Published online May 18, 2022. doi: 10.5312/wjo.v13.i5.481
Peer-review started: February 21, 2021
First decision: July 28, 2021
Revised: August 1, 2021
Accepted: April 8, 2022
Article in press: April 8, 2022
Published online: May 18, 2022
Processing time: 445 Days and 7 Hours
The management of idiopathic scoliosis (IS) in skeletally immature patients should aim at three-dimensional deformity correction, without compromising spinal and chest growth. In 2019, the US Food and Drug Administration approved the first instrumentation system for anterior vertebral body tethering (AVBT), under a Humanitarian Device Exception, for skeletally immature patients with curves having a Cobb angle between 35° and 65°.
To summarize current evidence about the efficacy and safety of AVBT in the management of IS in skeletally immature patients.
From January 2014 to January 2021, Ovid Medline, Embase, Cochrane Library, Scopus, Web of Science, Google Scholar and PubMed were searched to identify relevant studies. The methodological quality of the studies was evaluated and relevant data were extracted.
Seven clinical trials recruiting 163 patients were included in the present review. Five studies out of seven were classified as high quality, whereas the remaining two studies were classified as moderate quality. A total of 151 of 163 AVBT procedures were performed in the thoracic spine, and the remaining 12 tethering in the lumbar spine. Only 117 of 163 (71.8%) patients had a nonprogressive curve at skeletal maturity. Twenty-three of 163 (14.11%) patients required unplanned revision surgery within the follow-up period. Conversion to posterior spinal fusion (PSF) was performed in 18 of 163 (11%) patients.
AVBT is a promising growth-friendly technique for treatment of IS in growing patients. However, it has moderate success and perioperative complications, revision and conversion to PSF.
Core tip: Although anterior vertebral body tethering is a promising growth-friendly technique for treatment of idiopathic scoliosis in growing patients, it has a moderate success rate and has perioperative complications, revision and conversion to posterior spinal fusion. Future level I studies, with long-term follow-up, are needed to best define the limits and potentials of this emerging surgical technique.
- Citation: Bizzoca D, Piazzolla A, Moretti L, Vicenti G, Moretti B, Solarino G. Anterior vertebral body tethering for idiopathic scoliosis in growing children: A systematic review. World J Orthop 2022; 13(5): 481-493
- URL: https://www.wjgnet.com/2218-5836/full/v13/i5/481.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i5.481
The management of idiopathic scoliosis (IS) in skeletally immature patients should aim at three-dimensional (3D) deformity correction, without compromising the spinal and chest growth and complete lung development[1-3]. In order to achieve all these goals, besides the classic conservative treatments for IS in growing children - i.e., bracing[4-6] and serial casting - several growth-friendly surgical procedures have been introduced in clinical practice in recent years[7]. These include growing rods[8,9], Shilla procedure[10], vertebral body stapling[11], posterior dynamic deformity correction device[12] and anterior vertebral body tethering (AVBT)[11-16].
AVBT for IS correction, in skeletally immature patients, relies on the asymmetric inhibition of vertebral growth, by applying the Hueter-Volkmann principle[17-21]. Each vertebral body grows both in length, via endochondral ossification, and in circumference, by appositional growth[22-25]. The subsequent compression of the growth plate on the curve convexity inhibits vertebral body growth, while the concomitant distraction on the curve concavity promotes vertebral body growth[15]. This dynamic phenomenon finally limits the curve progression and, ideally, reduces deformity without affecting spinal growth and mobility.
After preclinical studies performed in animal models[26-28], in 2010 Crawford and Lenke[16] reported the first case of an 8-year-old child, with a 40° right thoracic curve successfully managed through AVBT. In the following years, based on these encouraging results, different spinal surgeons started the use of off-label devices and the first case series describing the use of AVBT were published by Samdani et al[24,29].
In 2019, the US Food and Drug Administration (FDA) approved the first instrumentation system for AVBT, under a Humanitarian Device Exception, for skeletally immature patients with curves having a Cobb angle between 35° and 65°[30]. Since then, several clinical trials focusing on AVBT have been published[8-12]. However, some controversies still exist about this emerging surgical technique and few data are available about the long-term results.
This systematic review aimed to summarize the current evidence about the efficacy and safety of AVBT in the management of IS in skeletally immature patients. Particular attention was given to surgical indications, clinical and radiological outcomes, postoperative complications, re-intervention rates and conversion rates to posterior spinal fusion (PSF).
The study was conducted with methods described in PRISMA[31]. It was registered in PROSPERO (ID: CRD42020183915) before the data extraction and analysis.
Scopus, Web of Science, Springer Link, Ovid Medline, Embase, Cochrane Library, Google Scholar and PubMed were searched from January 2014 to January 2021 to identify relevant papers for further analysis. The main keywords were: “anterior vertebral body tethering (AVBT)” or “tethering” and “scoliosis” and “growing spine” or “growing child” or “immature patients”. A manual search of the reference lists of the selected publications was also performed to identify additional studies for potential inclusion. Due to the paucity of studies on AVBT, both retrospective and prospective studies were included in the present systematic review. The following exclusion criteria were applied: (1) < 24 mo of follow-up; (2) Lack of surgical intervention description; and (3) Dropout > 20% at the final follow-up. The review was restricted to articles published in English. When multiple papers from the same centre or trial were depicted, the most thorough publication was selected. Two review authors (Bizzoca D and Piazzolla A) analysed the titles and abstracts. Potentially relevant articles were acquired for full-length text and authors were contacted when the full text was not available.
Information was extracted from each study by two review authors (Bizzoca D and Piazzolla A) and finally checked by two other authors (Moretti B and Solarino G), including: (1) Characteristics of study participants (age, gender, preoperative Cobb angle); (2) Study inclusion; (3) Surgical approach; (4) Clinical outcome; (5) Radiological outcome; (6) Percentage of successful AVBT procedures; (7) Perioperative complication rate and type; (8) Re-intervention rate; and (9) Number of conversions to PSF. Disagreements were resolved by discussion between them.
The quality of the analysed papers was evaluated following the American Academy of Orthopedic Surgeons (AAOS) clinical practice guidelines and review methodology version 2[32]. We assessed the following features: Inclusion and exclusion criteria description; sample size and features; number of patients lost to follow-up; prognostic factors evaluation; outcome evaluation; appropriate statistical analysis; references of the study; data evaluation; presence of bias; presence of confounding factors; and follow-up duration. Based on the study design and the depicted flaws, the quality of each study included in this systematic review was defined as follows: High (< 2 flaws); moderate (≥ 2 and < 4 flaws); low (≥ 4 and < 6 flaws) and very low (≥ 6 flaws). Two authors (Bizzoca D and Piazzolla A) independently evaluated all the studies. In case of disagreement between them, a new combined evaluation was performed. Two senior authors (Moretti B and Solarino G) finally approved the quality assessment procedure. Publication bias could not be assessed by a funnel plot considering the low number of patients in each study.
The primary outcome was to assess the success of AVBT at skeletal maturity, with a minimum 24-mo follow-up, in patients managed with this growth-friendly technique. The secondary outcome was to identify the rate of perioperative complications, re-interventions and conversions to PSF, in patients who underwent AVBT. The tertiary outcome was to depict the correct indications for AVBT and the correct preoperative workup, as well as to describe the main feature of the surgical procedure.
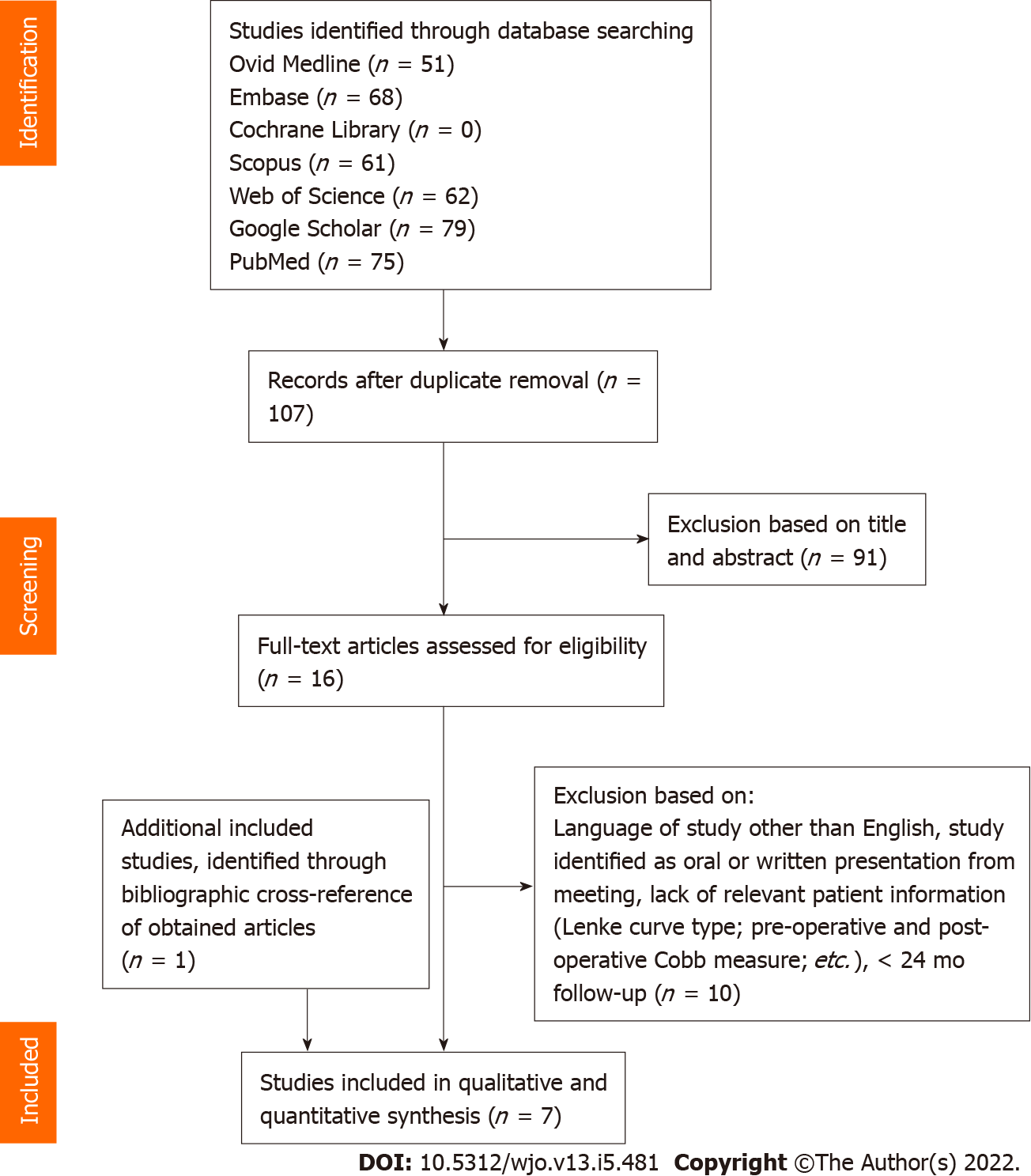
The Scopus, Springer Link, Web of Science, Ovid Medline, Embase, Cochrane Library, Google Scholar and PubMed database searches provided a total of 396 studies for potential inclusion in the review (Figure 1). After adjusting for duplicates, 107 studies remained. Of these, 91 studies were discarded after reading titles and reviewing abstracts. The full text of the remaining 16 studies was examined in greater detail. Of these, 10 studies did not meet the inclusion criteria. One additional study was identified through a bibliographic cross-reference of obtained articles. A total of seven articles were finally included in this systematic review.
The process of quality assessment, performed according to the AAOS clinical practice guidelines and review methodology version 2, gave the following results: Five[14,20-23] studies out of seven (71.43%) were classified as high quality, whereas the remaining two[17,24] studies out of 10 (28.57%) were classified as moderate quality (Table 1).
| Ref. | Design (level of evidence) | Study quality according to AAOS methodology | Inclusion criteria for AVBT | Study group | Control group | AVBT surgical approach | Follow-up | Outcomes at the final FU | Preoperative main features | Results at the final FU |
| Miyanji et al[14], 2020 | Retrospective study (level IV) | High-quality study | Major main T or L curves ≥ 40°. Risser score ≤ 3. Sanders score < 5 | AVBTs (n = 57). Female: 54 (94.74%). Mean age: 12.7 yr (8-16). Curves: Lenke 1: 48; Lenke 2: 6; Lenke 3: 1; Lenke 4: 0; Lenke 5: 1; Lenke 6: 1. Tether location: Thoracic (n = 55); lumbar (n = 2) | None | VATS plus mini-open for TL/L curves | Minimum 24 mo | Clinical and radiological assessment (success: Residual curve < 35° at maturity) | Tethered curve mean Cobb: 51°. Tethered curve flexibility: 41.8%. Untethered minor curve Cobb: 31.5°. TK (T5-T12): 18°. LL (L1-S1): -55.4°. Rib hump: 14.9 mm. Lumbar prominence: 3.9 mm | Tethered curve Cobb: 23°a. Tethered curve correction: 42.9%. Untethered minor curve Cobb: 22.3°a. TK (T5-T12): 22°a. LL (L1-S1): -56.5°. Rib hump: 10.3 mma. Lumbar prominence: 2.3 mma. Successful AVBT: 44 (77.19%) |
| Baker et al[17], 2021 | Retrospective study (level IV) | Moderate quality study | N/A | AVBTs (n = 19 in 17 pts). Female: 12 (70.6%). Mean age: 12.9 yr. Curves: Lenke 1: 9 pts; Lenke 2: 3 pts; Lenke 3: 1 pts; Lenke 4: 0; Lenke 5: 4 pts; Lenke 6: 0. Tether location: Thoracic (n = 13); lumbar (n = 6) | None | VATS plus mini-open for TL/L curves | Minimum 24 mo (2 to 4 yr) | Radiological assessment (success: Residual curve < 35° at maturity) | Tethered curve Cobb: 45°. Tethered curve flexibility: 63%. Untethered minor curve Cobb: 28°. TK (T5-T12): 20°. LL (L1-S1): -59°. Rib hump: N/A. Lumbar prominence: N/A | Tethered curve Cobb: 20°a. Tethered curve correction: 73%. Untethered minor curve Cobb: 26°. TK (T5-T12): N/A. LL (L1-S1): -52°. Rib hump: N/A. Lumbar prominence: N/A. Successful AVBT: 9 (52.94%) |
| Hoernschemeyer et al[20], 2020 | Retrospective study (level IV) | High-quality study | N/A | AVBTs (n = 29). Female: 26 (89.65%). Mean age: 12.7 yr (10-16). Curves: Lenke 1: 23; Lenke 2: 1; Lenke 3: 1; Lenke 4: 0; Lenke 5: 4; Lenke 6: 0. Tether location: Thoracic (n = 22); TL (n = 3); lumbar (n = 4) | None | VATS plus mini-open for TL/L curves | Minimum 24 mo (2 to 5 yr) | Radiological assessment (success: Residual curve ≤ 30° at maturity) | Tethered curve Cobb: MT: 40°. Long thoracic: MT = 56°; L = 22°; Left TL: L = 49°. Tether top, brace bottom: MT = 48°; L=38°. Tether top & bottom: MT = 48°; L = 42°; TK: 36.2°; LL: -60.83°. Rib hump: N/A. Lumbar prominence: N/A | Tethered curve Cobb: MT: 9°b. Long thoracic: MT = 21°; L = -1°. Left TL: L = 21°b. Tether top, brace bottom: MT = 23°a; L = 24°a. Tether top & bottom: MT = 24°a; L = 15°a; TK: 34.48°; LL: -57°. Rib hump: N/A. Lumbar prominence: N/A. Successful AVBT: 20 (74%) |
| Pehlivanoglu et al[21], 2020 | Prospective cohort study (level IV) | High-quality study | Age: 9-14 yr. Risser ≤ 2. Sanders ≤ 4). Curve progression after at least 6 mo of brace (> 40°). MT curve > 35°. Curve flexibility > 30% | AVBTs (n = 21). Female: 15 (71.43%). Mean age: 11.1 yr (9-14). Curves: Lenke 1: 21. Tether location: Thoracic (n = 21) | None | VATS | Minimum 24 mo | Radiological assessment | Tethered curve Cobb: 48.2°. Tethered curve flexibility: N/A. Untethered minor curve Cobb: 24.8°. TK (T5-T12): 26.8°; LL (L1-S1): -51.3°. Rib hump: N/A. Lumbar prominence: N/A | Tethered curve Cobb: 10.1°a. Tethered curve flexibility: N/A. Untethered minor curve Cobb: 9.6°a. TK (T5-T12): 26°; LL (L1-S1): -51.8°. Rib hump: N/A. Lumbar prominence: N/A. Successful AVBT: 20 (95.24%) |
| Newton et al[22], 2020 | Retrospective case-control study (level III) | High-quality study | Age: 9-15 yr. Primary thoracic idiopathic scoliosis. Cobb angle: 40°-67°. Risser ≤ 1. No prior spine surgery | AVBTs (n = 23). Female: 16 (69.56%). Mean age: 12 yr (9-15). Curves: Lenke 1: 23. Tether location: Thoracic (n = 23) | PSF (n = 26). Female: 23 (88.46%). Mean age: 13 yr (10-14). Curves: Lenke 1: 26. Tether location: Thoracic (n = 26) | VATS | Minimum 24 mo (2 to 5 yr) | Clinical and radiological assessment (success: Residual curve < 35° at maturity) | AVBT group: Tethered curve Cobb: 53°. Untethered curve Cobb: 34°. TK (T2-T12): 25°. LL (L1-S1): N/A. Rib hump: N/A. Lumbar prominence: N/A. PSF group: MT: 54°; LT: 34°; TK (T2-T12): 25° | AVBT group: Tethered curve Cobb: 33°a. Untethered minor curve Cobb: 29°. TK (T2-T12): 12°; LL (L1-S1): N/A. Rib hump: N/A. Lumbar prominence: N/A. Successful AVBT: 12 (52%). PSF group: MT: 16°a; LT: 12°a; TK (T2-T12): 29° |
| Wong et al[23], 2019 | Prospective cohort study; a single-centre, Phase-2A pilot study (level IV) | High-quality study | Juvenile or adolescent IS. Age: ≥ 8 and < 15 yr. Risser stage = 0. Bone age of ≤ 13 yr (hand/wrist X-ray). Major right thoracic scoliosis with a Cobb angle of 35°-55° and Lenke-1 curve pattern. TK (T5-T12) < 40°. Instrumentation to be applied no more cephalad than T4 and no more caudal than L2 (inclusive). Menses < 4 mo | AVBTs (n = 5). Female: All. Mean age: 11 yr (9-12). Curves: Lenke 1: All. Tether location: Thoracic (all) | None | VATS | Minimum 4 yr | Clinical and radiological assessment | Tethered curve mean Cobb: 40°. Tethered curve flexibility: 63.7%. Untethered curve Cobb: 20.6°. TK (T5-T12): N/A; LL (L1-S1): N/A; Rib hump: N/A. Lumbar prominence: N/A | Tethered curve Cobb: 18.9°a. Tethered curve correction: 53.8%. Untethered minor curve Cobb: 5°. Successful AVBT: 3 (60%) |
| Samdani et al[24], 2014 | Retrospective study (level IV) | Moderate quality study | N/A | AVBTs (n = 11). Female: 8 (73%). Mean age: 12.3 yr. Curves: Lenke 1: All. Tether location: Thoracic (all) | None | VATS | Minimum 24 mo | Clinical and radiological assessment | Tethered curve Cobb: 44°. Tethered curve flexibility: 57%. Untethered curve Cobb: 25.1°. TK (T5-T12): 20.8°; LL (L1-S1): -47.5°. Rib hump: N/A. Lumbar prominence: N/A | Tethered curve Cobb: 13.5°a. Tethered curve correction: 70%. Untethered curve Cobb: 7.2°. TK (T5-T12): 21.6°; LL (L1-S1): -54.9°. Successful AVBT: 9 (81.8%) |
The features of the included papers are summarised in Table 1. Seven clinical trials, i.e., one retro-spective comparative study (level III)[22], two prospective observational studies (level IV)[21,23] and four retrospective studies[14,17,20,24], recruiting 163 patients were included in the present review. Only one of the included studies (14.3%) compared the outcomes between patients managed with AVBT and a matched cohort of patients treated with PSF and instrumentation[22]. The number of patients, gender, age, minimum follow-up length, clinical and radiological outcomes at the final follow-up and the successful AVBT rate are reported in Table 1. The patients undergoing AVBT had the following scoliosis pattern distribution, according to Lenke’s classification: Lenke 1 (n = 140; 85.9%), Lenke 2 (n = 10; 6.13%), Lenke 3 (n = 3; 1.84%), Lenke 5 (n = 9; 5.52%), Lenke 6 (n = 1; 0.61%). A total of 151 of 163 AVBT procedures were performed in the thoracic spine, whereas the remaining 12 were in the lumbar spine. Perioperative complications, number of tether revisions and conversion to PSF of the AVBT procedures are reported in Table 2.
| Ref. | Patients (n) | Perioperative complications | Tether revision | Conversion to PSF | ||||
| Type of complication | n of cases (%) | Causes | n of cases (%) | n of revisions (%) | Causes | n of cases (%) | ||
| Miyanji et al[14], 2020 | 57 | Pulmonary. Atelectasis. Pneumonia. Superficial wound infection. Hip and shoulder pain. Numbness in the arm and breast | 3 (5.26). 1 (1.75). 1 (1.75). 1 (1.75). 1 (1.75) | Overcorrection (loosening tether). Tether breakage (replaced). Adding on (extension of tether) | 1 (1.75). 1 (1.75). 1 (1.75) | 1 (1.75). 1 (1.75). 1 (1.75) | Insufficient correction of tethered curve and progression of the deformity. Adding on | 5 (8.77). 1 (1.75) |
| Baker et al[17], 2020 | 17 | N/A | N/A | Broken tether. Other complications | 9 (52.94). 3 (17.7) | 1 (5.88). 3 (17.7) | Overcorrection. Progression of the untethered thoracic curve in a patient with lumbar AVBT | 1 (5.88). 1 (5.88) |
| Hoernschemeyer et al[20], 2020 | 29 | Recurrent pneumothorax. Syncopal episodes (decompression of a Chiari 1 malformation, diagnosed after AVBT) | 1 (3.45). 1 (3.45) | Broken tether. Overcorrection. Adding on | 14 (48.275). 2 (6.9). 1 (3.45) | 3 (10.3): 1 revisio. 2 PSF. 2 (6.9). 1 (3.45) | Progression of the tethered curve after broken tether | 2 (6.9) |
| Pehlivanoglu et al[21], 2020 | 21 | Chylothorax (conservatively managed) | 1 (4.76) | Broken tether | 1 (4.76) | 1 (4.76) | - | - |
| Newton et al[22], 2020 | 23 | Atelectasis with pulmonary oedema (treated with positive airway pressure that resolved by postoperative day 6). Pain radiating down the leg (3 yr postop resolved with physical therapy). Horner syndrome (withasymmetric pupils remaining) | 1 (4.35). 1 (4.35). 1 (4.35) | Broken tether (revision for curve progression). Overcorrection (tether removal, tether replaced with less tension). Progression of the untethered curve. Second revision (broken tether with progression, progression) | 12. 3. 2. 2 | 2 (8.7). 2 (8.7). 1 (4.35). 2 (8.7). 1 (4.35). 1 (4.35) | Curve progression (converted to PSF, indication to PSF, but not yet undergone) | 3 (13). 3 (13) |
| Wong et al[23], 2019 | 5 | Fever. Postop. Nausea. Postop. Vomiting. Postop. Haematuria. Reactive airways. Right pneumothorax. Left/dependent lung pleural effusion. Pneumonia. Conjunctivitis. Trunk listing | 5 (100). 1 (20). 1 (20). 1 (20). 1 (20). 2 (40). 1 (20). 1 (20). 1 (20). 1 (20) | - | - | - | Overcorrection. Curve progression/distal decompensation | 1 (20). 1 (20) |
| Samdani et al[24], 2014 | 11 | Persistent atelectasis (bronchoscopy) | 1 (9.1) | Overcorrection | 2 (18.2) | 2 (18.2) | - | - |
Currently, there is still not a universal consensus on AVBT indications, about Lenke type, curve size and remaining skeletal growth at the time of surgery. Clinical trials showed the features of the ideal patient for vertebral tethering, but the rate of postoperative complications and the lack of long-term results should be carefully considered when recommending AVBT. Krakow et al[30], in a retrospective analysis of 359 patients treated between 2016 and 2019 at a large paediatric centre, showed 75 patients (20.9%) could have been tethered in the years preceding approval FDA approval of AVBT device, by applying the FDA IDE criteria. Nonetheless, all the following points should be carefully assessed before considering this growth-friendly surgical procedure.
AVBT has been used in boys and girls aged mainly from 8 to 16 years. Besides biological age, however, skeletal maturity should be carefully evaluated, to estimate the potential curve progression entity, as well as to allow the asymmetrical modulation of the spinal growth via the Hueter-Volkmann principle. The ideal skeletal age for AVBT is defined by a Risser score[33] of ≤ 2 and a Sanders score[34] of 3-4. It is important to note Sanders score has shown a strong correlation with the probability of curve progression[35], hence it should be always performed in children eligible for AVBT. Indeed, if the vertebral tethering is performed too early, a higher risk of curve overcorrection should be considered. If it is performed in an almost skeletal mature patient, there will not be enough remaining growth, thus leading to the lack of a relevant curve correction and relevant risk of tethering rupture[36].
AVBT has been proposed for idiopathic curves only, since patients with syndromic scoliosis may not respond as predictably, compared with IS. In this kind of patient, the growth of the untethered portion of the spine may be unpredictable, thus potentially increasing the re-intervention rate. Similarly, left-sided thoracic curves are not an absolute contraindication for AVBT, but the surgeon must rule out the presence of a syndromic condition, before recommending AVBT. Finally, the surgeon should be aware the left-sided approach might be high-demanding, from a technical point of view, since segmentary vessels lie closer to the aorta, compared with the right side, thus ligation could be more difficult.
AVBT has been largely studied in idiopathic flexible thoracic curves, Lenke type 1, with a Cobb angle between 35° and 65°, according to FDA IDE criteria[37]. Published and ongoing clinical trials have also focused on other Lenke types, i.e., types 2, 3C and 5[38]; the Cobb angle for lumbar curves should be < 35°. Although lumbar curves are not contraindications for AVBT, this technique has been described for thoracic curves; consequently, particular caution should be taken when performing surgery of the lumbar spine (i.e., open laparotomy or mini-laparotomy could be needed to access the lumbar spine)[39]. Furthermore, as suggested by Newton et al[15], tethering more than one curve potentially reduces the predictability of the outcome. Curve flexibility should be preoperatively assessed on supine bending radiographs; a curve showing a 50% flexibility is an ideal candidate for AVBT[15]. Thoracic kyphosis > 40°[29] is a relative contraindication for AVBT, since this growing-friendly technique, by involving the tethering of the most anterior portion of the spine, could improve the patient’s kyphosis[39]. Finally, a careful preoperative evaluation of the patient’s sagittal profile, spinopelvic and 3D parameters can help reduce the risk of flat back or decreased lordosis[39].
The preoperative workup for patients undergoing AVBT includes upstanding and supine full spine films in anteroposterior and lateral projections, supine bending films and full spine and brain magnetic resonance imaging. Buyuk et al[13], in a retrospective study recruiting 51 patients, confirmed preoperative bending radiographs provide a reasonable estimate of postoperative correction for patients undergoing AVBT. An increase of the major Cobb angle, however, is expected on first upstanding spine radiographs, compared to intraoperative X-rays. Spine levels are typically instrumented from upper to lower vertebra; tension should be applied on the tether, to bring the tilted discs into neutral alignment where possible[14].
AVBT should be carried out using a strict lateral decubitus position, with the convex side of the thoracic deformity facing upward, on a radiolucent table. The patient is induced under general anaesthesia, using a double-lumen endotracheal tube, thus allowing the anaesthetist to deflate the right lung (or left lung, in presence of left-sided thoracic curves) during the procedure, to access the anterior thoracic vertebral bodies. Care should be taken to protect the brachial plexus by placing a soft gel roll under the axilla[39]. The right arm should be placed on an armrest, and a soft gel pad should be used to protect the ulnar nerve. The patient is finally secured with tape. Intraoperative neuromonitoring, with somatosensory evoked potential and transcranial motor evoked potentials should be used to monitor spinal cord function during surgery and assess upper and lower extremities. All the vertebral bodies to be instrumented should be identified under fluoroscopic guidance and marked on the skin. The right lung (left lung in left-sided thoracic curves) should be deflated by the anaesthetist before starting surgery. After standard skin preparation and draping, anterior surgical access is performed; thoracoscopic, mini-open and traditional open access have been described.
Although video-assisted thoracoscopy surgery (VATS) usually allows vertebral instrumentation from T4 to L2, in some cases, the diaphragmatic attachments may make the instrumentation of the vertebrae distally to T12 more technically demanding. An additional open or mini-open retroperitoneal approach is usually needed to instrument the vertebrae distally to L2. VATS is generally performed using two anterior viewing portals of 1 cm in length, placed on the anterior axillary line, and two/three posterior instrumentation portals of about 3 cm in length, placed on the posterior axillary line, overlying the vertebral bodies.
In deep dissection, the parietal pleura is opened over the spine and segmental vessels should be ligated on the convex side. Once vertebral dissection and exposure are completed, under fluoroscopic guidance, a staple and a bicortical screw are implanted in each instrumented vertebra. The entry point for the staple and the screw is just anterior to the rib head in the vertebral body. After completing all levels of instrumentation, the polyethylene cable is installed. Tension on the cable is applied on each instrumented level; care should be taken to maximally tighten the tether at the curve apex, while minimal tension should be applied at the upper and lower instrumented vertebrae, to avoid screw plough and adding-on. However, there is no consensus about the exact amount of tension to be applied.
Before wound closure, the thoracic cavity should be irrigated with saline and accurate haemostasis should be performed. The lung is reinflated, and a chest drainage tube is typically placed and set to suction. All wounds finally undergo layered sutures. The chest tube should be put on suction for 48 h with daily radiographic control; on postoperative day 3, if there is no residual pneumothorax, the tube should be put off suction and then removed on postoperative day four.
The clinical success of AVBT is defined as the achievement of a nonprogressive scoliosis curve - i.e., Cobb angle < 35° - at skeletal maturity, avoiding PSF. Patients who needed one or more revision procedures were considered successful if they finally presented a stable curve at skeletal maturity. Only 117 of 163 (71.8%) patients carried out a nonprogressive curve at skeletal maturity. The success rate of AVBT also showed a wide heterogeneity in the analysed studies, ranging from 52%[22] to 95.24%[21].
A postoperative complication rate of 17.8% was observed, and complications were also observed in patients that achieved a successful outcome at skeletal maturity. Postoperative complications included pulmonary complications (n = 12; 7.4%), including atelectasis (n = 5; 3.07%), pneumonia (n = 2; 1.23 %), pneumothorax (n = 4; 2.45%) and chylothorax (n = 1; 0.6%). All these complications were successfully managed conservatively.
Twenty-three of 163 (14.11%) patients required unplanned revision surgery within the follow-up period. The main indications for AVBT revision were: Curve overcorrection (n = 11; 6.75%); broken tether with curve progression (n = 8; 4.9%); adding-on (n = 2; 1.23%); and progression of the untethered curve (n = 2; 1.23%). Overcorrection was defined by a reduction of the preoperative Cobb angle progressing beyond the neutral axis, and was recorded as a negative number. Broken tethers, identified as a change in screw angulation > 5° on consecutive standing spine radiographs, were not an indication for revision surgery. A re-intervention was needed when curve progression was detected because of the tether breakage. Adding-on, i.e., postoperative loss of correction due to curve progression, was managed with tether extension.
Untethered curve progression is another concern of AVBT. Hoernschemeyer et al[20] described the combined use of thoracic tether and lumbar brace in eight patients with larger main thoracic curves and smaller lumbar curves. In this subset of patients, a significant decrease in all the three measured curves, from preoperatively to the latest postoperative follow-up was observed[20]. This therapeutic strategy, combining thoracic AVBT with a lumbar brace, could be useful in the management of scoliosis in growing children.
Conversion to PSF was performed in 18 of 163 (11%) patients during follow-up. In these patients, AVBT gave no significant advantages, since the patients could not avoid PSF surgery, within 24-mo after tethering.
PSF and instrumentation is the gold standard for the treatment of patients with scoliotic curves > 45°[40,41]. Newton et al[22] in a retrospective comparative study, have recently compared outcomes of patients with immature IS, who underwent AVBT, with those of a matched cohort of patients treated with PSF, at a minimum 24-mo follow-up. Although the post-intervention patient-reported outcomes (PROMs) were similar in both groups, at the final follow-up, the AVBT group had a significantly higher residual deformity, compared with patients receiving PSF (P < 0.001). In the AVBT cohort, only 52% of patients were successful in having curves of < 35° at skeletal maturity. In the PSF cohort, no patient needed revision surgery, whereas in the AVBT group, five of 23 (21.74%) patients underwent one AVBT revision and the other two patients (8.7%) needed two AVBT revisions procedures. A broken tether was observed in 12 of 23 (52%) patients. Three of 23 patients needed surgical conversion to PSF and an additional three were indicated for PSF, but they had not yet undergone PSF within the study period (overall conversion rate to PSF: 26%). Finally, the proposed advantages of tethering, including progressive postoperative curve correction and maintenance of spinal motion, were not demonstrated in the AVBT group.
AVBT is a promising emerging technique for the surgical treatment of IS in growing patients[36]. It mainly aims for 3D correction of the scoliotic deformity, without reverting to spinal fusion or delaying the need for PSF[15,36]. In 2019, the first instrumentation system for AVBT received FDA clearance, under a Humanitarian Device Exemption, based on the results of a Phase 2A pilot study, performed by Wong et al[23]. Although AVBT has shown encouraging results in the treatment of IS in growing patients, there is a paucity of published data about this growth-friendly procedure and long-term results are not yet available. This systematic review aimed to summarise current evidence about the efficacy and safety of AVBT in the management of IS in skeletally immature patients.
Although there is still not a universal consensus on AVBT indications, clinical trials have shown the features of the ideal patient for vertebral tethering, i.e., a skeletally immature patient, with a primary and flexible idiopathic thoracic curve. More recent clinical studies[14,17,20] have also investigated the role of AVBT in scoliosis patterns other than Lenke 1. Baker et al[17] in a retrospective study analysing the results of 19 AVBT procedures performed in 17 patients, compared 13 thoracic AVBT procedures to lumbar ones. The two groups had comparable demographic features in terms of gender, body mass index and skeletal age. These authors observed in lumbar AVBTs a greater immediate percentage correction and a higher correction rate per level per month compared with the thoracic cohort. Nonetheless, one revision procedure only (8%) was performed in the thoracic group, whereas three revision surgical procedures were needed in lumbar AVBT (50%).
Hoernschemeyer et al[20] in a retrospective study recruiting 29 patients, identified five distinct subgroups of skeletally immature patients, each receiving different treatments. Patients with a single, main thoracic curve received thoracic AVBT only. In these patients, the structural curve and both compensatory curves demonstrated continued postoperative improvement and achieved good control at the final follow-up[20]. Patients receiving thoracic AVBT and a lumbar brace also showed postoperative improvement of both curves[20]. Similar findings were observed in patients with left thoracolumbar curves and those with large main thoracic and lumbar curves treated with a combined thoracic and lumbar AVBT[20]. Finally, patients with a long thoracic curve received a single tether and exhibited a decrease in the main thoracic curve at the latest follow-up[20]. The last subgroup of patients, however, should be monitored over time since they have the largest number of consecutive levels tethered[20].
The anterior approach to the spine needed in the vertebral tethering could be another concern. In the last decades, posterior approaches have largely replaced the anterior access to the spine, therefore several surgeons have not been trained to perform an anterior approach to the spine. However, Baroncini et al[18] in a retrospective study that recruited 90 patients, have recently observed that AVBT has a rapid learning curve. These authors showed intubation time and surgical time per screw decrease by > 50% for each treated patient; the estimated blood loss per screw decreased by 66% for each surgical procedure; and intubation and hospitalization decreased by 32%.
Despite AVBT being a promising growth-friendly surgical procedure, endowed with several potential advantages, it has still a lower success rate and a higher complication rate compared with PSF. Hence, the gathered data of the studies included showed AVBT was successful only in 117 of 163 (71.8%) patients. Moreover, 23 of 163 (14.11%) patients required unplanned revision surgery and 18 of 163 (11%) patients needed conversion to PSF within the follow-up period. A postoperative complication rate of 17.8% was also observed in the studies included in the present review.
This is, to the best of our knowledge, the first systematic review to investigate the effectiveness and safety of AVBT in the management of IS in growing children. The main limitation of the present study was the low level of evidence of the included studies, since no randomised clinical trials have been published on AVBT. Currently, six ongoing clinical trials are available on Clinicaltrials.gov[42]: Four prospective clinical trials focusing on AVBT and one prospective comparative nonrandomised and one randomised clinical trial are aiming to compare AVBT to PSF. The ongoing and future studies should confirm the surgical criteria for AVBT, prove tethering long-term effectiveness and safeness, focus on PROMs, and propose strategies to avoid perioperative complications and long-term implant failures. A more durable, fatigue-resistant cable should be also developed to prevent the high number of broken tethers observed in the published studies.
The analysis of the literature included in this systematic review showed that AVBT is a promising growth-friendly technique for the treatment of IS in growing patients. However, AVBT has a moderate success rate and has perioperative complications, revision and conversion to PSF. Future level I studies, with long-term follow-up, are needed to define the limits and potentials of this emerging surgical technique.
Anterior vertebral body tethering (AVBT) was originally described in 2010 by Crawford and Lenke[16], who reported the first case of an 8-year-old child, with a 40° right thoracic curve successfully managed with this growth-friendly technique. In 2019, the US Food and Drug Administration approved the first instrumentation system for AVBT, under a Humanitarian Device Exception, for skeletally immature patients with curves having a Cobb angle between 35° and 65°. However, some controversies still exist in this emerging surgical technique.
This systematic review was designed to summarise current evidence about the efficacy and safety of AVBT in the management of idiopathic scoliosis in skeletally immature patients.
The objectives of this systematic review were: (1) To assess the success of AVBT at a minimum 24-mo follow-up; (2) To identify the rate of perioperative complications, re-interventions and conversions to posterior spinal fusion (PSF), in patients who underwent AVBT; and (3) To identify the correct indications for AVBT.
The search of electronic databases was performed to identify relevant clinical studies, dealing with AVBT, for further analysis. A total of 107 studies were identified, but only seven of these were included in the present review.
The pooled data of seven studies with 163 patients showed that AVBT was successful only in 117 patients (71.8%). Moreover, 23 patients (14.11%) required unplanned revision surgery and 18 (11%) needed conversion to PSF within the follow-up period. A postoperative complication rate of 17.8% was also observed.
AVBT is a promising growth-friendly technique for the treatment of idiopathic scoliosis in growing patients. However, AVBT has a moderate success rate has perioperative complications, revision and conversion to PSF.
Future studies should confirm the surgical criteria for AVBT, prove tethering long-term effectiveness and safety, focus on patient-reported outcomes measures, and propose strategies to avoid perioperative complications and long-term implant failures. A more durable, fatigue-resistant cable should be developed to prevent the high number of broken tethers observed in the published studies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Speciality type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Muthu S, India S-Editor: Wang JJ L-Editor: Kerr C P-Editor: Wang JJ
| 1. | Akbarnia BA. Management themes in early onset scoliosis. J Bone Joint Surg Am. 2007;89 Suppl 1:42-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Williams BA, Matsumoto H, McCalla DJ, Akbarnia BA, Blakemore LC, Betz RR, Flynn JM, Johnston CE, McCarthy RE, Roye DP Jr, Skaggs DL, Smith JT, Snyder BD, Sponseller PD, Sturm PF, Thompson GH, Yazici M, Vitale MG. Development and initial validation of the Classification of Early-Onset Scoliosis (C-EOS). J Bone Joint Surg Am. 2014;96:1359-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 204] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 3. | Ruf M, Drumm J, Jeszenszky D. Anterior instrumented fusion for adolescent idiopathic scoliosis. Ann Transl Med. 2020;8:31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Piazzolla A, Bizzoca D, Solarino G, Brayda-Bruno M, Tombolini G, Ariagno A, Moretti B. Maria Adelaide brace in the management of Scheuermann's Kyphosis. Spine Deform. 2021;9:549-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Hawary RE, Zaaroor-Regev D, Floman Y, Lonner BS, Alkhalife YI, Betz RR. Brace treatment in adolescent idiopathic scoliosis: risk factors for failure-a literature review. Spine J. 2019;19:1917-1925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 6. | Halsey M, Dolan LA, Hostin RA, Adobor RD, Dayer R, Dema E, Letaif OB. Scoliosis Research Society survey: brace management in adolescent idiopathic scoliosis. Spine Deform. 2021;9:697-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Dimeglio A, Canavese F. The immature spine: growth and idiopathic scoliosis. Ann Transl Med. 2020;8:22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Skaggs DL, Akbarnia BA, Flynn JM, Myung KS, Sponseller PD, Vitale MG; Chest Wall and Spine Deformity Study Group; Growing Spine Study Group; Pediatric Orthopaedic Society of North America; Scoliosis Research Society Growing Spine Study Committee. A classification of growth friendly spine implants. J Pediatr Orthop. 2014;34:260-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 145] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 9. | Jeszenszky D, Kaiser B, Meuli M, Fekete TF, Haschtmann D. Surgical growth guidance with non-fused anchoring segments in early-onset scoliosis. Eur Spine J. 2019;28:1301-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | McCarthy RE, Luhmann S, Lenke L, McCullough FL. The Shilla growth guidance technique for early-onset spinal deformities at 2-year follow-up: a preliminary report. J Pediatr Orthop. 2014;34:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Cuddihy L, Danielsson AJ, Cahill PJ, Samdani AF, Grewal H, Richmond JM, Mulcahey MJ, Gaughan JP, Antonacci MD, Betz RR. Vertebral Body Stapling versus Bracing for Patients with High-Risk Moderate Idiopathic Scoliosis. Biomed Res Int. 2015;2015:438452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Floman Y, El-Hawary R, Lonner BS, Betz RR, Arnin U. Vertebral growth modulation by posterior dynamic deformity correction device in skeletally immature patients with moderate adolescent idiopathic scoliosis. Spine Deform. 2021;9:149-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Buyuk AF, Milbrandt TA, Mathew SE, Potter DD, Larson AN. Does preoperative and intraoperative imaging for anterior vertebral body tethering predict postoperative correction? Spine Deform. 2021;9:743-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Miyanji F, Pawelek J, Nasto LA, Rushton P, Simmonds A, Parent S. Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Joint J. 2020;102-B:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 15. | Newton PO. Spinal growth tethering: indications and limits. Ann Transl Med. 2020;8:27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 16. | Crawford CH 3rd, Lenke LG. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am. 2010;92:202-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 17. | Baker CE, Kiebzak GM, Neal KM. Anterior vertebral body tethering shows mixed results at 2-year follow-up. Spine Deform. 2021;9:481-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 18. | Baroncini A, Trobisch PD, Migliorini F. Learning curve for vertebral body tethering: analysis on 90 consecutive patients. Spine Deform. 2021;9:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 19. | Baroncini A, Rodriguez L, Verma K, Trobisch PD. Feasibility of Single-Staged Bilateral Anterior Scoliosis Correction in Growing Patients. Global Spine J. 2021;11:76-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Hoernschemeyer DG, Boeyer ME, Robertson ME, Loftis CM, Worley JR, Tweedy NM, Gupta SU, Duren DL, Holzhauser CM, Ramachandran VM. Anterior Vertebral Body Tethering for Adolescent Scoliosis with Growth Remaining: A Retrospective Review of 2 to 5-Year Postoperative Results. J Bone Joint Surg Am. 2020;102:1169-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 120] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 21. | Pehlivanoglu T, Oltulu I, Ofluoglu E, Sarioglu E, Altun G, Korkmaz M, Yildirim K, Aydogan M. Thoracoscopic Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: A Minimum of 2 Years' Results of 21 Patients. J Pediatr Orthop. 2020;40:575-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 22. | Newton PO, Bartley CE, Bastrom TP, Kluck DG, Saito W, Yaszay B. Anterior Spinal Growth Modulation in Skeletally Immature Patients with Idiopathic Scoliosis: A Comparison with Posterior Spinal Fusion at 2 to 5 Years Postoperatively. J Bone Joint Surg Am. 2020;102:769-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 115] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 23. | Wong HK, Ruiz JNM, Newton PO, Gabriel Liu KP. Non-Fusion Surgical Correction of Thoracic Idiopathic Scoliosis Using a Novel, Braided Vertebral Body Tethering Device: Minimum Follow-up of 4 Years. JB JS Open Access. 2019;4:e0026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976). 2014;39:1688-1693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 155] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 25. | ROAF R. Vertebral growth and its mechanical control. J Bone Joint Surg Br. 1960;42-B:40-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 152] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Newton PO, Upasani VV, Farnsworth CL, Oka R, Chambers RC, Dwek J, Kim JR, Perry A, Mahar AT. Spinal growth modulation with use of a tether in an immature porcine model. J Bone Joint Surg Am. 2008;90:2695-2706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Newton PO, Farnsworth CL, Faro FD, Mahar AT, Odell TR, Mohamad F, Breisch E, Fricka K, Upasani VV, Amiel D. Spinal growth modulation with an anterolateral flexible tether in an immature bovine model: disc health and motion preservation. Spine (Phila Pa 1976). 2008;33:724-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Newton PO, Fricka KB, Lee SS, Farnsworth CL, Cox TG, Mahar AT. Asymmetrical flexible tethering of spine growth in an immature bovine model. Spine (Phila Pa 1976). 2002;27:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24:1533-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 30. | Krakow AR, Magee LC, Cahill PJ, Flynn JM. Could have tethered: predicting the proportion of scoliosis patients most appropriate for thoracic anterior spinal tethering. Spine Deform. 2021;9:1005-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13335] [Article Influence: 833.4] [Reference Citation Analysis (0)] |
| 32. | AAOS. AAOS Clinical Practice Guideline and Systematic Review Methodology. [cited 20 January 2021]. Available from: https://aaos-app-prod-aaoswww01.azurewebsites.net/uploadedFiles/PreProduction/Quality/Guidelines_and_Reviews/Guideline%20and%20Systematic%20Review%20Processes_v4.0_Final8cd7.pdf?_ga=2.244485197.938110896.1540216238-29030028.1531151248. |
| 33. | Risser JC, Brand RA. The iliac apophysis: An invaluable sign in the management of scoliosis. Clinical Orthopaedics and Related Research. 2010;468:646-653. |
| 34. | Sanders JO, Khoury JG, Kishan S, Browne RH, Mooney JF 3rd, Arnold KD, McConnell SJ, Bauman JA, Finegold DN. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90:540-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 264] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 35. | Sitoula P, Verma K, Holmes L Jr, Gabos PG, Sanders JO, Yorgova P, Neiss G, Rogers K, Shah SA. Prediction of Curve Progression in Idiopathic Scoliosis: Validation of the Sanders Skeletal Maturity Staging System. Spine (Phila Pa 1976). 2015;40:1006-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 36. | Senkoylu A, Riise RB, Acaroglu E, Helenius I. Diverse approaches to scoliosis in young children. EFORT Open Rev. 2020;5:753-762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 37. | Cahill P. Vertebral Body Tethering Outcomes for Pediatric Idiopathic Scoliosis. In: ClinicalTrials.gov. [accessed 2021 Jan 20]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/NCT03194568 ClinicalTrials.gov Identifier: NCT03194568. |
| 38. | Larson NA. Anterior Vertebral Body Tethering (AVBT) Using Zimmer Biomet Tether System or Dynesys System Components to Treat Pediatric Scoliosis. Available from: https://clinicaltrials.gov/ct2/show/NCT03506334 ClinicalTrials.gov Identifier: NCT03506334. |
| 39. | Parent S, Shen J. Anterior Vertebral Body Growth-Modulation Tethering in Idiopathic Scoliosis: Surgical Technique. J Am Acad Orthop Surg. 2020;28:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 40. | Piazzolla A, Montemurro V, Bizzoca D, Parato C, Carlucci S, Moretti B. Accuracy of plain radiographs to identify wrong positioned free hand pedicle screw in the deformed spine. J Neurosurg Sci. 2019;63:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Piazzolla A, Bizzoca D, Solarino G, Parato C, Moretti B. Plasma Technology Reduces Blood Loss in Adolescent Idiopathic Scoliosis Surgery: A Prospective Randomized Clinical Trial. Global Spine J. 2021;11:874-880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Clinicaltrials.gov. Clinicaltrials.org: search for “Anterior Vertebral Body Tethering” [cited 20 January 2021]. Available from: https://www.clinicaltrials.gov/ct2/results?cond=tethering+scoliosis&term=&cntry=&state=&city=&dist=. |