Published online Nov 18, 2022. doi: 10.5312/wjo.v13.i11.955
Peer-review started: April 6, 2022
First decision: May 31, 2022
Revised: July 13, 2022
Accepted: October 19, 2022
Article in press: October 19, 2022
Published online: November 18, 2022
Processing time: 223 Days and 21 Hours
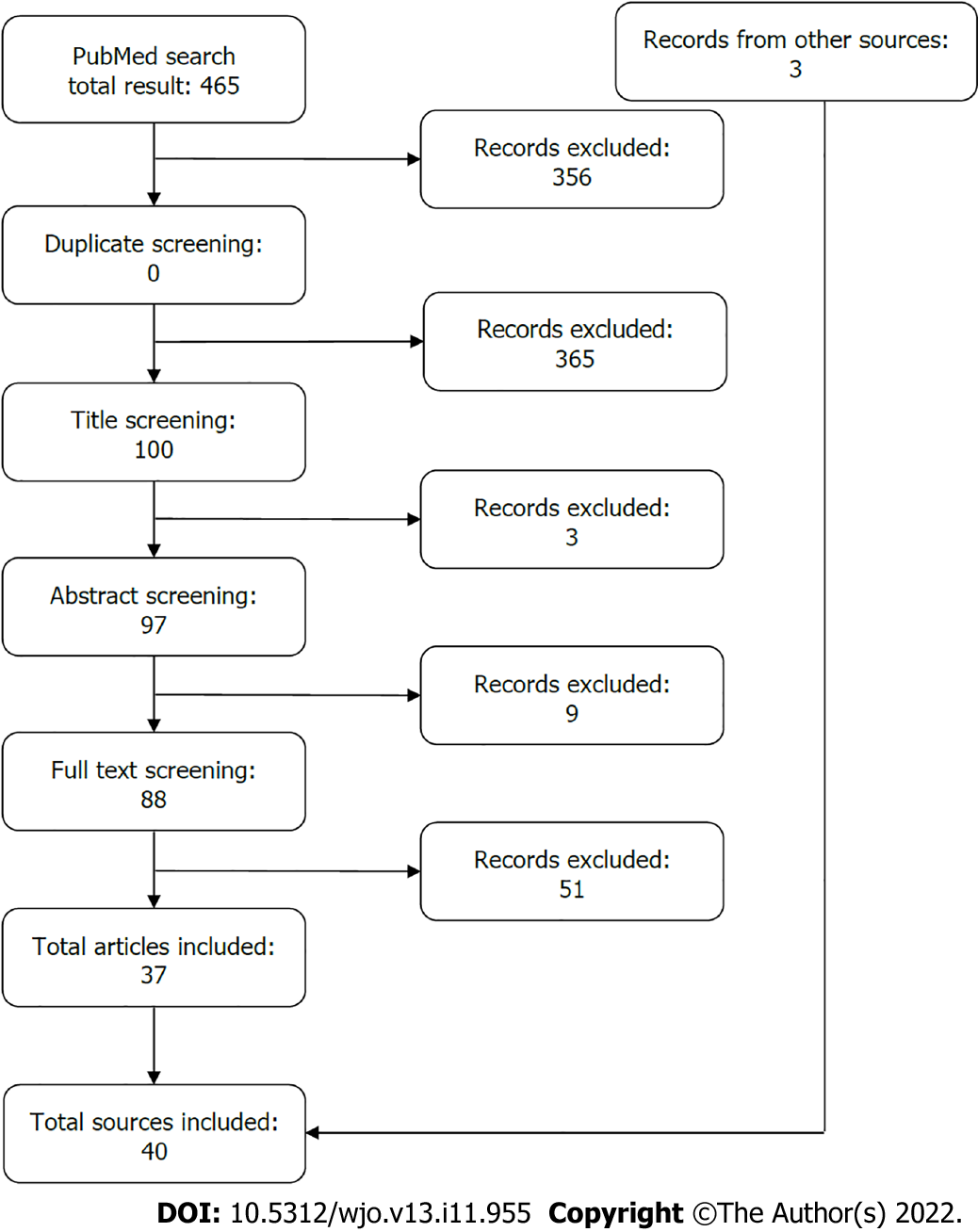
As of June 10, 2022, the World Health Organization has recorded over 532 million documented coronavirus disease 2019 (COVID-19) [(Coronavirus) SARS-CoV-2] cases and almost 6.3 million deaths worldwide, which has caused strain on medical specialties globally. The aim of this review is to explore the impact that COVID-19 has had on orthopedic practices. Providers observed a rapid decline in the number of orthopedic patients’ admissions due to cancellation of elective procedures; however, emergent cases still required treatment. Various observational studies, case reports, and clinical trials were collected through a PubMed database search. Additional sources were found through Google. The search was refined to publications in English and between the years of 2019 and 2021. The keywords used were “COVID-19” and/or “Orthopedic Injuries”. Thirty-seven studies were retained. The pandemic brought on significant changes to the mechanism of injury, number of admissions, type of injuries, and patient outcomes. Mortality rates significantly increased particularly amongst patients with hip fractures and COVID-19. Road traffic injuries remained a common cause of injury and domestic injuries became more prevalent with lockdown. Social isolation negatively affected mental health resulting in several orthopedic injuries. Telehealth services and separation for COVID-positive and COVID-negative patients benefited both patients and providers. While hospitals and medical facilities are still facing COVID-19 case surges, it is important to understand how this pandemic has impacted preparation, care, and opportunities for prevention education and ongoing care.
Core Tip: Previous and impending surges of coronavirus disease 2019 have caused a disruption in orthopedic specialties in elective procedures and changed the causation and outcomes of emergent cases. The pandemic has also impacted patient care and short-term and long-term outcomes.
- Citation: Obamiro E, Trivedi R, Ahmed N. Changes in trends of orthopedic services due to the COVID-19 pandemic: A review. World J Orthop 2022; 13(11): 955-968
- URL: https://www.wjgnet.com/2218-5836/full/v13/i11/955.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i11.955
Now entering the third year of the coronavirus disease 2019 (COVID-19) [caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)] pandemic, the number of globally reported cases continues to increase at a rapid rate despite the introduction of authorized vaccines. As of June 10, 2022, there have been almost 532 million cases and over 6.3 million deaths worldwide[1]. Hospitals continue to be overwhelmed with positive cases as new variants emerge. Hospital protocols in patient care have been changing to keep health care workers and patients safe and to keep resources on hand[2]. Non-emergent procedures were delayed in stages to reduce the burden on healthcare services. The long-term effects of these delays have not yet been fully understood as the pandemic continues. These delays occurred across all specialties. In particular, many orthopedic surgeries were postponed, being one of the most common specialties to oversee elective procedures.
The lockdown brought on by the pandemic presented many challenges; routine procedures became more complex, patients were forced to seek medical care later than anticipated due to fear of contracting the disease or an overload in medical care facilities, and unavailability of rehabilitation centers postoperatively due to COVID-19 restrictions. Furthermore, limited mobility in certain age groups may have impacted bone and joint health. The focus of this review is to assess the overall impact that COVID-19 has had on patient care in the orthopedic service and evaluate new management methods for future implementation.
The PubMed database was searched for relevant studies. The search was refined to publications in English and between the years 2019 and 2021. The keywords used were “COVID-19” and/or “Orthopedic Injuries”. Observational studies, clinical trials, and case reports were included in the selection process. Reviews, meta-analyses, and systematic reviews were excluded. Articles that were related to spinal injuries or oncology were also excluded due to the complex nature of these cases. This review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Additional resources were found using a Google web search (Figure 1). The Baishideng Publishing Group Reference Citation Analysis (RCA) tool was used to create and verify citations according to the journal’s guidelines. The RCA tool also provided the Impact Index for articles. A total of 37 articles were identified and selected for the review (Table 1).
| Title | Author | Country | Study during lockdown? | Extremity injured | Patient outcomes | Article impact index |
| Lower extremity fractures | ||||||
| The COVID-19 Pandemic: The effect on open lower limb fractures in a London major trauma centre - a plastic surgery perspective | Campbell et al[3] | England | Yes | Lower extremity fractures | Despite a 64% reduction in ER attendance and 50% decrease in traffic, RTA were the most common mechanism of injury and oLLFs were reduced from 22 to 18; there was a rise in oLLFs in those with mental health diagnoses | 1 |
| Increased Mortality and Major Complications in Hip Fracture Care During the COVID-19 Pandemic: A New York City Perspective | Egol et al[4] | United States | Yes | Hip fractures | Rates of mortality in hip fracture patients in COVID-positive, suspected COVID, and COVID-negative groups were 35.3%, 7.1%, and 0.9%, respectively | 28 |
| Hip fracture care and mortality among patients treated in dedicated COVID-19 and non-COVID-19 circuits | Ojeda-Thies et al[5] | Spain | Yes | Hip fractures | COVID-negative patients were able to receive timely and adequate care; COVID-positive patients also received adequate care but there were delays in surgeries; separating COVID-positive and negative patients helped efficiently treat patients | 1 |
| Effect of Covid-19 on best practice care of hip fracture patients: An analysis from the National Hip Fracture Database (NHFD) | Tyas et al[6] | UK | Yes | Hip fractures | COVID-19 led to a significant reduction in best practice tariff with decreases in timely surgery, postoperative delirium, 20-d mortality, length of stay, and timely orthogeriatric review | 0 |
| Rehabilitation guidance for hip fracture patients during the COVID-19 pandemic using chat software: A new model | Gao et al[7] | China | Yes | Hip fractures | Complications and mortality were higher in the group that did not use WeChat; complications included UTIs, deep vein thrombosis, dislocation, and infections | 1 |
| Hip Fracture Outcomes During the COVID-19 Pandemic: Early Results From New York | Lebrun et al[8] | United States | Yes | Hip fractures | Mortality was 56% amongst COVID-19 patients and were at higher risk for pneumonia and hyperinflammation | 19 |
| IMPACT-Scot report on COVID-19 and hip fractures | Hall et al[9] | Scotland | Yes | Hip fractures | Low platelet count was an indicator for an increased risk of COVID-19 infection and COVID-19 was related with an increased risk of 30-d mortality | 27.5 |
| Hip fracture care during Covid-19: a regional trauma centre's experience | Crozier-Shaw et al[10] | Ireland | Yes | Hip fractures | Though there was a 20% reduction in hip fractures, the 30-d mortality rate increased from 2.2% to 8.3% and having COVID-19 also increased mortality rates | 2 |
| Clinical Characteristics and Perioperative Complication Profiles of COVID-19-Positive Patients Undergoing Hip Fracture Surgery | Galivanche et al[11] | United States | Yes | Hip fractures | COVID-positive patients presented with more comorbidities which resulted in a higher incidence of adverse events perioperatively | 0 |
| Treatment of Proximal Femoral Fragility Fractures in Patients with COVID-19 During the SARS-CoV-2 Outbreak in Northern Italy | Catellani et al[12] | Italy | Yes | Femur fractures | Surgery is required for positive outcomes, but respiratory stabilization is crucial to ensure survival, comfort, and stability | 30 |
| Influence of coronavirus disease 2019 pandemic state of emergency in orthopaedic fracture surgical treatment | Mitkovic et al[13] | Serbia | Yes | All | Overall number of fractures decreased, female patients were observed more for femoral neck fractures | 2.5 |
| The effect of COVID-19 pandemic on the care of fragility hip fracture patients in the United Kingdom | Orfanos et al[14] | United Kingdom | Yes | Hip fractures | Early intervention resulted in better outcomes, higher mortality rates amongst COVID-positive patients | 0 |
| How SARS-CoV-2 Pandemic Changed Traumatology and Hospital Setting: An Analysis of 498 Fractured Patients | Brayda-Bruno et al[15] | Italy | Yes | All | More femoral fractures during COVID era, average injury age increased to 69, separating COVID-negative and positive patients allowed patients to remain negative, faster diagnoses to discharge times | 0 |
| Do standards of care and early outcomes of periprosthetic fractures change during the COVID-19 pandemic? A multicentre study | Zagra et al[16] | Italy | Yes | All | Delays in surgery, hip fractures were associated with higher mortality rates, 60% of orthopedic patients were at risk of developing perioperative complications | 0 |
| Perioperative management of patients with hip fractures and COVID-19: A single institution's early experiences | Muse et al[17] | United States | Yes | Femur fractures | Early intervention improved patient outcomes in COVID-positive patients; spinal anesthesia was used to prevent viral aerosolization; treatment plans should be altered based on severity of infection | 1.5 |
| Foot and ankle trauma management during the COVID-19 pandemic: Experiences from a major trauma unit | Shah et al[18] | England | Yes | Foot and ankle fractures | Telemedicine aided in reducing patient-provider contact and eased the burden of follow-up | 1 |
| Effect of the COVID-19 pandemic on foot surgeries | Kuliński et al[19] | Poland | Yes | Foot fractures | Total orthopedic surgeries declined by 55% and elective surgeries were not eliminated. The length of stay was decreased by 2.5 d for adults and 1.7 d for children | 0 |
| Outcomes of orthopaedic trauma surgery in COVID-19 positive patients | Al-Humadi et al[20] | United States | Yes | Lower Extremity | Operations in COVID-positive patients were accomplished with anticoagulation and hematologic and pulmonary management; complications and mortality still occurred | 0 |
| Upper extremity fractures | ||||||
| Patient care modifications and hospital regulations during the COVID-19 crisis created inequality and functional hazard for patients with orthopaedic trauma | Dunkerley et al[21] | United Kingdom | Yes | Upper extremity fractures | The increase in use of telemedicine services resulted in 12% of patients discharged with potentially unstable fractures with a danger of mal-union | 1.5 |
| A Call to Arms: Emergency Hand and Upper-Extremity Operations During the COVID-19 Pandemic | Diamond et al[22] | United States | Yes | Hand and upper extremity | A 40% increase in volume injuries attributed to high risk behaviors such as lawlessness, assault, and high-speed auto accidents; lack of social and physical impacted and aggravated injuries | 2 |
| Upper extremity emergencies during SARS-COV-2 pandemic: Turnout trends | Fyllos et al[23] | Greece | Yes | Upper extremity fractures | The mechanisms for which emergency upper extremity and hand and wrist injuries occurred were mostly from domestic accidents such as new hobbies | 0 |
| The impact of COVID-19 on shoulder and elbow trauma in a skeletally immature population: an Italian survey | Gumina et al[24] | Italy | Yes | Shoulder and elbow | Pediatric cases decreased by 84.6%, shoulder and elbow traumas were caused by domestic accidents | 1.5 |
| Other fractures | ||||||
| Outcomes of Orthopaedic Trauma Services at a UK Major Trauma Centre During a National Lockdown and Pandemic: The Need for Continuing the Provision of Services | Donovan et al[25] | United Kingdom | Yes | All | Theater time increased by 14 min due to new PPE requirements. Complication and mortality rates remained unchanged and there was not a higher risk of transmitting COVID-19 in the hospital | 0.5 |
| Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic | Maniscalco et al[26] | Italy | Yes | Femur fractures | There was a decrease of emergency ortho cases by 26.8%; femur fractures decreased, and other fracture types increased; school traumas were 0%, sports injuries decreased by 75.3%, work injuries decreased by 42.2% | 0 |
| Evaluation of containment measures' effect on orthopaedic trauma surgery during the COVID-19 pandemic: a retrospective comparison between 2019 and 2020 | Druel et al[27] | France | Yes | Upper extremity, lower extremity, hand fractures | Work-related accidents, RTAs, and altercations decreased, but domestic accidents increased. Rates of infection decreased; overall there was a 28.7% decrease in trauma surgery patients | 3 |
| Impact of the COVID-19 pandemic on the trauma and orthopaedic department at level one Major Trauma Centre in the republic of Ireland | Elbardesy et al[28] | Ireland | Yes | All | Adult distal radius fractures increased by 88% and pediatric elbow fractures decreased by 13%. Fractures were mostly caused by independent outdoor activities | 0 |
| The impact of COVID-19 on orthopaedic trauma: A retrospective comparative study from a single university hospital in Italy | Andreozzi et al[29] | Italy | Yes | All | Average age of patients increased, 67% of injuries occurred in the home, and the most commonly injured body part was the hand | 0 |
| Effects of COVID-19 pandemic curfew on orthopedic trauma in a tertiary care hospital in Turkey | Kalem et al[30] | Turkey | Yes | All | Center saw a 65% decrease in upper extremity injuries. Overall human movement has decreased by about 40% which is correlated to the decrease in admissions | 0 |
| Elective surgeries | ||||||
| COVID-19 consent and return to elective orthopaedic surgery: allowing a true patient choice? | Clough et al[31] | England | Yes | All | Rates of COVID-19 were lower at elective surgery compared to trauma sites | 1 |
| Practice patterns | ||||||
| The Effect of COVID-19 on Orthopedic Practices and Surgeons in Louisiana | Kale et al[32] | United States | No | All | COVID-19 restructuring led to delays in care, injuries not properly healed, and increase in pain. | 2 |
| A clinical pathway for pre-operative screening of COVID-19 and its influence on clinical outcome in patients with traumatic fractures | Meng et al[33] | China | Yes | All | Average wait time to surgery increased by 4.1 d, resulting in complications such as pneumonia, fever, venous thromboembolism, and cardiovascular complications | 7.5 |
| Lessons Learnt from Managing Orthopaedic Trauma During the First Wave of the COVID-19 Pandemic at a UK District General Hospital | Patel et al[34] | United Kingdom | Yes | All | Delays to surgery were doubled and postoperative complications were more present but were not directly associated with COVID-19 status | 1 |
| Effect of COVID-19 on surgical management of open fractures and infection rates: A tertiary care experience in Indian set-up | Gupta et al[35] | India | Yes | All- open fractures | Even though this center saw a decrease of cases, there was a delay of patient presentation to the ER, delay in administering antibiotics, and an increase of emergency temporary fixations, infection rates, and readmissions | 0.5 |
| Pooling of neglected and delayed trauma patients - Consequences of 'lockdown' and 'Unlock' phases of COVID-19 pandemic- A retrospective cohort analysis from a tertiary centre | Saini et al[36] | India | Yes | Upper and lower extremity fractures | Complications (blood loss, requirement for bone grafts) rates increased, delays to surgery significantly increased from an average of 8.23 d to 21.38 d | 0 |
| Miscellaneous | ||||||
| Mortality risk of surgically managing orthopaedic trauma during the COVID-19 pandemic | Balakumar et al[37] | United Kingdom | Yes | Femur fractures | The risk of contracting COVID-19 perioperatively was 11%, separating COVID-negative and -positive patients did not improve patient outcomes | 0 |
| Effect of COVID-19 on Ulnar Collateral Ligament Reconstruction in Major League Baseball Pitchers | Paul et al[38] | United States | No | Ulnar Collateral Ligament | Decreased movement had an impact on ulnar collateral ligament reconstruction rates when sporting practices resumed | 0 |
| The patterns and management of fracture patients under COVID-19 outbreak in China | Yu et al[39] | China | Yes | Upper and lower extremity fractures | Delays in surgery, decrease in total number of patients but increase in forearm, thigh, hand, and foot fractures. Hip fractures most prevalent | 2 |
Campbell et al[3] utilized a prospective and retrospective study to compare the management of open lower limb fractures (oLLFs) in the pre- and peri-COVID pandemic periods. oLLFs comprised of open fractures of long bones, and hind or mid foot. A 64% reduction in ED attendances pre-COVID (25264) compared to that peri-COVID (9042) and 18% reduction in oLLFs have been observed. Despite a decrease of almost 50% in traffic, road traffic accidents (RTA) were still the most common cause of injury in this COVID period. There was a rise in incidents of oLLFs following a fall from a height, mostly seen in relatively young patients due to an increased incidence of suicide. Despite reassignments of junior surgical staff, some senior level surgical staff remained committed to provide emergency orthopedic surgery care that resulted in timely intervention of open long bone fractures.
Egol et al[4] researched the mortality and major complications in hip fracture care during the pandemic across seven musculoskeletal care centers across New York. The study focused on the health care system’s response to the essential care of its hip fracture patients and its effects on patient outcomes. This prospective study was employed from February 1, 2020 through April 15, 2020, to compare 138 recent and 115 pre-COVID hip fracture patients. Patients with recent hip fractures were grouped into three classes: COVID-positive, suspected COVID, and COVID-negative groups. The COVID-negative patients underwent surgery immediately whereas COVID-positive patients’ surgery was delayed. The approach to surgery for hip fractures was the same regardless of COVID status. The majority of patients received general anesthesia and a proportion of patients underwent spinal anesthesia. As expected, higher mortality was found in COVID-positive patients compared to suspected or COVID-negative patients: 35.3%, 7.1%, and 0.9% respectively.
Ojeda-Thies et al[5] retrospectively studied patients treated for hip fractures during the COVID-19 pandemic from March 1, 2020 through May 1, 2020. This center divided 64 patients into three cohorts: pre-cohort of 17 patients, 14 COVID-positive patients, and 33 COVID-negative patients. More than 90% of patients received spinal anesthesia. There was a higher incidence of COVID positivity (23.5%) rate after the patients were discharged from the hospital following hip surgery and 50% of those patients died. That resulted in separating the anesthesia circuit for COVID-positive and COVID-negative patients. The study revealed that separate circuits for COVID-19 and non-COVID-19 patients allows adequate hip fracture care, despite delayed surgery in patients with severe respiratory illness from COVID. Separating patients that were not infected from those that were, helped with the efficiency of treating fractures amongst COVID-negative patients and significantly reduced the 30-day mortality and the conversion rates.
Tyas et al[6] studied the effect of COVID-19 on Best Practice Tariff for hip fractures in 40000 patients collected from the National Hip Fracture Database (NHFD) from England, Wales, and Northern Ireland. Best Practice Tariff was used to optimize care for patients, incentivize providers, and yield better outcome. Quality metrics such as timely surgery, postoperative delirium, 30-d mortality, hospital length of stay, and timely orthogeriatric review were assessed. Researchers concluded that COVID-19 led to a significant reduction in best practice tariff. Prompt geriatric review dropped over the review period. Significant changes in bone health assessments, reduction in falls assessments, and postoperative delirium were also observed. Mortality rates peaked at 13.7%. Therefore, it is important to maintain the quality care and assessment of geriatric hip fractures and management in next pandemic.
Gao et al[7] piloted a study at a hospital in China for tracking hip fracture patients postoperatively and providing rehabilitation guidance using a chat software called WeChat. The study selected 80 patients and divided them into two equal groups of observation and control. The control group was given traditional discharge instructions and the observation group received additional instructions that provided continuous instruction of physical therapy exercises through WeChat apps. This study was done at the peak season of COVID-19 between February 1, 2020 and April 30, 2020. Complications and mortality were significantly higher in the control group. Complications observed include urinary tract infections, deep vein thrombosis, dislocation or fracture around prosthesis, surgical site infection, and pneumonia. It was recommended that during the COVID-19 pandemic, it was helpful to use WeChat or another similar chat software to guide the rehabilitation of hip fractures to minimize postoperative complications.
LeBrun et al[8] studied 59 hip fracture patients in New York City over a 5-wk period, from March 20, 2020 to April 25, 2020 during the COVID-19 pandemic. Centralized care was established for emergency hip fracture management. Patients were separated into COVID-positive and COVID-negative groups based on infection status. The study showed that hospital mortality was significantly increased in the COVID-positive patients (56%) compared to COVID-negative patients (4%). All deaths in COVID-positive patients were related to COVID-19. COVID-positive patients were also at higher risk for complications such as pneumonia or hyperinflammation.
Hall et al[9] assessed the effects of COVID-19 on 30-d mortality for 317 patients with hip fractures in a multicenter retrospective study. The effects of social lockdown on the epidemiology of hip fractures were also assessed. Results showed that COVID-19 was independently related with an increased risk of 30-d mortality in hip fracture patients.
Crozier-Shaw et al[10] studied hip fracture care pre-COVID (45 hip fractures) and peri-COVID (36 hip fractures). A 20% reduction in hip fracture presentation was noted; however, the 30-day mortality was increased from 2.2% to 8.3%. Despite improved quality indicators that were observed in hip fracture management during the COVID-19 period, there was a 3-fold increase in mortality. Although four patients tested positive on swab test for COVID-19, two of them died. Therefore, COVID-19 was associated with increased mortality in hip fracture patients that were positive and undergoing surgery. Researchers found that these findings will be important to apply to orthogeriatric care during future COVID-19 waves.
Galivanche et al[11] collected 42002 patients through claims data that had undergone hip fracture surgical repair between April and December 2020. Of these, 678 were COVID-positive and while there were no significant differences in age, sex, or procedure type between the patients who were tested positive or negative for COVID-19, COVID-positive patients did present with a higher incidence of comorbidities. Propensity score matching was used to balance the two groups (COVID-positive vs COVID-negative). After matching, the COVID-19-positive group had a higher incidence of adverse events perioperatively such as venous thromboembolism (6.64% compared to 3.43%) and pneumonia (11.21% compared to 4.56%).
Catellani et al[12] studied 16 patients with femoral neck fractures that were COVID-positive with active infection and were receiving protocolized treatment for COVID-19 during the pandemic in northern Italy. Three patients died before surgery because of complications from COVID-19. After surgery, four patients died of respiratory failure. The overall mortality of hip fracture with active COVID-19 infection was 43.7%. Surgical mortality of hip fracture in patients with active COVID-19 infection was 30.77%. Patients who underwent surgery in the face of active infection had to pass strict criteria. Most patients received spinal anesthesia. A stabilization of respiratory parameters was observed in COVID-positive patients after the surgery. It was suggested that surgery may have contributed to the overall respiratory stability of patients, mobilization, comfort, and improvement in physiological ventilation in COVID-19-positive patients with proximal femoral fragility fractures.
Mitkovic et al[13] investigated the frequency and distribution of orthopedic fractures during the stay-at-home lockdown in Serbia. Researchers examined how the lockdown influenced the frequency of different fracture types. Staying at home for 54 d decreased the total number of fractures by 18.9% and females were more likely to suffer from femoral neck fractures during this time. However, femoral neck fractures occurred more frequently in the state of lockdown than during the same period in a non-emergency state in 2019. Mitkovic type method of external fixation was assumed to be an alternative method of tibial fracture fixation during the lockdown. That methodology presumed to be a reducing factor of intraoperative COVID-19 transmission among medical staff and hospitalization time.
Orfanos et al[14] performed a retrospective study on geriatric patients aged 60 years and above who sustained hip fracture after a fall in the United Kingdom. Of the 199 patients, 102 were included from the COVID-19 pandemic period and was compared to 97 patients from the same period in 2019. Approximately 11% of patients tested positive for COVID during the observation period. A higher proportion of female patients suffered hip fracture from a fall. However, mortality was found to be higher amongst males between the two groups (P = 0.005). There was no significant difference between the groups regarding 30-d all-cause mortality and morbidity. Early surgical intervention along with sufficient optimization prior to surgery in a COVID-positive patient was critical for his/her survival. Patients were also moved rapidly to rehabilitation facilities which aided in recovery.
Brayda-Bruno et al[15] studied 498 fracture patients in Italy during the COVID-19 pandemic to assess how the pandemic has changed traumatology and the hospital setting. It was assessed that unspecified femoral fractures were much more common in this time period than the previous time period (181/352 compared to 57/146). The average age of orthopedic patients prior to the pandemic was 61 years of age compared to during the pandemic which was 69 years of age. This institution required COVID-19 testing which expedited orthopedic services by separating COVID-negative and -positive patients. Patients that were admitted as COVID-negative remained COVID-negative during admission. Ten patients died in the pandemic group compared to zero deaths in the control group. Out of these ten patients, three died due to comorbidities and seven due to thromboembolic events related to COVID-19. Time between diagnoses and discharge was significantly lower (P = 0.03) despite an increase in orthopedic cases. The difference was attributed to early operative intervention in the pandemic group.
Zagra et al[16] conducted a retrospective multicenter study in patients with periprosthetic fractures (PPF) during COVID-19 pandemic in northern Italy. Out of 1390 patients, 38 were found to suffer from PPF. Most of the patients had femoral PPF. There was no difference in the incidence of PPF during the pandemic when compared with the earlier year prior to the pandemic. Routine screening for COVID-19 was performed and found around 10% or more with COVID-19 positivity because of positive test or the positive symptoms and imaging findings. Standard operative care was performed in PPF patients during the pandemic. Hip fracture was associated with increased 30-d mortality in COVID-positive patients compared to COVID-negative patients. Approximately 60% of PPF patients developed complications.
In a letter to the editor, Muse et al[17] used a retrospective case series of five COVID-19 orthopedic patients who sustained hip fractures, one femoral neck fracture and four intertrochanteric fracture, that underwent surgery at Montefiore Medical Center, New York. As per recommendation, hip fracture should be repaired within 48 h of admission to reduce mortality and morbidity, but only three out of the five patients underwent surgery within the 48 h timeframe and two had surgeries after 72 h of admission. While regional anesthesia is safe for COVID-positive patients, spinal anesthesia was used to prevent viral aerosolization in four patients. Only one patient received general anesthesia. None of the patients died. The most common complication was the need for packed red blood cell transfusion. Providers suggested that surgical treatment plans can be delayed if necessary.
Shah et al[18] evaluated the impact of the pandemic on foot and ankle services in a single trauma center in the UK using a retrospective cohort study. A total of 206 patients were evaluated from admission to discharge to compare pre-lockdown and lockdown phases and stable and unstable fractures. Of 100 patients with stable ankle fractures, 35 (35%) were discharged from the emergency department without a planned follow-up. The majority of patients who presented unstable fractures required some form of interventions. Some of the patients were sent home with cast, advised elevation, non-weight bearing, and to follow up for definite treatment. In another group, partial fixations were employed to reduce intraoperative time and avert the need for invasive surgeries. Most of the operated patients were followed up within 2 wk for a wound check. Patients were advised on pain and plaster management to avoid face-to-face interactions with providers. Telemedicine reduced the patient-physician contact and reduced the burden of follow-up.
Kuliński et al[19] researched the effect of the COVID-19 pandemic on both elective and emergency foot surgeries on 145 orthopedic patients in Poland. The data showed a reduction in the total number of orthopedic admissions by 55% during the pandemic. Elective orthopedic interventions declined by 72% and emergency orthopedic interventions increased by 27% during the pandemic as compared to pre-pandemic era. Length of hospital stay decreased by 2.5 d in adults and 1.7 d in children. There was a decline of 32% in the number of patients coming to ED for injuries. The pandemic did not affect the average age of patients and the male to female ratio. It is suggested that the COVID-19 pandemic has affected the epidemiology and prevalence of foot surgeries in children and adults.
Al-Humadi et al[20] conducted a retrospective case series of 11 patients to investigate outcomes of lower extremity trauma surgery in COVID-19-positive patients. Most of the patients had hip fractures and the rest sustained femur and tibia and fibular fractures. Orthopedic operations in COVID-19-positive patients were successfully done with patient anticoagulation and hematologic and pulmonary management. These three were optimized prior to surgery to reduce venous thromboembolic events and avoid blood transfusion. Complications such as deep vein thrombosis, acute renal failure, and pneumonia still occurred and two patients died postoperatively. The patients who died were more than 50 years old and had a prior history of more than one comorbid condition.
Dunkerley et al[21] noted that the pandemic has decreased operative intervention of unspecified upper extremity fractures and increased the use of telemedicine clinics. In this prospective study which was performed at the peak of the COVID-19 outbreak from April 14 through April 28, 2020, of the 154 patients that were analyzed, 51% were managed as in a normal circumstance, whereas 49% of managements were impacted by the pandemic. Of those affected, 12% were discharged at diagnosis with potentially unstable upper extremities fractures, and this had the danger of mal-union. Additionally, 29% were discharged from the orthopedic virtual clinic as opposed to having in person clinical or radiological follow-up. Nurses in the trauma team would virtually request patient care instructions from physicians working remotely. Discharged patients were fixated with removable immobilization. Follow-up surveys given to patients who were treated by the virtual clinic showed a very high satisfaction rate of 4.8/5. While telemedicine played a vital role in orthopedic management and is economical and efficient to both patients and providers, there is a potential risk of poor outcomes such as mal-union, requiring corrective treatments in the future.
Diamond et al[22] conducted a multi-center study from two Level I trauma centers in Pennsylvania and California. Researchers studied the occurrence of emergency upper extremity operations during the COVID-19 pandemic specifically during shelter-on-place orders. Injuries included trauma to the forearm, hand, wrist, and finger. It was found that there was a 40% increase in volume attributed to high-risk behavior which was defined as lawlessness, assault, and high-speed auto accidents. Additionally, it was found that home improvement projects, lack of social and physical resources, and delay of treatment due to avoidance of treatment facilities are also impacting the high volume of upper extremity injuries.
Fyllos et al[23] compared the turnout of patients with orthopedic, upper extremity, and hand and wrist emergencies during pre-pandemic and peri-pandemic periods. During the pandemic, it was found that the numbers of patients with orthopedic, upper extremity, and hand and wrist problems (e.g., arthritis and tendinopathy) were significantly reduced by 57.09%, 49.77%, and 49.95%, respectively, compared to a patient population in 2019. However, upper extremity injury emergencies (e.g., fractures and dislocations) increased from 37.17% to 43.32% and hand and wrist injury emergencies increased from 25.07% to 29.15%. Although other causes of injury have decreased, it is suggested that the increase of domestic accidents from new hobbies during the lockdown have been the probable cause of the surge.
Gumina et al[24] evaluated 404 patients under the age of 18 that were treated at the trauma center for shoulder and elbow injuries before and during the pandemic (from March 8, 2020 through April 8, 2020). Young people typically incur high-energy injuries from social activities, school activities, sports, parks, and clubs. Due to the prohibition of these events, injuries caused by these activities were almost eliminated. There were no cases of contusions, physeal fractures, other fractures, or dislocations of the elbow. The shoulder and elbow injuries seen at this center were mainly caused by falls in the home, offering an opportunity for education.
Donovan et al[25] performed a retrospective case-controlled study at a Level 1 trauma center in the UK. Factors such as anatomical area of injury, cause of injury, operative procedure, type of anesthesia, total operating time, complications, and 30-d mortality were analyzed against a dataset of 248 patients. The 248-patient dataset was comprised of 142 patients that required 165 operations pre-pandemic and 106 peri-pandemic patients that underwent 124 operations. During the COVID period, the results showed a 30% decrease in overall orthopedic injuries due to a reduced number of road traffic accidents and sporting injuries. Also, the number of hip fractures and low impact injuries remained the same. Operative time increased by 14 min due to the new personal protective equipment (PPE) requirements. During the COVID-19 pandemic, a higher number of patients received spinal anesthesia and fewer patients received general anesthesia. Complications and mortality rates did not change. The incidence of COVID-19 in the patients tested in the hospital and in the general population at the time of the study was the same at 8.5%.
Maniscalco et al[26] conducted a study on the impact of COVID-19 on orthopedic traumas presenting to the emergency orthopedic departments in Parma and Piacenza Hospital, Italy, evaluating patients admitted with proximal femur fractures. The study collected data for patients between February 22, 2020 and April 18, 2020 and was compared with 2019 data. The results showed a decrease in orthopedic cases at the ER by 26.8%. Regular mechanisms of injury vastly changed, where there was a 19.1% increase of the traumas occurring in the home, sports injuries decreased by 75.3%, work injuries decreased by 42.2%, and school traumas were reduced to 0%. A decrease in femur fractures from 38.9% to 33.5% was also observed during the pandemic. A higher mortality was reported during the pandemic in elderly patients with femur fracture due to COVID-19.
Druel et al[27] studied the effects of COVID-19 containment measures on 888 orthopedic trauma surgeries during the pandemic at a trauma center in France. Participants were divided into three cohorts: Reference, pre-containment, and containment groups. The occurrence of domestic accidents increased from 51.6% to 64.8% whereas work-related accidents, altercations, and RTA decreased. The decrease in the number of cases (from 6.7% to 4.0%) could be due to fear of going to medical facilities, fear of containment rules, or minimizing the seriousness of symptoms. Overall, the results showed a decrease of 28.7% in the number of patients undergoing trauma surgery services during the containment period.
Elbardesy et al[28] investigated the impact of COVID-19 pandemic on trauma and orthopedic center in Ireland among 505 patients. The study was conducted between March 1, 2020 and April 14, 2020 and compared patients from 2019 in the same time period. The total number of trauma and orthopedic surgeries performed decreased by 10.5%. Likewise, the number of pediatric orthopedic procedures decreased by 40.32%. Adult distal radius and pediatric elbow fractures increased by 88% and 13%, respectively, while hip fractures remained the most common trauma. Overall, the COVID-19 pandemic led to a decrease in the total number of trauma surgeries. Notably, injuries directly related to solo outdoor activities such as ankle, radius, elbow, and hand fractures increased.
Andreozzi et al[29] performed a retrospective comparative study of the impact of COVID-19 on orthopedic trauma in Italy. They analyzed the impact of the lockdown on acute orthopedic trauma. The overall number of admissions in the pre-COVID era was 995 as compared to 204 during COVID-19 outbreak. Average age of patients (51.9 years old) was significantly higher during the pandemic as compared to pre-pandemic (41.4 years old). Most injuries (65.7%) occurred at home during the pandemic as compared to 32.3% pre-pandemic. The most injured extremity during the pandemic was the hand (14.2%) compared to before the pandemic which was polytrauma (22.8%). While overall rates of acute traumas have decreased, the incidence of hip fractures remained high, indicating a need for focus on orthogeriatric care.
Kalem et al[30] studied the effect of COVID-19 pandemic on the prevalence and epidemiology in 361 orthopedic trauma patients in Turkey. The study examined the fractures distribution in three age categories (≤ 20 years, 21-64 years, and ≥ 65 years). The overall number of admissions decreased by 50.9% and upper extremity injuries decreased by 65%. The type of trauma and the mechanism of injury changed with a significant increase in low energy trauma and the upper extremities more affected during the pandemic (49.9% vs 30.5% peri-pandemic and pre-pandemic, respectively). However, there was no difference in occurrence of fractures in geriatric patients. It is suggested that the decrease in admissions was parallel with a 40% decrease in overall human movement.
Clough et al[31] examined the risk of contracting COVID-19 in patients undergoing orthopedic surgery. The data was collected for March 2020 to June 2020. The 225 orthopedic trauma surgery patients were separated into three surgery sites to minimize the perioperative spread of COVID infection. At the acute site that had both COVID-positive and COVID-negative patients undergoing surgery for upper and lower limb fractures, the incidence of post-surgical COVID infection was 6.5% with a 50% mortality rate. Seven (8.3%) of the 84 patients who underwent surgeries for femoral neck fractures became positive, of whom five (71%) died. On the other hand, of the patients who had surgeries in the hospital that only performed elective cases, only 0.9% patients developed COVID-19 without any mortality.
Kale et al[32] analyzed the effects of COVID-19 on orthopedic practices. A survey study was conducted with orthopedic surgeons by Louisiana Orthopaedic Association (LOA) at the peak of the pandemic. The response rate of the survey was 33%. The survey found that most surgeons delayed their elective surgeries. The decrease of patients in offices resulted in substantial loss of revenue. Furthermore, there was an increase in pain and deformities in patients due to the delay in elective procedures. Researchers found that many surgeons increased their revenue with the use of telehealth. This adaptation opens a new era of medicine.
Meng et al[33] performed a case series study at Beijing Chaoyang Hospital. Researchers aimed to analyze clinical outcomes of patients that were required to undergo orthopedic surgery. Fracture types included clavicle, scapular, vertebral compression, and upper and lower extremity fractures. Results showed an increase in average wait time from injury to surgery of 8.7 ± 3.4 d in March and April 2020 from 4.6 ± 2.6 d in the same period in 2019, almost doubling waiting time for surgeries in the pandemic. A higher percentage of patients in the pandemic developed complications such as pneumonia, fever, venous thromboembolism, and cardiovascular complications. This led to introduction of a novel clinical pathway for preoperative screening of COVID-19 in traumatic orthopedic patients, thereby reducing waiting time from injury to surgery.
Patel et al[34] conducted a retrospective study on orthopedic patients in the UK during in the pre-COVID-19 (328 patients) and peri-COVID-19 (178 patients) eras. The sample included patients with periprosthetic, pelvis, spine, upper and lower extremity, or multiple fractures. There was a reduction in orthopedic patients during the peri-COVID period and restructuring of orthopedic services in response to the COVID-19 pandemic was associated with a delay in surgery (4.91 d compared to 2.94 d) and increase in severity of postoperative complications such as nausea, vomiting, and superficial phlebitis. Complications, however, were not associated with COVID-19 status. Fast-track emergency operative orthopedic services during the pandemic were recommended.
Gupta et al[35] performed a retrospective study to compare the surgical management of upper and lower extremity open fractures during the pre-COVID (89 patients) and peri-COVID (52 patients) eras. The results showed that despite the decrease in total trauma cases, there were delays in presentation to the ED. Due to this interruption, there was a delay in administration of first dose of antibiotics; however, there was no significant delay in presentation to surgery. There was a trend of higher infection rate perhaps due to delay in antibiotics administration.
Saini et al[36] performed a retrospective study on 488 upper and lower limb fracture patients in India to explore the consequences of neglected and delayed care during and after the lockdown. It was discovered that the average delay in surgical time and hospital stay was significantly increased during each period. During lockdown, the average delay was 8.23 ± 6.1 d and after lockdown the average delay was 21.38 ± 26.14 d. Complications such as blood loss, stay in the ICU, surgical time, and requirement for bone grafts were greatly increased after the lockdown period was over though not statistically significant. Out of 45 patients who developed non-union or malunion, 42 required corrective procedures.
Balakumar et al[37] researched the risk of operating on a variety of urgent orthopedic cases during the COVID-19 pandemic first lockdown, between March 26, 2020 and May 20, 2020, for clinical decision making and efficiency of medical resource utilization. Researchers included 433 patients in the study. The average age of the patients was 65 years and the majority were involved in low energy mechanism, with femoral neck fracture being the dominant orthopedic injury. Of all patients, 72% were treated at an elective surgery site (ESS) and 23% were treated at major trauma centers (MTC). The overall mortality in femoral neck fracture was identified at 15.9%. Higher mortality was observed at the ESS (13.7%) compared to the MTC (7.7%). The higher mortality at the ESS was observed in patients who were tested positive for COVID (40.1% vs 20%). The main outcome was mortality risk considering that orthopedic patients were being treated at the MTC which admitted both COVID-positive and COVID-negative patients. It was suggested that there was an 11% rate of contracting COVID-19 peri-operatively due to being admitted to the hospital. However, using a site not designated for treating COVID-19 patients for orthopedic surgery and performing surgery at an ESS did not improve the outcome of mortality, risk of infection, or length of stay.
Paul et al[38] studied the effect of COVID-19 on ulnar collateral ligament repair (UCLR) in 106 major league baseball (MLB) players. The study observed at all pitchers of the MLB who underwent UCLR repair and found no difference in overall UCLR repair from baseball seasons 2017 through 2020 (n = 16, 20, 16, and 18). However, when the repair was examined with the number of games played pre-pandemic compared to pandemic season, it was found that pitchers were about three times more likely to undergo UCLR repair after the COVID-19 lockdown. The higher rate of UCLR was most likely due to the lack of preseason activity during lockdown periods.
Yu et al[39] compared patterns and management of fracture patients in the pre-COVID and peri-COVID eras (January 24, 2020 through March 9, 2020) in China. Fracture types included upper and lower extremities and vertebra. Researchers found a 42% decrease in the number of orthopedic patients during the COVID-19 pandemic. Time of injury to hospitalization of the patients did not change; however, time of injury to operation significantly increased during the pandemic (4.5 ± 4.1 d vs 2.0 ± 1.5 d, P < 0.001) when compared with 2019 data. Similarly, length of stay of patients after surgery was longer in the pandemic when compared to 2019 data. Mandatory screenings delayed surgery by more than 48 h. It was recommended that screening of emergency patients should be a priority to minimize risk of infection among other patients and hospital staff.
The presentation of coronavirus, while not entirely mysterious, was bound to have unprecedented effects on healthcare workers, regulations in medical specialties, and patients. Orthopedic specialties globally observed numerous changes over the evolution of the pandemic. Orthopedic cases varied in severity. Medical facilities were forced to create alternative treatment plans for emergent and elective orthopedic procedures, and the data presented showed the impact of COVID-19 on orthopedic injury. Some of the changes implemented during this time showed to be beneficial and could be potential long-term solutions for optimizing medical orthopedic management.
Hip replacements are generally the most common elective procedure, but elective procedures were halted and therefore most institutions did not perform them. Hip fractures have still been very common during this time[4,25,28]; however, the pandemic has increased the mortality and complication rate particularly amongst COVID-positive patients[5,8,11,16,38]. The importance of early treatment and proper rehabilitation was strongly emphasized in order to ensure prompt recovery[14].
Mechanism of injury also changed during the pandemic. COVID-19 impacted the number of RTAs significantly as well as sporting injuries due to lockdowns and cancellation of group gatherings[3,25,27]. Work injuries also decreased significantly due to lockdowns and remote work[26,28]. School traumas were reduced as students were engaged in online learning[24,26]. With the vast population sheltering at home, there was a dramatic increase in domestic injuries that included home improvement projects, running, and cycling[22,28,29]. There was also a rise from 18% to 35% in oLLFs in patients with mental health conditions, implying that social isolation even if necessary, negatively impacts mental health[3,22]. A 40% increase in upper extremity injuries due to high-risk behaviors was observed during this time which could also be a consequence of social isolation[22].
The use of telehealth services was introduced in several facilities to alleviate the burden on healthcare facilities as well as limit exposure of both patients and providers to COVID-19. Virtual patient care proved to have a positive impact on the rehabilitation of patients postoperatively, lowering the rate of complications[7]. The use of telehealth services, while beneficial, did have adverse effects in patients that required more hands-on treatment[21]. These patients will be required to seek care or corrective treatment for the injury in the future[21]. To take full advantage of the benefits of telehealth, the screening for the patients that can be seen virtually should be stringent in order to ensure quality care.
From the management changes that were seen during this period, there were some takeaways that should be emphasized in current standards of practice. Early intervention was and should be a priority. This is essential for patients with hip fractures or other severe fractures to minimize the risk of mal-union. Telehealth was a service to bridge the gap in healthcare for those that were COVID-positive and needed treatment or even for facilities that were not allowing any patients to be seen in person[7]. This is a service that in the future would be valuable to patients that are immobile, are ill, or have transportation issues[40]. Since appropriate PPE allows healthcare providers to treat COVID-19 patients with minimal exposure, separating COVID-positive and COVID-negative patients allowed for timely injury management and COVID management. Knowing that COVID-19 will continue to be prevalent, separating COVID-positive and negative patients can help expedite treatment for both groups of patients. This literature review emphasized the necessity of being prepared to perform routine but emergent procedures even in unprecedented crises.
There were some limitations in this study. The previous and current literature does not allow us to explore how new approaches in orthopedic management would impact patient care in the long term. Also, as we are still facing COVID-19 surges, the data to support an outcomes study is not yet available. Further research should be conducted to examine how orthopedic injury management has changed when COVID-19 is at its nadir.
To summarize, while hospitals and medical facilities are still facing COVID-19 case surges, it is important to understand how this pandemic has impacted the various specialties of healthcare. Significant changes were noted in orthopedic practices since the start of the COVID-19 pandemic including different mechanisms of injury, higher mortality rates, and injury to different areas of the body. Changes that positively impacted patient outcomes should be made standards of practice and practices that negatively impacted patient outcomes should be actively evaluated to not only be avoided in regular care but also in times of crises.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jeyaraman M, India; Lelisho ME; Velázquez-Saornil J, Spain S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | WHO. World Health Organization. COVID-19 Dashboard. Feb/03/2022. Available from: https://covid19.who.int/. |
| 2. | Guy, DK, Bosco, JA, Savoie, FH. AAOS Guidelines for Elective Surgery During the COVID-19 Pandemic. American Academy of Orthopedic Surgeons. April 2, 2020. Online Publication. Available from: https://www.aaos.org/about/covid-19-information-for-our-members/aaos-guidelines-for-elective-surgery/. |
| 3. | Campbell E, Zahoor U, Payne A, Popova D, Welman T, Pahal GS, Sadigh P. The COVID-19 Pandemic: The effect on open lower limb fractures in a London major trauma centre - a plastic surgery perspective. Injury. 2021;52:402-406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Egol KA, Konda SR, Bird ML, Dedhia N, Landes EK, Ranson RA, Solasz SJ, Aggarwal VK, Bosco JA 3rd, Furgiuele DL, Ganta A, Gould J, Lyon TR, McLaurin TM, Tejwani NC, Zuckerman JD, Leucht P; NYU COVID Hip Fracture Research Group. Increased Mortality and Major Complications in Hip Fracture Care During the COVID-19 Pandemic: A New York City Perspective. J Orthop Trauma. 2020;34:395-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 156] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 5. | Ojeda-Thies C, Cuarental-García J, García-Gómez E, Salazar-Zamorano CH, Alberti-Maroño J, Ramos-Pascua LR. Hip fracture care and mortality among patients treated in dedicated COVID-19 and non-COVID-19 circuits. Eur Geriatr Med. 2021;12:749-757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Tyas B, Wilkinson M, Singisetti K. Effect of Covid-19 on best practice care of hip fracture patients: An analysis from the National Hip Fracture Database (NHFD). Surgeon. 2021;19:e298-e303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Gao SS, Wang YJ, Zhang GX, Zhang WT. Rehabilitation guidance for hip fracture patients during the COVID-19 pandemic using chat software: A new model. J Back Musculoskelet Rehabil. 2021;34:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | LeBrun DG, Konnaris MA, Ghahramani GC, Premkumar A, DeFrancesco CJ, Gruskay JA, Dvorzhinskiy A, Sandhu MS, Goldwyn EM, Mendias CL, Ricci WM. Hip Fracture Outcomes During the COVID-19 Pandemic: Early Results From New York. J Orthop Trauma. 2020;34:403-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 9. | Hall AJ, Clement ND, Farrow L, MacLullich AMJ, Dall GF, Scott CEH, Jenkins PJ, White TO, Duckworth AD; IMPACT-Scot Study Group. IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint J. 2020;102-B:1219-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 108] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 10. | Crozier-Shaw G, Hughes AJ, Conlon B, Sheehan E, Merghani K. Hip fracture care during Covid-19: a regional trauma centre's experience. Ir J Med Sci. 2021;190:1275-1280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Galivanche AR, Mercier MR, Schneble CA, Brand J, Pathak N, Varthi AG, Rubin LE, Grauer JN. Clinical Characteristics and Perioperative Complication Profiles of COVID-19-Positive Patients Undergoing Hip Fracture Surgery. J Am Acad Orthop Surg Glob Res Rev. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Catellani F, Coscione A, D'Ambrosi R, Usai L, Roscitano C, Fiorentino G. Treatment of Proximal Femoral Fragility Fractures in Patients with COVID-19 During the SARS-CoV-2 Outbreak in Northern Italy. J Bone Joint Surg Am. 2020;102:e58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 13. | Mitkovic MM, Bumbasirevic M, Milenkovic S, Gajdobranski D, Bumbasirevic V, Mitkovic MB. Influence of coronavirus disease 2019 pandemic state of emergency in orthopaedic fracture surgical treatment. Int Orthop. 2021;45:815-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Orfanos G, Al Kaisi K, Jaiswal A, Lim J, Youssef B. The effect of COVID-19 pandemic on the care of fragility hip fracture patients in the United Kingdom. A case control study in a major trauma centre. Surgeon. 2021;19:e440-e445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Brayda-Bruno M, Giorgino R, Gallazzi E, Morelli I, Manfroni F, Briguglio M, Accetta R, Mangiavini L, Peretti GM. How SARS-CoV-2 Pandemic Changed Traumatology and Hospital Setting: An Analysis of 498 Fractured Patients. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Zagra L, D'Apolito R, Guindani N, Zatti G, Rivera F, Ravasi F, Mosconi M, Momoli A, Massè A, Franceschini M, D'Angelo F, Dallari D, Catani F, Casiraghi A, Bove F, Castelli CC. Do standards of care and early outcomes of periprosthetic fractures change during the COVID-19 pandemic? J Orthop Traumatol. 2021;22:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Muse IO, Montilla E, Gruson KI, Berger J. Perioperative management of patients with hip fractures and COVID-19: A single institution's early experiences. J Clin Anesth. 2020;67:110017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Shah R, Ahad A, Faizi M, Mangwani J. Foot and ankle trauma management during the COVID-19 pandemic: Experiences from a major trauma unit. J Clin Orthop Trauma. 2021;16:285-291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Kuliński P, Tomczyk Ł, Morasiewicz P. Effect of the COVID-19 pandemic on foot surgeries. Adv Clin Exp Med. 2021;30:1249-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Al-Humadi SM, Tantone R, Nazemi AK, Hays T, Pawlak A, Komatsu DE, Namm JD. Outcomes of orthopaedic trauma surgery in COVID-19 positive patients. OTA Int. 2021;4:e129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Dunkerley S, Thelwall C, Omiawele J, Smith A, Deo S, Lowdon I. Patient care modifications and hospital regulations during the COVID-19 crisis created inequality and functional hazard for patients with orthopaedic trauma. Int Orthop. 2020;44:2481-2485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Diamond S, Lundy JB, Weber EL, Lalezari S, Rafijah G, Leis A, Gray BL, Lin IC, Gupta R. A Call to Arms: Emergency Hand and Upper-Extremity Operations During the COVID-19 Pandemic. J Hand Surg Glob Online. 2020;2:175-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Fyllos A, Varitimidis S, Papageorgiou F, Karamanis N, Alexiou K, Veloni A, Malizos K, Dailiana Z. Upper extremity emergencies during SARS-COV-2 pandemic: Turnout trends. Injury. 2021;52:387-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Gumina S, Proietti R, Villani C, Carbone S, Candela V. The impact of COVID-19 on shoulder and elbow trauma in a skeletally immature population: an Italian survey. JSES Int. 2021;5:3-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Donovan RL, Tilston T, Frostick R, Chesser T. Outcomes of Orthopaedic Trauma Services at a UK Major Trauma Centre During a National Lockdown and Pandemic: The Need for Continuing the Provision of Services. Cureus. 2020;12:e11056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Maniscalco P, Poggiali E, Quattrini F, Ciatti C, Magnacavallo A, Vercelli A, Domenichini M, Vaienti E, Pogliacomi F, Ceccarelli F. Proximal femur fractures in COVID-19 emergency: the experience of two Orthopedics and Traumatology Departments in the first eight weeks of the Italian epidemic. Acta Biomed. 2020;91:89-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 69] [Reference Citation Analysis (0)] |
| 27. | Druel T, Andeol Q, Rongieras F, Bertani A, Bordes M, Alvernhe A. Evaluation of containment measures' effect on orthopaedic trauma surgery during the COVID-19 pandemic: a retrospective comparison between 2019 and 2020. Int Orthop. 2020;44:2229-2234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Elbardesy H, Meagher E, Guerin S. Impact of the COVID-19 pandemic on the trauma and orthopaedic department at level one Major Trauma Centre in the republic of Ireland. Acta Orthop Belg. 2021;87:571-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Andreozzi V, Marzilli F, Muselli M, Previ L, Cantagalli MR, Princi G, Ferretti A. The impact of COVID-19 on orthopaedic trauma: A retrospective comparative study from a single university hospital in Italy. Orthop Rev (Pavia). 2020;12:8941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Kalem M, Kocaoğlu H, Merter A, Karaca MO, Özbek EA, Kınık HH. Effects of COVID-19 pandemic curfew on orthopedic trauma in a tertiary care hospital in Turkey. Acta Orthop Traumatol Turc. 2021;55:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Clough TM, Shah N, Divecha H, Talwalkar S. COVID-19 consent and return to elective orthopaedic surgery: allowing a true patient choice? Bone Jt Open. 2020;1:556-561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Kale NN, Patel AH, Leddy MJ 3rd, Savoie FH 3rd, Sherman WF. The Effect of COVID-19 on Orthopedic Practices and Surgeons in Louisiana. Orthopedics. 2020;43:351-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Meng Y, Leng K, Shan L, Guo M, Zhou J, Tian Q, Hai Y. A clinical pathway for pre-operative screening of COVID-19 and its influence on clinical outcome in patients with traumatic fractures. Int Orthop. 2020;44:1549-1555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Patel BA, Green SF, Henessy C, Adamu-Biu F, Davda K, Chennagiri R, Kankate R, Ghani Y. Lessons Learnt from Managing Orthopaedic Trauma During the First Wave of the COVID-19 Pandemic at a UK District General Hospital. Indian J Orthop. 2021;1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Gupta R, Singhal A, Kapoor A, Dhillon M, Masih GD. Effect of COVID-19 on surgical management of open fractures and infection rates: A tertiary care experience in Indian set-up. J Clin Orthop Trauma. 2021;12:16-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Saini N, Ranjan R, Jain VK, Shukla A. Pooling of neglected and delayed trauma patients - Consequences of 'lockdown' and 'Unlock' phases of COVID-19 pandemic- A retrospective cohort analysis from a tertiary centre. J Clin Orthop Trauma. 2021;21:101533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Balakumar B, Nandra RS, Woffenden H, Atkin B, Mahmood A, Cooper G, Cooper J, Hindle P. Mortality risk of surgically managing orthopaedic trauma during the COVID-19 pandemic. Bone Jt Open. 2021;2:330-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Paul RW, Omari A, Fliegel B, Bishop ME, Erickson BJ, Alberta FG. Effect of COVID-19 on Ulnar Collateral Ligament Reconstruction in Major League Baseball Pitchers. Orthop J Sports Med. 2021;9:23259671211041359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Yu P, Wu C, Zhuang C, Ye T, Zhang Y, Liu J, Wang L. The patterns and management of fracture patients under COVID-19 outbreak in China. Ann Transl Med. 2020;8:932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 40. | McMaster T, Wright T, Mori K, Stelmach W, To H. Current and future use of telemedicine in surgical clinics during and beyond COVID-19: A narrative review. Ann Med Surg (Lond). 2021;66:102378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |