Published online Oct 18, 2022. doi: 10.5312/wjo.v13.i10.921
Peer-review started: May 8, 2022
First decision: August 4, 2022
Revised: August 17, 2022
Accepted: September 23, 2022
Article in press: September 23, 2022
Published online: October 18, 2022
Processing time: 161 Days and 12.8 Hours
Coronavirus disease 2019 (COVID-19) has necessitated adaptations in local trauma services, with implementation of novel methods of practice, strategic adaptations, and shifting of resource management. Many of these may serve the driver for landmark changes to future healthcare provision.
To analyse the impact of COVID-19 on service provision by comparing throughput and productivity metrics with preceding years to identify differences in practice that were successful, cost-effective, and sustainable.
We quantified orthopaedic trauma care provision at a single University Teaching Hospital over a three consecutive year period, from 1st January 2018 to 31st December 2020. Each year was split into four phases based on the 2020 national COVID-19 pandemic periods. We quantitatively analysed change in rates of inpatient trauma operative case load, sub-specialty variation, theatre throughput, and changes in management strategy. Qualitative analysis was based on multidisciplinary team interviews to highlight changes to care pathways.
Of 1704 cases were admitted in 2020, 11.9% and 12.4% fewer than 2019 and 2018, respectively. During phase 1, hip fractures encompassed the majority (48.8%) of trauma throughput, with all other subspecialties seeing a reduction. Mean length of stay was shorter during phase 1 (5.7 d); however, the time in theatre was longer (144.3 min). Both, Charlson (0.90) and Elixhauser (1.55) Comorbidity Indices indicated the most co-morbid admissions during 2020 phase 1.
COVID-19 has resulted in a paradigm shift in how care is accessed and delivered, with many evolving changes and adaptations likely to leave an impression upon healthcare provision in the future.
Core Tip: Based on our findings, we have made several recommendations that we will adopt locally going forward. We encourage other teams facing similar challenges to consider these factors to improve the care of trauma patients: (1) Dynamic elective approaches to care can reduce length of stay (LOS): The ‘elective mindset’ of the elective hospital nursing/physical therapy/occupational therapy teams yielded more expeditious post-operative rehabilitation our trauma patients, ensuring faster optimisation of a more co-morbid cohort of patients and reduced LOS; (2) Sustain the rising trend in safe non-operative management to reduce inpatient workload: This was a trend particularly observed in hand and wrist/foot and ankle trauma where the care pathways were altered in the face of rising coronavirus disease 2019 cases; and (3) Maintaining rapid re-education of skills: By rapidly adopting locally-relevant versions of national guidance and developing standardised algorithms and training pathways.
- Citation: Kulkarni K, Shah R, Mangwani J, Ullah A, Gabbar O, James E, Dias J. Utilising the impact of COVID-19 on trauma throughput to adapt elective care models for more efficient trauma care. World J Orthop 2022; 13(10): 921-931
- URL: https://www.wjgnet.com/2218-5836/full/v13/i10/921.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i10.921
The coronavirus disease 2019 (COVID-19) pandemic has significantly impacted the provision of healthcare globally. Not only were elective planned care services largely paused, but ongoing essential services, such as trauma, had to adapt their ways of working to maintain safety for patients and healthcare professionals[1].
With the National Health Service (NHS) slow to effect change, these COVID-19 necessitated adap
With this in mind, we sought to gain an in-depth view of the impact of COVID-19 on our local trauma service provision, by comparing our trauma throughput and other key productivity metrics with the preceding years to identify any key differences and adaptations that had occurred within the department to sustain clinical practice. By evaluating changes to practices implemented due to COVID-19 at our trauma unit, our goal was to evaluate those changes that were successful, cost-effective, easily adapted by clinicians, and deemed sustainable for the future, with a view to sharing our learnings more widely.
We performed a comprehensive retrospective analysis of the objective impact of COVID-19 on our local trauma service provision, by comparing 2020 metrics with the equivalent 12-mo time periods in both 2019 and 2018. This study was formally registered and approved by our (KK1) Clinical Audit and Quality Improvement Team. The specific aspects of care provision we sought to evaluate included: (1) Change in rates of inpatient trauma case load; (2) Sub-specialty variation in trauma case load; (3) Theatre throughput (numbers of cases, duration, turnaround time); (4) Changes in trends in trauma management (particularly rates of non-operative interventions); and (5) Changes to local strategy to care delivery.
Comparison of all trauma clinical activity at the Orthopaedic Trauma Unit of a single United Kingdom University Teaching Hospital over a three consecutive year period, from 1st January 2018 to 31st December 2020 (i.e., 2018, 2019, 2020). For the purpose of this evaluation, each year was split into four phases based upon the main national COVID-19 pandemic periods in 2021 (Table 1).
| Phase | Description | Dates | Days |
| Phase 0 | Pre-lockdown | 1st January - 22nd March | 81 |
| Phase 1 | Lockdown | 23rd March - 31st May | 70 |
| Phase 2 | Post-lockdown | 1st June - 30st September | 122 |
| Phase 3 | To year end | 1st October - 31st December | 92 |
Data was obtained using the Hospital Information Support System (HISS) specifically coded for Trauma and Orthopaedics (HISS code 10). This data included information on patient co-morbidities [converted to Charlson Comorbidity Index (CCI)], patient demographic and mortality data. Operative data and timings were obtained using our Operating Theatre Software (ORMIS, code 10) and cross-referenced with a manually maintained Microsoft Excel (v16.46) encrypted spreadsheet of cases booked for theatre by our Trauma Coordinators. Descriptions of changes to patient care pathways were obtained through interviews of the multidisciplinary team (MDT), including senior management, Orthopaedic and Orthogeriatric clinicians, and ward teams (nursing and therapy).
Rates of all trauma caseload management across the three years, including a breakdown of: (1) Variation in total trauma throughput each year by phase; (2) Variation in specific subspecialty trauma by phase (subspecialties included: Hip, knee, foot and ankle, hand & wrist, shoulder, elbow, and complex multi-site); (3) CCI, Elixhauser Comorbidity Sum Index (ECI); (4) Inpatient length of stay (LOS); and (4) For operated cases, the time interval & delay to treatment (i.e., from admission time to surgery start time).
Descriptive statistics were presented as means ± SD. Qualitative analysis of interviews was performed to group the key changes to care pathways. The quantitative data was then analysed in the context of changes to practice, with a view to identifying sustainable interventions to maintain going forward.
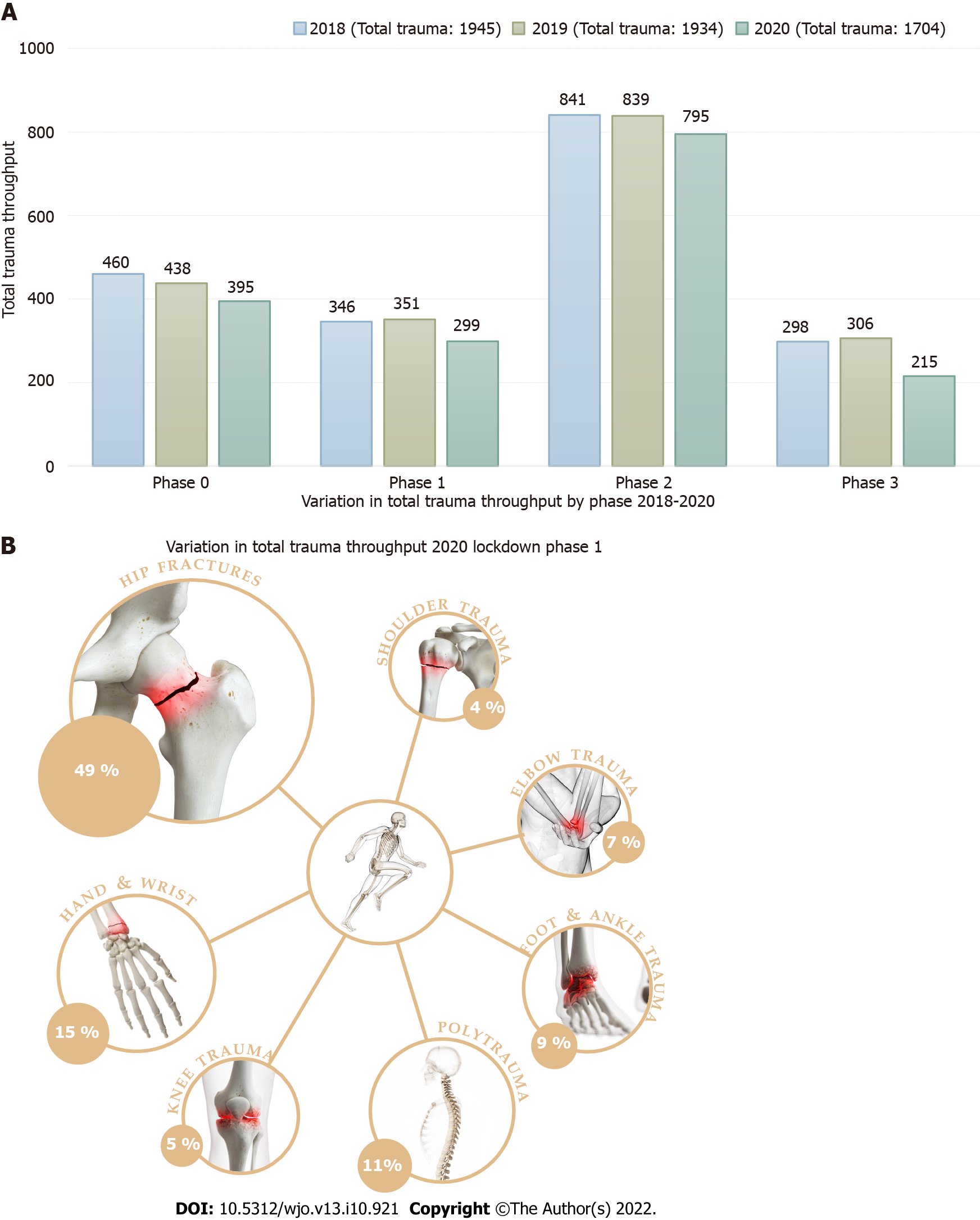
A total of 1704 trauma cases were admitted to our trauma unit in 2020. This was 11.9% fewer than in 2019 (1934 cases) and 12.4% fewer than in 2018 (1945 cases) (Table 2). Figure 1A highlights the variation in total trauma throughput by phase.
| Subspecialty | Year | Phase 0 | Phase 1 | Phase 2 | Phase 3 | Total |
| Pre-lockdown | Lockdown | Post-lockdown | To year end | |||
| Hip | 2018 | 183 (39.8%) | 131 (37.9%) | 311 (37.0%) | 118 (39.6%) | 743 (38.2%) |
| 2019 | 172 (39.3%) | 146 (41.6%) | 339 (40.4%) | 139 (45.4%) | 796 (41.2%) | |
| 2020 | 163 (41.3%) | 146 (48.8%) | 291 (36.6%) | 76 (35.3%) | 676 (39.7%) | |
| Knee | 2018 | 26 (5.7%) | 14 (4.0%) | 47 (5.6%) | 16 (5.4%) | 103 (5.3%) |
| 2019 | 37 (8.4%) | 24 (6.8%) | 53 (6.3%) | 27 (8.8%) | 141 (7.3%) | |
| 2020 | 36 (9.1%) | 16 (5.4%) | 55 (6.9%) | 7 (3.3%) | 114 (6.7%) | |
| Foot & ankle | 2018 | 69 (15.0%) | 60 (17.3%) | 120 (14.3%) | 45 (15.1%) | 294 (15.1%) |
| 2019 | 65 (14.8%) | 47 (13.4%) | 102 (12.2%) | 39 (12.7%) | 253 (13.1%) | |
| 2020 | 45 (11.4%) | 26 (8.7%) | 98 (12.3%) | 36 (16.7%) | 205 (12.0%) | |
| Hand & wrist | 2018 | 70 (15.2%) | 53 (15.3%) | 148 (17.6%) | 51 (17.1%) | 322 (16.6%) |
| 2019 | 58 (13.2%) | 54 (15.4%) | 149 (17.8%) | 33 (10.8%) | 294 (15.2%) | |
| 2020 | 60 (15.2%) | 44 (14.7%) | 147 (18.5%) | 42 (19.5%) | 293 (17.2%) | |
| Shoulder | 2018 | 27 (5.9%) | 25 (7.2%) | 45 (5.4%) | 20 (6.7%) | 117 (6.0%) |
| 2019 | 30 (6.8%) | 22 (6.3%) | 47 (5.6%) | 21 (6.9%) | 120 (6.2%) | |
| 2020 | 27 (6.8%) | 13 (4.3%) | 52 (6.5%) | 21 (9.8%) | 113 (6.6%) | |
| Elbow | 2018 | 32 (7.0%) | 32 (9.2%) | 87 (10.3%) | 16 (5.4%) | 167 (8.6%) |
| 2019 | 29 (6.6%) | 19 (5.4%) | 62 (7.4%) | 12 (3.9%) | 122 (6.3%) | |
| 2020 | 24 (6.1%) | 21 (7.0%) | 75 (9.4%) | 15 (7.0%) | 135 (7.9%) | |
| Complex multi-site | 2018 | 16 (3.5%) | 8 (2.3%) | 16 (1.9%) | 7 (2.3%) | 47 (2.4%) |
| 2019 | 4 (0.9%) | 7 (2.0%) | 14 (1.7%) | 7 (2.3%) | 32 (1.7%) | |
| 2020 | 4 (1.0%) | 1 (0.3%) | 9 (1.1%) | 3 (1.4%) | 17 (1.0%) | |
| Polytrauma | 2018 | 37 (8.0%) | 23 (6.6%) | 67 (8.0%) | 25 (8.4%) | 152 (7.8%) |
| 2019 | 43 (9.8%) | 32 (9.1%) | 73 (8.7%) | 28 (9.2%) | 176 (9.1%) | |
| 2020 | 36 (9.1%) | 32 (10.7%) | 68 (8.6%) | 15 (7.0%) | 151 (8.9%) |
Table 2 highlight the variation in subspecialty trauma for phases 0-3 for each year investigated. During the 2020 lockdown (phase 1), hip fractures remained the bulk (48.4%) of the surgical workload. This was a slightly higher proportion than in 2019 (41.6%), and 2018 (37.9%). Absolute numbers for hip trauma remained equivalent (146 procedures). Figure 1B highlights the variation in trauma load during the lockdown period. Conversely, we noted a reduction in foot and ankle procedures during phase 1 in 2020 (26 procedures; 8.7% of overall workload) compared to 2019 (47 procedures; 13.4% of overall workload) and 2018 (60 procedures; 17.3% of overall workload). Similar reductions were noted for hand and wrist trauma in 2020 (44 procedures; 14.7% of overall workload) compared to 2019 (54 procedures; 15.4% of overall workload) and 2018 (53 procedures; 15.3% of overall workload). In 2020, surgical throughput during lockdown phase 1 was lower by 52 procedures than 2019 and by 47 in comparison to 2018. Additionally, all subspecialties, except for hips (146 procedures in both 2020 and 2019) and elbows (21 procedures in 2020, 19 in 2019), saw a reduction in absolute procedural numbers in comparison to 2019.
Tables 3-5 highlight the variation in patient demographic, LOS, comorbidity indices, and theatre parameters from 2018 to 2020. More detailed breakdown of variation is presented in Supplementary Tables 1-3. The mean LOS was significantly shorter during the 2020 phase 1 (lockdown phase) (5.7 d) compared to 2019 (7.5 d) and 2018 (6.8 d). CCI[6], which encompasses 19 medical conditions and is the most widely used comorbidity risk adjustment model for Orthopaedic surgery, showed a higher mean index during the 2020 lockdown (0.90) compared to 2019 (0.84) and 2018 (0.65). These findings were replicated using the ECI[7], which utilises 31 conditions, highlighting more co-morbid patients during phase 1 in 2020 [1.55 vs 1.36 (2019) vs 1.09 (2018)].
| Phase 0 (n = 709) | Phase 1 (n = 571) | Phase 2 (n = 1363) | Phase 3 (n = 486) | Total (n = 3129) | |
| mean ± SD | |||||
| Age at injury | 61.23 ± 22.40 | 56.40 ± 24.04 | 57.52 ± 24.36 | 59.06 ± 23.79 | 58.39 ± 23.83 |
| Length of spell (d) | 8.39 ± 10.31 | 6.84 ± 8.57 | 6.76 ± 10.19 | 7.02 ± 9.45 | 7.18 ± 9.84 |
| Charlson Comorbidity Index | 0.72 ± 1.31 | 0.65 ± 1.24 | 0.68 ± 1.26 | 0.60 ± 1.21 | 0.67 ± 1.26 |
| Elixhauser Comorbidity Index | 1.19 ± 1.39 | 1.09 ± 1.36 | 1.14 ± 1.38 | 1.06 ± 1.31 | 1.13 ± 1.37 |
| Hours to surgery | 29.24 ± 50.75 | 31.46 ± 48.29 | 34.72 ± 91.27 | 26.22 ± 52.95 | 31.54 ± 71.10 |
| Time in theatre | 98.59 ± 58.34 | 92.86 ± 48.23 | 94.33 ± 46.30 | 95.49 ± 48.66 | 95.23 ± 50.04 |
| Time in theatre/recovery | 61.23 ± 22.40 | 56.40 ± 24.04 | 57.52 ± 24.36 | 59.06 ± 23.79 | 58.39 ± 23.83 |
| Sex: Female | 383 ± 54.0% | 296 ± 51.8% | 726 ± 53.3% | 249 ± 51.2% | 1654 ± 52.9% |
| Sex: Male | 326 ± 46.0% | 275 ± 48.2% | 637 ± 46.7% | 237 ± 48.8% | 1475 ± 47.1% |
| Phase 0 (n = 664) | Phase 1 (n = 563) | Phase 2 (n = 1315) | Phase 3 (n = 471) | Total (n = 3013) | |
| mean ± SD | |||||
| Age at injury | 58.89 ± 24.03 | 60.66 ± 23.17 | 58.66 ± 23.95 | 61.11 ± 22.98 | 59.47 ± 23.68 |
| Length of spell (d) | 7.30 ± 8.05 | 7.50 ± 9.90 | 6.67 ± 8.60 | 8.01 ± 10.88 | 7.18 ± 9.14 |
| Charlson Comorbidity Index | 0.71 ± 1.28 | 0.84 ± 1.49 | 0.78 ± 1.35 | 0.77 ± 1.30 | 0.77 ± 1.35 |
| Elixhauser Comorbidity Index | 1.20 ± 1.38 | 1.36 ± 1.55 | 1.39 ± 1.53 | 1.34 ± 1.42 | 1.33 ± 1.49 |
| Hours to surgery | 32.02 ± 57.64 | 32.13 ± 51.56 | 29.17 ± 47.03 | 31.96 ± 56.83 | 30.79 ± 51.99 |
| Time in theatre | 101.03 ± 49.49 | 96.30 ± 67.04 | 94.85 ± 57.61 | 95.95 ± 47.63 | 96.64 ± 56.36 |
| Time in theatre/recovery | 213.08 ± 110.23 | 208.29 ± 115.17 | 214.99 ± 141.51 | 228.39 ± 146.20 | 215.56 ± 131.70 |
| Sex: Female | 332 ± 50.0% | 291 ± 51.7% | 675 ± 51.3% | 239 ± 50.7% | 1537 ± 51.0% |
| Sex: Male | 332 ± 50.0% | 272 ± 48.3% | 640 ± 48.7% | 232 ± 49.3% | 1476 ± 49.0% |
| Phase 0 (n = 640) | Phase 1 (n = 425) | Phase 2 (n = 1210) | Phase 3 (n = 413) | Total (n = 2688) | |
| mean ± SD | |||||
| Age at injury | 59.46 ± 23.95 | 62.16 ± 23.61 | 57.70 ± 24.07 | 60.97 ± 23.47 | 59.33 ± 23.93 |
| Length of spell (d) | 7.05 ± 7.87 | 5.69 ± 5.90 | 5.71 ± 7.54 | 7.53 ± 8.86 | 6.30 ± 7.64 |
| Charlson Comorbidity Index | 0.77 ± 1.23 | 0.90 ± 1.45 | 0.68 ± 1.19 | 0.68 ± 1.25 | 0.73 ± 1.26 |
| Elixhauser Comorbidity Index | 1.27 ± 1.46 | 1.55 ± 1.63 | 1.21 ± 1.37 | 1.19 ± 1.39 | 1.28 ± 1.44 |
| Hours to surgery | 30.71 ± 49.37 | 30.84 ± 34.56 | 24.50 ± 37.98 | 24.59 ± 37.14 | 26.97 ± 40.41 |
| Time in theatre | 95.62 ± 50.10 | 144.25 ± 64.24 | 127.98 ± 54.37 | 123.20 ± 54.48 | 122.11 ± 57.35 |
| Time in theatre/recovery | 215.97 ± 124.31 | 175.22 ± 117.92 | 195.23 ± 106.09 | 203.28 ± 132.37 | 199.65 ± 117.42 |
| Sex: Female | 347 ± 54.2% | 237 ± 55.8% | 649 ± 53.6% | 234 ± 56.7% | 1467 ± 54.6% |
| Sex: Male | 293 ± 45.8% | 188 ± 44.2% | 561 ± 46.4% | 179 ± 43.3% | 1221 ± 45.4% |
The ‘hours to surgery’ metric was calculated from the decision to admit the patient to hospital to the time to surgery. There was no significant variation between the three years for both phase 0 (30.7 h vs 32.0 h vs 29.2 h) and phase 1 (30.8 h vs 32.1 h vs 31.5 h). However, the actual time in theatre (en
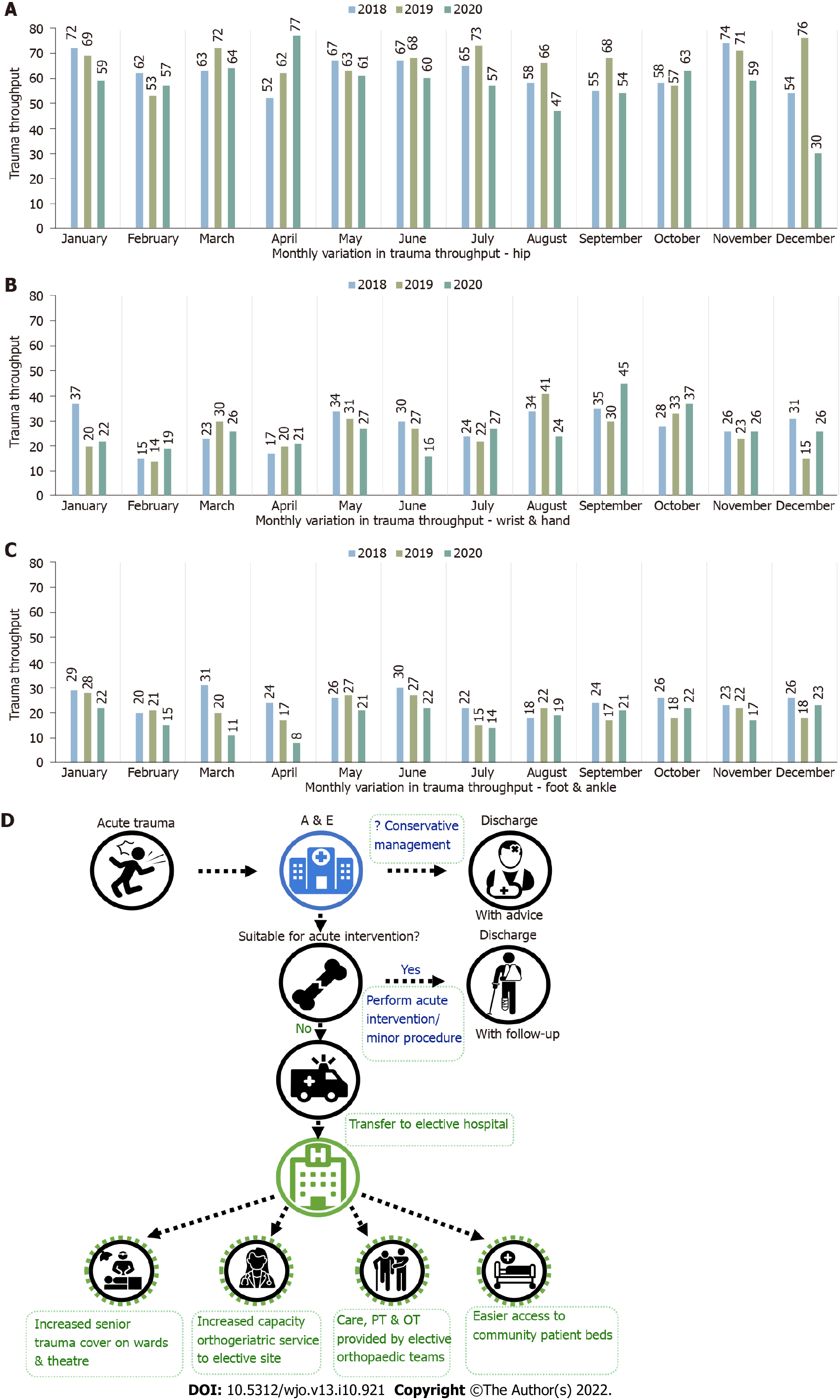
Figures 2A-C highlight the monthly variation in the highest throughput trauma sub-specialties (hip, hand & wrist, and foot & ankle). Consistent with previous years, hip fracture surgery encompassed the bulk of monthly surgical trauma, including the period affected by the COVID-19 pandemic. Supplementary Figures 1-4 highlights monthly variation in the remainder of the sub-specialties.
The pandemic ushered in several significant changes to the way in which trauma care was delivered (Figure 2D). Alongside the key changes described below, other changes that impacted our department included partial redeployment of all Orthopaedic Specialty Registrars to the intensive care units, and cessation of all but selected urgent elective cases (e.g., infected arthroplasty). Structured colleague interviews provided valuable MDT insight into what worked, and what was less successful.
Trauma care shift to our elective site: Patients requiring admission from the emergency department (ED) at our acute site were transferred by ambulance to our elective orthopaedic site to free capacity for COVID-19 admissions. Clinical staffing cover was accordingly adapted to ensure patient safety and prompt senior decision making. This transition was made swiftly and successfully as soon as elective activity was suspended, also lowering the exposure of our trauma patients to COVID-19.
Ward based nursing care and therapy provided by elective orthopaedic teams: The strategies adopted by these teams included similar protocols to the equivalent elective group (e.g., early mobilisation regimes for total hip replacement patients applied following hip fracture surgery). Adopting more ‘dynamic’ approaches, with multiple therapy sessions per day, helped get patients safely mobilising sooner and facilitated discharge.
Transfer of increased capacity orthogeriatric service to elective site: Daily consultant-led ward-rounds facilitated rapid pre-operative stabilisation of patients with fragility femur fractures, alongside reduced surgical delay and LOS.
Easier access to community patient beds: Facilitated in conjunction with our community teams, a rapid electronic referral method was adopted during the pandemic, accelerating the request process for community beds and enabling more rapid discharge of patients that were ‘medically’ well but in need of rehabilitation prior to discharge home.
Increased senior trauma cover: Trauma care was led by a combination of our elective and trauma orthopaedic consultants and higher specialty trainees, working flexibly as required, with shadow rotas made to provide enhanced sickness cover. Whereas our usual trauma care is led by individual consultants’ teams, supported by a supporting ‘hot’ floating consultant, the COVID-19 strategy involved a named consultant providing daily ward rounds of all admitted trauma patients, 7-d a week. This allowed issues to be identified and addressed early. In particular, weekend inpatient reviews facilitated on-day weekend discharges and preparation for anticipated Monday discharges.
Virtual clinics: While face-to-face elective clinics were significantly reduced, virtual telephone consultations were adopted. These were initially successfully applied to elective care, and thereafter to our trauma fracture clinics, enabling these acute services to reduce face-to-face contact, while maintaining overall throughput.
The COVID-19 pandemic has had a significant impact on both, our clinical ability to effectively manage trauma, as well as the way in which our patients have accessed trauma care. This has resulted in a paradigm shift in practice for the delivery of our trauma service, with many evolving changes and adaptations likely to leave their impression upon how healthcare will be provided in the future. Several centres across the United Kingdom.
This service evaluation project provided a quantitative and qualitative assessment of collective trauma throughput during four pre-determined phases, comparing throughput with the same periods in 2019 and 2018. Evaluation of phase 1 (i.e., the ‘lockdown’ phase spanning 70 d) highlighted several important learning points. One of the expected key findings was that overall trauma throughput during phase 1 was reduced compared to 2019 and 2018 (299 procedures in vs 351 and 346, respectively). Despite this, hip fragility fracture numbers remained static at 146 procedures in both 2020 and 2019, still accounting for the bulk of the surgical workload during the lockdown phase (48.8% vs 41.6% vs 37.9%). There was a 45% reduction in the number of foot and ankle procedures between the 2020 phase 1 and its equivalent in 2019 as well as 2018 (26 procedures vs 47 vs 60). Similarly, hand procedures saw a 19% reduction compared to 2019 and 2018 (44 procedures vs 54 vs 53). There was no variation in polytrauma in phase 1 between 2020 and 2019 (32 cases).
Interpretation of these findings are suggestive of a reduction in overall emergency trauma presentations (which was anticipated in view of United Kingdom Government restrictions) and a shift towards more conservative measures for selective trauma, in keeping with updated national COVID-19 British Orthopaedic Association Standards for Trauma guidance[8]. For certain subspecialties (for example, foot and ankle, or hand and wrist), the nature of the trauma was conducive to more early interventions performed at presentation in the ED, without the need for admission and operative intervention.
A decrease was also observed in the overall mean LOS during phase 1 (5.69 d vs 7.50 vs 6.84). While successful approaches to determine (and reduce) the LOS through hospital are determined on mapping patient flow, replicating and understanding care models adopted by subspecialties during phase 1 to facilitate early discharge could have significant long-term benefits. Reducing the LOS has the potential to provide an effective means of containing and bridging the gap between service demand and resource constraints, particularly during the pandemic. Maintained orthogeriatric ward cover, daily consultant ward presence, and improved availability of community beds played important roles in ensuring efficient management of hip fracture patients - the majority of the patient mix - and therefore those contributing most to LOS. Fewer outliers also facilitated more efficient patient management. Best Practice Tariffs for hip fragility fractures require prompt surgery and appropriate orthogeriatric involvement - both factors contributing to a shorter LOS[9]. Phase 1 in 2020 demonstrated a shorter LOS for these patients; if maintained in the post-COVID era, this could result in improved care and resource benefits for our trust.
Both the CCI and the ECI are useful tools to quantify the underlying comorbid disease status. Both indices were raised for the 2020 phase 1 cohort (CCI - 0.90 vs 0.84 vs 0.65; ECI - 1.55 vs 1.36 vs 1.09), suggesting that trauma service had more multi-morbid patients with non-communicable disease admitted and operated during the lockdown phase, whist the ‘fitter’ cohort stayed at home. This also correlates with the fact that hip fragility fracture surgery numbers remained static between 2019 and 2020. One theory to account for this is that the lockdown may have resulted in an overall reduction in the support system offered to vulnerable and multimorbid patients, who therefore had to manage in isolation, increasing their likelihood of sustaining a serious injury requiring operative intervention.
We recognise that our study has several limitations. While every attempt was made to capture all trauma admissions, the total figures do not encompass all trauma presentations to the ED (for example, those patients who had interventions at presentation in ED and were subsequently discharged or followed up in clinic). However, we are confident that our figures do indeed represent the majority of inpatient trauma admissions. We were also potentially limited by the accuracy of coding of admitted patients and HISS data, which in turn would affect parameters such as the comorbidity indices. Finally, the local hospitals found themselves in an unusual position where partial restrictions were imposed for an extended period of time (54 d) due to the Leicestershire region being a higher risk area, which overlapped with phase 2, resulting in a lack of clear distinction between these phases.
Based on our findings, we have made several recommendations that we will adopt locally going forward. We encourage other teams facing similar challenges to consider these factors to improve the care of trauma patients.
Dynamic elective approaches to care can reduce LOS: The ‘elective mindset’ of the LGH nursing/ physical therapy/occupational therapy teams yielded more expeditious post-operative rehabilitation our trauma patients, ensuring more rapid optimisation of a more comorbid cohort of patients and reduced LOS during phases 1 and 2.
Sustain the rising trend in safe non-operative management to reduce inpatient workload: This was a trend particularly observed in hand and wrist/foot and ankle trauma where the care pathways were altered in the face of rising COVID-19 cases. We have since capitalised upon this opportunity to change our combined ED fracture management pathways for certain injuries to facilitate an increase the number of interventions and minor procedures performed at presentation at the front door under either ketamine or Penthrox® (Methoxyflurane), utilising our 24-h availability of fluoroscopic guidance for adult patients with our mobile C-arm X-ray in fracture clinic.
Maintaining rapid re-education of skills: By rapidly adopting local versions of national PPE guidance and developing standardised algorithms and training pathways, we maintained the hours to surgery and the improvements in time in theatre metrics. Redeploying these training pathways via designated trained senior staff will be integral to a rapid response in the face of future challenges, including from another COVID-19 wave.
The impact of the COVID-19 pandemic on healthcare systems globally cannot be underestimated. As the growing body of evidence and best-practice advice during the pandemic evolves, clinical practices will undoubtedly need to adapt accordingly. Our study allowed us to evaluate, analyse, and compare local trauma throughput variation during the pandemic, thus developing targeted interventions utilising an ‘elective care model’. This culminated in a more streamlined trauma patient care pathway from admission to discharge. By incorporating these modifications to clinical practice into our ‘new normal’ of clinical practice, we hope to build on this opportunity from adversity to improve patient care going forward.
Coronavirus disease 2019 (COVID-19) has necessitated adaptations in local trauma services, with implementation of novel methods of practice, strategic changes, and shifting of resource management. Many of these changes may serve the driver for landmark changes to future healthcare provision. The pandemic environment is full of opportunities to capitalise upon to improve the flexibility of care provision for the benefits of both, patients and providers, with the ultimate aim of creating a long-term self-sustaining care model.
We sought to compare throughput and productivity metrics with preceding years to identify differences in practice that were successful, cost-effective, and sustainable. Should these changes prove successful, they may yield more sustained differences to the way we deliver care in the future.
By evaluating changes to practices implemented due to COVID-19 at our trauma unit, our goal was to evaluate those changes that were successful, cost-effective, easily adapted by clinicians, and deemed sustainable for the future, with a view to sharing our learnings more widely.
We performed a comprehensive retrospective analysis of the objective impact of COVID-19 on our local trauma service provision, by comparing 2020 metrics with the equivalent 12-mo time periods in both 2019 and 2018.
Of 1704 cases were admitted in 2020, 11.9% and 12.4% fewer than 2019 and 2018, respectively. Hip fractures remained the bulk of surgical workload at the height of the pandemic. Mean length of stay was shorter during phase 1 (5.7 d). The time in theatre was longer (144.3 min) as a consequence of COVID-19 related measures that were introduced into theatre practice. Only the most co-morbid patients were admitted into hospital during phase 1, indicated by higher Charlson (0.90) and Elixhauser Comorbidity Indices (1.55).
By evaluating, analysing, and comparing local trauma throughput variation during the pandemic, we developed targeted interventions utilising an ‘elective care model’ for more efficient trauma care.
COVID-19 has resulted in a paradigm shift in how care is accessed and delivered, with many evolving changes and adaptations likely to leave an impression upon healthcare provision in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ferreira GSA, Brazil; Mahmoud MZ, Saudi Arabia S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Bevan Brittan. Elective care in England. Assessing the impact of COVID-19 and where next. [cited 20 June 2022]. Available from: https://www.bevanbrittan.com/insights/articles/2020/elective-care-in-england-assessing-the-impact-of-covid-19-and-where-next/. |
| 2. | The Health Foundation. Constructive comfort: accelerating change in the NHS. [cited 20 June 2022]. Available from: https://www.health.org.uk/research-projects/constructive-comfort-accelerating-change-in-the-nhs. |
| 3. | Murphy T, Akehurst H, Mutimer J. Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury. 2020;51:2142-2147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | Madanipour S, Iranpour F, Goetz T, Khan S. COVID-19: lessons learnt and priorities in trauma and orthopaedic surgery. Ann R Coll Surg Engl. 2021;103:390-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Gibbons JP, Forman S, Keogh P, Curtin P, Kiely R, O'Leary G, Skerritt C, O'Sullivan K, Synnott K, Cashman JP, O'Byrne JM. Crisis change management during COVID-19 in the elective orthopaedic hospital: Easing the trauma burden of acute hospitals. Surgeon. 2021;19:e59-e66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38229] [Article Influence: 1006.0] [Reference Citation Analysis (0)] |
| 7. | Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6456] [Cited by in RCA: 7783] [Article Influence: 288.3] [Reference Citation Analysis (0)] |
| 8. | British Orthopaedic Association. Specialty and subspecialty guidance and resources during the COVID-19 pandemic. [cited 20 June 2022]. Available from: https://www.boa.ac.uk/latest-news/specialty-and-subspecialty-guidance-and-resources.html. |
| 9. | British Geriatrics Society. The Care of Patients with Fragility Fractures (Blue Book). [cited 20 June 2022]. Available from: https://www.bgs.org.uk/resources/care-of-patients-with-fragility-fracture-blue-book. |