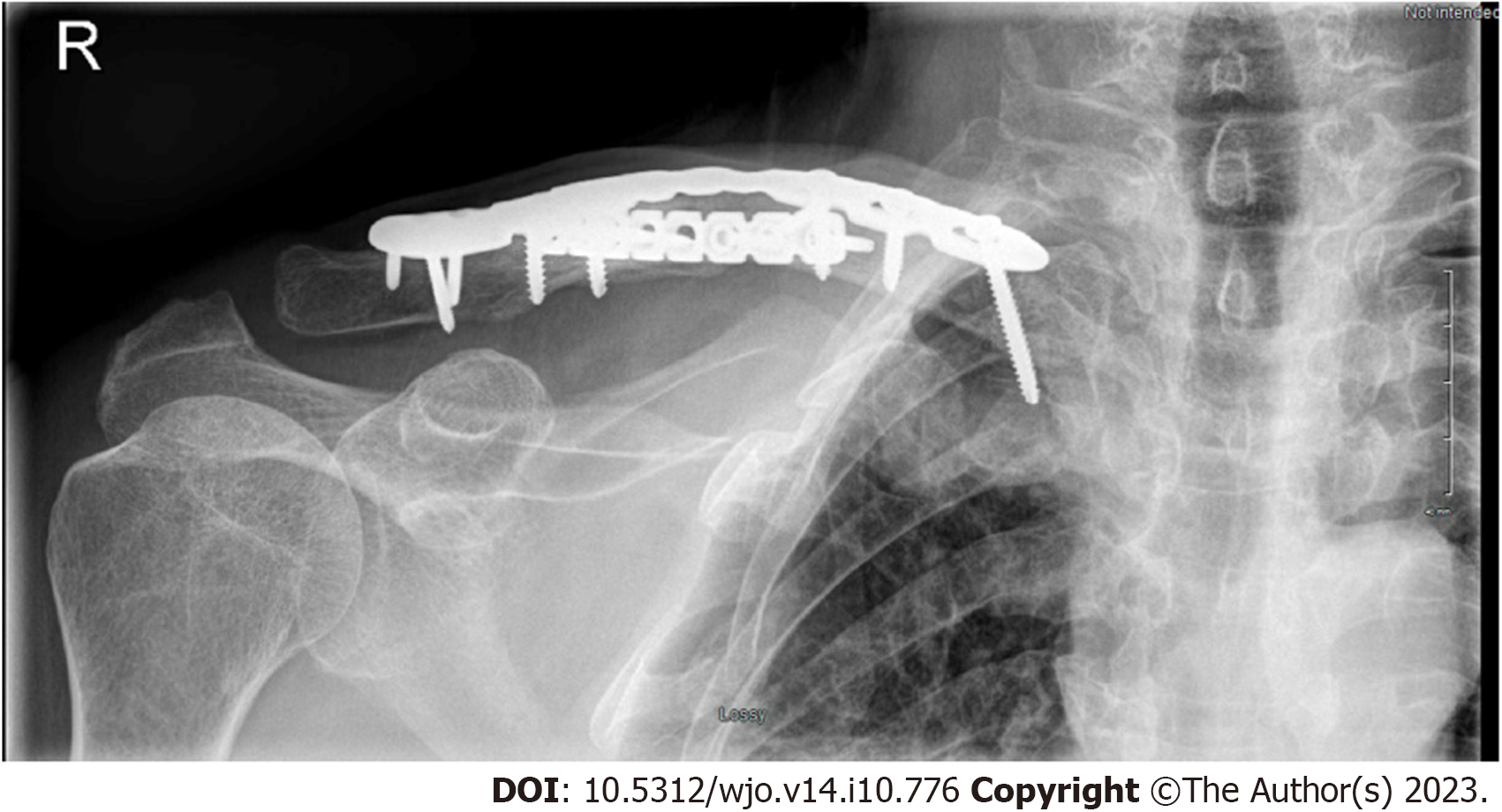
At both 3 and 6 mo follow ups the patient noted improved motor function of the hand and gradual resolution of his sensory deficits. He also indicated improvement of the radiculopathic pain in the right upper extremity. Plain radiographs of the right clavicle showed progression of the fracture healing and maintained implant fixation (Figure 7).
Brachial plexus injuries are rarely caused by clavicle fractures with the majority of cases being caused by tractional injury at the time of trauma, which commonly affect the supraclavicular region of the brachial plexus. Della Santa et al[7] reported an incidence of only 1% of clavicle fractures associated with brachial plexus palsy during a 20-year period.
In our case report, the patient had a delayed palsy of the brachial plexus due to compression from the excessive callus formation. This entity is considered extremely rare, with only some case reports and case series reported in the literature[6-9]. The resultant compression can be due to excessive callus or granulation tissue formation, hypertrophic nonunion or vascular pseudo-aneurysm[10-12]. Commonly this compression affects the infra- or retroclavicular region of the brachial plexus, and these patients have a delayed presentation with late onset neurological deficits in the ipsilateral upper extremity[8,11,13].
A high index of suspicion and careful physical exam are required to avoid misdiagnosis and delay in management. Documentation of motor and sensory exam both at the time of injury and in subsequent visits is critical to identify any evidence of brachial plexus palsy in the early phase. In addition, adequate plain radiographs and CT scan can identify any excessive callus formation or hypertrophic nonunion as the cause of compression. A CT angiogram can be indicated to rule out a subclavian pseudoaneurysm as the cause of compression[12]. Documentation of brachial plexus compression can be identified with an MRI of the clavicular and brachial plexus region, which can also identify other causes of compression (i.e., excessive granulation tissue). Nerve conduction studies and electromyography can also help identify level of compression and involved brachial plexus region.
Management of these injuries involves decompression of the brachial plexus and open reduction internal fixation of the associated clavicle fracture. Typically, these injuries have good prognosis when compared to injuries due to tractional injuries[7,8,13]. The majority of patients can be expected to have a complete neurological recovery once the brachial plexus is decompressed, and fracture adequately stabilized[4,9,14].
We reported a case of a rare occurrence of delayed brachial plexus palsy due to compression from excessive callus formation in a midshaft clavicle fracture. Early diagnosis and surgical decompression of the brachial plexus is critical, as when managed efficiently, a full recovery of the brachial plexus palsy can be expected in these patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mesregah MK, Egypt; Primadhi RA, Indonesia S-Editor: Wang JJ L-Editor: A P-Editor: Zhang YL
| 1. | Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452-456. [PubMed] [DOI] [Full Text] |
| 2. | Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. 2017;18:82. [PubMed] [DOI] [Full Text] |
| 3. | Alzahrani MM, Cota A, Alkhelaifi K, Aleidan A, Berry G, Reindl R, Harvey E. Are clinical outcomes affected by type of plate used for management of mid-shaft clavicle fractures? J Orthop Traumatol. 2018;19:8. [PubMed] [DOI] [Full Text] |
| 4. | Saito T, Matusmura T, Takeshita K. Brachial plexus palsy after clavicle fracture: 3 cases. J Shoulder Elbow Surg. 2020;29:e60-e65. [PubMed] [DOI] [Full Text] |
| 5. | Kim MS. Conservative treatment for brachial plexus injury after a displaced clavicle fracture: a case report and literature review. BMC Musculoskelet Disord. 2022;23:632. [PubMed] [DOI] [Full Text] |
| 6. | Chen CE, Liu HC. Delayed brachial plexus neurapraxia complicating malunion of the clavicle. Am J Orthop (Belle Mead NJ). 2000;29:321-322. [PubMed] |
| 7. | Della Santa D, Narakas A, Bonnard C. Late lesions of the brachial plexus after fracture of the clavicle. Ann Chir Main Memb Super. 1991;10:531-540. [PubMed] [DOI] [Full Text] |
| 8. | Kay SP, Eckardt JJ. Brachial plexus palsy secondary to clavicular nonunion. Case report and literature survey. Clin Orthop Relat Res. 1986;219-222. [PubMed] |
| 9. | Rumball KM, Da Silva VF, Preston DN, Carruthers CC. Brachial-plexus injury after clavicular fracture: case report and literature review. Canadian J Surg. 1991;34:264-266. |
| 10. | Thavarajah D, Scadden J. Iatrogenic postoperative brachial plexus compression secondary to hypertrophic non-union of a clavicle fracture. Ann R Coll Surg Engl. 2013;95:e55-e57. [PubMed] [DOI] [Full Text] |
| 11. | Gadinsky NE, Smolev ET, Ricci MJ, Mintz DN, Wellman DS. Two cases of brachial plexus compression secondary to displaced clavicle fractures. Trauma Case Rep. 2019;23:100219. [PubMed] [DOI] [Full Text] |
| 12. | Hansky B, Murray E, Minami K, Körfer R. Delayed brachial plexus paralysis due to subclavian pseudoaneurysm after clavicular fracture. Eur J Cardiothorac Surg. 1993;7:497-498. [PubMed] [DOI] [Full Text] |
| 13. | Barbier O, Malghem J, Delaere O, Vande Berg B, Rombouts JJ. Injury to the brachial plexus by a fragment of bone after fracture of the clavicle. J Bone Joint Surg Br. 1997;79:534-536. [PubMed] [DOI] [Full Text] |
| 14. | McGillivray MK, Doherty C, Bristol SG, Lawlor DK, Baxter KA, Lefaivre KA. Surgical Management of Delayed Brachial Plexopathy After Clavicle Nonunion. J Orthop Trauma. 2022;36:e399-e404. [PubMed] [DOI] [Full Text] |