Published online Nov 18, 2022. doi: 10.5312/wjo.v13.i11.978
Peer-review started: June 23, 2022
First decision: August 22, 2022
Revised: September 6, 2022
Accepted: October 19, 2022
Article in press: October 19, 2022
Published online: November 18, 2022
Processing time: 146 Days and 4.6 Hours
The extensor indicis proprius (EIP) tendon is a frequently used donor for a variety of tendon transfers, most commonly for reconstruction of the extensor pollicis longus (EPL). EIP is known to have frequent anatomic variants including split tendons and variations in tendon arrangement.
To characterize the anatomy of the EIP at the level of the extensor retinaculum, where tendon harvest is often performed, and share our preferred technique for EIP to EPL transfer.
Twenty-nine fresh-frozen cadaveric forearms without history of forearm or hand injury or surgery were dissected. Tendon circumference and relationship of the EIP and extensor digitorum communis to the index (EDCI) at the metacarpophalangeal (MCP) joint and the distal extensor retinaculum were recorded. Distance from the distal extensor retinaculum to the EIP myotendinous junction was measured.
EIP was ulnar to the EDCI in 96.5% of specimens (28/29) at the distal edge of the extensor retinaculum. In the remaining specimen, EIP was volar to EDCI. Tendon circumference at the distal extensor retinaculum averaged (9.3 mm ± 1.7 mm) for EDCI and 11.1 mm (± 2.7 mm) for EIP (P = 0.0010). The tendon circumference at the index MCP joint averaged 11.0 mm (± 1.7 mm) for EDCI and 10.6 mm (± 2.1 mm) for EIP (P = 0.33). EIP had a greater circumference in 76% (22/29) of specimens at the distal extensor retinaculum whereas EIP had a greater circumference in only 31% (9/29) of specimens at the MCP joint.
The EIP tendon is frequently ulnar to and greater in circumference than the EDCI at the distal extensor retinaculum, which can be taken into consideration for tendon transfers involving EIP.
Core Tip: We found that extensor indicis proprius (EIP) was consistently ulnar to extensor digitorum communis to the index in 96.5% of specimens at the distal extensor retinaculum. The EIP had a greater circumference in 76% (22/29) of specimens at the distal extensor retinaculum. This research contributes to the body of knowledge on extensor tendon anatomy and facilitates the smaller incisions and dissection of EIP needed for tendon transfers.
- Citation: Zhou J, Frey C, Segovia N, Yao J. Anatomic relationship of extensor indicis propius and extensor digitorum communis: Implications for tendon transfer. World J Orthop 2022; 13(11): 978-985
- URL: https://www.wjgnet.com/2218-5836/full/v13/i11/978.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i11.978
The extensor indicis proprius (EIP) is a redundant extrinsic extensor of the index finger. It is present in 96.5% of the population and is commonly used for tendon transfers[1]. To correctly harvest the EIP and plan procedural incisions, a thorough understanding of the arrangement of the extensor tendons and their junctural connections is required.
Understanding the variability in anatomic relationships is important when harvesting EIP through a small incision. These variations have been documented in clinical and anatomic studies[2]. The EIP originates from the dorsal aspect of the ulna, the interosseus membrane, and the extensor pollicis longus (EPL) septum[3]. It has the most distal muscle belly of all the extensor tendons, and is the only muscle belly that enters the fourth compartment, under the extensor retinaculum and deep to the extensor digitorum communis (EDC) tendons[1]. Multiple studies have noted that anatomic variants are frequent (10%)[4-7] with regards to arrangement and number of slips. Defining each slip as the presence of independent fascial sheaths at the metacarpal level, the EIP has been cited to have double slips in 16% and triple slips in 7% of cadaveric studies[5]. Gonzalez et al[6] classified the arrangement of EIP and extensor digitorum communis to the index (EDCI) at the metacarpophalangeal (MCP) joint into six types: (1) Single EIP ulnar to a single EDCI; (2) Single EDCI between two slips of EIP; (3) Two slips of EIP ulnar to a single EDCI; (4) Single EIP ulnar to two slips of EDCI; (5) Single EIP radial to a single EDCI; and (6) Single EIP volar to a single EDCI. The most common arrangement is a single EIP inserting ulnar to a single EDCI on the extensor hood in 81%-98.3% of specimens[1,4,6], volar to the EDCI in 10% to 11%[4,5,7], and radial to EDCI in 3%-8%[5]. In other tendon transfers, tendon circumference may also be used as a distinguishing characteristic. Celik et al[8] examined the width and thickness of EDCI and EIP tendons at the level of mid-diaphyseal metacarpal bones and found similar thickness for EDCI and EIP (1.5 mm ± 0.4 mm and 1.47 mm ± 0.38 mm respectively). To our knowledge, no studies have examined the relationship and anatomy of the EIP and EDCI at the level of tendon harvest.
EPL ruptures occur in 0.7% of non-displaced distal radius fractures and 3% of dorsally displaced distal radius fractures[9,10]. Tendon attrition is attributed to friction and compression in the poorly vascularized third compartment between the extensor retinaculum and displaced bone fragments of the dorsal radial tubercle[11]. EIP to EPL transfer is one of the most common tendon transfers in the upper extremity. In addition to anatomic proximity and its redundancy for index finger extension, EIP is synergistic to EPL: The motion of extending the index finger and the thumb interphalangeal (IP) joint is commonly performed together during tasks, allowing patients to recover thumb extension after transfer without extensive relearning. Many techniques exist for harvesting and performing this tendon transfer. The incision for harvest can be made longitudinally or transversely, at the level of the distal or proximal extensor retinaculum, and transfer can occur with two incisions or three with a pulvertaft distal to the retinaculum[12]. Classically described, this tendon transfer has been performed through three incisions: A transverse incision over the MCP joint to transect the ulnar EIP, a longitudinal incision over the thumb metacarpal to dissect out the ruptured tendon and carry out the transfer, and a longitudinal incision at the extensor retinaculum to identify EIP and perform tendon harvest. However, technique adaptations may be considered that use the anatomic relationship of these tendons. We performed a cadaveric study to evaluate the relationship between EDCI and EIP and share our preferred surgical technique for EIP to EPL tendon transfer. We sought to characterize the circumference and relationship of the EIP and EDCI tendons at the distal extensor retinaculum, which is relevant for tendon identification when performing an EPL transfer.
Twenty-nine skeletally mature fresh frozen cadaveric forearms ages 19 to 52 were obtained. Clinical histories confirmed no previous trauma or surgery to the donor. Tendons were defined as independent bands originating from muscle. Tendons were occasionally divided into one or more separable smaller slips at the retinaculum. Individual slips were defined distal to the muscle belly with independent fascial sheaths.
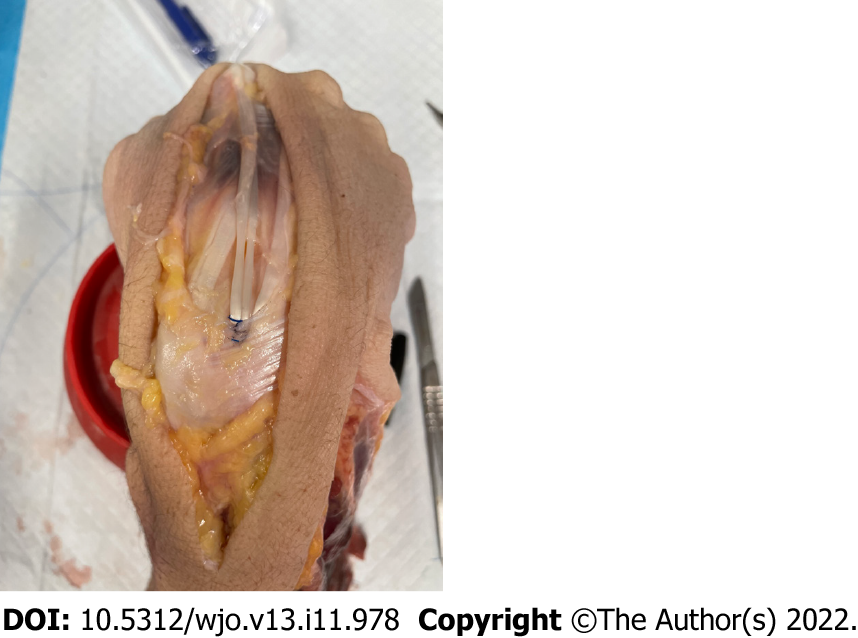
All specimens were dissected with a single dorsal longitudinal incision made just ulnar to Lister’s tubercle extending from the index MCP joint to proximal to the extensor retinaculum. Subcutaneous fat and superficial nerves and veins were elevated in a single flap and tenosynovium was dissected off the EDCI and EIP. The extensor retinaculum was identified as oblique transverse fibers with roughly parallel proximal and distal edges. A 4-0 Prolene suture was used to measure the circumference of the two tendons at the distal edge of extensor retinaculum and the MCP joint (Figure 1) with a single simple knot, and dissection scissors were used to cut the knot at the intersection. The remaining Prolene suture was then measured with a ruler to derive circumference of the tendon. Prolene was chosen for its high intrinsic memory and thus decreased risk for error in measurement of small caliber circumference tendons[13]. The distance in millimeters between the distal edge of the extensor retinaculum and the myotendinous junction of EIP was measured as well. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
To assess our sample with a statistical two-tailed significance of 0.05, power of 80%, and effect size r = 0.6, our a priori power analysis yielded a sample size of 25 was required. Paired t-tests were applied to compare the values obtained from the EIP and EDCI tendon measurements at the distal extensor retinaculum and MCP joint. P < 0.05 was considered to be significant.
Twenty-nine fresh frozen human cadaver forearms were dissected. They were from 20 men and 9 women. The right forearm was dissected in 16 cases and the left in 13 cases. None of the specimens had vascular or nerve variations that were apparent upon dissection. None had evidence of prior surgery to the hand, forearm, or wrist, and clinical histories of the specimens confirmed no history of trauma to the area.
In all but one specimen, the EIP tendon was ulnar to the EDCI tendon (96.5%, 28/29); in the remaining specimen, the EIP was volar to the EDCI. The tendon circumference at the distal edge of the extensor retinaculum averaged 9.3 mm (± 1.7 mm) for the EDCI and 11.1 mm (± 2.7 mm) for the EIP (P = 0.001). The tendon circumference at the index MCP joint was measured to be 11.0 mm (± 1.7 mm) for the EDCI and 10.6 mm (± 2.1 mm) for the EIP (P = 0.331). The EIP had a greater circumference in 76% (22/29) of specimens at the distal extensor retinaculum whereas the EIP had a greater circumference in 31% (9/29) of specimens at the MCP joint. The distance from the distal extensor retinaculum to the myotendinous junction of EIP varied widely but averaged 16.2 mm (± 11.1 mm), which is similar to findings in other studies[11] (Table 1). We did not find significant differences in tendon circumference between specimens of different sex, but overall the tendon circumferences were lower for females as compared to male specimens (Table 2). In addition, the distance between the distal extensor retinaculum to myotendinous junction was lower in female specimens compared to that of males (Table 2); this was also not statistically significant.
| Laterality | Age (yr) | Sex | Circumference at dER (mm) | Circumference at MCP (mm) | EIP distance from dER to myotendinous junction (mm) | Relationship of EIP to EDCI | ||
| cEDCI | cEIP | cEDCI | cEIP | EIP | ||||
| Left | 52 | M | 8 | 15 | 12 | 14 | 29 | EIP ulnar |
| Left | 54 | F | 9 | 10 | 13 | 10 | 15 | EIP ulnar |
| Right | 38 | M | 12 | 13 | 12 | 12 | 16 | EIP ulnar |
| Left | 48 | M | 12 | 15 | 14 | 13 | 15 | EIP ulnar |
| Right | 54 | F | 11 | 11 | 13 | 9 | 14 | EIP ulnar |
| Right | 30 | M | 7 | 8 | 11 | 8 | 20 | EIP ulnar |
| Left | 24 | M | 11 | 12 | 9 | 10 | 18 | EIP ulnar |
| Right | 44 | M | 9 | 14 | 11 | 14 | 23 | EIP ulnar |
| Left | 38 | F | 9 | 8 | 10 | 9 | 27 | EIP ulnar |
| Right | 57 | F | 9 | 12 | 11 | 13 | 18 | EIP ulnar |
| Right | 19 | M | 8 | 9 | 10 | 10 | 2 | EIP ulnar |
| Right | 44 | M | 11 | 13 | 11 | 11 | 37 | EIP ulnar |
| Left | 30 | M | 7 | 5 | 14 | 9 | 22 | EIP ulnar |
| Left | 49 | F | 9 | 13 | 10 | 10 | 4 | EIP ulnar |
| Left | 19 | M | 9 | 9 | 8.5 | 11 | 2 | EIP ulnar |
| Right | 48 | M | 9 | 8 | 9 | 9 | 48 | EIP ulnar |
| Right | 48 | M | 8 | 14 | 12 | 14 | 25 | EIP ulnar |
| Left | 44 | M | 11 | 13 | 12 | 8 | 17 | EIP ulnar |
| Right | 24 | M | 10 | 14 | 13 | 12 | 13 | EIP ulnar |
| Left | 35 | M | 14 | 10 | 14 | 10 | 10 | EIP ulnar |
| Left | 20 | M | 9 | 11 | 10 | 8 | 2 | EIP ulnar |
| Right | 20 | M | 9 | 13 | 8 | 11 | 3 | EIP volar |
| Left | 20 | F | 10 | 7 | 11 | 8 | 10 | EIP ulnar |
| Right | 21 | F | 9 | 10 | 10 | 9 | 3 | EIP ulnar |
| Left | 40 | M | 7 | 11 | 10 | 8 | 24 | 2 slips of EIP ulnar |
| Right | 49 | F | 7 | 8 | 11 | 11 | 4 | EIP ulnar |
| Right | 33 | M | 9 | 12 | 9.5 | 12 | 18 | EIP ulnar |
| Right | 20 | F | 9 | 10 | 9 | 8 | 6 | EIP ulnar |
| Left | 33 | M | 9 | 15 | 11 | 15 | 24 | EIP ulnar |
| Average | 36.4 | 9.3 | 11.1 | 11.0 | 10.6 | 16.2 | ||
| Standard deviation | 12.7 | 1.7 | 2.7 | 1.7 | 2.1 | 11.1 | ||
| Sex | Age (yr) ± Std | Circumference at dER (mm) ± Std | Circumference at MCP (mm) ± Std | EIP distance from dER to myotendinous junction (mm) ± Std | ||
| cEDCI | cEIP | cEDCI | cEIP | EIP | ||
| M | 34.7 ± 11.1 | 9.5 ± 1.9 | 11.7±2.8 | 11.1 ± 1.8 | 11.0 ± 2.3 | 18.4 ± 11.8 |
| F | 40.2 ±1 5.8 | 9.1 ± 1.1 | 9.9 ± 2.0 | 10.9 ± 1.4 | 9.7 ± 1.6 | 11.2 ± 8.0 |
| P value | 0.28 | 0.56 | 0.09 | 0.77 | 0.14 | 0.11 |
In one specimen, the EIP tendon was split at the extensor retinaculum, with the radial branch joining the EDCI tendon at the MCP. However, both slips of the EIP were still found to be ulnar to the EDCI tendon at the distal extensor retinaculum (Figure 2).
Although EIP has a role in index finger extension, it also possesses utility in tendon transfers. It is most often used in cases of EPL rupture, and many anatomic studies have been performed on extensor tendon variations[1,4,8,14]. The causes of these differences remain obscure, although differences in racial grouping have been suggested. South Asian populations have the highest rate of single-slip EIP and the lowest rate of double-slip EIP when compared to Japanese, Europeans and North Americans[1].
We chose to measure EIP and EDCI circumference at the distal edge of the extensor retinaculum because this is where EIP is typically harvested to attain sufficient tendon length for transfer. Given that the EIP has the most distal muscle belly, often in the extensor retinaculum, we hypothesized that the EIP would have a greater circumference than the EDCI at the distal extensor retinaculum. Although the EIP circumference 11.1 mm (± 2.7 mm) was statistically greater than EDCI circumference 9.3 mm (± 1.7 mm) (P = 0.001), this was found to be true in only in 76% (22/29) of specimens. Perhaps this could be attributed to the wide variety in distance between the distal edge of the extensor retinaculum and the muscle belly of EIP, which averaged 16.2 mm (± 11.1 mm), similar to findings in other studies[11]. Although we hypothesized that a smaller distance between the myotendinous junction of EIP and the distal edge of the extensor retinaculum would be associated with a greater difference in circumference between EIP and EDCI, this was not found to be statistically significant (P = 0.510).
In 28/29 specimens with a single insertion for EIP, the EIP was located ulnar to the EDCI at the extensor retinaculum. It was located directly volar in the other specimen. The specimen with a split EIP had both branches ulnar to EDCI. These findings are consistent with the known literature where the vast majority (approximately 99%) of single slip EIP tendons are ulnar to EDCI[15], even when 7% of EIPs had two slips and of these, half had both tendons ulnar[1]. These findings are useful when identifying tendons for transfer with small transverse incisions at the distal extensor retinaculum. Although there are other reports of minimally invasive single incision EIP to EPL transfer[15] with a 3 cm incision placed midway between the course of the EIP and EPL at the level of mid-diaphyseal metacarpal, we believe the frequent anatomic variations in the EDCI and EIP relationship warrant additional incisions for EIP harvest and identification.
Given the finding of the frequently more ulnar EIP to EDCI tendon at the level of the distal extensor retinaculum, we recommend performing a small transverse as opposed to a longitudinal incision at the extensor retinaculum, allowing for a more cosmetic scar. Here, we share our preferred technique using wide awake local EIP to EPL tendon transfer[16].
Begin by injecting 30 mL of 1% lidocaine with 1 : 100000 epinephrine 2 cm beyond the distal extent of the planned incisions. For incisions, we recommend a small 1 cm transverse incision just ulnar to Lister’s tubercle at the distal aspect of the extensor retinaculum over the EIP tendon, a 1cm transverse incision over the index metacarpophalangeal joint, and a 2 cm longitudinal incision over the thumb carpometacarpal joint, where the distal stump of the EPL is often located for transfer. At the distal extensor retinaculum, fully flex the wrist and identify the ulnar EIP tendon. Perform a small 1cm transverse incision at the index MCP joint to transect the more ulnar EIP tendon. The extensor indicis is consistently “free” from junctura tendinae[3,8], and after dissecting the EIP tendon from EDCI, a small Ragnell retractor may be used to harvest the EIP tendon through the 1 cm incision at the distal extensor retinaculum. A transverse incision acknowledging the frequent relationship of the EIP being more ulnar or volar to EDCI at the distal extensor retinaculum avoids the longitudinal incision previously used by the authors for dissection to the myotendinous junction, improving cosmesis with an incision hidden along Langer’s lines. Use a single 4-0 Fiberwire (Arthrex, Naples, FL) suture to secure any remaining distal EIP tendon stump to EDCI at the MCP joint to prevent the tendon stump from interfering with range of motion of the MCP joint. Transfer the harvested tendon subcutaneously into the longitudinal thumb incision (underneath dorsal radial branch of radial nerve), leaving the tendon in the extensor retinaculum. Use a tendon weaver to make 3 Pulvertaft weaves at 90 degree angles to each other and set the appropriate tension for the tendon to allow full extension of MCP and IP joints, or just shy of full extension to accommodate for loosening of the transfer. Place a single 4-0 Fiberwire suture before asking the patient to move the thumb. Check full flexion and full extension to ensure appropriate range of motion. Place a 4-0 Fiberwire horizontal mattress suture through each subsequent weave. Splint in thumb spica with thumb fully extended for 4 wk and start the retraining process with a hand therapist. In cases of suspected abnormal anatomy, we recommend following the EIP tendon proximally with an additional incision at the myotendinous junction to evaluate for the most distal muscle belly in order to isolate the correct slip(s) for tendon transfer. Should there be a split tendon, consider using a single slip for the tendon transfer.
Although a power analysis was implemented to detect significance for an effect size of 0.6 with 2 mm difference in tendon circumference, it is inadequately powered to capture all variations due to the relatively low incidence of these tendon variations. We performed our dissections from a random selection of cadaveric specimens but there is a chance that it is not representative of the population as a whole. Lastly, there is a chance of measurement error given the small values being analyzed. To counteract this, Prolene, a synthetic monofilament composed of isostatic crystalline stereoisomer of polypropylene was chosen for its intrinsic high memory characteristics and thus decreased risk for error in measurement with small caliber tendons[13]. Considering these limitations, we believe that our study is well designed to accurately depict the relationship between the EIP and EDCI at the distal retinaculum and builds on the existing literature characterizing the complex relationship of dorsal hand tendons.
We found that EIP was consistently ulnar to EDCI in 96.5% of specimens at the distal extensor retinaculum. The EIP had a greater circumference in 76% (22/29) of specimens at the distal extensor retinaculum. This research contributes to the body of knowledge on extensor tendon anatomy and facilitates the smaller incisions and dissection of EIP needed for tendon transfers.
We sought to characterize the arrangement and circumference of the extensor indicis proprius (EIP) tendon with respect to the extensor digitorum communis tendon to the index finger (EDCI) at the level of the extensor retinaculum, where tendon harvest is often performed, and share our preferred technique for EIP to extensor pollicis longus (EPL) transfer.
Twenty-nine fresh-frozen cadaveric forearms were dissected. Tendon circumference and relationship of the EIP and EDCI at the metacarpophalangeal (MCP) joint and the distal extensor retinaculum were recorded. Distance from the distal extensor retinaculum to the EIP myotendinous junction was measured.
EIP was ulnar to the EDCI in 96.5% of specimens (28/29) at the distal edge of the extensor retinaculum. In the remaining specimen, EIP was volar to EDCI. Tendon circumference at the distal extensor retinaculum averaged (9.3 mm ± 1.7 mm) for EDCI and 11.1 mm (± 2.7 mm) for EIP (P = 0.0010). The tendon circumference at the index MCP joint averaged 11.0 mm (± 1.7 mm) for EDCI and 10.6 mm (± 2.1 mm) for EIP (P = 0.33). EIP had a greater circumference in 76% (22/29) of specimens at the distal extensor retinaculum whereas EIP had a greater circumference in only 31% (9/29) of specimens at the MCP joint.
The EIP tendon is frequently ulnar to and greater in circumference than the EDCI at the distal extensor retinaculum, suggesting a minimally invasive approach to tendon transfer using transverse incisions hidden in Langer's lines would be effective and safe.
This research contributes to the body of knowledge on extensor tendon anatomy and facilitates the smaller incisions and dissection of EIP needed for tendon transfers.
Understanding the variability in anatomic relationships is important when harvesting EIP through a small incision. To our knowledge, no studies have examined the relationship and anatomy of the EIP and EDCI at the level of tendon harvest at the distal extensor retinaculum.
The EIP is a redundant extrinsic extensor of the index finger, commonly used in tendon transfer for EPL ruptures. Many variations of the course and arrangement of the tendons have been previously described. It is important to understand the arrangement and anatomy of the EIP tendon at the level of tendon harvest.
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind's overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anatomy and morphology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Luo ZW, China; Pace V, Italy S-Editor: Wang DM L-Editor: A P-Editor: Wang DM
| 1. | Yammine K. The prevalence of the extensor indicis tendon and its variants: a systematic review and meta-analysis. Surg Radiol Anat. 2015;37:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Hirai Y, Yoshida K, Yamanaka K, Inoue A, Yamaki K, Yoshizuka M. An anatomic study of the extensor tendons of the human hand. J Hand Surg Am. 2001;26:1009-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Zilber S, Oberlin C. Anatomical variations of the extensor tendons to the fingers over the dorsum of the hand: a study of 50 hands and a review of the literature. Plast Reconstr Surg. 2004;113:214-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | von Schroeder HP, Botte MJ. Anatomy of the extensor tendons of the fingers: variations and multiplicity. J Hand Surg Am. 1995;20:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | von Schroeder HP, Botte MJ. Anatomy and functional significance of the long extensors to the fingers and thumb. Clin Orthop Relat Res. 2001;74-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Gonzalez MH, Weinzweig N, Kay T, Grindel S. Anatomy of the extensor tendons to the index finger. J Hand Surg Am. 1996;21:988-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Mestdagh H, Bailleul JP, Vilette B, Bocquet F, Depreux R. Organization of the extensor complex of the digits. Anat Clin. 1985;7:49-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Celik S, Bilge O, Pinar Y, Govsa F. The anatomical variations of the extensor tendons to the dorsum of the hand. Clin Anat. 2008;21:652-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Skoff HD. Postfracture extensor pollicis longus tenosynovitis and tendon rupture: a scientific study and personal series. Am J Orthop (Belle Mead NJ). 2003;32:245-247. [PubMed] |
| 10. | Heidemann J, Gausepohl T, Pennig D. [Narrowing of the third extensor tendon compartment in minimal displaced distal radius fractures with impending rupture of the EPL tendon]. Handchir Mikrochir Plast Chir. 2002;34:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Lepage D, Tatu L, Loisel F, Vuillier F, Parratte B. Cadaver study of the topography of the musculotendinous junction of the finger extensor muscles: applicability to tendon rupture following closed wrist trauma. Surg Radiol Anat. 2015;37:853-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Schneider LH, Rosenstein RG. Restoration of extensor pollicis longus function by tendon transfer. Plast Reconstr Surg. 1983;71:533-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Swanson NA, Tromovitch TA. Suture materials, 1980s: properties, uses, and abuses. Int J Dermatol. 1982;21:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 56] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Ozturk K, Kastamoni Y, Dursun A, Albay S. Prevalence of the extensor digitorum, extensor digiti minimi and extensor indicis tendons and their variations. Hand Surg Rehabil. 2020;39:320-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Lahiri A. A Simple and Quick Tendon Transfer Technique to Restore Thumb Function OPEN ACCESS Surgical Technique. World J Surg Surg Res. 2020;3:1208. |
| 16. | Lalonde DH. Wide-awake extensor indicis proprius to extensor pollicis longus tendon transfer. J Hand Surg Am. 2014;39:2297-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |