Published online Feb 18, 2022. doi: 10.5312/wjo.v13.i2.131
Peer-review started: June 11, 2021
First decision: July 28, 2021
Revised: August 5, 2021
Accepted: January 13, 2022
Article in press: January 13, 2022
Published online: February 18, 2022
Processing time: 252 Days and 6.2 Hours
Tillaux fractures occur primarily in adolescents due to the pattern of physeal closure and are classified as Salter-Harris type III physeal fractures. Operative management with screw fixation is recommended for more than 2 mm of displacement or more than 1 mm of translation. However, the efficacy and complications of trans-physeal vs all-physeal screw fixation have not been investigated extensively.
To compare the clinical and functional outcomes of trans-physeal (oblique) and all-epiphyseal (parallel) screw fixation in management of Tillaux fractures among pediatric patients.
This was an ethics board approved retrospective review of pediatric patients who presented to our tertiary children’s care facility with Tillaux fractures. We included patients who had surgical fixation of a Tillaux fracture over a 10 year period. Data analysis included demographics, mode of injury, management protocols, and functional outcomes. The patients were divided into group 1 (oblique fixation) and group 2 (parallel fixation). Baseline patient characteristics and functional outcomes were compared between groups. Statistical tests to evaluate differences included Fisher’s Exact or Chi-squared and independent samples t or Mann Whitney tests for categorical and continuous variables, respectively.
A total of 42 patients (28 females and 14 males) were included. There were no significant differences in body mass index, sex, age, or time to surgery between the groups [IK2]. Sports injuries accounted for 61.9% of the cases, particularly non-contact (57.1%) and skating (28.6%) injuries. Computed Tomography (CT) scan was ordered for 28 patients (66.7%), leading to diagnosis confirmation in 17 patients and change in management plan in 11 patients. [GRC3] Groups 1 and 2 consisted of 17 and 25 patients, respectively. For mid to long-term functional outcomes, there were 14 and 10 patients in groups 1 and 2, respectively. Statistical analysis revealed no significant differences in the functional outcomes, pain scores, or satisfaction between groups. No infections, non-unions, physeal arrest, or post-operative ankle deformities were reported. Two (4.8%) patients had difficulty returning to sports post-surgery due to pain. One was a dancer, and the other patient had pain while running, which led to hardware removal. Both patients had parallel fixation. Hardware removal for groups 1 and 2 were 4 (23.5%) and 5 (20.0%) patients, respectively. The reasons for removal was pain in 2 patients, and parental preference in the remaining.
This is the largest reported series of pediatric patients with Tillaux fractures comparing functional outcomes of different methods of screw fixation orientation to the physis, which showed no difference regarding functional outcomes.
Core Tip: Tillaux fractures that require surgery can undergo screw fixation by all-epiphyseal or trans-epiphyseal techniques. This study shows that there were no statistically significant differences between the functional outcomes or complications between the two techniques. Therefore, we suggest using the trans-epiphyseal techniques because it has an easier screw trajectory in surgery, all-epiphyseal screws have been shown to increase pressure in the tibiotalar joint, and the trajectory is trigonometrically a better angle to compress the fracture.
- Citation: Heldt B, Roepe I, Guo R, Attia E, Inneh I, Shenava V, Kushare I. All-epiphyseal versus trans-epiphyseal screw fixation for tillaux fractures: Does it matter? World J Orthop 2022; 13(2): 131-138
- URL: https://www.wjgnet.com/2218-5836/full/v13/i2/131.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i2.131
Tillaux fracture is an avulsion fracture of the anterolateral distal tibial epiphysis that occurs primarily in adolescents due to the pattern of physeal closure, and is classified as a Salter-Harris type III physeal fracture[1]. They occur most commonly in children near skeletal maturity at around ages 12-14 years old during the period of distal tibial physis closure, with supination-external rotation being the typical mechanism of injury. In children, the cartilaginous physes are more susceptible to injury than the surrounding tissues, leading to bone failure prior to the failure of ligamentous attachments. The physis initially closes centrally, then medially, and finally laterally, giving rise to the anterolateral location of the Tillaux fracture[2]. In the Tillaux fracture pattern, this manifests as an avulsion of the distal lateral tibial epiphysis at the site of attachment of the anterior inferior tibiofibular ligament where the physis is still cartilaginous and weaker than the ligament[3].
Ankle fractures account for approximately 5% of all pediatric fractures and 15% of all injuries involving a physis[4]. Tillaux fractures specifically account for 3%-5% of all pediatric ankle fractures[5,6], and the amount of data in the literature on these fractures is limited. Operative management with screw fixation is recommended for fractures with more than 2 mm of displacement or more than 1 mm of translation[2]. Fixation can be performed by an all-epiphyseal (parallel) or trans-physeal (oblique) screw orientation. Traditional treatment of this injury involved all–epiphyseal screw fixation (parallel to the ankle joint line) because it avoids the open physis, theoretically preventing growth arrest. However, a previous cadaveric study showed that parallel screw fixation can lead to increased joint pressures[7], potentially altering ankle joint biomechanics and increasing the risk of arthritis and complications in the long term[8]. Oblique screws may have an easier to achieve intra-operative trajectory, serve as a better fixation construct as they are relatively more perpendicular to the fracture line, and would not lead to increased pressure in the ankle joint articular cartilage.
To our knowledge, the efficacy (including functional outcomes) and complications of oblique vs parallel screw fixation for Tillaux fractures have not yet been investigated in the literature. This study aims to compare the healing and functional outcomes of both fixation techniques. We hypothesized that oblique fixation would result in no differences in bone healing, complications, or functional outcomes compared to parallel fixation.
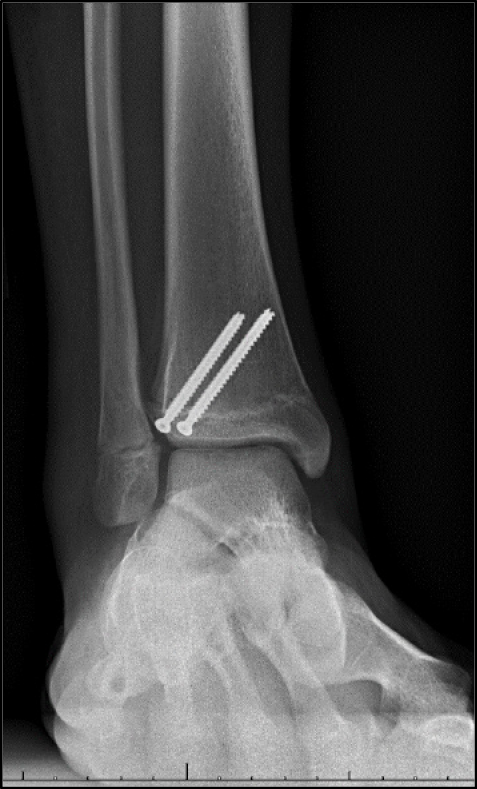
This cohort study was conducted at a single-center following institution review board approval. All patients under 18 years old who underwent surgical fixation of Tillaux fractures between January 2010 and March 2020 were included in the study. Patients were excluded if they had underlying conditions interfering with either bone physiology, anatomy, or healing, such as cerebral palsy, osteogenesis imperfecta, etc. Patients were stratified into two groups based on the screw fixation technique: Group 1 consisted of patients with oblique (trans-physeal) fixation (Figure 1), and group 2 consisted of patients with parallel to the ankle (all-epiphyseal) fixation (Figure 2). Screw fixation technique was determined by a review of operative notes and post-operative radiographs.
Patients’ charts were reviewed for the following data: Age, sex, body mass index (BMI), mechanisms of injury (Sports Contact, Sports Non-Contact, Motor Vehicle Collision [MVC], Non-Sports related Fall, and Other), radiographs and advanced imaging, and time to surgery. Complications such as physeal/growth arrest, deformity of the ankle at follow-up, revisions/hardware removal, and infections were analyzed. Functional outcomes were obtained at a minimum of 1 year post-operatively and included the Oxford Ankle Foot Questionnaire for Children (OxAFQ-C) score, Single Assessment Numeric Evaluation (SANE) score, Visual Analog Scale (VAS) pain scores, and patient satisfaction. Satisfaction was set as a binary variable, with answers categorized as satisfied or dissatisfied.
Baseline patient characteristics, complications and functional outcomes were compared between groups. Statistical tests to evaluate differences included Fisher’s Exact or Chi-squared and independent samples t or Mann Whitney tests for categorical and continuous variables, respectively. Normality assessments were conducted using the Kolmogorov-Smirnov test for all continuous variables. All statistical analyses were performed and reviewed by BH and IAI trained in these techniques using IBM SPSS Statistics V.27.0 (IBM Corp, Armonk, NY). The P value was set at < 0.05 for statistical significance. Results are reported as counts with corresponding percentages or means with standard deviation.
A total of 42 patients (28 females and 14 males) were included in the analysis. There were no significant differences in BMI, sex, age, or time-to-surgery between the groups (Table 1). Sports injuries accounted for 61.9% of all injuries, particularly non-contact (57.1%) and skating (28.6%) (Table 2). However, there were no significant differences between groups. A CT scan was ordered for 28 patients (66.7%), which led to 11 patients (26.2%) changing treatment plan from non-operative treatment to surgery, and the remaining led to the confirmation of surgical management.
| Variable | Total Sample (n = 42) | Oblique (n = 17) | Parallel (n = 25) | P value |
| Sex | ||||
| Female | 28 (66.7) | 13 (76.5) | 15 (60.0) | 0.27 |
| Male | 14 (33.3) | 4 (23.5) | 10 (40.0) | |
| Age (yr.) | 13.5 ± 1.4 | 13.4 ± 1.7 | 13.6 ± 1.2 | 0.43 |
| Body mass index (lbs/m2) | 26.3 ± 6.4 | 26.2 ± 4.5 | 26.4 ± 7.3 | 0.93 |
| Time-to-surgery (d) | 7.6 ± 9.6 | 6.9 ± 4.7 | 8.0 ± 11.8 | 0.38 |
| Factor | Total sample (n = 42) | Oblique (n = 17) | Parallel (n = 25) | P value |
| Sports | 26 (61.9) | 11 (64.7) | 15 (60.0) | 1.00 |
| Skating | 12 (28.6) | 7 (41.2) | 5 (20.0) | 0.17 |
| Contact | 3 (7.1) | 1 (5.9) | 2 (8.0) | 1.00 |
| Non-contact | 24 (57.1) | 10 (58.8) | 14 (56.6) | 0.86 |
| Motor vehicle collision | 0 | 0 | 0 | - |
| Fall | 10 (23.8) | 3 (17.6) | 7 (28.0) | 0.49 |
Groups 1 and 2 consisted of 17 and 25 patients, respectively. Functional outcomes were available for 14 (82.4%) and 10 (40.0%) patients in groups 1 and 2, respectively. The average follow-up for the long-term outcomes was 3.5 (± 2.8) years. Statistical analysis revealed no statistically significant differences in functional outcomes between groups (Table 3). No infections, non-unions, physeal arrest, or post-operative ankle deformities were reported. Two patients had difficulty returning to sports post-surgery due to pain (1 from each group). One was a dancer, and the other patient had pain while running, which resulted in hardware removal. Hardware removal occurred for 4 and 5 patients in groups 1 and 2, respectively. The reason for removal was the persistence of pain in 2 patients (1 from each group), and parental preference in the remaining.
| Variable | Oblique (n = 14) | Parallel (n = 10) | P value |
| SANE score (0-100) | 90 ± 18.58 | 88.5 ± 16.3 | 0.86 |
| Pain score (0-10) | 1.8 ± 1.7 | 1.7 ± 1.9 | 0.61 |
| Oxford score (0-100) | |||
| Physical scale score | 76.2 ± 20.6 | 82.5 ± 20.95 | 0.70 |
| School and play scale score | 91.5 ± 14.6 | 93.8 ± 13.5 | 0.67 |
| Emotional scale score | 91.5 ± 14.6 | 96.9 ± 7.9 | 0.36 |
| Satisfaction | |||
| Satisfied | 13 (92.9) | 10 (100) | 1.00 |
| Dissatisfied | 1 (7.1) | 0 |
Our study assessed the functional outcomes of Tillaux fracture patients, and compared them based on screw fixation technique (oblique vs parallel). The results suggest no differences in the SANE, VAS and Oxford scores, or patient satisfaction. These findings support our hypothesis that there would not be any differences between the two groups.
The radiographic cutoffs for surgical or non-surgical management of Tillaux fractures is generally recognized as more than 2 mm of displacement or greater than 1 mm of translation[9]. Liporace et al[10] questioned the efficacy of CT scans in this patient population because the addition of CT scans did not significantly change the impression of the amount of displacement per case. However, it did influence the decision to operate as seen in our cohort, as 40% of the patients who underwent CT scans were changed to surgical management.
During surgery, the fracture can be fixed with a screw in oblique or parallel orientation relative to the tibiotalar joint. The oblique fixation technique involves placing a screw directly through the Tillaux fragment and ending in the metaphysis, which violates the physis[6,11,12]. Lintecum et al[13] described a parallel fixation technique that involves placing a screw parallel to the tibiotalar joint, through the Tillaux fragment, and into the distal epiphysis. The rationale of this technique was to avoid interrupting the physis and subsequently, growth potential. However, Crawford et al[14] found that growth interruption rarely occurred in patients who underwent surgical fixation. Another case series has found that obliquely oriented screws did not lead to leg length discrepancy[15]. This is most likely due to imminent physeal closure and the fact that there is little remaining linear growth potential. Further, parallel screws are not ideal because they lead to increased pressure in the joint, fixation is not perpendicular to the physeal fracture line, and the all-epiphyseal trajectory is more challenging to achieve with fear of penetrating the articular cartilage due to proximity.
Charlton et al[7] showed in cadavers that parallel screw fixation led to a statistically significant increase of forces in the tibiotalar joint following fixation and that the increase in force disappeared following removal of the screw. Theoretically, increased joint pressures can lead to altered joint biomechanics and associated complications such as arthritis over time. However, there are no long-term studies following surgical fixation of Tillaux fractures to prove this.
In normal ankle fractures, hardware removal is a controversial topic and generally left up to surgeon preference[16]. Some studies have shown negative outcomes with leaving in the screws[17], and Jung et al showed that functional outcomes and pain improve with removal[18]. The negative outcomes of parallel screw fixation could be avoided if an oblique screw trajectory led to less post-operative pain, decreased joint pressures and associated complications, and similar functional outcomes compared to parallel screw fixation. As the Tillaux fragment is avulsed from the anterolateral corner of the distal tibia, a parallel screw does not sit perpendicular to the fracture (Figure 1), which could lead to worse fixation compared to an oblique screw which could instead be placed perpendicular to the fracture line.
Multiple small studies have examined the functional outcomes of surgically treated Tillaux fractures and have found excellent outcomes[2,19-23]. These studies often consisted of a mixture of fixation techniques and did not compare between them. In a study of 7 patients treated with screw fixation (1 patient and 6 patients via open and closed reduction internal fixation, respectively), 6 had full and immediate recovery without complication with a mean Foot and Ankle score of 96.71 out of 100. One patient had pain and joint stiffness in the post-operative period with resolution following conservative management[21]. A study of 23 children with 2-5 mm of displacement following Tillaux fracture reported a mean Foot and Ankle Ability Measure of 91.2% following both open and closed reduction with no difference in outcomes between the two types of management[20]. Another study of 13 adolescent patients with Tillaux fractures treated with a 4 mm partially threaded cancellous screw directed horizontally into the epiphysis via anterolateral approach found radiographical evidence of fracture union in all cases (100%) and a mean Foot and Ankle Score of 97[6]. Another study of 6 children treated with screw fixation found that patients regained complete and painless ankle mobility after a follow-up of 5-7 months[19]. These studies show excellent outcomes but do not compare the two fixation techniques. The fact that most patients have excellent outcomes regardless of the fixation type was the basis of our hypothesis that the oblique screw is most likely an equivalent, if not better, option.
Pilla et al[15] demonstrated that oblique compression screw fixation in 10 patients with an average final follow-up of 15 months resulted in equal leg lengths and no angulation, joint stiffness, or limitations of activities. This study serves to disprove the notion that placing the screw across the physis will have adverse functional and leg length outcomes. Combined with our results of equal functional outcomes, it is evident that patients would only benefit from oblique screws due to previously mentioned reasons as opposed to negative outcomes. However, there is still no data on whether oblique screws lead to increased joint pressures as do parallel screws. There is additionally no data on long-term complications, such as post-operative pain or arthritis, between groups. Our findings of equivalent functional outcomes between screw placement groups validates the need to obtain more information on long-term complications of oblique screw fixation in order to properly evaluate whether this method is equivalent or superior to parallel screw fixation.
Approximately 62% of the Tillaux fracture patients in our cohort were related to sports injuries, with 46% of these sports injuries resulting from skating accidents. We speculate that high and hard booted skates (hockey and roller) may provide a fulcrum at the level of the ankle that leads to increased risk of supination-external rotation type injuries, which is the most common mechanism leading to Tillaux fractures. One study that analyzed injuries sustained while rollerblading found that the ankle was involved in 10% (3rd most) of injuries[24]. All ankle injuries sustained involved a rotational mechanism, and supination-external rotation injuries were associated with high top skates. Thus, an activity that leads to extreme rotation about the ankle and/or a supination-external rotation moment increases the risk of a Tillaux fracture, especially in the appropriate age group[24]. Participation in skating sports and activities (street or ice hockey, roller-blading, roller-skating, etc.) is likely associated with an increased risk of Tillaux fracture compared to other sports.
The limitations of this study are that the patient numbers are relatively small which could lead to the study being underpowered. However, due to the rarity of the injury, our numbers are the largest reported in the literature for this type of comparison. The assignment of patients and perioperative complications were all based on a retrospective review of patient records, which leaves the opportunity for error and misinterpretation. While the type of surgical fixation performed was determined by individual surgeon preference, there was no standardized criteria for assigning patients to undergo either parallel or oblique fixation. [GRC1] In addition, we were only able to contact 57% of the patients for functional outcomes, but these limitations are shared among similar studies on this topic. Despite these limitations, this study is one of the largest studies on Tillaux fractures with mid to long-term outcomes. To our knowledge, it is the only study that has compared functional outcomes based on screw orientation techniques.
In comparing functional outcomes of different methods of screw fixation orientation to the physis, we concluded that there were no differences with a mean follow-up of 3.5 years. This suggests that the oblique fixation is equivalent to parallel fixation; however, more rigorous longitudinal[GRC1] studies are needed to assess long-term complications of oblique screw fixation to further prove superiority.
Operative management of Tillaux fractures in adolescent patients is recommended for more than 2 mm of displacement or more than 1 mm of translation with screw fixation.
The efficacy, superiority and complications of trans-physeal vs all-physeal screw fixation have not been investigated in literature yet.
To compare outcomes of trans-physeal and all-epiphyseal screw fixation in management of Tillaux fractures in young patients.
The patients were divided into group 1 (oblique screw fixation) and group 2 (parallel screw fixation). Patient characteristics and functional outcomes were compared between groups.
A total of 42 patients (28 females and 14 males) were divided into Groups 1 and 2, which consisted of 17 and 25 patients, respectively. Statistical analysis revealed no significant differences in the functional outcomes, pain scores, or satisfaction between groups.
In young patients with Tillaux fractures, comparing functional outcomes of different methods of screw fixation orientation to the physis, showed no difference regarding functional outcomes.
Based on our findings, oblique screws, which provide better compression of the Tillaux fracture, are recommended over parallel screws, which create more joint forces and require a more difficult screw trajectory.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Muthu S S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | Duchesneau S, Fallat LM. The Tillaux fracture. J Foot Ankle Surg. 1996;35:127-33; discussion 189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Ali Al-Ashhab ME, Mahmoud Mohamed AA. Treatment for displaced Tillaux fractures in adolescent age group. Foot Ankle Surg. 2020;26:295-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Wuerz TH, Gurd DP. Pediatric physeal ankle fracture. J Am Acad Orthop Surg. 2013;21:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Kay RM, Matthys GA. Pediatric ankle fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001;9:268-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 62] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula. A retrospective study of two hundred and thirty-seven cases in children. J Bone Joint Surg Am. 1978;60:1046-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 137] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Dias LS, Giegerich CR. Fractures of the distal tibial epiphysis in adolescence. J Bone Joint Surg Am. 1983;65:438-444. [PubMed] |
| 7. | Charlton M, Costello R, Mooney JF 3rd, Podeszwa DA. Ankle joint biomechanics following transepiphyseal screw fixation of the distal tibia. J Pediatr Orthop. 2005;25:635-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Ewalefo SO, Dombrowski M, Hirase T, Rocha JL, Weaver M, Kline A, Carney D, Hogan MV. Management of Posttraumatic Ankle Arthritis: Literature Review. Curr Rev Musculoskelet Med. 2018;11:546-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Gourineni P, Gupta A. Medial joint space widening of the ankle in displaced Tillaux and Triplane fractures in children. J Orthop Trauma. 2011;25:608-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Liporace FA, Yoon RS, Kubiak EN, Parisi DM, Koval KJ, Feldman DS, Egol KA. Does adding computed tomography change the diagnosis and treatment of Tillaux and triplane pediatric ankle fractures? Orthopedics. 2012;35:e208-e212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Gordon JE, Schoenecker PL, Klein SE. Juvenile Tillaux Fractures: A Comparison of Direct and Indirect Fixation. Integr J Orthop Traumatol. 2019;2:1-6. [DOI] [Full Text] |
| 12. | Kling TF Jr, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. J Bone Joint Surg Am. 1984;66:647-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 74] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Lintecum N, Blasier RD. Direct reduction with indirect fixation of distal tibial physeal fractures: a report of a technique. J Pediatr Orthop. 1996;16:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Crawford AH. Triplane and Tillaux fractures: is a 2 mm residual gap acceptable? J Pediatr Orthop. 2012;32 Suppl 1:S69-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Pilla NI, Borusiewicz M, Smith E, Hennrikus WL. Oblique Compression Screw Fixation across the Physis for Tillaux Fractures in Adolescent. J Orthop Sports Med. 2020;2:150-156. [DOI] [Full Text] |
| 16. | Hanson B, van der Werken C, Stengel D. Surgeons' beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. 2008;9:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Böstman O, Pihlajamäki H. Routine implant removal after fracture surgery: a potentially reducible consumer of hospital resources in trauma units. J Trauma. 1996;41:846-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 117] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Jung HG, Kim JI, Park JY, Park JT, Eom JS, Lee DO. Is Hardware Removal Recommended after Ankle Fracture Repair? Biomed Res Int. 2016;2016:5250672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Aguilar Ezquerra A, Monge Vazquez ME, Torralba LG, Angulo Tabernero M. Tillaux fractures: functional results after surgical treatment. Rev Fac Cien Med Univ Nac Cordoba. 2017;74:7-9. [PubMed] |
| 20. | Lurie B, Van Rysselberghe N, Pennock AT, Upasani VV. Functional Outcomes of Tillaux and Triplane Fractures with 2 to 5 Millimeters of Intra-Articular Gap. J Bone Joint Surg Am. 2020;102:679-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Tiefenboeck TM, Binder H, Joestl J, Tiefenboeck MM, Boesmueller S, Krestan C, Schurz M. Displaced juvenile Tillaux fractures : Surgical treatment and outcome. Wien Klin Wochenschr. 2017;129:169-175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Feng SM, Sun QQ, Wang AG, Li CK. "All-Inside" Arthroscopic Treatment of Tillaux-Chaput Fractures: Clinical Experience and Outcomes Analysis. J Foot Ankle Surg. 2018;57:56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Choudhry IK, Wall EJ, Eismann EA, Crawford AH, Wilson L. Functional outcome analysis of triplane and tillaux fractures after closed reduction and percutaneous fixation. J Pediatr Orthop. 2014;34:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Ferkel RD, Mai LL, Ullis KC, Finerman GA. An analysis of roller skating injuries. Am J Sports Med. 1982;10:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |