Published online Sep 18, 2022. doi: 10.5312/wjo.v13.i9.777
Peer-review started: March 11, 2022
First decision: June 8, 2022
Revised: June 16, 2022
Accepted: August 17, 2022
Article in press: August 17, 2022
Published online: September 18, 2022
Processing time: 189 Days and 1.5 Hours
Background: Knee examination guidelines in minors are intended to aid decision-making in the management of knee instability. Clinical question: A Delphi study was conducted with a formal consensus process using a validated methodology with sufficient scientific evidence. A group consensus meeting was held to develop recommendations and practical guidelines for use in the assessment of instability injuries in children. Key findings: there is a lack of evidence to analyse anterior cruciate ligament injuries in children and their subsequent surgical management if necessary. Diagnostic guidelines and clinical assessment of the patient based on a thorough examination of the knee are performed and a guide to anterior cruciate ligament exploration in children is developed. Clinical ap
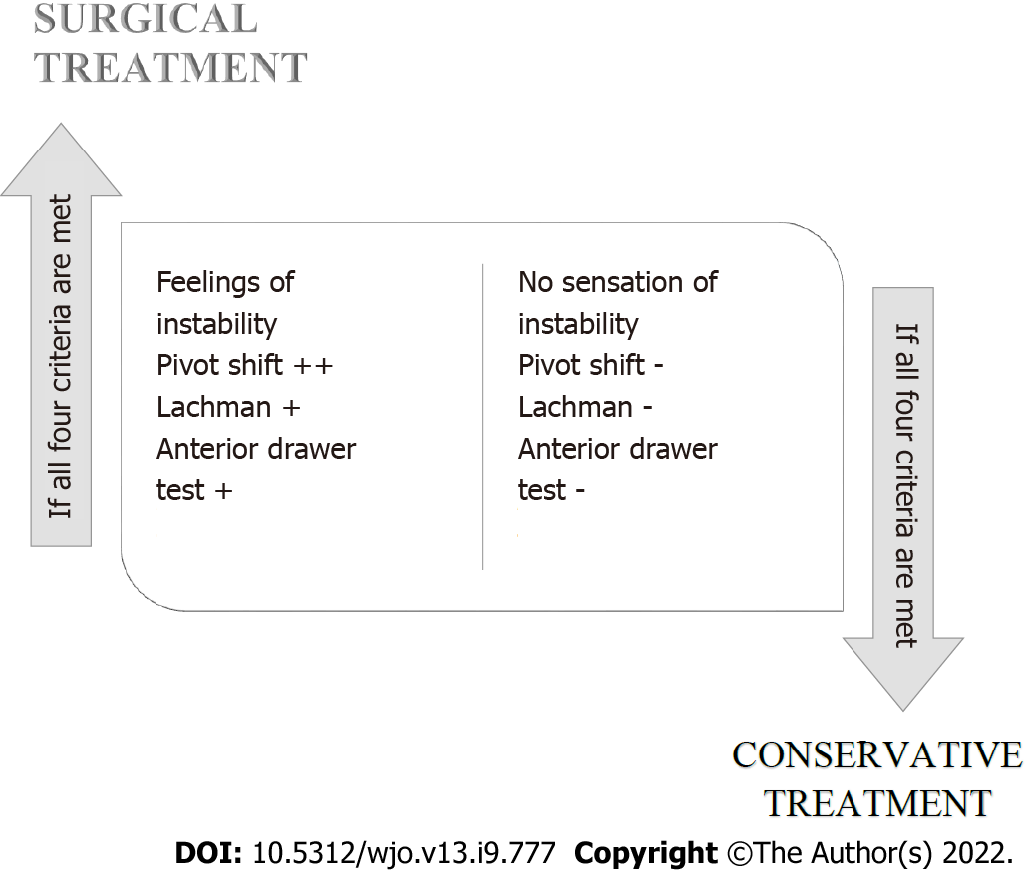
Core Tip: A Delphi study was conducted with a formal consensus process using validated methodology with scientific evidence to develop recommendations and practical guidelines for the assessment of instability injuries in children. Following this expert consensus, surgical treatment is advised when the patient has a subjective sensation of instability accompanied by a pivot shift test ++, and may include an anterior drawer test + and a Lachman test +. If these conditions are not present, the conservative approach should be chosen, as the anatomical and functional development of children, together with a physiotherapy programme, may improve the evolution of the injury.
- Citation: Campón Chekroun A, Velázquez-Saornil J, Guillén Vicente I, Sánchez Milá Z, Rodríguez-Sanz D, Romero-Morales C, Fernandez-Jaén T, Garrido González JI, Sánchez-Garrido MÁ, Guillén García P. Consensus Delphi study on guidelines for the assessment of anterior cruciate ligament injuries in children. World J Orthop 2022; 13(9): 777-790
- URL: https://www.wjgnet.com/2218-5836/full/v13/i9/777.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i9.777
The anterior cruciate ligament (ACL) has a viscoelastic capacity that provides the possibility of dissipating the energy received through adjustments in its length and in the internal distribution of loads[1,2], that is, it has the capacity to generate microscopic adjustments in relation to the internal stresses it has to withstand[3].
ACL injury occurs as a result of excessive force in the anterior translational direction of the tibia or rotation of the femur on the tibia[4].
The most common mechanism of ligament failure is the sequential rupture of bundles of collagen fibres distributed throughout the ligament and not located in a specific area. As it does not have the plastic capacity to deform, ruptures of the ligament are defined as total or partial. There is controversy regarding what is a partial rupture, and there are studies that define it as a hemorrhage in the femoral insertion while others define it as a rupture of the anteromedial and posterolateral fascicles. The American Medical Association establishes a classification in which partial tears correspond to second-degree ligament injuries. Another way of estimating the type of injury is in relation to the percentage of the ligament injured. Partial tears are considered to be between 25% and 75%[5-8]. Partial tears in turn can be classified as high grade when more than 50% of the fibres of the ligament are involved or low grade when the involvement is less than 50%[8].
In general, a partial ACL injury can be defined as a combination of the following factors[8]: (1) Asymmetrical Lachman test result; (2) Pivot Shift negative; (3) Measurement with KT-1000 less than or equal to 3 mm; and (4) Arthroscopic evidence of partial ACL injury.
Adults more frequently suffer ruptures in the medial substance while lesion settlement in children is more frequently observed between the layers of mineralized and non-mineralized fibrocartilage[9].
Once the histological rupture occurs, the ACL goes through four phases: inflammatory, epiligamentous regeneration, proliferative and remodeling. These states are similar to those occurring in other connective tissues but with peculiarities, probably related to two facts: Firstly, the ACL is immersed in the synovial fluid which, due to its characteristics, modifies cell metabolism and the inflammatory response, also preventing the formation of the fibrin clot necessary for the union of the ends of the rupture; furthermore, the vascularization of the ACL after rupture is compromised as the vascular branches that irrigate it also break[10-13]. The flow of synovial fluid is responsible for the fibrin clot not forming by dispersing the blood in the form of hemarthrosis[13]. As a consequence of this lack of fibrin clot there is a decrease in proteins of the extracellular matrix and cytosines such as fibrinogen and fibronectin and Willebrand factor within the ACL wound[14,15].
In injuries of tibial eminence fractures it has been observed that ACL fibres suffer plastic deformation with permanent elongation of the fibers. This fact may be responsible for residual clinical laxity even in cases where surgical reduction or healing has occurred[16].
The mechanisms of injury are multifactorial and include both extrinsic and intrinsic causes[17-24].
The type of pattern of ACL injury depends on the degree of skeletal maturity, this fact may be related to differences in skeletal rigidity and conditions the type of injury in both groups. Tibial avulsion injuries and partial ACL ruptures are more frequent in patients with skeletal immaturity and complete ruptures are more frequent in mature or partially mature patients[25].
The ACL can be injured by two mechanisms, direct contact or non-contact. Approximately 70% of them are due to non-contact injury mechanisms[24-26]. Not all authors define ACL contact injuries in the same way; while some authors define them in relation to those that occur in the absence of contact between players, others define them as the absence of a direct blow to the knee. In fact, there are authors who define "non-contact injuries with disturbance" by referring to injuries resulting from body-body contact, but without direct trauma to the knee[25]. Contact injuries involve injurious mechanisms of hyperextension or excessive valgus stress while the mechanisms that occur in non-contact injuries occur during the development of rapid decelerations or rotations performed in gestures involving pivoting on a fixed foot[27]. In addition, non-contact injuries are often accompanied by an internal hip rotation. This body position in non-contact injuries leads to a collapse in knee valgus or "dynamic knee valgus"[28-30]. It has also been observed that in non-contact injuries the centre of body mass is delayed in relation to the supporting base[24]. Although, as indicated above, the type of injury may be influenced by the degree of skeletal maturity, the injury mechanisms are the same in children and adults[25].
Several studies have shown that non-contact injuries from team ball sports occur at a bending angle of less than 30°. Modifications of the knee valgus angle were observed: in basketball where there was an increase from 4° to 15° in 30 ms, in handball from 3° to 16° in 40 ms, and these periods coincide with the maximum vertical force[31-33]. From this it can be deduced that the valgus position in a relatively straight leg (15°-40°) may be a key factor in the risk of ACL injury. It has also been observed that female athletes with a higher risk of injury land in a position of higher dynamic valgus and high loads of separation. In alpine skiing, other situations are observed such as phantom foot mechanisms, boot-induced anterior drawer mechanisms or external valgus-rotation mechanism[34,35].
It is also important to know the injury mechanisms affecting the posterolateral complex (PCL) of the knee as they represent 16% of all ligament injuries of the knee; of the total PCL injuries only 28% occur in isolation, the rest being associated with ACL injury[36,37]. The common mechanisms of injury of this complex are related to forces in the posterolateral direction of the tibia, hyperextension of the knee and elevated external rotation of the tibia when the knee is in a position of partial flexion. The most frequent contexts in which these injuries occur are sports injuries, road accidents and falls[38].
After an injury at the level of the ACL, a significant increase in metalloproteinases and interleukins at the level of the matrix is observed. Due to the existence of poor vascularization of the articular cartilage and tendons of the knee, the possibility and capacity to eliminate these inflammatory cytokines is diminished. The effects of this difficulty in elimination, causes an increase in the activity of the same that can be translated with irreversible alterations at the level of the collagen and the anchorage points of the ACL[39].
Modifications have also been observed in terms of muscle mass and volume, with significant atrophy in the knee musculature of the injured extremity, mainly in the quadriceps, which may be related to the presence of edema in the knee joint[40]. Altered quadriceps activation and the appearance of asyn
At the biochemical level, alterations have been found in alpha-2 macroglobulin, myostatin, protein-72, mechano GF-C24E, synovial fluid and histochemical alterations at the level of collagen and cartilage[39].
In relation to the alteration of collagen after ACL injury, studies by Li et al[41] reveal that the degradation of collagen after ACL injury is irreversible and is replaced by another type of less structured collagen, thus affecting the integrity of the structure as a whole. This alteration in the synthesis of the correct collagen may be related to a greater probability of developing post-traumatic osteoarthritis.
Most knees with ACL injury experience altered levels of anti-inflammatory chemotactic cytosines causing longer periods of inflammation. In addition, pro-inflammatory and proteoglycan chemicals have been identified with consequent deterioration of the knee joint in patients with ACL injury[41]. Variations in the levels of certain chondrocyte-degrading interleukins have also been observed[42]. In addition, these biochemical modifications can also influence the level of bone tunnels in ACL reconstructions[43]. Therefore, the synovial fluid will have a significant and important effect on knee recovery[41].
Risk factors for injury are classified into extrinsic and intrinsic causes[17-24]. Intrinsic causes are related to factors specific to the individual such as genetic, hormonal, anatomical factors, gender, neuromuscular and cognitive function, as well as previous injury to the knee. Extrinsic causes are external to the individual and among these factors the most studied are the level and type of activity, the type and surface of play, environmental conditions and the material used for the development of the sport or activity[44].
It is interesting that trained athletes have a high risk of breakage[45]. This fact may be related to situations in which there is an increase in joint efficiency. This occurs in situations where the individual acquires a greater degree of skill after practicing joint movements, which causes a decrease in antagonistic coactivation, making the ACL the only joint stabilizer in these circumstances[46]. Other studies also show the synergy between the stabilizing function of the rotational laxity of the ACL and the antagonistic coactivation of the hamstrings[47].
The anatomical region with the highest number of injuries in children and adolescents is the knee, which suffers up to 60% of injuries in the sports environment[31]. Among knee injuries, ACL ruptures have a 10 times higher incidence than the rest of the injuries. The relationship between specific anatomical characteristics and the risk of ACL injury has been studied, as well as the relationship with changes in anatomical characteristics during the stages of growth and skeletal maturation. Kiapour Ata[48] in 2016 conducted a study in which he observed significant differences in both the size and orientation of the age-dependent ACL in both females and males in healthy knees. They presented preliminary results indicating that changes in ACL size in relation to length, cross-section and area are significantly different in boys than in girls. Although it was observed that the ACL became more vertical in both the sagittal and coronal planes with similar patterns in boys and girls, the area of the ACL (cross-section) increased more in boys during early school age and late adolescence while girls showed this modification only when they became adolescents[48]. The same author also studied modifications of femoral condyles in relation to age and sex: Both bicondylar width and intercondylar notch increased continuously in boys after becoming adolescents, remaining constant in young adolescents; girls showed a higher medial femoral condyle curvature in late adolescents compared to boys of the same age and a more curved lateral femoral condyle compared to boys. They also found age-related anatomical modifications of the tibial plateau in both girls and boys. There was a difference in size, more pronounced in boys; slope, greater in girls; and depth, greater in boys, of the tibial plateau between girls and boys in the stages following skeletal maturation[49-52].
Risk factors for ACL rupture in skeletally immature patients are divided into intrinsic and extrinsic factors.
The most studied, and therefore best known, intrinsic factors are those related to anatomy: increased pelvic tilt, increased femoral anteversion, increased Q-angle, increased tibial slope fall, increased foot pronation, scaphoid fall and decreased intercondylar notch[48,50]. Also very important as a risk factor is female gender where ACL ruptures are 6 times more frequent compared to men[50]. In relation to this data, it is known that female patients are usually accompanied by data on hypermobility-hyperlaxity together with genu valgus and genu recurvatum[51].
In relation to hormonal factors, the relationship between the phase of the menstrual cycle and rupture of the ACL has been observed to be greater in the follicular phase where the concentration of estrogen is higher[50].
In relation to extrinsic factors, the most important are climatic conditions, footwear and its interaction with the playing field and court.
During summer conditions of light rain followed by evaporation of the same, this causes the surface to harden increasing ACL injuries in these conditions. It has also been studied how certain characteristics of footwear such as size, height and position of the lateral margin of the sole may increase ACL injuries[48,50,52].
As previously mentioned, anatomical conditions are important in ACL injuries. The size of the ACL may be a risk factor for injury in those cases where there is a decrease in the size of the ACL. Davis et al[53] and Dienst et al[54] have presented studies relating the size of the ACL to greater risk of injury in load situations.
Intercondylar notch is another factor to be taken into account. Narrow intercondylar notches are associated with risk of ACL injury. Narrow intercondylar notches cause increased loading on the ACL[55-59]. With the consequent risk of injury; the correlation between narrow intercondylar notches and small ACLs has also been observed, with the width of the intercondylar notch being connected to the area of the ACL cross-section in pediatric populations, and is responsible for 24%-26% of the variations in the ACL cross-section area[48]. Narrow intercondylar notches produce a mechanical impact on the ACL and may have a tearing effect on the ACL when subjected to repetitive and high-risk movements, reducing the structural properties of the ligament over time[48].
Female sex in young adolescents is a risk factor for ACL injury, giving them a different anatomical profile[38]. One of the causes that may explain this fact may be related to a decrease in the inter-conditional space in this population of young adolescents compared to boys of the same age. Young adolescents also present steeper lateral tibial slopes and deeper tibial columns with the consequent greater risk of ACL injury[60-67].
As mentioned above, increased load on the ACL is associated with increased risk of ACL injury. The steep slopes of the posterior tibial plateau are related to this fact[68-74]. In activities involving weight loading, the posterior tibial slope causes a component of anterior shear force due to axial compression force[70].
The increase in the posterior tibial slope is found to be increased in adolescent girls[48] and may cause an increase in anterior tibial shear force[71-73] due to an acceleration of anterior tibial translation[74] with consequent damage to the ACL. Smaller tibial columns will stabilize less the femoral external rotation and femoral translation and may also cause an increase in ACL load[75,76].
Tibial depth has also been associated with the risk of ACL injury in cases where there is less medial tibial depth by providing less resistance to anterior tibial translation[71,72].
There is no unanimity among the various authors on the correlation between an alteration at the muscular level and ACL injuries. Authors such as Zaínos et al[26] present a direct relationship between imbalances in the agonist-antagonist muscles of the knee together with muscle fatigue as with ACL injury. This author states that high levels of fatigue can lead to altered motor control leading to muscle imbalances, although there are not many studies that prove these claims. In the same vein, Orchard et al[77] indicate that excessive extensor force of the quadriceps muscles together with a decrease in the flexor force of the posterior femoral muscles are related to ACL injury. For Malinzak et al[78], motor control may be related to postures that put the ACL at risk in fact when a rapid lower limb maneuver will cause an angular change and an imbalance of the knee and hip; these modifications cause muscle adjustments that increase the risk of ACL injury. However, Garrido[79] and Benell et al[80] state that there is no relationship between knee muscle imbalances and ACL injury.
ACL injury may occur in isolation or be associated with injuries to other structures. In general, the structures most commonly associated with ACL injuries are: Meniscal injuries: These may appear in conjunction with ACL injury in 30% to 60% of individuals. The external meniscus injury is the most frequent in acute ACL injuries and the internal meniscus injury in patients with chronic instabilities[80-82]. Chondral injuries: from bone edema to impacted fractures and even osteochondral fragments[83]. Capsuloligamentous lesions: Usually appear when there are combined injury mechanisms.
Different authors have identified the appearance of associated lesions in relation to sex and age. Posterolateral contusion of the tibial plate tends to appear more frequently in women, while involvement in the external femoral condyle and soft tissue is more prevalent in men. Similarly, a higher rate of patellar tendon rupture has been observed in the adolescent population[84-86].
A national group of surgeons, physiotherapists, basic scientists, orthopaedic surgeons and paediatric orthopaedic surgeons with experience in ACL instability was convened. A formal consensus process was conducted using a validated methodology. We reviewed the existing literature, held a consensus group meeting to develop recommendations, followed by a broader consultation meeting with an open invitation for final ratification. We conducted an iterative consensus (Delphi) study involving national and international experts in anterior cruciate ligament diagnosis. Group members were recruited through expressions of interest and specific invitations from experts. The Delphi study consisted of four rounds of anonymous surveys. Rounds 1 and 2 involved the generation and ranking of an extensive list of possible characteristics. In rounds 3 and 4, participants were presented with the results of previous rounds and asked to agree on a set of preliminary criteria. Panel participants (n = 34, range by Round 28-30) were predominantly highly experienced clinicians, representing a variety of clinical experience and all inhabited continents. Based on the initial rounds, a set of preliminary criteria was developed, incorporating three levels of diagnostic certainty: healthy ligament, partial rupture and suspected complete rupture. Consensus was reached in Round 4, with a very high level of agreement (> 89%) for all levels of criteria and subcategories. The adoption of the criteria was supported by 96% of the panel members and the guidelines were reviewed and authorised by the NEUMUSK research group, followed by the trauma and orthopaedic specialists of the CEMTRO clinic in Madrid before final publication.
Following the literature review and the multidisciplinary group meeting, an assessment including the following screening tests is proposed.
The assessment of ACL injury is mostly clinical[87-92]. Different exploration tests have been described to assess the integrity or insufficiency of the ACL throughout history.
Georges K Noulis in 1875 first described the Trillat-Lachman test to evaluate ACL integrity with the knee in extension. In 1938, Palmer first discussed the "drawer sign" indicating that the positivity of this sign is a pathognomonic sign of ACL rupture. In 1960, Ritchei described Trillat-Lachman's technique again and 1976 Torg et al[93] (Lachman's student) described the test and made it known. The test described by John Lachman and released by Torg demonstrated the biomechanical superiority of the test over the previous drawer test. In 1976, Hughston et al[49] presented a classification of knee ligament instabilities and indicated that the ACL increases in association with ACL tear and posterior oblique ligament injury. In 1968, Slocum et al[101] defined and described a technique for "rotational instability" of the knee in relation to injury of the medial and ACL components[94-102]. Also in this year, Galway and Macintosh described the phenomenon of pivot shift in relation to rupture of the external capsule with injury of the ACL[98].
The Lachman test has a sensitivity of 62% and a specificity of 82% and is a sign of laxity. It is more sensitive for fibres in the posterolateral beam. The anterior drawer test has a sensitivity of 56% and a specificity of 82% and is a sign of ACL rupture. It is more sensitive for fibres in the anteromedial beam[99,100]. There is a variety of the anterior drawer test that is externally rotated and specifically allows assessment of posterior-internal structures[102].
The pivot shift test, Jerk test, has a sensitivity of about 90%. The existence of concomitant lesions such as LLI rupture, iliotibial strap rupture or mechanical interposition may make this test difficult[99].
For a correct diagnosis it is necessary to establish the difference between laxity and instability[102]: Laxity: Objective and quantifiable exploratory sign in relation to capsuloligamentous insufficiency. Instability: Subjective symptom of discomfort experienced by the patient.
The loss of stability of the knee is objectified according to the existence of laxity in the knee. The AOSSM (American Orthopaedic Society for Sports Medicine) Committee on Research and Education classifies them as follows[103]: Non-rotating, single plane linear: There are several types (anterior, posterior, internal and external). It is graded from 0 to 3 through the anterior drawer tests: 0: Normal laxity; 1 +: Anterior translation less than 0.5 cm; 2 ++: Anterior translation between 0.5 cm and 1 cm; 3 +++: Anterior translation between 1 cm and 1.5 cm.
Rotary, single or two-plane: they can be: Anterointernal: Abduction, external rotation and tibial anterior translation. It causes the internal tibial plate to move or sublux anteriorly in relation to the femur. Posterointernal: This occurs when there is a posterior translation of the internal tibial plate in relation to the femur. Anteroexternal: Excessive anterior translation of the external tibial plate. Posteroexternal: posterior translation of the external tibial plate.
Combined: all types of combinations can be found, the most common being: Anterointernal/antero-external, anterointernal/posterointernal and anterointernal/posteroexternal. Considering the approach followed by Guillén García et al[104] and his team regarding the diagnosis of knee stability, different criteria should be followed: (1) Anatomical: The proximal and distal insertion of the ACL is behind the femoral axis. This is why when the lesion mechanism is produced by a knee rotation and the foot is fixed, the ACL and menisci are broken; (2) Biomechanical: It is impossible for the PCL to be the axis of the knee. The PCL changes its angular arrangement on the tibial platform between 20º and 85º in relation to the knee's flexo-extension angle; and (3) Clinical: Both the healing and the tolerance of the patient to the ACL rupture are bad in contrast to the PCL in which maintaining a state of rest produces its healing and the tolerance of isolated injuries of the same by the patient are good.
In relation to the above, the classification of knee instabilities is as follows: Anterior laxity: Anterior laxity: Isolated ACL tear (very rare); Anteromedial laxity: ACL rupture next to the medial system; Antero-posterolateral laxity: ACL rupture next to the posterolateral system. Posterior laxity: Posterior laxity: Isolated PCL tear; Posteromedial laxity: Rupture of the PCL next to the posteromedial system; Posterolateral laxity: LCP rupture together with the posterolateral system. Combined antero-posterior laxity: ACL, PCL rupture along with medial or lateral systems.
Before performing the specific tests, the healthy knee should be explored as a control for guidance. The tests that produce the least pain should be started first to prevent the muscle spasm from interfering with the rest of the tests.
Lachman test: This is the main test to be carried out on an acute injury[100]. It is performed with the knee in a 30° knee flexion position and a force is applied in an anterior direction. It is considered positive in cases where the anterior displacement of the tibia is increased compared to the contralateral knee. It is important to note the end point of tibial displacement. This end point is soft or weak when there is a break in the ACL[100-105].
Anterior drawer flex/rotate test: Combines Lachman's test and lateral pivot shift. Both hands are used to firmly grip the calf and move the knee in a 15° to 30° flexion arc. When the ACL is broken, at 15° of flexion there is an anterior subluxation of the tibia and an external rotation of the femur. Increasing the flexion to 30° produces a posterior reduction of the tibia and an internal rotation of the femur[106]. There are authors who claim that this test has less sensitivity than Lachman’s test, although it has more sensitivity than the tibial shift tests[107].
Anterior drawer test: This test assesses the anteroposterior femorotibial displacement with a starting position of 90º knee flexion and 45º hip flexion and the foot fixed on the table. From this position, traction and pressure movements are performed in a neutral anterior and posterior position, respectively; to put the capsuloligamentous structures in tension, the test is performed in internal rotation and external rotation. An important detail is to check the initial tibial starting point; if there is an injury at the level of the PCL it could give a false anterior tibial displacement when performing the technique[108].
Hughston et al[109] in 1976 described this technique by performing a proximal measurement in the tibia between the thumb and other fingers; the hamstrings are palpated to see if they are relaxed. From this position, an anterior tibial traction is performed to evidence the existence of laxity. If an end point is seen at the limit of the displacement, it is indicative of the continuity of the ACL. If the consistency of the endpoint is spongy and lacking in firmness, it is indicative of rupture of the ACL.
Anterior Neutral Box: The starting position is with the tibia in neutral position. If the test is positive it may be due to injury in: ACL, ACL and internal complex, ACL and external complex or both complexes[110].
Anterior drawer-external rotation: The starting position is with the external rotation of the tibia. In this position the structures of the internal complex are tightened. A moderate positive test result indicates injury of the internal complex, while a strong positive test result indicates injury of the posterior internal angle[101].
Anterior drawer test-Internal Rotation: The starting position is with tibial internal rotation. In this position the structures of the external complex are tightened. A moderate positive result indicates injury to the structures of the external complex. If it is intense positive, we must also think of injury of the PCL together with the structures of the external compartment (LCE, external capsule and posterior-external angle). In this case a further assessment of the postero-external capsule can be made by testing the external rotation recurvatum[109].
Pivot shift test: The starting position is in knee extension and valgus along with internal rotation of the tibia. A progressive flexion of the tibia is performed and towards 30° a posterior displacement of the tibia is felt on the femur. This displacement appears as a consequence of the reduction of the anterior subluxation of the tibia[110].
Hughston's jerk test: A 45° hip flexion is performed with the knee at 90°. A valgus force is applied and the knee is extended with the tibia in internal rotation. The test is positive when there is a transitory anterior subluxation of the tibia on the femur over the 30° of flexion, with a spontaneous reduction occurring as the knee is extended[109].
Test of internal rotation of the tibia: The starting position is with flexion of 45° or more of the knee and external rotation of the tibia. From this position, the leg is progressively extended, allowing internal rotation to occur while applying a valgus force with anterior pressure applied behind the head of the fibula. This produces anterior subluxation of the anterolateral tibia. As the knee approaches full extension, the tibia is reduced, producing an audible "snap"[111].
Slocum test: The patient is placed in the lateral position with the knee and hip of the healthy lower limb flexed. The pathological knee is placed in contact with the table in an extended position. Palpation of the fibula head is performed with the index finger of the left hand while the index finger of the right hand contacts the external femoral condyle. To perform the technique, a valgus force is applied to the knee in flexion. When the ACL is insufficient, the anterior subluxation of the tibia is reduced by reaching 30° of knee flexion. The reduction is felt with the fingers[112].
Figure 1 shows the summary diagram of the decision-making process regarding the assessment of the ACL and the decision to carry out conservative or surgical treatment.
In order to assess the existence of an associated lesion, together with the analysis of the stability of the knee, an exploration of the rest of the structures of the knee should be performed, paying special attention to the menisci and the internal and external collateral ligaments[100].
When there is an ACL lesion, the study and assessment of the capsuloligamentary structures should include the assessment of both the external/internal collateral complex and the postero-internal and postero-external capsular complex. For this purpose, both the valgus and the forced varus must be evaluated both in full extension and in 30º flexion. It is important to increase strength progressively to the point of onset of pain to verify maximum laxity without the appearance of muscle spasm[112,113].
Valgus in extension: When the test is positive, the structures that may be damaged are: the superficial and deep portion of the LCM, posterior oblique ligament, PAPI, peripheral disinsertion of the medial meniscus and ACL. If it is very severe there could be injury of the PCL[85].
Valgus in 30° flexion: A slight positivity in the test will indicate a rupture of the superficial portion of the LLI. If the result is a severe yawn, other structures of the internal complex besides the ACL and PCL will also be affected[85].
Varus in extension: When the test is positive it will indicate injury of the LLL, middle capsule, arcuate ligament and Maissiat band, in addition to the ACL. If it is very severe, the PCL will also be injured[85].
Varus at 30° flexion: Mild external yawning indicates injury to the CLL. If the test result is very severe there will be injury to the medial capsule, the Maissiat band and the arcuate ligament[85].
It is essential to assess the presence or absence of meniscal pathology concomitant to ACL injuries. The diagnosis will obviously be clinical through evaluative tests that can be divided into[114]: (1) Tests that cause pain or clicks with palpation of the interline; (2) Tests that generate pain with rotation of the tibia on the femur.
With regard to the reliability of the meniscal tests, several studies have tried to prove the effectiveness of the different meniscal tests. There are differences in results between the researchers. Both types of evaluation tests have low diagnostic value when applied individually, increasing their usefulness when combined with the clinical history[114]. A cross-sectional study by Gobbo et al[115] in 2011, studied the sensitivity and specificity of the McMurray, Steinmann I, Steinmann II, Childress and Apley tests for both the medial and lateral meniscus. The analysis showed that the sensitivity for the medial meniscus was 89% and the specificity was 31% while for the lateral meniscus the sensitivity was 85% vs a specificity of 24%. This study corroborates the data presented previously that tests performed in isolation have a lower diagnostic value. In relation to the independent analysis of each test, the Apley test has the best specificity for both the medial and the lateral meniscus. In relation to the precision for detecting lesions, greater precision was obtained in the evaluation of lesions in the medial meniscus than in the lateral meniscus, except for the Apley test which showed the same predictive value for both the lateral and medial meniscus lesions[115].
The knee has its own language with which it communicates what is happening to it. This language does so through sound. It is important to listen to the sounds that the knee shows us during its movement, which will help us to extract information about your injury[116].
ACL injuries are common in sports. Most ACL injuries are non-contact in nature and usually occur in certain athletic tasks. Complete ACL tears can lead to chronic knee problems, such as knee instability, damage to the meniscus and chondral surface, and osteoarthritis. Due to the increasing participation of children and adolescents in both organized sports and intense sports training at an early age, the number of ACL injuries in this age group has increased, accounting for 3.3% of ACL injuries[68-74].
Practice is not yet standardised and the literature to guide decision-making in children is very limited. This consensus process has been based on the expert experience of a diverse group of professionals treating and dealing with this injury, their thorough examination and subsequent decision-making focused on the prior assessment of the patient, and sometimes based on the experience of the healthcare professional conducting the patient study.
Although there is level 1 clinical evidence on screening for ACL rupture, this process is based on the practical and clinical experience of the examiner. However, there are few manuscripts that include screening for this injury in minors, so these guidelines have been developed in the healthcare setting. This consensus has been developed by a large group of experts in the field and has resulted in a solid and established method for the development of guidelines in the healthcare of the pathology in question. We believe that the knee has its own language with which it communicates what is happening to it. This language is expressed through sound, which is why the term genufonia is coined[116]. It is important to listen to the sounds that the knee shows us during its movement, which will help us to extract information about its injury.
It can be seen that the consensus statements cover the assessment and screening of ACL rupture in children. A decision is made in the evaluation of patients, depending on whether surgical treatment[117] or conservative treatment will be chosen.
ACL rupture is a complex pathology with multiple approaches that should be based primarily on patient assessment and evaluation. In the absence of a solid evidence base and the lack of consensus in the literature on the approach and exploration of this injury in minors, these established guidelines aim to contribute to that decision-making process to assist the clinician in performing the most optimal treatment with the goal of benefiting the patient as much as possible. Following this expert consensus, surgical treatment is advised when the patient has a subjective sensation of instability accompanied by a pivot Shift ++ test, and may include an anterior drawer + test and Lachman + test. If these conditions are not present, the conservative approach should be chosen, as the anatomical and functional development of the children, together with a physiotherapy programme, can improve the evolution of the injury.
The authors would like to thank all persons who contributed to the process of developing these screening and decision-making guidelines.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Konrads C, Germany; Liu P, China S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med. 1991;19:217-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 874] [Cited by in RCA: 735] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 2. | Chu D, LeBlanc R, D'Ambrosia P, D'Ambrosia R, Baratta RV, Solomonow M. Neuromuscular disorder in response to anterior cruciate ligament creep. Clin Biomech (Bristol, Avon). 2003;18:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 452] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 4. | DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 279] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 5. | Noyes FR, Mooar LA, Moorman CT 3rd, McGinniss GH. Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br. 1989;71:825-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 143] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Lamar DS, Bartolozzi AR, Freedman KB, Nagda SH, Fawcett C. Thermal modification of partial tears of the anterior cruciate ligament. Arthroscopy. 2005;21:809-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Messner K, Maletius W. Eighteen- to twenty-five-year follow-up after acute partial anterior cruciate ligament rupture. Am J Sports Med. 1999;27:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | DeFranco MJ, Bach BR Jr. A comprehensive review of partial anterior cruciate ligament tears. J Bone Joint Surg Am. 2009;91:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Souryal TO, Freeman TR. Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am J Sports Med. 1993;21:535-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 216] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Bolívar-Arroyo V, Raya-Villarraso A, Garrido-Gómez J. Anterior cruciate ligament injury. New treatment options by tissue engineering. Actual Medica. 2014;99: 157-161. [DOI] [Full Text] |
| 11. | Woo SL, Vogrin TM, Abramowitch SD. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg. 2000;8:364-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Murray MM, Martin SD, Martin TL, Spector M. Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am. 2000;82:1387-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 273] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 13. | Andersen RB, Gormsen J. Fibrin dissolution in synovial fluid. Acta Rheumatol Scand. 1970;16:319-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Murray MM, Spindler KP, Ballard P, Welch TP, Zurakowski D, Nanney LB. Enhanced histologic repair in a central wound in the anterior cruciate ligament with a collagen-platelet-rich plasma scaffold. J Orthop Res. 2007;25:1007-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 196] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 15. | Murray MM, Spindler KP, Devin C, Snyder BS, Muller J, Takahashi M, Ballard P, Nanney LB, Zurakowski D. Use of a collagen-platelet rich plasma scaffold to stimulate healing of a central defect in the canine ACL. J Orthop Res. 2006;24:820-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 135] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Trivedi V, Mishra P, Verma D. Pediatric ACL Injuries: A Review of Current Concepts. Open Orthop J. 2017;11:378-388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1025] [Cited by in RCA: 939] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 18. | McNair PJ, Marshall RN, Matheson JA. Important features associated with acute anterior cruciate ligament injury. N Z Med J. 1990;103:537-539. [PubMed] |
| 19. | Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. El efecto del entrenamiento neuromuscular sobre la incidencia de lesiones de rodilla en atletas femeninas. Un estudio prospectivo. Am J Sports Med. 1999;27:699-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 999] [Cited by in RCA: 884] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 20. | Ireland ML. Anterior cruciate ligament injury in female athletes: epidemiology. J Athl Train. 1999;34:150-154. [PubMed] |
| 21. | Nichol Allison M. Literature Review of Female Anterior Cruciate Ligament Injuries. Senior Honors Theses. 2004;88. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Romero D. Analysis models for the prevention of sports injuries. Epidemiological study of injuries: The UEFA model in football. Apunts Medicina de l'Esport. 2010;45:95-102. [DOI] [Full Text] |
| 23. | Silvers HJ, Mandelbaum BR. Prevention of anterior cruciate ligament injury in the female athlete. Br J Sports Med. 2007;41 Suppl 1:i52-i59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | LaBella CR, Hennrikus W, Hewett TE; Council on Sports Medicine and Fitness, and Section on Orthopaedics. Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics. 2014;133:e1437-e1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 139] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 25. | McKay S, Chen C, Rosenfeld S. Orthopedic perspective on selected pediatric and adolescent knee conditions. Pediatr Radiol. 2013;43 Suppl 1:S99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Zahínos JI, González C, Salinero J. Epidemiological study of the injuries, the processes of readaptation and prevention of the injury of anterior cruciate ligament in the professional football. JSHR. 2010;2:139-150. [DOI] [Full Text] |
| 27. | Dorizas JA, Stanitski CL. Anterior cruciate ligament injury in the skeletally immature. Orthop Clin North Am. 2003;34:355-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Hewett TE, Myer GD, Ford KR. Lesiones del ligamento cruzado anterior en atletas femeninas: parte 1, mecanismos y factores de riesgo. Am J Sports Med. 2006;34:299-311. [RCA] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 589] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 29. | Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43:417-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 424] [Cited by in RCA: 372] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 30. | Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37:252-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 290] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 31. | Kirkendall DT, Garrett WE Jr. The anterior cruciate ligament enigma. Injury mechanisms and prevention. Clin Orthop Relat Res. 2000;64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 80] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 32. | Teitz CC. Video analysis of ACL injuries. In: Griffin LY, ed. Prevention of noncontact ACL injuries. Rosemont, IL: American Association of Orthopaedic Surgeons. 2001; 87–92. [DOI] [Full Text] |
| 33. | Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 821] [Cited by in RCA: 804] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 34. | Krosshaug T, Slauterbeck JR, Engebretsen L, Bahr R. Biomechanical analysis of anterior cruciate ligament injury mechanisms: three-dimensional motion reconstruction from video sequences. Scand J Med Sci Sports. 2007;17:508-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 35. | Natri A, Beynnon BD, Ettlinger CF, Johnson RJ, Shealy JE. Alpine ski bindings and injuries. Current findings. Sports Med. 1999;28:35-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 60] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 226] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 37. | LaPrade RF, Wentorf FA, Fritts H, Gundry C, Hightower CD. A prospective magnetic resonance imaging study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy. 2007;23:1341-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 153] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 38. | Dean RS, LaPrade RF. ACL and Posterolateral Corner Injuries. Curr Rev Musculoskelet Med. 2020;13:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 39. | Reyes T, Willoughby D. Biochemical and Structural Alterations in Skeletal Muscle Following ACL Injury: A Narrative Review. IJKSS. 2020;8:8-13. [DOI] [Full Text] |
| 40. | Yoh K, Benjamin Infantolino W. Weekly Changes in Vastus Lateralis Volume Following ACL Injury. IJATT. 2017;22: 38-43. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 41. | Li H, Chen C, Chen S. Posttraumatic knee osteoarthritis following anterior cruciate ligament injury: Potential biochemical mediators of degenerative alteration and specific biochemical markers. Biomed Rep. 2015;3:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Larsson S, Struglics A, Lohmander LS, Frobell R. Surgical reconstruction of ruptured anterior cruciate ligament prolongs trauma-induced increase of inflammatory cytokines in synovial fluid: an exploratory analysis in the KANON trial. Osteoarthritis Cartilage. 2017;25:1443-1451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 43. | Bigoni M, Turati M, Gandolla M, Sacerdote P, Piatti M, Castelnuovo A, Franchi S, Gorla M, Munegato D, Gaddi D, Pedrocchi A, Omeljaniuk RJ, Locatelli V, Torsello A. Effects of ACL Reconstructive Surgery on Temporal Variations of Cytokine Levels in Synovial Fluid. Mediators Inflamm. 2016;2016:8243601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 44. | Smith HC, Vacek P, Johnson RJ, Slauterbeck JR, Hashemi J, Shultz S, Beynnon BD. Risk factors for anterior cruciate ligament injury: a review of the literature - part 1: neuromuscular and anatomic risk. Sports Health. 2012;4:69-78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 198] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 45. | Renström P, Arms SW, Stanwyck TS, Johnson RJ, Pope MH. Strain within the anterior cruciate ligament during hamstring and quadriceps activity. Am J Sports Med. 1986;14:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 346] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 46. | Person RS. [Electromyographic investigations of coordination of the antagonistic muscles in development of motor habit]. Zh Vyssh Nerv Deiat Im I P Pavlova. 1958;8:17-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Louie JK, Mote CD Jr. Contribution of the musculature to rotatory laxity and torsional stiffness at the knee. J Biomech. 1987;20:281-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Kiapour Ata. Age and Sex Dependent Variations in Knee Anatomy During Skeletal Maturation in Children and Adolescents. Master's thesis, Harvard Medical School. 2016;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | 49 Hughston JC, Whatley GS, Dodelin RA. The athlete and his knees. South Med J. 1961;54: 1372-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 50. | Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lázaro-Haro C, Cugat R. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17:705-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 538] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 51. | Hinton RY, Rivera VR, Pautz MJ, Sponseller PD. Ligamentous laxity of the knee during childhood and adolescence. J Pediatr Orthop. 2008;28:184-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 52. | Gracia G, Thévenin-Lemoine C, Laumonerie P, Sales de Gauzy J, Accadbled F; French Arthroscopy Society. Anterior cruciate ligament tears in children: Management and growth disturbances. A survey of French Arthroscopy Society members. Orthop Traumatol Surg Res. 2019;105:747-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 53. | Davis TJ, Shelbourne KD, Klootwyk TE. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1999;7:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 86] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 54. | Dienst M, Schneider G, Altmeyer K, Voelkering K, Georg T, Kramann B, Kohn D. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127:253-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 55. | Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 218] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 56. | LaPrade RF, Burnett QM 2nd. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1994;22:198-202; discussion 203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 201] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 57. | Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 225] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 58. | Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43:1702-1707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 209] [Cited by in RCA: 192] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 59. | Whitney DC, Sturnick DR, Vacek PM, DeSarno MJ, Gardner-Morse M, Tourville TW, Smith HC, Slauterbeck JR, Johnson RJ, Shultz SJ, Hashemi J, Beynnon BD. Relationship Between the Risk of Suffering a First-Time Noncontact ACL Injury and Geometry of the Femoral Notch and ACL: A Prospective Cohort Study With a Nested Case-Control Analysis. Am J Sports Med. 2014;42:1796-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 60. | Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1056] [Cited by in RCA: 966] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 61. | Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86-92. [PubMed] |
| 62. | Gwinn DE, Wilckens JH, McDevitt ER, Ross G, Kao TC. La incidencia relativa de lesión del ligamento cruzado anterior en hombres y mujeres en la Academia Naval de los Estados Unidos. Am J Sports Med. 2000;28:98-102. [RCA] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 235] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 63. | Lindenfeld TN, Schmitt DJ, Hendy MP, Mangine RE, Noyes FR. Incidence of injury in indoor soccer. Am J Sports Med. 1994;22:364-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 198] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 64. | Messina DF, Farney WC, DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999;27:294-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 205] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 65. | Myklebust G, Maehlum S, Holm I, Bahr R. A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998;8:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 270] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 66. | Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, Georgoulis T, Hewett TE, Johnson R, Krosshaug T, Mandelbaum B, Micheli L, Myklebust G, Roos E, Roos H, Schamasch P, Shultz S, Werner S, Wojtys E, Engebretsen L. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394-412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 559] [Cited by in RCA: 442] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 67. | Stevenson H, Webster J, Johnson R, Beynnon B. Gender differences in knee injury epidemiology among competitive alpine ski racers. Iowa Orthop J. 1998;18:64-66. [PubMed] |
| 68. | Beynnon BD, Hall JS, Sturnick DR, Desarno MJ, Gardner-Morse M, Tourville TW, Smith HC, Slauterbeck JR, Shultz SJ, Johnson RJ, Vacek PM. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42:1039-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 138] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 69. | Beynnon BD, Vacek PM, Sturnick DR, Holterman LA, Gardner-Morse M, Tourville TW, Smith HC, Slauterbeck JR, Johnson RJ, Shultz SJ. Geometric profile of the tibial plateau cartilage surface is associated with the risk of non-contact anterior cruciate ligament injury. J Orthop Res. 2014;32:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 70. | Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Efectos del aumento de la pendiente tibial en la biomecánica de la rodilla. Am J Sports Med. 2004;32:376-382. [RCA] [DOI] [Full Text] [Cited by in Crossref: 523] [Cited by in RCA: 572] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 71. | Hashemi J, Chandrashekar N, Mansouri H, Slauterbeck JR, Hardy DM. The human anterior cruciate ligament: sex differences in ultrastructure and correlation with biomechanical properties. J Orthop Res. 2008;26:945-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 72. | Hashemi J, Chandrashekar N, Mansouri H, Gill B, Slauterbeck JR, Schutt RC Jr, Dabezies E, Beynnon BD. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 290] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 73. | Lipps DB, Oh YK, Ashton-Miller JA, Wojtys EM. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med. 2012;40:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 74. | McLean SG, Oh YK, Palmer ML, Lucey SM, Lucarelli DG, Ashton-Miller JA, Wojtys EM. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am. 2011;93:1310-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 75. | McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech (Bristol, Avon). 2010;25:781-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 76. | Sturnick DR, Argentieri EC, Vacek PM, DeSarno MJ, Gardner-Morse MG, Tourville TW, Slauterbeck JR, Johnson RJ, Shultz SJ, Beynnon BD. A decreased volume of the medial tibial spine is associated with an increased risk of suffering an anterior cruciate ligament injury for males but not females. J Orthop Res. 2014;32:1451-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 77. | Orchard J, Seward H, Garlick D. Ground conditions and AFL injuries. In: Australian Conference of Science and Medicine in Sport. Canberra: Sports Medicine Australia 1997. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 78. | Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon). 2001;16:438-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 414] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 79. | Garrido J, Pineda Y, Piñeros A, Rodríguez M. Imbalancemuscular como factor de riesgo para lesiones deportivas de rodilla en futbolistas profesionales. Acta Colombiana de Medicina del Deporte. 2003. Available from: http://amedco.encolombia.com/deporte1091imbalance.htm. |
| 80. | Bennell K, Wajswelner H, Lew P, Schall-Riaucour A, Leslie S, Plant D, Cirone J. Isokinetic strength testing does not predict hamstring injury in Australian Rules footballers. Br J Sports Med. 1998;32:309-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 203] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 81. | Dejour H, Walch G, Neyret P, Adeleine P. [Results of surgically treated chronic anterior laxities. Apropos of 251 cases reviewed with a minimum follow-up of 3 years]. Rev Chir Orthop Reparatrice Appar Mot. 1988;74:622-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 82. | Wexler G, Hurwitz DE, Bush-Joseph CA, Andriacchi TP, Bach BR Jr. Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop Relat Res. 1998;166-175. [PubMed] |
| 83. | Goldstein J, Bosco JA. 3rd La rodilla deficiente en el LCA: historia natural y opciones de tratamiento. Bull Hosp Jt Dis. 2001;60:173-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 84. | Fayad LM, Parellada JA, Parker L, Schweitzer ME. MR imaging of anterior cruciate ligament tears: is there a gender gap? Skeletal Radiol. 2003;32:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 85. | Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18:955-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 254] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 86. | Futch LA, Garth WP, Folsom GJ, Ogard WK. Acute rupture of the anterior cruciate ligament and patellar tendon in a collegiate athlete. Arthroscopy. 2007;23:112.e1-112.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 87. | Huang W, Zhang Y, Yao Z, Ma L. Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthop Traumatol Turc. 2016;50:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 88. | Abruscato K, Browning K, Deleandro D, Menard Q, Wilhelm M, Hassen A. Diagnostic accuracy of the lever sign in detecting anterior cruciate ligament tears: A systematic review and meta-analysis. Int J Sports Phys Ther. 2019;14:2-13. [PubMed] |
| 89. | Lelli A, Di Turi RP, Spenciner DB, Dòmini M. The "Lever Sign": a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2016;24:2794-2797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 90. | Leblanc MC, Kowalczuk M, Andruszkiewicz N, Simunovic N, Farrokhyar F, Turnbull TL, Debski RE, Ayeni OR. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:2805-2813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 91. | Décary S, Ouellet P, Vendittoli PA, Desmeules F. Reliability of physical examination tests for the diagnosis of knee disorders: Evidence from a systematic review. Man Ther. 2016;26:172-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 92. | Brady MP, Weiss W. Clinical Diagnostic Tests Versus MRI Diagnosis of ACL Tears. J Sport Rehabil. 2018;27:596-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 93. | Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 383] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 94. | Lichtenberg MC, Koster CH, Teunissen LPJ, Oosterveld FGJ, Harmsen AMK, Haverkamp D, Hoornenborg D, Berg RP, Bloemers FW, Faber IR. Does the Lever Sign Test Have Added Value for Diagnosing Anterior Cruciate Ligament Ruptures? Orthop J Sports Med. 2018;6:2325967118759631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 95. | Lange T, Freiberg A, Dröge P, Lützner J, Schmitt J, Kopkow C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture--A systematic review. Man Ther. 2015;20:402-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 96. | Décary S, Ouellet P, Vendittoli PA, Roy JS, Desmeules F. Diagnostic validity of physical examination tests for common knee disorders: An overview of systematic reviews and meta-analysis. Phys Ther Sport. 2017;23:143-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 97. | O'Shea KJ, Murphy KP, Heekin RD, Herzwurm PJ. The diagnostic accuracy of history, physical examination, and radiographs in the evaluation of traumatic knee disorders. Am J Sports Med. 1996;24:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 98. | Leyes Vences M, Forriol Campos F. Historia de la reparación del ligamento cruzado anterior History of anterior cruciate ligament repair. Rev Esp Artrosc Cir. 24:38-58. [DOI] [Full Text] |
| 99. | Boeree NR, Ackroyd CE. Assessment of the menisci and cruciate ligaments: an audit of clinical practice. Injury. 1991;22:291-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 100. | Gürpınar T, Polat B, Polat AE, Çarkçı E, Öztürkmen Y. Diagnostic Accuracy of Lever Sign Test in Acute, Chronic, and Postreconstructive ACL Injuries. Biomed Res Int. 2019;2019:3639693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 101. | Slocum DB, Larson RL. Rotatory instability of the knee. Its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am. 1968;50:211-225. [PubMed] |
| 102. | Noyes FR GE. Diagnosis of the knee ligaments injuries: technical concepts. Part II. New York: Churchill Livingstone 1988; 261-285 . [DOI] [Full Text] |
| 103. | Manzano-Serrano E. Tesis Doctoral resultados de la cirugía del ACL plastias mixtas biológicas-sintéticas. Departamento de Cirugía. Facultad de Medicina. Universidad Complutense. Madrid, Mayo 1.995. [DOI] [Full Text] |
| 104. | Guillén García PJC, Madrigal J, Royo J, Concejero López V, Sobrado Pérez J. Traumatismos deportivos de la rodilla. Revista de Ortopedia y Traumtología. 1985;29. [DOI] [Full Text] |
| 105. | Trillat A, Dejour H, Bousquet G. Chirurgie du genou III Journées Lionaises 1978; 75-80. [DOI] [Full Text] |
| 106. | Noyes F, Butíer D, Grood E. Clinical paradoxes of anterior cruciate inestability and a new test to detect its inestability. Orthop Trans. 2:36-37. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 107. | Tria AJ, Mores TM. Diagnóstico de las lesiones de los ligamentos de la rodilla. En: Scott W.N. (ed). Lesiones del ligamento y el mecanismo extensor de la rodilla. Madrid. Mosby-Year Book de España: 1992; 87-99. [DOI] [Full Text] |
| 108. | Cabot JR. Lesiones ligamentosas de la rodilla. Ponencia oficial III. Congreso Hispano-Argentino de Cirugía ortopédica y traumatología, 1.973. |
| 109. | Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am. 1976;58:173-179. [PubMed] |
| 110. | Galway RD, Beaupre A. , MacIntosh DL. Pivot shift: A clinical sign of symptomatic anterior cruciate insufficiency. J Bone Joint Surg. 763-764. [RCA] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 218] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 111. | Losee RE, Johnson TR, Southwick WO. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am. 1978;60:1015-1030. [PubMed] |
| 112. | Slocum DB, James SL, Larson RL, Singer KM. Clinical test for anterolateral rotary instability of the knee. Clin Orthop Relat Res. 1976;63-69. [PubMed] [DOI] [Full Text] |
| 113. | Navarro Quilis A. Inestabilidad ligamentosa de la rodilla. Ponencia oficial XXI Congreso de la SECOT. Garsi Madrid. 1983;. [DOI] [Full Text] |
| 114. | Gupta Y, Mahara D, Lamichhane A. McMurray's Test and Joint Line Tenderness for Medial Meniscus Tear: Are They Accurate? Ethiop J Health Sci. 2016;26:567-572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 115. | Gobbo Rda R, Rangel Vde O, Karam FC, Pires LA. Physical examinations for diagnosing meniscal injuries: Correlation with surgical findings. Rev Bras Ortop. 2011;46:726-729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 116. | Guillén García P. Lenguaje de la rodilla. Medicina RANd editor. Discurso de ingreso Madrid. 1997;169-190. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 117. | Velázquez-Saornil J, Ruíz-Ruíz B, Rodríguez-Sanz D, Romero-Morales C, López-López D, Calvo-Lobo C. Efficacy of quadriceps vastus medialis dry needling in a rehabilitation protocol after surgical reconstruction of complete anterior cruciate ligament rupture. Medicine (Baltimore). 2017;96:e6726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |