Published online Jan 18, 2022. doi: 10.5312/wjo.v13.i1.70
Peer-review started: September 16, 2021
First decision: December 9, 2021
Revised: December 10, 2021
Accepted: January 11, 2022
Article in press: January 11, 2022
Published online: January 18, 2022
Processing time: 123 Days and 0.8 Hours
Coronavirus disease 2019 (COVID-19) has a major influence on all parts of society.
To examine the consequences of the national lockdown and political initiatives during the first surge of the COVID-19 pandemic expressed by changes in incidences of musculoskeletal paediatric injuries.
Study design was a retrospective multicenter cohort study. A ‘pandemic’ cohort was established from 16 March 2020 to 21 April 2020, where all institutions including day care and schools were closed. A ‘pre-pandemic’ cohort was established from the same period in 2019 for comparison. Included were all patients admitted at the emergency departments with paediatric musculoskeletal injuries (aged 0-15 years) identified by a relevant musculoskeletal ICD-10 diagnosis (DSxxx), concussions (DZ033D), or burns (DT2xx).
The ‘pre-pandemic’ cohort consisted of 2101 patients, and the ‘pandemic’ cohort consisted of 1070 patients, indicating a decrease of paediatric musculoskeletal injuries of 51%. The incidence of paediatric injury in the ‘pre-pandemic’ cohort was 10460/100000/year. In the ‘pandemic’ cohort, the incidence was 5344/100000/year.
A resource re-allocation to help serve the COVID-19 patients might be possible without reducing the level of care for injury-related paediatric patients.
Core Tip: Coronavirus disease 2019 (COVID-19) has had a significant impact on all parts of society and medical services. Here we compare the epidemiology of paediatric trauma at major university hospitals and rural hospitals before and during COVID-19 lockdown in 3171 emergency department contacts.
- Citation: Rasmussen MK, Larsen P, Rölfing JD, Kirkegaard BL, Thorninger R, Elsoe R. Epidemiology and incidence of paediatric orthopaedic trauma workload during the COVID-19 pandemic: A multicenter cohort study of 3171 patients. World J Orthop 2022; 13(1): 70-77
- URL: https://www.wjgnet.com/2218-5836/full/v13/i1/70.htm
- DOI: https://dx.doi.org/10.5312/wjo.v13.i1.70
From the first reported case of coronavirus disease 2019 (COVID-19) in December 2019 in Wuhan, China, the severe acute respiratory syndrome coronavirus 2 virus spread around the globe at a rapid pace. The World Health Organization declared it a global pandemic on 11 March 2020.
A national lockdown was issued on 11 March 2020 in Denmark, including prolonged closure of schools and the cessation of sporting activities, social activities, and other close-contact situations. The aetiology of paediatric injury is coherent to physical and sporting activities; hence a reduction in paediatric injuries and consultations at the emergency department was to be expected[1-4].
Several epidemiological studies before the COVID-19 pandemic have shown incidence rates of paediatric fracture of 1800-2000/100000/year[3-7]. However, a general overview of musculoskeletal injury treated at emergency departments is poorly reported[8]. To the authors' knowledge, only one former study examined musculoskeletal injuries seen at the emergency department using a population-based incidence rate and reported an incidence of 6300/100000/year[9].
Although current literature investigates the frequencies of paediatric injuries during the COVID-19 pandemic, no overview of the pandemic’s consequences of the pandemic on population-based incidences of paediatric injuries and related trauma mechanisms is available[10-15].
The present study aimed to examine the consequences of the national lockdown from 16 March till 21 April 2020 and political initiatives during the first surge of the COVID-19 pandemic expressed by changes in incidences of musculoskeletal paediatric injuries at the emergency departments across multiple hospitals. Furthermore, the aim was to examine changes in the mode of injury and related trauma mechanisms observed.
The study design was a retrospective cohort study investigating the incidence of paediatric musculoskeletal injuries in patients aged 0–15 years, before and during the national COVID-19 pandemic lockdown in the northern and middle parts of Denmark.
A ‘pandemic’ cohort was established from 16 March 2020 to 21 April 2020, where all institutions including day care and schools were closed. A ‘pre-pandemic’ cohort was established from the same period in 2019 for comparison.
Included were five regional hospitals and two university hospitals. The hospitals serve rural and suburban areas with a population of 198138 citizens between 0–15 years of age during the study period in 2019, representing the ‘pre-pandemic cohort’. The ‘pandemic’ cohort includes a population of 197516 citizens during the study period.
In Denmark, a unique possibility of performing population-based studies is present since Danish law requires all patient contact with hospitals and clinics to be registered in the Danish National Patient Register (DNPR)[16]. All Danish residents receive a civil registration number that is registered in the Civil Registration System. Hospital identification, date and time of hospitalization, and municipality are registered. Therefore, a complete registry of all health-related issues, both individual and population-based, is obtainable.
Based on the DNPR, the ‘pandemic’ and the ‘pre-pandemic’ cohorts were established for comparison.
Included were all patients admitted at the emergency departments with paediatric musculoskeletal injuries identified by a relevant musculoskeletal ICD-10 diagnosis (DSxxx), concussions (DZ033D), or burns (DT2xx).
Clinical information about diagnosis, age, gender, date, and mode of injury was obtained. Manual chart and X-ray review of 50% of the medical charts (n = 1546) was performed for validating the register data.
This study was conducted in accordance with the ethical standards of the responsible committee and with the ethical principles of the 1975 Declaration of Helsinki. The Danish Data Protection Agency approved the study. The reporting of the study complies with the Strengthening the Reporting of Observational Studies in Epidemiology Statement[17].
In total, 3171 paediatric injuries leading to an emergency department visit at one of the five hospitals were included in the study. The ‘pre-pandemic’ cohort consisted of 2101 patients, and the ‘pandemic’ cohort consisted of 1070 patients, indicating a decrease of paediatric musculoskeletal injuries in patients aged 0–15 years of 51% during the COVID-19 pandemic.
The overall incidence of paediatric injury in the ‘pre-pandemic’ cohort was 10460/100000/year. In the ‘pandemic’ cohort, the overall incidence was 5344/100000/year, indicating a twofold decrease in paediatric emergency patients during the COVID19 pandemic.
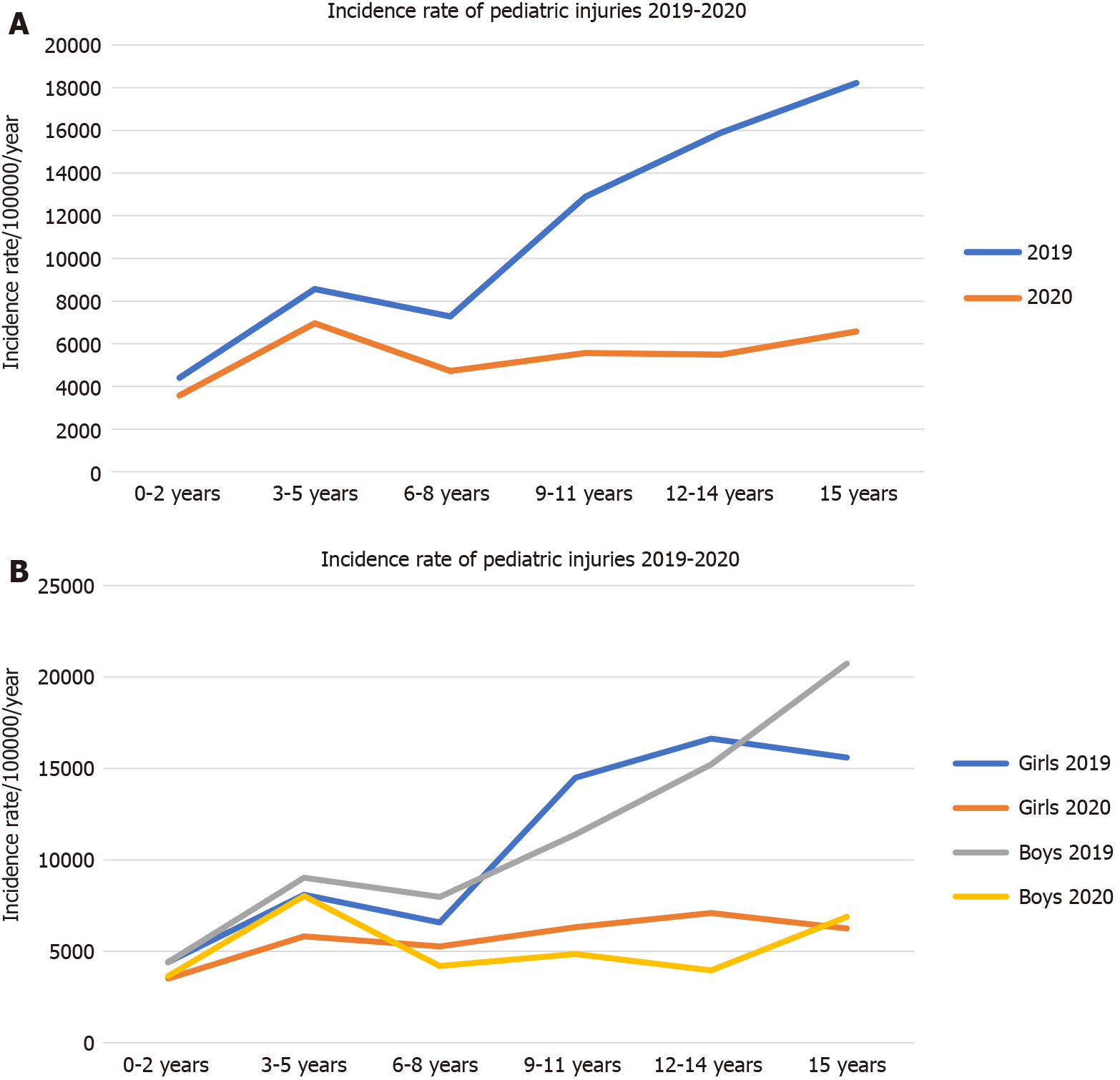
Gender-divided and age-specific incidence rates are depicted in Figure 1A and B. The incidence rates showed a similar bimodal trend for both genders. Before the pandemic the incidence rates were significantly higher in the age group from 9-15 years compared with the incidence during lockdown of the society (Figure 1A).
No differences were found in the proportion of the various diagnoses, with fractures being the most common in both cohorts. A higher proportion of injuries were found on school days in the ‘pre-pandemic’ cohort than the ‘pandemic’ cohort (Supplementary Table 1).
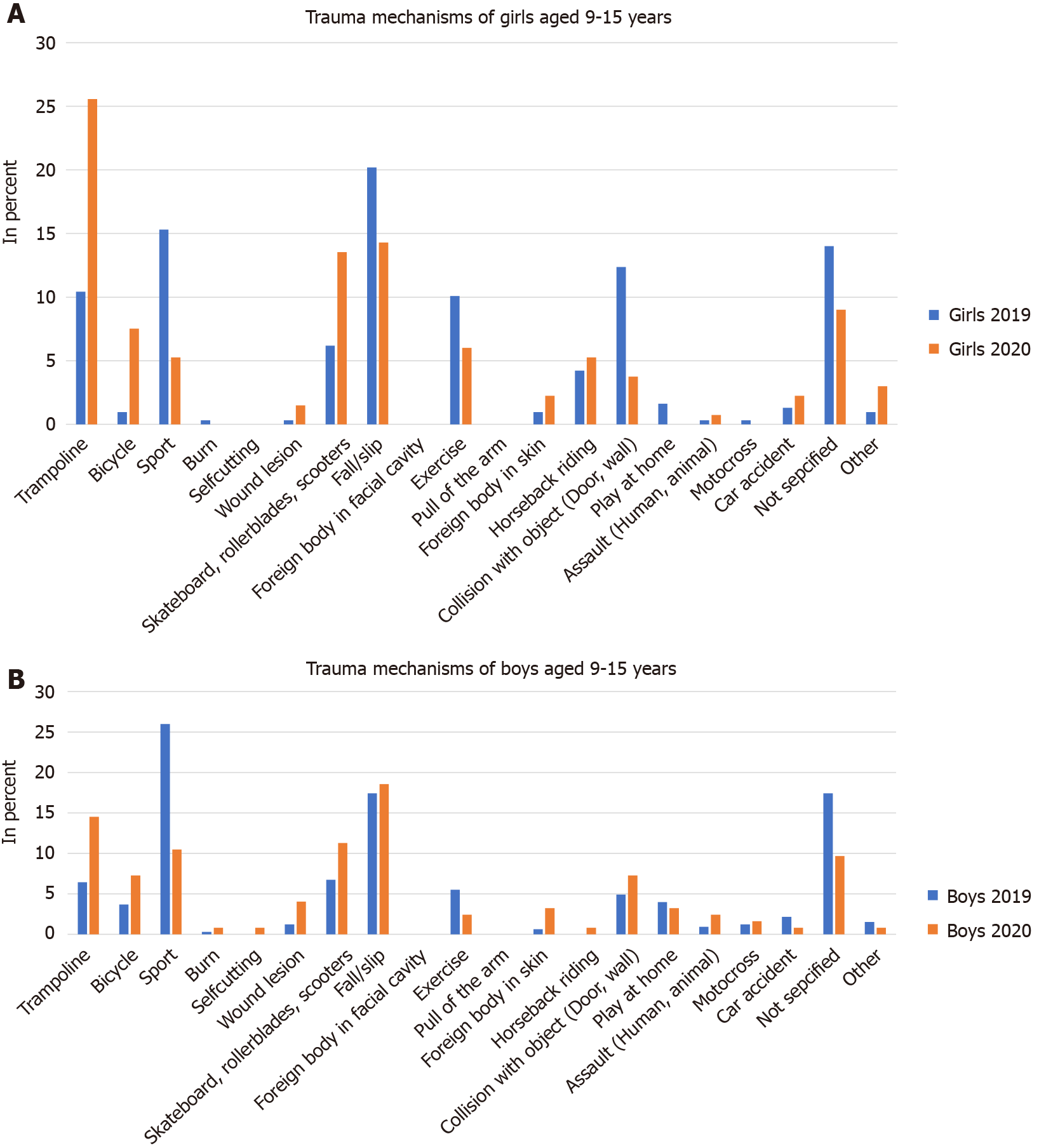
A proportional increase in bicycle (51%), skateboard, scooter, rollerblade (36 %), and trampoline injuries (98%) between the ‘pre-pandemic’ and the ‘pandemic’ cohorts was observed. A marked decrease in sports-related injuries and collisions with objects was observed in the ‘pandemic period’ compared to the pre-pandemic period. (Supplementary Table 2) In the age group 9–15 years of age (Figure 2A and B), a similar distribution was observed, indicating a shift in sporting activities to home-based activities.
The manual review of 50% of all contacts showed a high level of accuracy of both diagnosis (< 99%) and trauma mechanism (< 99%), indicating that register data are of very high quality.
The overall incidence rate for paediatric injury decreased two-fold during the COVID-19 national lockdown from 16 March 2020 – 21 April 2020 compared with the same weeks in 2019. The overall incidence was 10460/100000/year in 2019 and 5344/100000/year during the lockdown in 2020.
Results from the present study are supported by Sheridan et al[18], examining the effect of COVID-19 regulations using the incidence rate for paediatric trauma admissions in Ireland. A reduction of paediatric admissions from 0.146 admissions/ person-year to 0.139 admissions/person-year in the pandemic period was reported. Sheridan et al[18] reported on relatively small numbers, with only 28 paediatric patients included in the pandemic group. Most other studies evaluating the effect of the COVID-19 pandemic did not report on the incidence, making a further comparison of results from the present study difficult.
Several studies examined the effect of the COVID-19 Lockdown with regards to the prevalence and found a decrease between 33%-68% of paediatric fractures[10-13]. These results align with the present study reporting a decrease of paediatric musculoskeletal injuries in patients aged 0–15 years of 51% during the COVID-19 pandemic.
The age-specific incidence rates showed a bimodal distribution. Children below nine years of age showed similar distributions between the ‘pandemic’ and the ‘pre-pandemic’ cohorts. In contrast, children above nine years of age in the ‘pandemic’ cohort showed a marked decrease in the incidence rates during the COVID-19 Lockdown. This pattern was similar for both genders.
These findings are corroborated by Bram et al[10] and Keays et al[14], reporting that the prevalence of paediatric fracture and injury-related emergency department visits decreased the most in children above 12 years of age during the COVID-19 pandemic. The observed decrease in the incidence in the adolescent populations during the COVID-19 pandemic may be due to a reduction in sporting activities and social activities compared to the younger children.
The distribution of paediatric musculoskeletal injuries in patients aged 0–15 years was almost comparable between the ‘pre-pandemic’ and the ‘pandemic’ cohorts. The most common diagnose was fracture (2019: 34.0%, 2020: 33.9%) followed by contusion (2019: 19.2%, 2020: 16.2%) and distortion (2019: 18.5%, 2020: 14.3%).
Several studies report change in the distribution of trauma mechanisms during the COVID-19 pandemic[10-12,14]. The present study showed that a higher proportion of injuries in the ‘pandemic’ cohort was caused by trampoline, bicycling, skateboarding, scooters, and rollerblades compared to the ‘pre-pandemic’ cohort. Furthermore, a lower proportion of injuries was due to other sporting activities and exercise. Keays et al[14] reported a proportional rise in bicycling injuries in the pandemic period, but no change in injuries caused by trampoline, skateboarding, and scootering. Bram et al[10] reported an increase in the proportion of injuries during the COVID-19 pandemic occurring at home or on bicycles and a decrease in those related to sports. Other studies reported a reduction of injuries related to sports during the pandemic period[11-12]. These observed small differences between studies may be explained by differences in lockdown procedures in the different countries, influencing the closure of schools, cessation of sporting activities, social activities, and other close contact situations. Furthermore, regardless of the COVID-19 pandemic, differences in trauma mechanisms between different countries are well-known.
At present, the health care system worldwide is strained due to a large number of patients with COVID-19. A simultaneous reduction in paediatric injuries is observed and well reported. A resource re-allocation to help serve the COVID-19 patients might be possible without reducing the level of care for injury-related paediatric patients. This knowledge could benefit the health care system in a future pandemic. Conversely, when reopening schools and returning to sports, an increase in emergency department visits by paediatric patients is to be expected.
The significant drop in incidence of pediatric injuries during the COVID-19 pandemic may indicates that safety priority issues and the development of prevention strategies may be needed. Guardians may help children to adhere to safety recommendations at play grounds, such as a maximum of one child per trampoline. However, most pediatric musculoskeletal injuries are minor and not complicated. The impact of COVID-19 on children and young people’s mental health and well-being has been reported to weigh heavily[19]. The disruption to routines, education, recreation, as well as concern for family income and health, is leaving many young people with significant consequences due to the lock down. Furthermore, the lock down has been reported to significant decrease the level of children’s physical activity[20]. Regular physical activity is well-known to improve cardiorespiratory fitness, build strong bones and muscles, control weight, reduce symptoms of depression, and reduce the risk of developing serious health conditions[21].
The present study has several limitations. A limitation may be the use of register data from the DNPR. However, reporting to the DNPR is required by law in Denmark, and allocation of cost to the health providers is partly based on the register. The DNPR is reported with an overall high quality of data, and the positive predictive value of orthopaedic diseases is reported to be 89%–91%[22]. Furthermore, a manual review of 50% of the data for validation showed high data completeness. Another potential limitation is a difference in coding between the different hospitals. However, variation among the various hospitals is of less importance as a difference in coding practice between the ‘pandemic’ and ‘pre-pandemic’ cohorts is expected to be comparable. Importantly, the manual check of 50% of the data did not reveal any signs of increase in non-accidental injuries, i.e. physical child abuse. However, health care workers should be aware that there may be an increased incidence during the pandemic[23].
The overall incidence rate for paediatric injury in the ‘pre-pandemic’ cohort was 10460/100000 persons/year. The overall incidence rate decreased to 5344/100000 persons/year in the ‘pandemic’ cohort. The primary decrease in incidence between the ‘pandemic’ and ‘pre-pandemic’ cohorts was observed in the adolescents.
Coronavirus disease 2019 (COVID-19) had a major influence on all parts of society. During the total lockdown of the Danish society, we noticed a substantial change in the pediatric and adolescent trauma.
We aimed to quantify the change in workload and estimate the incidence rates.
The aim was to examine the consequences of the national lockdown and political initiatives during the first surge of the COVID-19 pandemic expressed by changes in incidences of musculoskeletal paediatric injuries.
We compared the epidemiology of pediatric and adolescent trauma during the lockdown period of approximately one month with the same period of the previous year.
The ‘pre-pandemic’ cohort consisted of 2101 patients, and the ‘pandemic’ cohort consisted of 1070 patients, indicating a decrease of paediatric musculoskeletal injuries of 51%. The incidence of paediatric injury in the ‘pre-pandemic’ cohort was 10460/100000/year. In the ‘pandemic’ cohort, the incidence was 5344/100000/year.
A resource re-allocation to help serve the COVID-19 patients might be possible without reducing the level of care for injury-related paediatric patients.
If new lockdowns are enforced, hospitals and emergency and orthopedic departments in particular may be able to redistribute workforce without compromising patient care.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Denmark
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ren M S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Joeris A, Lutz N, Wicki B, Slongo T, Audigé L. An epidemiological evaluation of pediatric long bone fractures - a retrospective cohort study of 2716 patients from two Swiss tertiary pediatric hospitals. BMC Pediatr. 2014;14:314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Schalamon J, Dampf S, Singer G, Ainoedhofer H, Petnehazy T, Hoellwarth ME, Saxena AK. Evaluation of fractures in children and adolescents in a Level I Trauma Center in Austria. J Trauma. 2011;71:E19-E25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81:148-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 301] [Cited by in RCA: 351] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 4. | Randsborg PH, Gulbrandsen P, Saltytė Benth J, Sivertsen EA, Hammer OL, Fuglesang HF, Arøen A. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am. 2013;95:e42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Ramaesh R, Clement ND, Rennie L, Court-Brown C, Gaston MS. Social deprivation as a risk factor for fractures in childhood. Bone Joint J. 2015;97-B:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Kosuge D, Barry M. Changing trends in the management of children's fractures. Bone Joint J. 2015;97-B:442-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19:1976-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 440] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 8. | de Inocencio J, Carro MÁ, Flores M, Carpio C, Mesa S, Marín M. Epidemiology of musculoskeletal pain in a pediatric emergency department. Rheumatol Int. 2016;36:83-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Gunz AC, Canizares M, Mackay C, Badley EM. Magnitude of impact and healthcare use for musculoskeletal disorders in the paediatric: a population-based study. BMC Musculoskelet Disord. 2012;13:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Bram JT, Johnson MA, Magee LC, Mehta NN, Fazal FZ, Baldwin KD, Riley J, Shah AS. Where Have All the Fractures Gone? J Pediatr Orthop. 2020;40:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 171] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 11. | Sugand K, Park C, Morgan C, Dyke R, Aframian A, Hulme A, Evans S, Sarraf KM, Baker C, Bennett-Brown K, Simon H, Bray E, Li L, Lee N, Pakroo N, Rahman K, Harrison A. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: a multi-centre longitudinal observational study over the "golden weeks". Acta Orthop. 2020;91:633-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 12. | Baxter I, Hancock G, Clark M, Hampton M, Fishlock A, Widnall J, Flowers M, Evans O. Paediatric orthopaedics in lockdown: A study on the effect of the SARS-Cov-2 pandemic on acute paediatric orthopaedics and trauma. Bone Jt Open. 2020;1:424-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Hashmi PM, Zahid M, Ali A, Naqi H, Pidani AS, Hashmi AP, Noordin S. Change in the spectrum of orthopedic trauma: Effects of COVID-19 pandemic in a developing nation during the upsurge; a cross-sectional study. Ann Med Surg (Lond). 2020;60:504-508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Keays G, Friedman D, Gagnon I. Injuries in the time of COVID-19. Health Promot Chronic Dis Prev Can. 2020;40:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 15. | Memeo A, Priano D, Caldarini C, Trezza P, Laquidara M, Montanari L, Randelli P. How the pandemic spread of COVID-19 affected children's traumatology in Italy: changes of numbers, anatomical locations, and severity. Minerva Pediatr. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39:30-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2554] [Cited by in RCA: 3317] [Article Influence: 236.9] [Reference Citation Analysis (0)] |
| 17. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3438] [Cited by in RCA: 6246] [Article Influence: 347.0] [Reference Citation Analysis (0)] |
| 18. | Sheridan GA, Nagle M, Russell S, Varghese S, O'Loughlin PF, Boran S, Taylor C, Harty JA. Pediatric Trauma and the COVID-19 Pandemic: A 12-Year Comparison in a Level-1 Trauma Center. HSS J. 2020;1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 19. | Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, Letterie M, Davis MM. Well-being of Parents and Children During the COVID-19 Pandemic: A National Survey. Pediatrics. 2020;146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 678] [Article Influence: 135.6] [Reference Citation Analysis (0)] |
| 20. | Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63:531-532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 339] [Cited by in RCA: 441] [Article Influence: 88.2] [Reference Citation Analysis (0)] |
| 21. | Sallis JF, Simons-Morton BG, Stone EJ, Corbin CB, Epstein LH, Faucette N, Iannotti RJ, Killen JD, Klesges RC, Petray CK. Determinants of physical activity and interventions in youth. Med Sci Sports Exerc. 1992;24:S248-S257. [PubMed] |
| 22. | Andersen JS, Olivarius Nde F, Krasnik A. The Danish National Health Service Register. Scand J Public Health. 2011;39:34-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 665] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 23. | Martinkevich P, Larsen LL, Græsholt-Knudsen T, Hesthaven G, Hellfritzsch MB, Petersen KK, Møller-Madsen B, Rölfing JD. Physical child abuse demands increased awareness during health and socioeconomic crises like COVID-19. Acta Orthop. 2020;91:527-533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |