Published online Sep 18, 2022. doi: 10.5312/wjo.v13.i9.802
Peer-review started: February 27, 2022
First decision: May 31, 2022
Revised: June 15, 2022
Accepted: August 7, 2022
Article in press: August 7, 2022
Published online: September 18, 2022
Processing time: 200 Days and 22.7 Hours
Distal radius fractures (DRFs) are a common challenge in orthopaedic trauma care, yet for those fractures that are treated nonoperatively, strong evidence to guide cast treatment is still lacking.
To compare the efficacy of below elbow cast (BEC) and above elbow cast (AEC) in maintaining reduction of manipulated DRFs.
We conducted a prospective, monocentric, randomized, parallel-group, open label, blinded, noninferiority trial comparing the efficacy of BEC and AEC in the nonoperative treatment of DRFs. Two hundred and eighty patients > 18 years of age diagnosed with DRFs were successfully randomized and included for analysis over a 3-year period. Noninferiority thresholds were defined as a 2 mm difference for radial length (RL), a 3° difference for radial inclination (RI), and volar tilt (VT). The trial is registered at Clinicaltrials.gov (NCT03468023).
One hundred and forty-three patients were treated with BEC, and 137 were treated with AEC. The mean time of immobilization was 33 d. The mean loss of RL, RI, and VT was 1.59 mm, 2.83°, and 4.11° for BEC and 1.63 mm, 2.54°, and 3.52° for AEC, respectively. The end treatment differences between BEC and AEC in RL, RI, and VT loss were respectively 0.04 mm (95%CI: -0.36-0.44), -0.29° (95%CI: -1.03-0.45), and 0.59° (95%CI: -1.39-2.57), and they were all below the prefixed noninferiority thresholds. The rate of loss of reduction was similar.
BEC performs as well as AEC in maintaining the reduction of a manipulated DRF. Being more comfortable to patients, BEC may be preferable for nonoperative treatment of DRFs.
Core Tip: Currently, there is no general agreement on how best to immobilize a distal radius fracture (DRF) although classic teaching was that immobilization of the elbow would ensure better control of fracture instability. This has been recently challenged by a number of new randomized controlled trials (RCTs) but no one was designed as a non-inferiority RCT, which is the most appropriate way to evaluate the hypothesis that blocking the elbow is unnecessary. We devised a large population noninferiority RCT to give statistical evidence that short arm cast is as effective as long arm cast to treat DRFs using predetermined noninferiority thresholds.
- Citation: Dib G, Maluta T, Cengarle M, Bernasconi A, Marconato G, Corain M, Magnan B. Short arm cast is as effective as long arm cast in maintaining distal radius fracture reduction: Results of the SLA-VER noninferiority trial. World J Orthop 2022; 13(9): 802-811
- URL: https://www.wjgnet.com/2218-5836/full/v13/i9/802.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i9.802
Distal radius fractures (DRFs) are a common clinical challenge in orthopaedic trauma care. Tra
In this paper, the terms short arm cast and BEC or long arm cast and AEC are used interchangeably.
The SLA-VER trial is a prospective, monocentric, randomized, parallel-group, open label, blinded, noninferiority trial (PROBE design), comparing the efficacy of BEC and AEC in maintaining reduction of manipulated DRFs. This study was approved by the local institutional review board (CE\1165CESC), conducted in accordance with the Declaration of Helsinki, and registered on ClinicalTrials.org (NCT03468023). All patients enrolled gave written informed consent.
The primary outcome was fracture reduction maintenance, measured as variation in radial length (RL), radial inclination (RI), and volar tilt (VT). The secondary outcomes included disability of arm, shoulder and hand (DASH) scores and short form 12 (SF-12) scores as measures of cast tolerability.
All patients admitted to the emergency room with a diagnosis of DRF were enrolled according to the following inclusion criteria: Age ≥ 18 years; candidates for nonoperative treatment; displaced fracture requiring manipulation. The exclusion criteria were: Skeletally immature patients (less than 18); undisplaced fracture; fracture requiring surgical treatment; open fracture; hand/wrist/forehand skin lesion on fractured limb; vascular or neurological deficit; bilateral fracture; association with homolateral upper limb fracture. Patients with any medical comorbidity were included, but pregnant patients or patients requiring urgent or life-saving procedures were excluded. Patients were excluded from the study (i.e. dropouts) if reduction could not be achieved after two attempts (after which surgical treatment was offered), the cast was damaged or removed during treatment, or consent was withdrawn[13].
Randomization was carried out by a statistician with no involvement in the clinical care of patients. Software random allocation in blocks of 4 resulted in 353 sequentially numbered opaque sealed envelopes. When a patient was eligible for enrollment, an envelope was opened to assign the participant to a treatment group. Closed manipulation was performed under hematoma block, and the forearm was immobilized in an opposite-to-dislocation position. The arm cast was a radial gutter made of plaster of Paris (POP) that was left open on the volar side to allow for swelling and then circumferentially closed 5-7 d later by applying an extra layer of POP (Figure 1). BEC patients were treated with a BEC extending from the metacarpal heads to 2-4 cm from the elbow crease. AEC patients were treated with an AEC extending from the metacarpal heads to the middle third of the arm. Posteroanterior (PA) and lateral view X-rays were taken pre and post manipulation and at 7 and 35 d. The radial gutter was closed at the first office visit and removed at the final visit. If closed manipulation failed to achieve satisfactory reduction, patients were offered surgical treatment and excluded from the study. If reduction was lost at 7 d, patients were offered surgical treatment. These patients were still considered for analysis as subjects who did not maintain satisfactory reduction at the final follow-up. Radiographic parameters were determined at each X-ray examination. RL was measured on the PA view as the distance between two lines drawn perpendicularly to the radial shaft long axis: one at the tip of the radial styloid and one at the ulnar border of the radius articular surface at the central reference point, which is a point midway between the volar and dorsal ulnar corners to eliminate variation caused by dorsal angulation as described by Slutsky[14]. RI was measured on the PA view by determining the angle between a line passing through the tip of the radial styloid and the medial corner of the articular surface of the radius and a line perpendicular to the shaft of the radius. VT was measured on the lateral view by the angle between the line of the distal articular surface (passing through the two most distal points of the dorsal and volar lips of the radius) and the longitudinal axis of the radius[14,15]. Fracture stability was assessed according to Lafontaine (dorsal angulation > 20°, dorsal comminution, articular involvement, associated ulnar fracture, and age > 60 years): If three or more of these criteria were present, the fracture was defined unstable[16]. The casting technique was assessed by means of cast index and three-point index[17,18]. Reduction was considered to be maintained when the following criteria, described by Graham, were met[13]: Loss of radial length < 5 mm, radial inclination ≥ 15°, and volar tilt between +15° and -20°. Given the variability of the criteria used to assess acceptability of reduction, we decided to further test the dataset against three other sets of criteria (combinations of different thresholds of RL, RI, and VT). All measurements were performed by three investigators, none of whom were involved in patient recruitment and all of whom were blinded to patient group assignment. Patients were stratified by age, sex, presence of osteoporosis (indirectly assessed by osteoporosis-specific drug consumption), fracture type (according to AO classification), and fracture stability (according to Lafontaine’s criteria)[19]. At the final follow-up visit, patients were asked to complete DASH and SF-12 questionnaires and elbow range of movement (ROM) after cast removal was also recorded[20,21]. Protocol details have been published previously[22] and are available at https://clinicaltrials.gov/ct2/show/NCT03468023.
For the study to have 80% power to show a difference between the treatments with a two-sided type 1 error rate of 5%, we calculated that approximately 150 patients would be required for each group using a 2 mm difference in RL and a 3° difference in RI and VT as noninferiority thresholds. These estimates of minimal clinically important differences were based on previous reports of interobserver variability of up to 3° in radiographic parameter measurement and considerable deterioration of clinical outcome when shortening of RL was > 5 mm[15,23,24]. We included 53 additional patients to make up for a predicted 15% dropout rate. Since our aim was to identify the real treatment efficacy under optimal conditions, we conducted a per-protocol analysis. In noninferiority trials, both intention-to-treat and per-protocol analyses are recommended[25]. In this trial, we did not include dropouts in the final analysis, since doing so would have introduced a confounding effect of surgery. We did not use baseline differences to decide whether and which covariates should be used to adjust treatment effect because we assumed that, in RCTs, any baseline difference between the two groups is attributable to chance and thus negligible[26]. The 95%CI was calculated for continuous variables following a normal distribution. Noninferiority t-tests were used to compare radiological parameters, and chi-squared tests were used to compare percentages of loss of reduction between the two groups. DASH and SF-12 scores between the BEC and AEC groups were compared using superiority t-tests. All variables included in the analysis were complete, with no missing data. Analyses were performed using SAS 9.4.
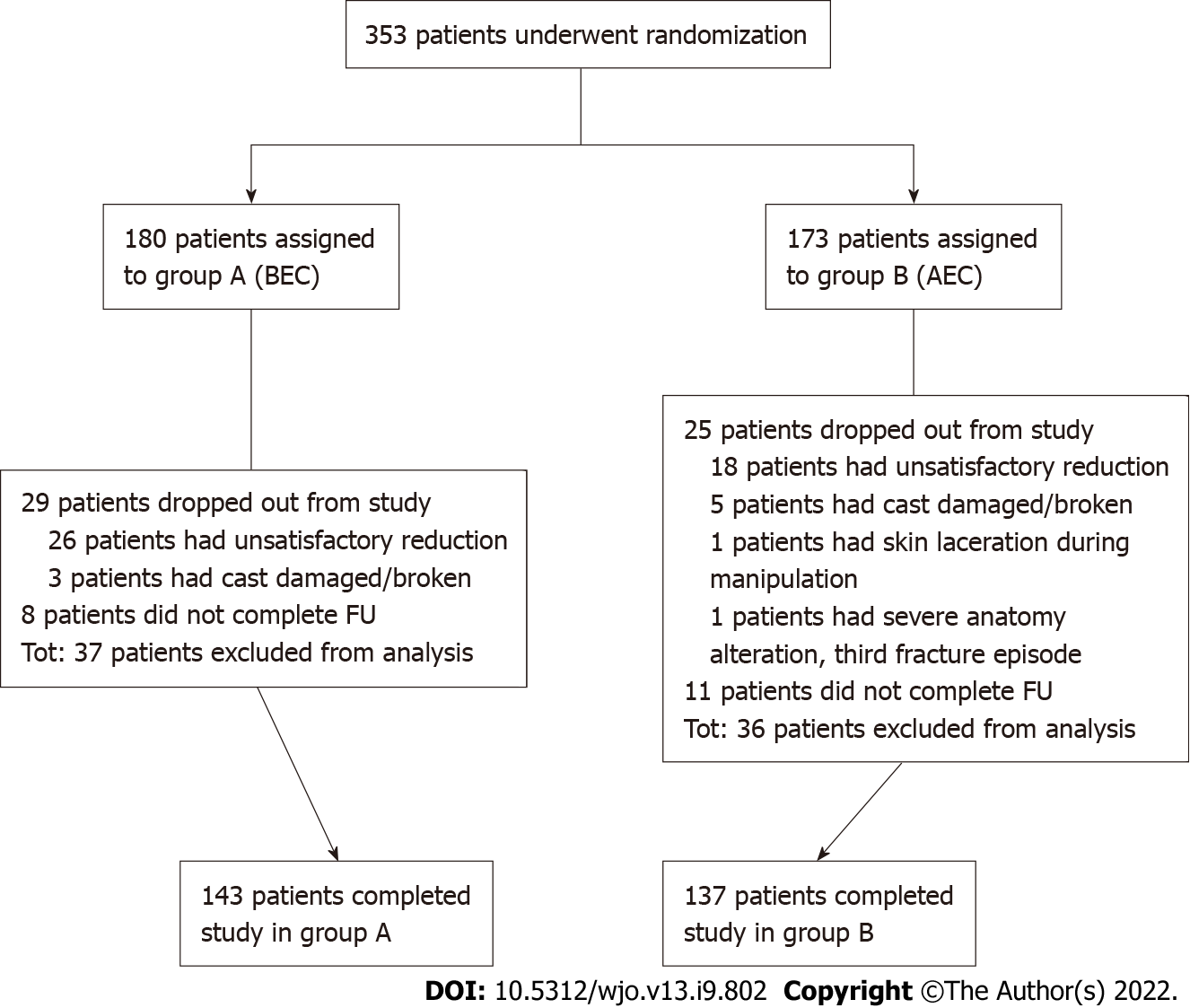
Between March 2017 and February 2020, 353 eligible patients were enrolled in the trial. Of these, 180 patients were randomly assigned to treatment group A (BEC) and 173 were randomly assigned to treatment group B (AEC). In group A, 29 patients dropped out of the study, and 8 did not complete the follow-up. In group B, 25 patients dropped out from the study, and 11 did not complete the follow-up (Figure 2). Dropouts (and dropout reasons) were similar between the groups. A total of 280 patients (143 in group A and 137 in group B) completed the study and were included in the analysis. The study groups were similar with respect to age, sex, osteoporosis, type of fracture (AO classification), and stability of fracture, as shown in Table 1. Cast index and three-point index were homogeneous between the groups (χ2 = 1.72, P = 0.19 and χ2 = 0.06, P = 0.79, respectively). Randomization resulted in two well-balanced study groups. The mean time of immobilization was 33 d (95%CI: 31.88-34.10) for BEC patients and 32.6 d (95%CI: 31.5-33.63) for AEC patients. Nine patients treated with BEC and ten treated with AEC lost reduction at 7 d. Seven were treated surgically, and two continued nonoperative treatment in the BEC group; seven were treated surgically, and three continued nonoperative treatment in the AEC group. Upon removal of cast at the final follow-up, the mean loss of RL was -1.59 mm for BEC vs -1.63 mm for AEC (between-group difference: 0.04 mm; 95%CI: -0.36-0.44); the mean loss of RI was -2.83° in BEC vs -2.54° in AEC (between-group difference: -0.29°; 95%CI: -1.03-0.45); the mean loss of VT was 4.11° in BEC vs 3.52° in AEC (between-group difference: 0.59°; 95%CI: -1.39-2.57). Differences in loss of RL, RI, and VT during treatment between the groups reached statistical significance when tested for noninferiority (P < 0.0001 for RL, P < 0.0001 for RI, and P = 0.0087 for VT), and all differences were below the prefixed thresholds outlined above. Differences between the final and baseline radiographic parameters are reported in Table 2. According to Graham’s criteria, 99 (69%) out of 143 patients treated with BEC maintained satisfactory reduction as opposed to 106 (77%) out of 137 patients treated with AEC. This difference was not significant (P = 0.12; Table 3). Considering that the percentage of fractures labelled as “maintained” varies according to the criteria of acceptability of reduction used, we tested a further three sets of criteria as described above. In all cases, no statistically significant difference was observed (66% maintained in BEC vs 74% in AEC for type 2, 61% maintained in BEC vs 62% in AEC for type 3, and 62% maintained in BEC vs 61% in AEC for type 4; Table 3). DASH score, SF-12 [physical component summary (PCS) and mental component summary (MCS)] scores, and elbow ROM were collected for 122 out of 280 patients: 55 (38%) patients in group A and 67 (49%) patients in group B. DASH score for BEC patients was 59 (95%CI: 53.8-64.2) and 59.9 (95%CI: 55.6-64.3) for AEC patients; the mean PCS and MCS scores were 34.9 (95%CI: 32.9-36.9) and 43.6 (95%CI: 40.5-46.8), respectively, for BEC patients and 36.6 (95%CI: 34.9-38.2) and 41.8 (95%CI: 39.1-44.5) for AEC patients. No difference was observed between patient groups. Subgroup analysis for dominant side fracture did not change the result. Regarding elbow ROM, BEC patients exhibited a mean flexion of 123.6° (95%CI: 117.1-130.1), mean extension of 6.7° (95%CI: 2.5-10.8), mean pronation of 69.5° (95%CI: 63.8-75.3), and mean supination of 52.5° (95%CI: 45.6-59.3). AEC patients had similar ROM, with a mean flexion of 123.9° (95%CI: 118.9-128.9), mean extension of 5.5° (95%CI: 1.4-9.5), mean pronation of 72.1° (95%CI: 66.4-77.9), and mean supination of 52.9° (95%CI: 45.5-60.3). Again, no difference was observed between the groups.
| Characteristic | Group A (below-elbow cast) | Group B (above-elbow cast) | t-test (t) or Chi-squared test (χ2) | P value |
| Age (yr), mean ± SD | 70.2 ± 13.7 | 69.5 ± 15.4 | t = 0.42 | P = 0.68 |
| Sex, n (%) | χ2 = 0.02 | P = 0.89 | ||
| Male | 19 (13) | 19 (14) | ||
| Female | 124 (87) | 118 (86) | ||
| Osteoporosis, n (%) | χ2 = 1.53 | P = 0.46 | ||
| Yes | 44 (31) | 78 (57) | ||
| No | 84 (59) | 38 (28) | ||
| Missing | 15 (10) | 21 (15) | ||
| Type of fracture (AO classification), n (%) | χ2 = 0.20 | P = 0.90 | ||
| Type A | 48 (34) | 43 (31) | ||
| Type B | 17 (12) | 18 (13) | ||
| Type C | 78 (55) | 76 (55) | ||
| Stability of fracture (Lafontaine), n (%) | χ2 = 0.12 | P = 0.73 | ||
| Stable | 68 (48) | 68 (50) | ||
| Unstable | 75 (52) | 69 (50) |
| Parameter | Group A (BEC), mean (95%CI) | Group B (AEC), mean (95%CI) | t-test (t) comparing groups | P value |
| Baseline (post reduction) | ||||
| RL | 11.31 mm (11.03; 11.60) | 11.35 mm (11.05; 11.64) | t = -0.17 | P = 0.86 |
| RI | 20.90° (20.41; 21.39) | 21.08° (20.58; 21.59) | t = -0.50 | P = 0.62 |
| VT | -8.06° (-9.11; -7.01) | -6.55° (-7.56; -5.55) | t = -2.05 | P = 0.04 |
| Final control (35 d) | ||||
| RL | 9.73 mm (9.33; 10.12) | 9.72 mm (9.35; 10.09) | t = 0.02 | P = 0.99 |
| RI | 18.07° (17.42; 18.72) | 18.54° (17.88; 19.19) | t = -1.01 | P = 0.31 |
| VT | -3.95° (-5.61; -2.29) | -3.03° (-4,35; -1,71) | t = -0.86 | P = 0.39 |
| Δ final control–baseline | ||||
| Parameter | ||||
| RL | -1.59 mm (-1.88; -1.29) | -1.63 mm (-1.89; -1.36) | t = 0.2 | P = 0.84 |
| RI | -2.83° (-3.37; -2.29) | -2.54° (-3.05; -2.03) | t = -0.77 | P = 0.44 |
| VT | 4.11° (2.61; 5.61) | 3.53° (2.22; 4.83) | t = 0.58 | P = 0.56 |
| Δ of loss of radiographic parameters during treatment (BEC–AEC) | ||||
| Parameter | Group A-B, mean (95%CI) | |||
| RL | 0.04 mm (-0.36; 0.44) | |||
| RI | -0.29° (-1.03; 0.45) | |||
| VT | 0.59° (-1.39; 2.57) | |||
| Type I (Graham) | Type II (Gliatis) | Type III (Aro and Koivunen) | Type IV (Fernandez) | |
| Radiographic criterion/acceptable measurement | ||||
| RL shortening | < 5 mm | < 5 mm | < 3 mm | < 3 mm |
| RI | ≥ 15° | ≥ 15° | ≥ 15° | ≥ 15° |
| VT | Between 15° and 20° | Between 10° and 20° | Between 15° and 20° | Between 10° and 20° |
| Maintenance, n (%) | ||||
| Group A (BEC) | 99 (69) | 95 (66) | 87 (61) | 89 (62) |
| Group B (AEC) | 106 (77) | 101 (74) | 87 (63) | 83 (61) |
| Chi-squared test (χ2) | χ2 = 2.36 | χ2 = 1.77 | χ2 = 0.21 | χ2 = 0.09 |
| P value | P = 0.12 | P = 0.18 | P = 0.65 | P = 0.75 |
Noninferiority tests are the most appropriate way to evaluate the hypothesis that BEC and AEC have similar efficacy. They are based on minimal clinically important thresholds that are established a priori by drawing on empirical assumptions. When observed between-treatment differences fall below these thresholds, treatments can be considered equivalent. Statistical superiority tests, for example, the percentage of fractures that maintain reduction vs the percentage of fractures that lose reduction, can be misleading since they tell us nothing about equivalence[12]. Therefore, in the current study, we analysed both dichotomic variables (i.e., percentage of reduction maintenance) and continuous variables (i.e., radiographic radial parameters) for which noninferiority thresholds could be predetermined. By employing a noninferiority design, the current study showed that the efficacy of BEC in maintaining the reduction of manipulated DRFs is similar to that of AEC. According to our model, when clinicians have to choose between using BEC or AEC to immobilize a DRF, the maximum predictable outcome difference between the two treatments does not exceed 2 mm in terms of RL loss and 3° in terms of RI and VT loss. Maintenance of reduction of DRFs is more likely to depend on factors other than length of cast used, for example, patient age and stability or type of fracture. SLA-VER has some limitations that warrant discussion. Quality of reduction was not assessed and could have potentially influenced the difference between BEC and AEC. Given that no computerized tomography was carried out, we may not have accurately measured every articular gap, and it is possible that its prevalence might be different between the study groups. However, our approach is consistent with general clinical practice. Furthermore, we limited our investigation to radiological outcomes only and did not include clinical outcome measures. SLA-VER aimed only at ascertaining whether the type of casting used affects the likelihood of fracture maintenance. A large amount of data about factors associated with loss of reduction risk and clinical outcome has already been published[16,27-39]. Only a small number of patients completed the DASH and SF-12 questionnaires and received elbow ROM measurements, even though this was a secondary study endpoint. Our data did not reveal a clear difference in patient comfort between BEC and AEC and this remained true even after subgroup analysis of dominant side fractures. Surprisingly, elbow range of motion was not affected by the type of cast as one would have expected. One explanation could be that the time of immobilization may have been too short to result in significant elbow stiffness or that the absence of elbow injury might have contributed to preserving joint mobility. This finding is also reported by Okamura et al[11]. Finally, it may be that DASH scores are not the most appropriate way to assess cast comfort. Bong et al[7] found better DASH scores in below-elbow splints, although to a lesser degree than expected, suggesting that DASH might not be able to specifically address the comfort level of the two constructs. Furthermore, Caruso et al[10] did not find any difference in DASH scores between BEC and AEC at the 4 wk follow-up but reported a significant difference in favour of BEC using the Mayo elbow score. Similarly, Park et al[8] did not find any difference in DASH score between BEC and AEC, although they found a correlation with the dominant side and a higher incidence of shoulder pain in the latter group. Nevertheless, BEC is broadly considered more comfortable and preferable than AEC[8].
Data from this trial lead us to conclude that BEC performs as well as AEC in maintaining reduction of a manipulated DRF. When clinicians have to choose between BEC and AEC, the maximum predictable difference does not exceed 2 mm in terms of RL loss and 3° in terms of RI and VT loss. We recommend BEC over AEC for its non-inferior performance and better tolerability.
Distal radius fracture (DRF) treatment is a common challenge in orthopaedic trauma care. Uncertainty exists on how best to immobilize a DRF.
The necessity of blocking the elbow when immobilizing a DRF is still a matter of debate.
To test the hypothesis that blocking the elbow is not necessary and that a below arm cast (BEC) performs as well as an above elbow cast (AEC).
A noninferiority randomized clinical trial was conducted on 280 patients diagnosed with a DRF managed nonsurgically. Loss of reduction was evaluated considering variation in radiographic parameters [radial length (RL), radial inclination (RI), and volar tilt (VT)].
Rates of loss of reduction were similar between BEC and AEC. Variation of radiographic parameters (RL, RI, and VT) was similar between BEC and AEC and fell within the predetermined noninferiority thresholds.
BEC performs as well as AEC in maintaining reduction of a manipulated DRF.
Further large population randomized controlled trials and meta-analyses are required to confirm the hypothesis that BEC should become the option of choice for DRF treatment.
The authors would like to sincerely thank Dr. Anna Powell, medical writer, for her expertise in proofreading the manuscript and Dr. Giuseppe Palazzolo, MD, for his help in reviewing patients’ radiological records.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Liu J, United States; Ozden F, Turkey S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Zhang H
| 1. | Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles' fractures. Functional bracing in supination. J Bone Joint Surg Am. 1975;57:311-317. [PubMed] |
| 2. | Sarmiento A. The brachioradialis as a deforming force in Colles' fractures. Clin Orthop Relat Res. 1965;38:86-92. [PubMed] |
| 3. | Bünger C, Sølund K, Rasmussen P. Early results after Colles' fracture: functional bracing in supination vs dorsal plaster immobilization. Arch Orthop Trauma Surg (1978). 1984;103:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Wahlström O. Treatment of Colles' fracture. A prospective comparison of three different positions of immobilization. Acta Orthop Scand. 1982;53:225-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Lichtman DM, Bindra RR, Boyer MI, Putnam MD, Ring D, Slutsky DJ, Taras JS, Watters WC 3rd, Goldberg MJ, Keith M, Turkelson CM, Wies JL, Haralson RH 3rd, Boyer KM, Hitchcock K, Raymond L. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 198] [Article Influence: 13.2] [Reference Citation Analysis (1)] |
| 6. | Sahin M, Taşbaş BA, Dağlar B, Bayrakci K, Savaş MS, Günel U. [The effect of long- or short-arm casting on the stability of reduction and bone mineral density in conservative treatment of Colles' fractures]. Acta Orthop Traumatol Turc. 2005;39:30-34. [PubMed] |
| 7. | Bong MR, Egol KA, Leibman M, Koval KJ. A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg Am. 2006;31:766-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Park MJ, Kim JP, Lee HI, Lim TK, Jung HS, Lee JS. Is a short arm cast appropriate for stable distal radius fractures in patients older than 55 years? J Hand Surg Eur Vol. 2017;42:487-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Gamba C, Fernandez FAM, Llavall MC, Diez XL, Perez FS. Which immobilization is better for distal radius fracture? Int Orthop. 2017;41:1723-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Caruso G, Tonon F, Gildone A, Andreotti M, Altavilla R, Valentini A, Valpiani G, Massari L. Below-elbow or above-elbow cast for conservative treatment of extra-articular distal radius fractures with dorsal displacement: a prospective randomized trial. J Orthop Surg Res. 2019;14:477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Okamura A, de Moraes VY, Neto JR, Tamaoki MJ, Faloppa F, Belloti JC. No benefit for elbow blocking on conservative treatment of distal radius fractures: A 6-month randomized controlled trial. PLoS One. 2021;16:e0252667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Harris AH, Fernandes-Taylor S, Giori N. "Not statistically different" does not necessarily mean "the same": the important but underappreciated distinction between difference and equivalence studies. J Bone Joint Surg Am. 2012;94:e29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Graham TJ. Surgical Correction of Malunited Fractures of the Distal Radius. J Am Acad Orthop Surg. 1997;5:270-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 84] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Slutsky DJ. Principles and practice of wrist surgery. Philadelphia PA: Saunders Elsevier, 2010. |
| 15. | Johnson PG, Szabo RM. Angle measurements of the distal radius: a cadaver study. Skeletal Radiol. 1993;22:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 230] [Article Influence: 6.4] [Reference Citation Analysis (1)] |
| 17. | Chess DG, Hyndman JC, Leahey JL, Brown DC, Sinclair AM. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 92] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Alemdaroğlu KB, Iltar S, Aydoğan NH, Say F, Kilinç CY, Tiftikçi U. Three-point index in predicting redisplacement of extra-articular distal radial fractures in adults. Injury. 2010;41:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Müller ME, Koch P, Nazarian S, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. Berlin, Heidelberg: Springer Berlin Heidelberg, 1990. |
| 20. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 21. | Jenkinson C, Layte R. Development and testing of the UK SF-12 (short form health survey). J Health Serv Res Policy. 1997;2:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 324] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 22. | Maluta T, Cengarle M, Dib G, Bernasconi A, Lavini F, Ricci M, Vecchini E, Samaila EM, Magnan B. SLA-VER: study protocol description and preliminar results of the first italian RCT on conservative treatment of distal radial fractures. Acta Biomed. 2019;90:54-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 23. | DiBenedetto MR, Lubbers LM, Ruff ME, Nappi JF, Coleman CR. Quantification of error in measurement of radial inclination angle and radial-carpal distance. J Hand Surg Am. 1991;16:399-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles' fracture treatment. J Hand Surg Am. 1991;16:392-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 119] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Shah PB. Intention-to-treat and per-protocol analysis. CMAJ. 2011;183:696; author reply 696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 26. | Senn S. Statistical issues in drug development. 2nd ed. Chichester, England, Hoboken, NJ: John Wiley & Sons, 2007. |
| 27. | Jaremko JL, Lambert RG, Rowe BH, Johnson JA, Majumdar SR. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 28. | Bentohami A, Bijlsma TS, Goslings JC, de Reuver P, Kaufmann L, Schep NW. Radiological criteria for acceptable reduction of extra-articular distal radial fractures are not predictive for patient-reported functional outcome. J Hand Surg Eur Vol. 2013;38:524-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Cowie J, Anakwe R, McQueen M. Factors associated with one-year outcome after distal radial fracture treatment. J Orthop Surg (Hong Kong). 2015;23:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Maluta T, Dib G, Cengarle M, Bernasconi A, Samaila E, Magnan B. Below- vs above-elbow cast for distal radius fractures: is elbow immobilization really effective for reduction maintenance? Int Orthop. 2019;43:2391-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Wadsten MÅ, Sayed-Noor AS, Englund E, Buttazzoni GG, Sjödén GO. Cortical comminution in distal radial fractures can predict the radiological outcome: a cohort multicentre study. Bone Joint J. 2014;96-B:978-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Walenkamp MM, Aydin S, Mulders MA, Goslings JC, Schep NW. Predictors of unstable distal radius fractures: a systematic review and meta-analysis. J Hand Surg Eur Vol. 2016;41:501-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of extra-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25:535-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 88] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 35. | Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y. Acceptable parameters for alignment of distal radius fracture with conservative treatment in elderly patients. J Orthop Sci. 2014;19:292-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 37. | Makhni EC, Ewald TJ, Kelly S, Day CS. Effect of patient age on the radiographic outcomes of distal radius fractures subject to nonoperative treatment. J Hand Surg Am. 2008;33:1301-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 38. | Gutiérrez-Monclus R, Gutiérrez-Espinoza H, Zavala-González J, Olguín-Huerta C, Rubio-Oyarzún D, Araya-Quintanilla F. Correlation Between Radiological Parameters and Functional Outcomes in Patients Older Than 60 Years of Age With Distal Radius Fracture. Hand (N Y). 2019;14:770-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 39. | Nesbitt KS, Failla JM, Les C. Assessment of instability factors in adult distal radius fractures. J Hand Surg Am. 2004;29:1128-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |