Published online Jul 18, 2022. doi: 10.5312/wjo.v13.i7.644
Peer-review started: February 28, 2022
First decision: April 13, 2022
Revised: May 27, 2022
Accepted: July 6, 2022
Article in press: July 6, 2022
Published online: July 18, 2022
Processing time: 139 Days and 5.6 Hours
Despite over 150000 amputations of lower limbs annually, there remains a wide variation in tourniquet practice patterns and no consensus on their necessity, especially among orthopedic patient populations. The purpose of this study was to determine whether tourniquet use in orthopedic patients undergoing below knee amputation (BKA) was associated with a difference in calculated blood loss relative to no tourniquet use.
To determine if tourniquet use in orthopedic patients undergoing BKA was associated with a difference in calculated blood loss relative to no tourniquet use.
We performed a retrospective review of consecutive patients undergoing BKA by orthopedic surgeons at a tertiary care hospital from 2008 through 2018. Blood loss was calculated using a combination of the Nadler equation for preoperative blood volume and a novel formula utilizing preoperative and postoperative hemoglobin levels and transfusions. Univariate and forwards step-wise multivariate linear regressions were performed to determine the association between tourniquet use and blood loss. A Wilcoxon was used to determine the univariate relationship between tourniquet use and blood loss for in the restricted subgroups of patients who underwent BKA for trauma, tumor, and infection.
Of 97 eligible patients identified, 67 underwent surgery with a tourniquet and 30 did not. In multivariate regression, tourniquet use was associated with a 488 mL decrease in calculated blood loss (CI 119-857, P = 0.01). In subgroup analysis, no individual group showed a statistically significant decrease in blood loss with tourniquet use. There was no significant association between tourniquet use and either postoperative transfusions or reoperation at one year.
We found that tourniquet use during BKA is associated with decreased calculated intraoperative blood loss. We recommend that surgeons performing this procedure use a tourniquet to minimize blood loss.
Core Tip: We retrospectively evaluated 138 patients who underwent a below knee amputation by an orthopedic surgeon and compared the calculated intraoperative blood loss between patients who received or did not receive a tourniquet. We found that patients who did receive a tourniquet had significantly lower blood loss than those who did not.
- Citation: Wyland AE, Woelber E, Wong LH, Arakawa J, Working ZM, Meeker J. Association between tourniquet use and intraoperative blood loss during below-knee amputation. World J Orthop 2022; 13(7): 644-651
- URL: https://www.wjgnet.com/2218-5836/full/v13/i7/644.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i7.644
Since its 2nd century introduction to amputation surgery by Heliodorus, the tourniquet has been nearly as enduring as the knife itself[1,2]. Yet despite the amputation of over 150000 Lower limbs annually in the United States, there are wide variations in tourniquet practice patterns and no consensus on their necessity during limb removal[3].
Tourniquet application during limb amputation is controversial. Historically, the high rate of mortality associated with early amputations was attributed to both delayed septicemia and immediate blood loss, leading surgeons such as Esmarch, Lister, and Cushing to improve upon early designs during the 19th and 20th centuries[2]. Today, tourniquet use is associated with decreased intraoperative blood loss and fewer transfusions in below knee amputations performed primarily in vascular surgery settings[4,5]. However, this has hardly settled the question of whether they should be used routinely for hemorrhage control during orthopedic limb removal. Throughout the dissection, use of a tourniquet may provide a drier surgical field by slowing intraoperative bleeding, but at the same time may limit the palpation of neurovascular structures[6-8]. Additionally, blood loss continues beyond the intraoperative period, and application of a tourniquet may prevent the surgeon from identifying damage to small vessels that continue to ooze postoperatively. There is also a theoretical risk of damaging fragile atherosclerotic vessels as pneumatic pressure increases, leading to swelling and blood loss in the perioperative period after the tourniquet has been removed[9]. This may explain studies finding no difference in total blood loss or transfusions with tourniquet use in studies of both below knee amputation and total knee arthroplasty[9-12].
There is a paucity of literature describing the association between tourniquet use and blood loss during below knee amputation in orthopedic populations, which include patients undergoing surgery for neoplastic disease, trauma, and infection[11]. Furthermore, blood loss in prior studies has typically been recorded using surgeon estimation, which is subjective, imprecise, and does not account for perioperative “hidden” blood loss that continues after closure of the wound[10,13,14].
The primary purpose of this study was to determine whether tourniquet use in orthopedic patients undergoing below knee amputation was associated with a difference in calculated blood loss relative to no tourniquet use. Secondarily, we assessed whether tourniquet application was associated with postoperative transfusions during the inpatient stay or reoperation within one year. We hypothesized that tourniquet use would not be associated with decreased blood loss, postoperative transfusions, or reoperation within one year.
With Institutional Review of Board approval, we retrospectively reviewed consecutive patients undergoing below knee amputation by orthopedic surgeons at a single academic institution over a ten-year period from January 1, 2008 to December 31, 2018. The hospital is a tertiary referral center for soft tissue sarcomas and a Level 1 trauma center. This study was conducted following STROBE guidelines[15].
Patients were identified by CPT code for below-knee amputation. To prevent confounding by other sources of bleeding, patients were excluded if the indication for below-knee amputation was a trauma that had occurred within one week, if they had active gastrointestinal bleeding, or if they had a diagnosed bleeding disorder. We excluded patients with through-knee amputations.
Data for identified patients was collected from chart review including demographic characteristics (e.g., age, sex), known or potential modifiers of blood loss (e.g., kidney dysfunction, platelet count), and surgical data (e.g., indication for surgery, intraoperative transfusions). A full list of variables that were collected can be found in Supplementary Table 1. Tourniquet use and tourniquet time were taken from surgeon operative reports. Post-operative hemoglobin and hematocrit results were taken within 72 h of the operation. We used the first post-operative hemoglobin in blood loss calculations.
| No tourniquet | Tourniquet | P value | |
| n | 30 | 67 | |
| Age, mean (SD) | 43.31 (18.53) | 56.05 (14.02) | < 0.001 |
| Gender = M (%) | 19 (63.3) | 43 (64.2) | 1 |
| Height (mean (SD)) | 1.73 (0.10) | 1.75 (0.10) | 0.423 |
| Weight (mean (SD)) | 90.63 (31.57) | 98.78 (32.46) | 0.252 |
| BMI (mean (SD)) | 29.96 (9.62) | 32.12 (9.81) | 0.315 |
| Diabetes (%) | 7 (23.3) | 27 (40.3) | 0.165 |
| Hepatitis C (%) | 0 (0.0) | 4 (6.0) | 0.415 |
| Smoking (%) | 6 (20.0) | 26 (38.8) | 0.112 |
| IV drug use (%) | 1 (3.3) | 5 (7.5) | 0.746 |
| Alcoholism (%) | 2 (6.7) | 10 (14.9) | 0.419 |
| Outside hospital transfer (%) | 3 (10.0) | 13 (19.4) | 0.391 |
| ASA score (%) | 0.433 | ||
| 1 | 1 (3.3) | 0 (0.0) | |
| 2 | 12 (40.0) | 20 (29.9) | |
| 3 | 15 (50.0) | 40 (59.7) | |
| 4 | 2 (6.7) | 6 (9.0) | |
| 5 | 0 (0.0) | 1 (1.5) | |
| Homeless (%) | 0 (0.0) | 1 (1.5) | 1 |
| Preoperative hemoglobin (mean (SD)) | 11.91 (2.64) | 11.78 (2.74) | 0.82 |
| Platelets (mean (SD)) | 270.83 (153.50) | 315.09 (114.02) | 0.117 |
| Indication for surgery (%) | < 0.001 | ||
| Infection | 14 (46.7) | 53 (79.1) | |
| Trauma | 2 (6.7) | 9 (13.4) | |
| Tumor | 14 (46.7) | 5 (7.5) |
Blood loss was determined using a series of calculations. Preoperative blood volume was calculated using patient height, weight, and gender by the Nadler formula[16]:
Blood volume (Male) = 0.3669 × H3 + 0.03219 × W + 0.6041.
Blood volume (Female) = 0.3561 × H3 + 0.03308 × W + 0.1833.
Total blood loss was then determined using calculated blood volume, change in hemoglobin concentration, and the mass of hemoglobin transfused intraoperatively, based on modification of the formula by Wied et al[10]: Total mass of Hgb lost = Blood volume (L) × (Hgb preop - Hgb postop) × 10 + mass of transfused Hgb. Where mass of transfused Hgb = 61.25g × intraoperative units transfused[16]. Blood loss (L)= total mass of Hgb lost/ (Hgb preop × 10).
We excluded five variables with > 5% data missingness (functional capacity, erythrocyte sedimen
For our primary outcome, we performed a univariate linear regression to determine the association between tourniquet use and blood loss. We also ran subgroup analyses by indication for surgery, using a Wilcoxon due to the non-parametric distribution of blood loss and the low number of observations in each subgroup. We then performed a forward stepwise regression with potential modifiers of the association between tourniquet use and blood loss, sequentially retaining variables that changed the estimation of the association by greater than 10 percent. We excluded the surgeon as a variable from this analysis as it was thought to lie on a causal pathway between indication and blood loss and was not generalizable. We also excluded operative time due to the directionality of its association with tourniquet use and because it likely lies along the causal pathway between tourniquet use and blood loss[11]. To avoid spurious associations, we only included variables that were logically associated tourniquet use and blood loss, and limited the variables tested to 10% of the number of observations. We included interaction terms for variables of interest.
We then performed two logistic regressions in a similar fashion using postoperative transfusion and reoperation in one year as outcomes. Postoperative transfusions were only included if administered during the immediate inpatient stay. Reoperations included stump revisions, revision to a higher-level amputation (e.g., above-the-knee), and irrigation and debridement.
All statistical analysis was performed using R version 3.6.3 including the packages tableone, dplyr, ggplot2, and chest. Statistical significance was determined at 0.05. The study was reviewed by our statistician Dr. Erik Woelber.
138 patients undergoing below knee amputation were identified by chart review. 41 patients were excluded because they sustained a trauma within the prior week, leaving 97 patients for analysis. Of the patients identified, 67 underwent surgery with a tourniquet and 30 did not. Indications included infection (69%, n = 67), trauma (11%, n = 11), and tumor (20%, n = 19). Demographic characteristics are shown in Table 1. The tourniquet group was older (56 vs 43 years, P < 0.001) and had categorical differences in indication for surgery (P < 0.001).
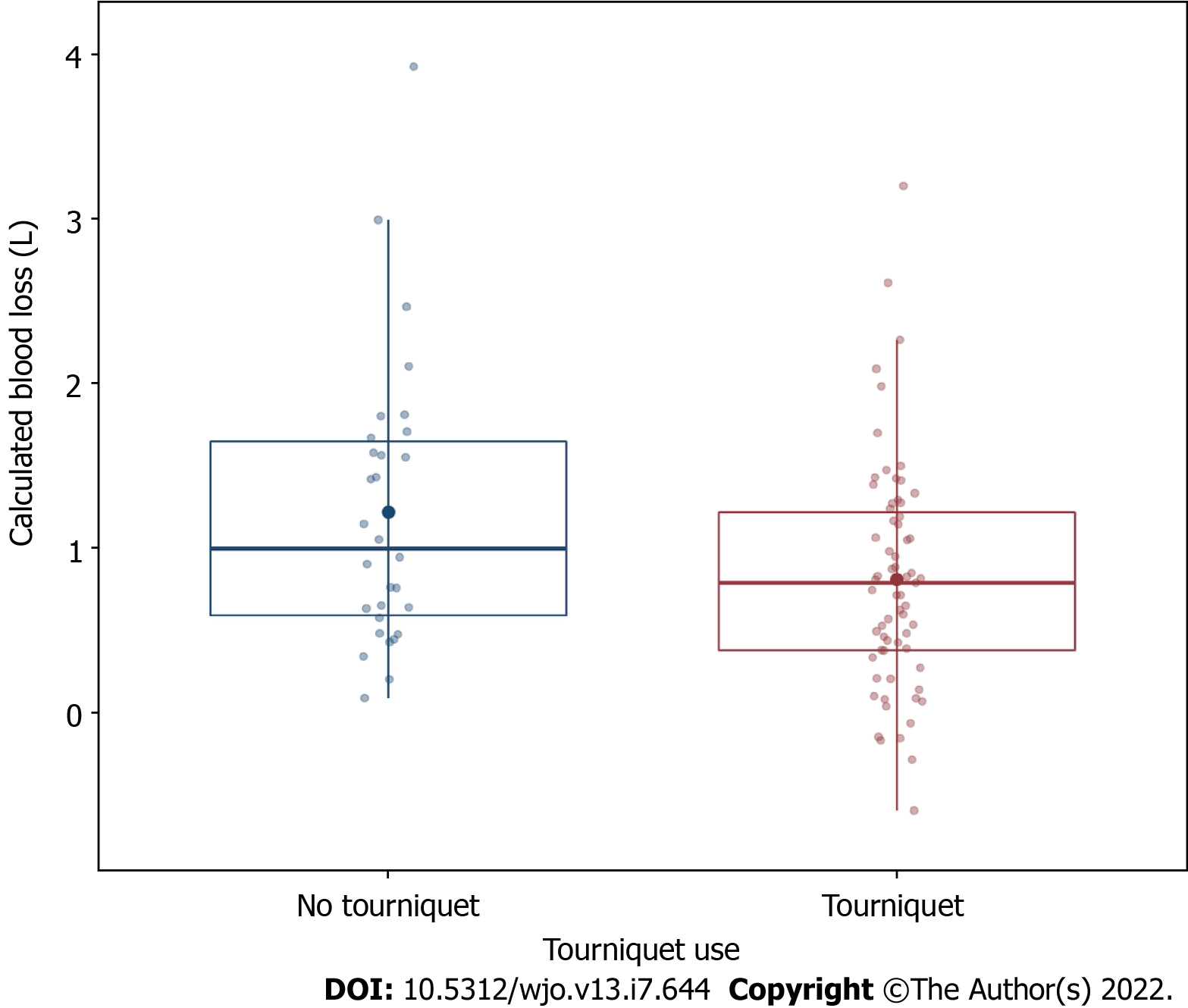
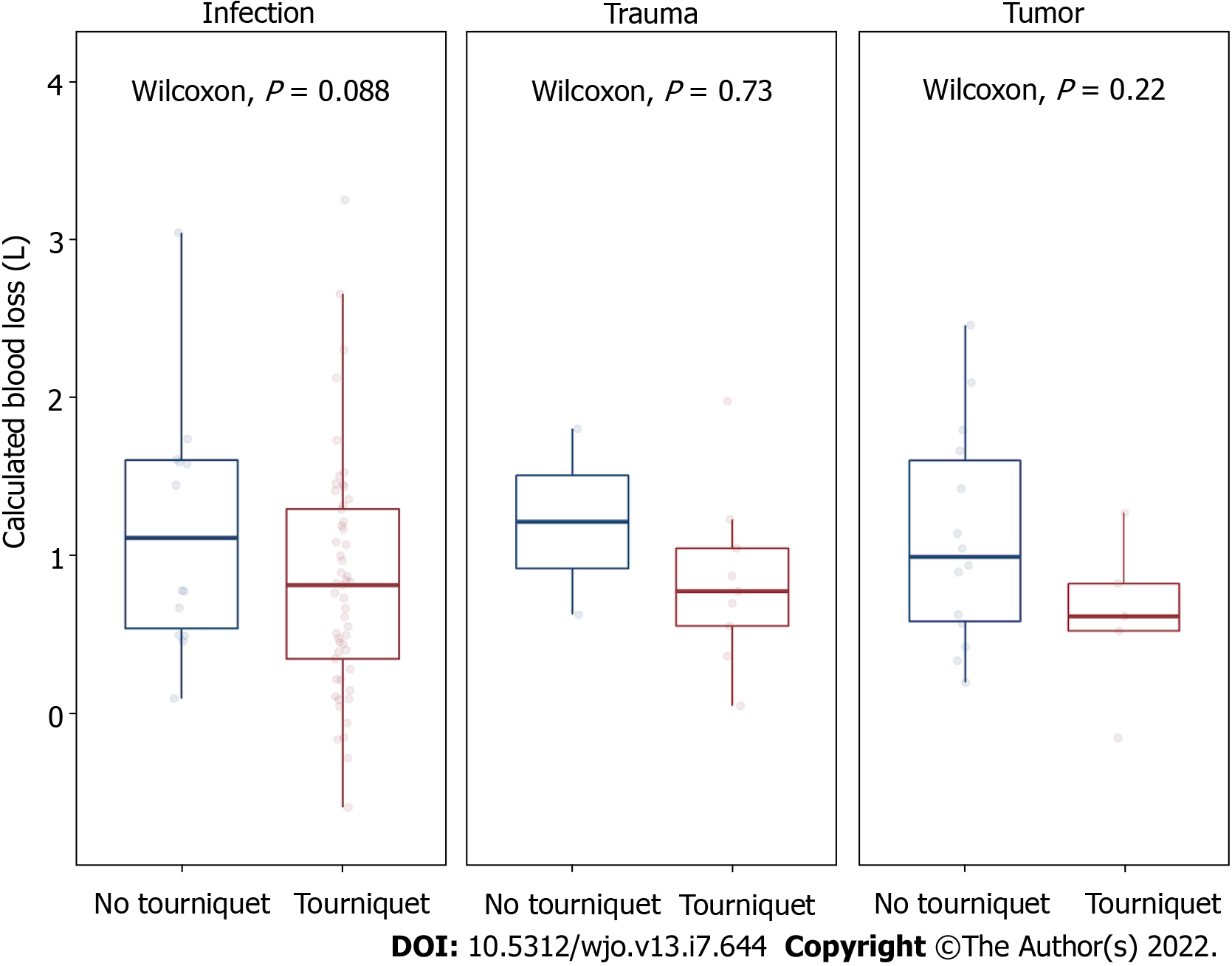
In simple linear regression, tourniquet use was associated with significantly decreased blood loss (-0.41 Liters, SE 0.17, P = 0.01) (Figure 1). The calculation allowed for negative blood loss values to occur for 6 patients (6%). The plots reveal a right-skewed distribution of calculated blood loss for both tourniquet and non-tourniquet patients. In the analysis of restricted subgroups, no individual group showed a statistically significant decrease in blood loss with tourniquet use (Figure 2).
Results of multivariate regression are shown in Table 2. Of the tested variables, only the indication for surgery modified the association between tourniquet use and blood loss above the 10% threshold for inclusion. Though it differed significantly between tourniquet and non-tourniquet groups, age did not significantly modify the association between tourniquet use and blood loss. Two patients with missing data for creatinine were excluded from stepwise regression modelling but were included in the final multivariate model. The interaction term between tourniquet use and indication for surgery was not significant (P = 0.84 for trauma and P = 0.99 for tumor, relative to infection).
| Variable | Estimate (95%CI) | P value |
| Tourniquet use | -488 mL (-857, -119) | 0.01 |
| Indication (vs infection) | ||
| Trauma | 12 mL (-474, 498) | 0.96 |
| Tumor | -190 mL (-624, 245) | 0.39 |
Thirteen patients in the tourniquet group (19%) and six patients in the non-tourniquet group (20%) received a postoperative transfusion. Twenty patients in the tourniquet group (30%) and 13 patients in the non-tourniquet group (43%) underwent an unplanned reoperation within one year of the index surgery. Adjusted secondary analyses showed no statistically significant association between tourniquet use and either inpatient blood transfusion after the first postoperative lab draw (OR 0.83, CI 0.25-2.72, P = 0.75) or reoperation at one year (OR 0.84, CI 0.26-2.79, P = 0.78).
Our results indicate that tourniquet use during below knee amputations performed on orthopedic surgery patients is associated with significantly decreased surgical blood loss. The magnitude of the as
sociation is noteworthy, as a 488 mL decrease with use of a tourniquet equates to an approximately ten percent difference in total blood volume lost.
Our findings are consistent with the results of prior studies in non-orthopedic populations. A non-randomized study found that tourniquet use in vascular patients undergoing below-knee amputation is associated with decreased surgical blood loss, fewer postoperative transfusions, and fewer complications[4]. Similarly, a prospective, randomized, blinded study found that tourniquet use in peripheral arterial disease patients is associated with less intraoperative blood loss, a smaller perioperative drop in hemoglobin, fewer transfusions, and similar complication rates[5].
Our secondary analysis did not demonstrate a statistically significant association between tourniquet use and inpatient postoperative transfusions. A prior study found that as much blood is lost following above-knee amputations postoperatively as during the procedure, which could explain this result[10]. Another study echoed the finding that tourniquet use during BKA is associated with less intraoperative blood loss, but no difference in total blood loss (including the postoperative period)[11]. In the joint arthroplasty literature, tourniquet use is not associated with a difference in transfusions or total blood loss[12]. In our study, it is also possible that we did not have adequate power to detect a difference in transfusions due to their rarity.
Our secondary analysis also did not demonstrate a statistically significant association between tourniquet use and reoperations at one year. At least one study comparing reoperation rates with and without a tourniquet found no difference in the rate of conversion to a higher-level amputation at 30 days[11].
This study had multiple limitations. First, the calculation of intraoperative blood loss relies on several assumptions: It assumes that all patients are adequately resuscitated following their operation at the time of their first postoperative blood draw (and thus may have underestimated total blood loss), and it does not account for changes in intravascular volume cause by vasoconstriction or fluid shifts. The calculation also does not account for any blood volume in the amputated limb. In theory, the equation overestimates blood loss because it is based off of a pre-operative patient weight, but this impact is negligible and should be equal in both groups. Patients taking anticoagulation or antiplatelet medications could also have increased blood loss and this was not taken into account in our analysis. However, patients are usually instructed to stop such medications before an operation. These calculations impose rigid mathematical formulas on patients representing a range of body compositions and physiologic responses to surgery that are dynamic and idiosyncratic. This may be particularly relevant in tertiary referral centers that see a non-representative range of body habitus and patients with impaired compensatory responses to hemorrhage. However, calculated blood loss has several advantages over surgeon estimation, including its standardization and immunity to the bias of a surgeon’s visual assessment. It is also easily replicable at other centers and avoids the logistical hassles of alternative methods such as weighing surgical drapes and sponges.
A second limitation is that our patient population was heterogenous and derived from an academic center, and therefore potentially less generalizable. This fact is offset by our study being the first to approach this question in an orthopedic patient population, which differs from the more commonly studied general surgery population in terms of indications and patient characteristics. Second, the patients underwent procedures by a diverse group of surgeons employing a range of surgical techniques, increasing the external validity of our results.
Another limitation is that in the patients with an infectious etiology, which was primarily due to diabetes, the presence of peripheral vascular disease was not taken into account, which could affect blood loss.
Our study found no evidence of effect modification by the indication for surgery, indicating that use of a tourniquet does not have a variable effect on blood loss in oncology, infection, and trauma patients. However, the subgroup analysis was not powered to detect a difference in blood loss; comparisons within these groups were affected by small sample sizes, particularly in the group undergoing amputation due to trauma (n = 11). Thus, both the individual subgroup analyses and the lack of evidence for effect modification should be interpreted with caution.
We found that tourniquet use during below knee amputation is associated with decreased calculated intraoperative blood loss. The decision to use a tourniquet depends on multiple factors related to the individual patient, the underlying pathology being treated, and surgeon preferences. However, based on these results, we recommend that surgeons performing this procedure use a tourniquet if they wish to minimize blood loss. Analysis of a larger database may provide supporting evidence for tourniquet use in specific patient subgroups including patients with malignant tumors and those who sustained acute traumatic injury.
Below-knee amputation (BKA) is common procedure in the orthopedic population. Etiology for patients requiring this surgery are primarily trauma, infection, and neoplastic disease. There is currently no consensus among orthopedic surgeons regarding the use of a tourniquet in these patients.
The motivation behind this study is to determine a possible method to minimize blood loss in BKA operations.
To compare blood loss between patients who received a tourniquet during their BKA procedure and those who did not.
We performed a retrospective cohort study on consecutive patients who underwent BKA over a ten-year period at a tertiary care hospital. Blood loss was estimated using the Nadler equation for preoperative blood volume and a novel formula that utilizes preoperative and postoperative hemoglobin levels and transfusions. Univariate and forwards stepwise multivariate linear regression were utilized to determine an association between tourniquet use and blood loss.
We found that patients undergoing a BKA operation with tourniquet use were associated with a 488 mL decrease in calculated blood loss. This is significant for orthopedic surgeons wanting to minimize blood loss in BKA operations.
This study utilized a calculated blood loss rather than the commonly utilized estimated blood loss, and proposes that a tourniquet should be used if orthopedic surgeons wish to minimize blood loss in BKA operation.
Research should be conducted on a larger population across multiple centers to determine a stronger association and increase external validity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liu C, China; Skok P, Slovenia; Vitiello R, Italy S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Kirkup J. A History of Limb Amputation. London: Springer, 2007: 1-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Bowker JH, Pritham CH. The history of amputation surgery and prosthetics. In: Smith DG, editor. Atlas of Amputation and Limb Deficiencies: Surgical, Prosthetic and Rehabilitation Principles, 3rd edition. Rosemont, IL: AAOS, 2004: 3-21. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95:875-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 173] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 4. | Wolthuis AM, Whitehead E, Ridler BM, Cowan AR, Campbell WB, Thompson JF. Use of a pneumatic tourniquet improves outcome following trans-tibial amputation. Eur J Vasc Endovasc Surg. 2006;31:642-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Choksy SA, Lee Chong P, Smith C, Ireland M, Beard J. A randomised controlled trial of the use of a tourniquet to reduce blood loss during transtibial amputation for peripheral arterial disease. Eur J Vasc Endovasc Surg. 2006;31:646-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Jarolem KL, Scott DF, Jaffe WL, Stein KS, Jaffe FF, Atik T. A comparison of blood loss and transfusion requirements in total knee arthroplasty with and without arterial tourniquet. Am J Orthop (Belle Mead NJ). 1995;24:906-909. [PubMed] |
| 7. | Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. 2000;169-177. [RCA] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 123] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Streichenberger R, Barjoud H, Konieczny M, Elias W. Surgical management of major varicose veins of the lower limb using a pneumatic tourniquet. Ann Vasc Surg. 1991;5:559-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Silver R, de la Garza J, Rang M, Koreska J. Limb swelling after release of a tourniquet. Clin Orthop Relat Res. 1986;86-89. [RCA] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Wied C, Tengberg PT, Kristensen MT, Holm G, Kallemose T, Troelsen A, Foss NB. Total Blood Loss After Transfemoral Amputations Is Twice the Intraoperative Loss: An Observational Cohort Study of 81 Nontraumatic Amputations. Geriatr Orthop Surg Rehabil. 2017;8:123-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Wied C, Tengberg PT, Holm G, Kallemose T, Foss NB, Troelsen A, Kristensen MT. Tourniquets do not increase the total blood loss or re-amputation risk in transtibial amputations. World J Orthop. 2017;8:62-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? Knee. 2010;17:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 13. | Wied C, Foss NB, Kristensen MT, Holm G, Kallemose T, Troelsen A. Surgical apgar score predicts early complication in transfemoral amputees: Retrospective study of 170 major amputations. World J Orthop. 2016;7:832-838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Rothermel LD, Lipman JM. Estimation of blood loss is inaccurate and unreliable. Surgery. 2016;160:946-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 15. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2924] [Cited by in RCA: 3445] [Article Influence: 191.4] [Reference Citation Analysis (0)] |