Published online Sep 18, 2021. doi: 10.5312/wjo.v12.i9.710
Peer-review started: February 17, 2021
First decision: May 3, 2021
Revised: May 17, 2021
Accepted: August 20, 2021
Article in press: August 20, 2021
Published online: September 18, 2021
Processing time: 209 Days and 5.2 Hours
Stress radiographs have demonstrated superior efficacy in the evaluation of ankle instability.
To determine if there is a degree of instability evidenced by stress radiographs that is associated with pathology concomitant with ankle ligamentous instability.
A retrospective review of 87 consecutive patients aged 18-74 who had stress radiographs performed at a single institution between 2014 and 2020 was performed. These manual radiographic stress views were then correlated with magnetic resonance imaging and operative findings.
A statistically significant association was determined for the mean and median stress radiographic values and the presence of peroneal pathology (P = 0.008 for tendonitis and P = 0.020 for peroneal tendon tears). A significant inverse relationship was found between the presence of an osteochondral defect and increasing degrees of instability (P = 0.043).
Although valuable in the clinical evaluation of ankle instability, stress radiographs are not an independent predictor of conditions associated with ankle in
Core Tip: Ankle Stress Radiographs were predictive of intraoperative findings. Specifically, they may assist the surgeon in clinical decision making regarding osteochondral lesions of the talus and peroneal tendon pathology.
- Citation: Sy JW, Lopez AJ, Lausé GE, Deal JB, Lustik MB, Ryan PM. Correlation of stress radiographs to injuries associated with lateral ankle instability. World J Orthop 2021; 12(9): 710-719
- URL: https://www.wjgnet.com/2218-5836/full/v12/i9/710.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i9.710
Ankle instability is one of the most common sports related injuries with an incidence of 7 per 1000 persons per year[1]. Close to 40% of patients who sustain an inversion injury to their ankle report residual symptoms long after they have recovered from the injury to their lateral ligaments. This residual pain may be secondary to associated conditions that occur at the time of the injury or as a result of chronic instability[2]. The differential diagnosis for associated injuries or causes of residual symptoms is large and includes: occult fractures of the ankle, fractures of the metatarsals, peroneal tendon tears, osteochondral lesions of the talus (OLT), tarsal coalitions, neurogenic injuries, radicular pain, autonomic dysreflexia, impingement, syndesmotic injuries, and subtalar instability. Determining which symptoms are related to ligamentous injury and which symptoms are related to associated conditions can be a diagnostic dilemma. Clinicians use multiple resources to determine which patients have sym
A retrospective review of consecutive patients aged 18-74 who had stress radiographs performed at a single institution between 2014 and 2020 was performed. Once the patients with documented stress radiographs were identified, the electronic medical record was utilized to collect the following information: degree of widening on the talar tilt stress radiograph, millimeters of anterior translation on the anterior drawer stress radiograph, presence of an OLT on MRI or noted in the operation report if an operation was performed, presence of a peroneal tendon tear or tendonitis noted on the MRI or in the operation report, and documentation of operative management of an OLT or peroneal tendon. All patients who had a stress radiograph performed were included in the study. The presence of operative instability was not an inclusion or exclusion criteria.
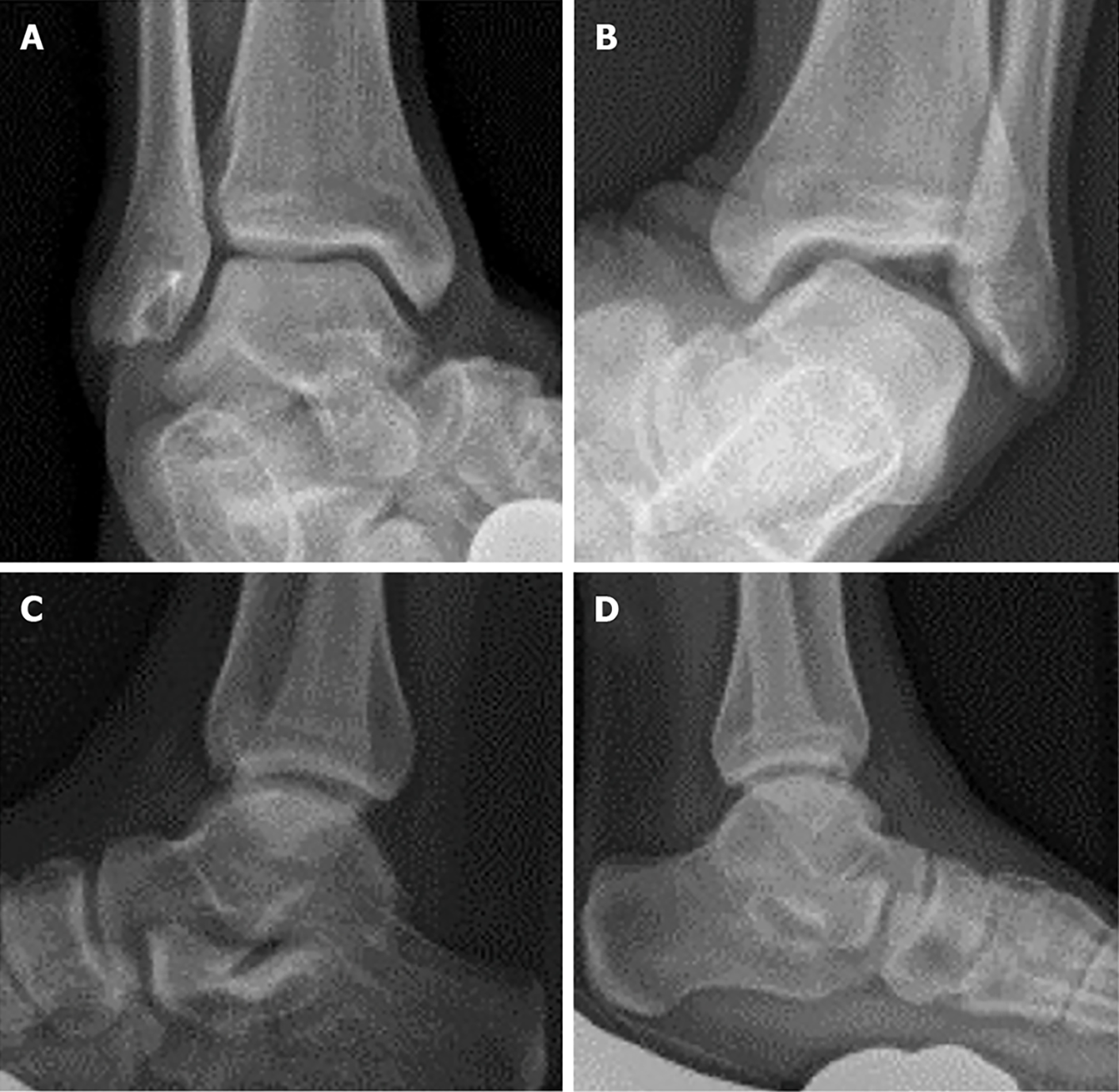
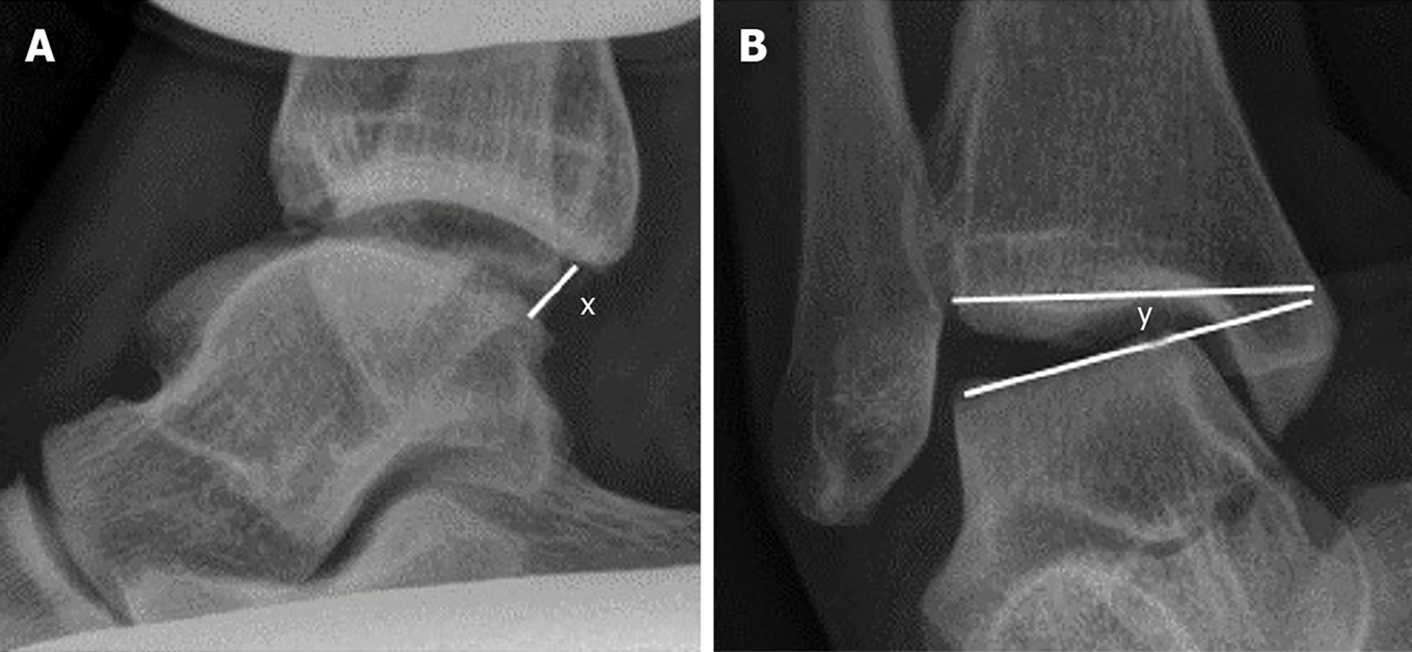
Stress radiographs were performed manually. Although various providers performed the radiographs, the technique was standardized. An example of a stress radiograph is seen in Figure 1. An initial mortise film was obtained prior to the talar tilt stress view. Once the mortise was aligned, the tibia was held to maintain the mortise while an inversion force was applied to the ankle. Verification of an appropriate mortise view was obtained. The anterior drawer was obtained by first verifying that a perfect lateral of the talus was visible on digital radiography. The tibia was then held in the same alignment and an anterior force was applied to the calcaneus. Verification of the lateral was obtained. All stress radiographs were routinely measured by a board-certified radiologist unaffiliated with the study. An example of the technique utilized to measure the stress radiographs is demonstrated in Figure 2.
The associated findings to include OLTs and peroneal pathology were determined from the MRI reports and operative reports. All MRI reports were read by board certified radiologists unaffiliated with the study. Operative findings were obtained from the dictated operation reports. Because continuous data were not normally distributed, statistical analysis was performed with a nonparametric Wilcoxon Rank Sum Test to assess differences in median levels of anterior drawer and talar tilt angel between patients with and without selected outcomes. All analyses were conducted using SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC, United States).
There were 87 patients meeting inclusion criteria including 14 females and 73 males. The mean talar tilt was 8.6° (range 0-25). The mean anterior drawer was 4.6 mm (range 0-9.9 mm). Peroneal tendonitis was documented in 22 patients (25%). Peroneal tendon tears were documented in 6 patients (7%). An OLT of any size was documented in 42 patients (48%). An OLT greater than 1 cm in its largest diameter was documented in 16 patients (18%). Operative management of an OLT to include microfracture or chondroplasty was performed in 35 patients (40%). Cartilage restoration with Biocartilage or DeNovo NT allograft was performed in 7 patients (8%). An operative exploration of the peroneal tendons was performed in 19 patients (22%). A peroneal tendon repair was required in 2 patients (2%). A lateral ligament repair or modified Broström procedure was performed in 64 patients (74%).
In order to evaluate the relationship between associated findings and stress view values, unpaired t-tests were utilized to evaluate mean differences in anterior drawer and talar tilt between patients with and without selected outcomes. There were no statistical associations based upon the anterior drawer as depicted in Table 1. By contrast, the talar tilt angle was associated with several outcomes. Patients with the diagnosis of peroneal tendonitis had a larger talar tilt on average than patients without peroneal tendonitis (mean = 11.8° vs 7.5°, P = 0.004). Similarly, patients with peroneal tears also had larger tilt angles on average than those without tears (mean = 13.8° vs 8.2°, P = 0.026). The remainder of associations are depicted in Table 2.
| Outcome | Outcome = No | Outcome = Yes | P value | ||||
| n | mean | SD | n | mean | SD | ||
| Peroneal tendonitis | 65 | 4.5 | 2.7 | 22 | 4.9 | 3.2 | 0.533 |
| Peroneal tear | 81 | 4.7 | 2.7 | 6 | 3.4 | 4.0 | 0.251 |
| MRI OLT | 45 | 5.0 | 3.0 | 42 | 4.2 | 2.5 | 0.206 |
| MRI OLT < 1 cm | 61 | 4.9 | 2.9 | 26 | 3.9 | 2.4 | 0.107 |
| MRI > 1 cm | 71 | 4.6 | 2.9 | 16 | 4.8 | 2.6 | 0.791 |
| Broström | 23 | 4.7 | 2.2 | 64 | 4.6 | 3.0 | 0.805 |
| Operative peroneal exploration | 68 | 4.7 | 2.8 | 19 | 4.4 | 2.8 | 0.675 |
| Operative peroneal repair | 85 | 4.6 | 2.8 | 2 | 5.8 | 1.7 | 0.548 |
| Operative OLT microfracture/chondroplasty | 52 | 5.1 | 2.8 | 35 | 3.9 | 2.7 | 0.066 |
| Operative OLT restoration/repair | 80 | 4.6 | 2.9 | 7 | 4.9 | 1.8 | 0.753 |
| Outcome | Outcome = No | Outcome = Yes | P value | ||||
| n | mean | SD | n | mean | SD | ||
| Peroneal tendonitis | 65 | 7.5 | 5.4 | 22 | 11.8 | 6.7 | 0.004 |
| Peroneal tear | 81 | 8.2 | 6.0 | 6 | 13.8 | 4.4 | 0.026 |
| MRI OLT | 45 | 9.8 | 6.0 | 42 | 7.3 | 5.8 | 0.051 |
| MRI OLT < 1 cm | 61 | 8.8 | 6.3 | 26 | 8.1 | 5.4 | 0.610 |
| MRI > 1 cm | 71 | 9.2 | 5.8 | 16 | 6.0 | 6.4 | 0.057 |
| Broström | 23 | 3.3 | 3.3 | 64 | 10.5 | 5.6 | < 0.001 |
| Operative peroneal exploration | 68 | 8.3 | 6.0 | 19 | 9.7 | 6.0 | 0.372 |
| Operative peroneal repair | 85 | 8.6 | 6.0 | 2 | 10.0 | 8.5 | 0.739 |
| Operative OLT microfracture/chondroplasty | 52 | 9.1 | 6.2 | 35 | 7.8 | 5.8 | 0.339 |
| Operative OLT restoration/repair | 80 | 9.0 | 6.0 | 7 | 4.4 | 4.9 | 0.057 |
Tables 3 and 4 summarize results of nonparametric analyses to assess differences in median levels of anterior drawer and talar tilt, respectively, between patients with and without selected reasons for surgery. For anterior drawer, the evaluation shows an inverse relationship found between the degree of instability as measured on the anterior drawer image and the presence of an OLT. Patients who had an OLT had a median anterior drawer of 4.1°, while patients without an OLT had an anterior drawer measurement of 5.1°, P = 0.035.
| Outcome | Outcome = No | Outcome = Yes | P value | ||||
| n | Median | IQR | n | Median | IQR | ||
| Peroneal tendonitis | 65 | 4.5 | 3.0-6.6 | 22 | 4.8 | 4.0-7.0 | 0.487 |
| Peroneal tear | 81 | 4.6 | 3.3-7.0 | 6 | 2.1 | 0.0-7.0 | 0.318 |
| MRI OLT | 45 | 5.2 | 2.7-7.5 | 42 | 4.3 | 3.0-5.6 | 0.110 |
| MRI OLT < 1 cm | 61 | 5.1 | 3.3-7.1 | 26 | 4.2 | 3.0-5.0 | 0.062 |
| MRI > 1 cm | 71 | 4.6 | 2.7-7.0 | 16 | 4.7 | 3.7-6.9 | 0.891 |
| Broström | 23 | 4.7 | 4.0-6.9 | 64 | 4.5 | 2.4-7.1 | 0.870 |
| Operative peroneal exploration | 68 | 4.9 | 3.3-6.9 | 19 | 4.3 | 2.7-7.0 | 0.550 |
| Operative peroneal repair | 85 | 4.5 | 3.0-7.0 | 2 | 5.8 | 4.6-7.0 | 0.514 |
| Operative OLT microfracture/chondroplasty | 52 | 5.1 | 3.7-7.2 | 35 | 4.1 | 2.7-5.6 | 0.035 |
| Operative OLT restoration/repair | 80 | 4.5 | 2.9-7.0 | 7 | 4.8 | 4.0-6.9 | 0.827 |
| Outcome | Outcome = No | Outcome = Yes | P value | ||||
| n | Median | IQR | n | Median | IQR | ||
| Peroneal tendonitis | 65 | 7 | 3-12 | 22 | 12 | 6-18 | 0.0081 |
| Peroneal tear | 81 | 8 | 3-12 | 6 | 15 | 10-16 | 0.0201 |
| MRI OLT | 45 | 9 | 5-14 | 42 | 6 | 2-13 | 0.0431 |
| MRI OLT < 1 cm | 61 | 8 | 3-14 | 26 | 8 | 3-13 | 0.763 |
| MRI > 1 cm | 71 | 8 | 4-13 | 16 | 3 | 1-10.5 | 0.0251 |
| Broström | 23 | 3 | 1-4 | 64 | 10 | 6.5-14 | < 0.0011 |
| Operative peroneal exploration | 68 | 8 | 3-12 | 19 | 11 | 4-15 | 0.318 |
| Operative peroneal repair | 85 | 8 | 3-13 | 2 | 10 | 4-16 | 0.670 |
| Operative OLT microfracture/chondroplasty | 52 | 8 | 4-13 | 35 | 7 | 3-13 | 0.360 |
| Operative OLT restoration/repair | 80 | 8 | 3.5-13 | 7 | 3 | 1-6 | 0.0391 |
For talar tilt, several significant findings are noted. Larger degrees of tilt were seen in patients who had peroneal tendonitis or peroneal tendon tears, and an inverse relationship was found between the degree of instability and the presence of an OLT. Patients with an OLT had a median talar tilt of 6° while patients without an OLT had a median talar tilt of 9°, P = 0.039. Large OLTs were evaluated separately from all OLTs and patients who had a large OLT of greater than 1 cm in diameter were found to have a talar tilt median of 3° while patients who did not have a large OLT were found to have a talar tilt of 8°, P = 0.025. As the senior surgeon utilized 9° of instability as an operative indication for a lateral ligament repair or Broström procedure, the data set confirms that selection criteria when utilizing both the mean and median values.
For each area of pathology that had a significant difference found for the mean or median values on stress radiographs, predictive statistics were performed to include sensitivity (Sn), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV). The results of this analysis are listed in Tables 5 and 6. Initial analysis of the talar tilt was performed using 10° as the threshold value as seen in Table 5. Given the significant inverted association demonstrated for OLTs and the anterior drawer stress radiograph, predictive analysis was performed for the anterior drawer test utilizing 5° as the threshold as seen in Table 6. Predictive statistics were not performed for the Broström procedure as the surgical candidates were selected largely based upon the stress radiographic results which resulted in the significant association between the Broström procedure and larger values on stress radiographs. In addition, predictive statistics were not performed for OLTs as a significant inverse relationship was demonstrated.
| Talar tilt ≥ 10° | Talar tilt < 10° | Sn (%) | Sp (%) | PPV (%) | NPV (%) | |
| Peroneal tendonitis | 13/35 | 9/52 | 59 | 66 | 37 | 83 |
| Peroneal tear | 5/35 | 1/52 | 83 | 63 | 14 | 98 |
| Any peroneal pathology | 14/35 | 10/52 | 58 | 67 | 40 | 81 |
| Any OLT | 15/35 | 27/52 | 36 | 56 | 43 | 48 |
| Anterior drawer < 5 mm | Anterior drawer ≥ 5 mm | Sn (%) | Sp (%) | PPV (%) | NPV (%) | |
| OLT | 30 | 13 | 70 | 57 | 64 | 68 |
The lateral ligaments of the tibiotalar joint do not provide stability to the joint in isolation. The bony architecture of the tibiotalar joint contributes to its stability with the talus widest anteriorly making the joint most stable in dorsiflexion[6]. In plantarflexion, the fibula internally rotates and moves inferiorly to maintain the stability of the mortise[7]. In addition to the syndesmotic ligaments, the tibiotalar joint is constrained medially by the deltoid ligamentous complex and laterally through the collateral ligament complex. Dynamic stability of the tibiotalar joint is provided by the surrounding extrinsic musculature. The tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneal tertius contribute to dorsiflexion in the anterior compartment. Within the compartment, the tibialis anterior and extensor hallucis longus also contribute to inversion. This is balanced by the peroneal tertius which provides eversion in addition to dorsiflexion. In the lateral compartment, the peroneal longus and brevis both contribute to eversion which helps to mitigate inversion stresses across the ankle. Posteriorly, the tibialis posterior, flexor digitorum longus, and flexor hallucis longus all help to produce ankle inversion in conjunction with plantar flexion due to the oblique rotational axis of the tibiotalar joint[6].
Given that the lateral ligaments do not provide stability to the ankle in isolation, it follows that the lateral ligaments are not injured in isolation. Clinical studies have demonstrated that that ankle instability occurs with associated pathology such as peroneal tendinopathy in up to 28% of cases[8]. Peroneal tendinopathy is considered to be an overuse injury related to inflammatory and degenerative changes[9]. In theory, chronic lateral ligament insufficiency may lead to overuse of the peroneal tendons as the peroneal longus and brevis provide dynamic support to the ankle. Our findings were consistent with this as we found a significant increase in peroneal tendonitis in patients who had a talar tilt of 11.8° when compared to patients who had a mean talar tilt of 7.5°.
Split tears of the peroneal brevis tendon are relatively common. A cadaveric study without clinical correlation found a prevalence of split tears in 37.5% of the 112 ankles evaluated[10]. Peroneal muscles are the first muscles to respond and contract in response to ankle inversion[11]. In theory, increasing inversion of an ankle secondary to ligamentous instability could place an increasing strain upon the peroneal tendons. In a review of 180 open ankle lateral ligament repair procedures, Strauss et al[8] found 51 (28%) ankles with a peroneal tendon injury. The authors did not further break down the type of injuries found or the treatment provided. Our study found that peroneal tendon tears occurred in patients with a mean talar tilt of 13.8° and was not seen in patients with a mean talar tilt of 8.2°. This data would suggest that increasing degrees of instability may be associated with an increasing incidence of peroneal tendon tears.
Classic imaging studies of peroneal pathology can include plain radiographs, ultrasound, computed tomography (CT), and MRI. Data from plain radiographs is limited in regard to peroneal pathology unless a ‘fleck’ sign is visualized which is pathognomonic for a superior peroneal retinaculum avulsion. Aside from evaluating associated osseous pathology, CT scan has a limited role in the evaluation of peroneal tendons. Ultrasound is provider dependent but has been shown to accurately predict peroneal tendon tears in 90% of cases[12]. MRI is commonly utilized and can document peroneal tendosynovitis or tears. The artifact that occurs as the tendons curve around the lateral malleolus, however, can decreased the sensitivity to 80% and the specificity to 75%[13].
Although we were able to find an association between larger degrees of instability and the presence of peroneal pathology, we were not able to find a degree of instability that was predictive of instability. Threshold values of 10 mm on the anterior drawer test or 10° on the talar tilt test have been found to correlate with clinical instability[14]. We evaluated the statistical performance of stress radiographs in terms of peroneal pathology. Since the mean talar tilt associated with peroneal tendonitis was 11.8°, and the mean talar tilt associated with a peroneal tendon tear was 13.8°, we evaluated the Sn, Sp, PPV, and NPV of the talar tilt utilizing 10° as the threshold for a positive test for peroneal pathology. We considered a value of 85% to be clinically meaningful given the significant association determined between the mean and medians for each pathology studied. A talar tilt test of < 10° had a NPV of 98% when evaluating the presence of a peroneal tendon tear in our analysis. The remainder of the values were not found to be clinically meaningful as demonstrated in Table 5.
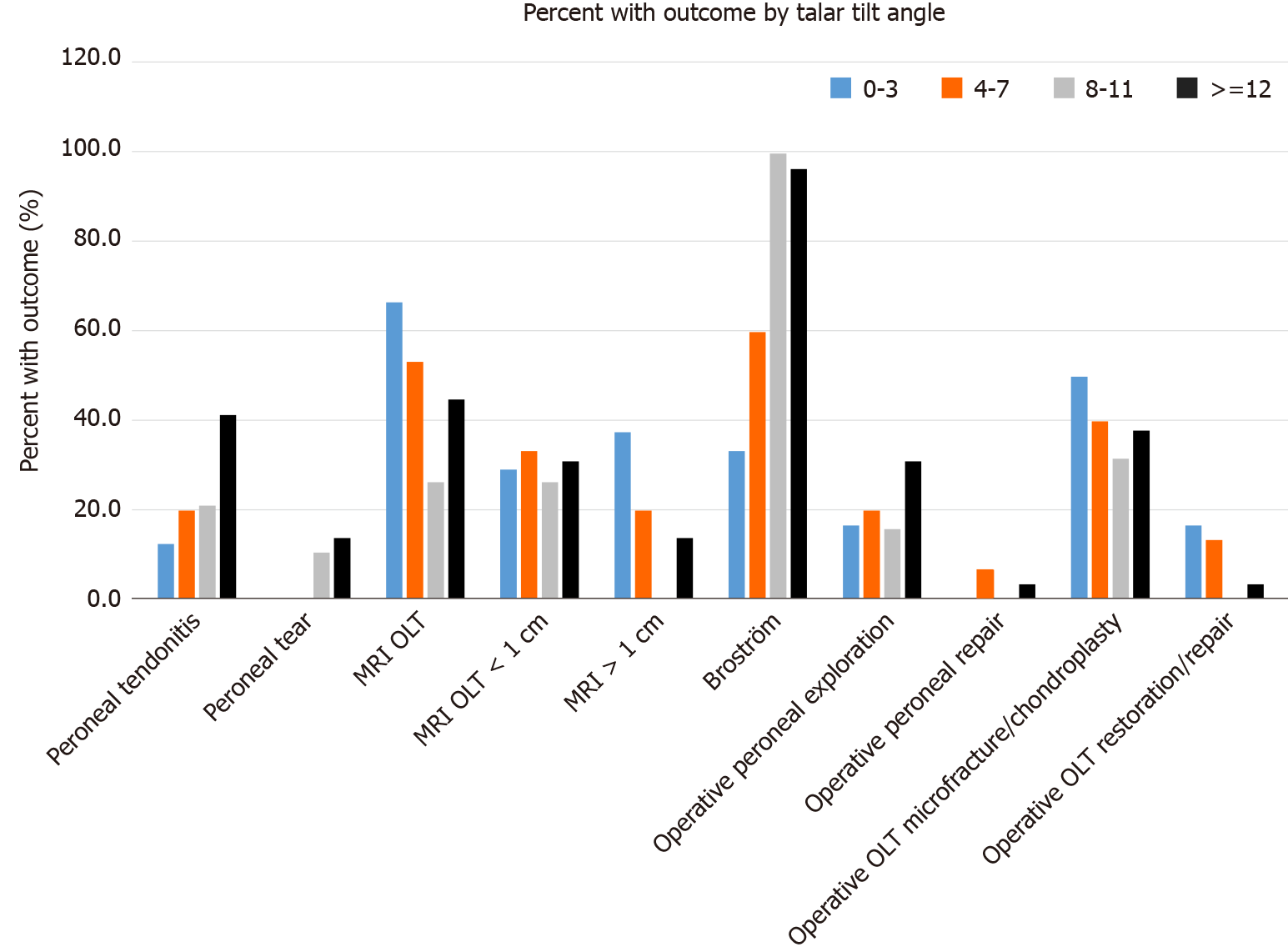
We also looked at the relationship between OLTs and instability. The tibiotalar joint has a high level of congruency. In plantarflexion and dorsiflexion, the contact surface area of the ankle is decreased and the contact pressures increased[15,16]. Multiple previous studies have suggested an association between increased instability and OLTs. In a study of 148 patients with ankle instability who underwent operative management, Hintermann et al[17] found 26 patients (18%) with full thickness cartilaginous lesions of the talus. In a similar study of 65 patients undergoing operative management for lateral ankle instability by Cha et al[18], the authors found OLTs in 33 patients (51%). In this study, 22 of these lesions were classified as softening or superficial fissuring with 20 (18%) being classified as deep fissures or exposed bone[18]. It is unclear as to how many of these lesions required surgical management. In a study of 283 patients requiring surgery for ankle fractures, OLTs were found in 61 patients (73%) during operative arthroscopy. More severe fracture patterns were associated with an increased incidence of OLTs[19]. The association of ankle instability with OLTs, however, has not been consistent in every study. In a recent study, Park et al[20] evaluated 195 patients with a history of an inversion injury who were evaluated with both MRI and stress radiographs. The authors defined radiographic instability as having a talar tilt of greater than or equal to 10°. An increased talar tilt was associated with a lower incidence of OLT and the presence of an OLT was associated with a decreased tibiotalar tilt. We found similar findings in our study group. Ankles that did not have an OLT had a mean talar tilt of 9.8° while patients who did have an OLT had a mean talar tilt of 7.3°. When we evaluated our data utilizing the median values rather than the mean to account for outliers, we found a very similar inverse relationship between the presence of an OLT and the degree of instability. We found that the 42 patients who had an OLT had a median talar tilt of 9° while the median talar tilt for the 45 patients who did have an OLT was 6°. As seen in Table 4, this inverse relationship remained significant for larger OLTs and for OLTs that underwent operative management. The inverse relationship in our data set is best depicted in Figure 3. We were not able to find a clinically meaningful value on the anterior drawer test or the talar tilt test in terms of sensitivity, specificity, the positive predictive value, or the negative predictive value. As seen in Table 5, we utilized 10° as the threshold for the talar tilt test. Given the inverse relationship noted for OLTs and instability, a positive test was described as a test having a value of less than 10°. Although a threshold of 10mm has been described for a positive anterior drawer test when evaluating for instability, we utilized a threshold of 5 mm based upon our evaluation of the medians with those patients with an OLT having a median anterior drawer of 3 mm vs 8 mm for patients without an OLT. Similar to the talar tilt results, a value of less than 5 mm on the anterior drawer was not predictive of an OLT in our analysis as demonstrated in Table 6.
This study has strengths and weaknesses. We evaluated not just the presence of associated conditions but also documented which conditions were treated surgically. With that said, the presence of conditions on imaging studies or documented during surgery is objective data, while the decision to perform a repair could be subject to bias. The relationship between stress radiographs and functional instability has not been clearly defined. For this reason, we did not evaluate the prevalence of associated conditions based upon a defined degree of instability but rather evaluated the mean and median instability measured when associated conditions were present. The data confirms the relationship between instability and peroneal pathology demonstrating that patients with peroneal pathology had a significantly higher mean and median talar tilt measurement. In addition, we documented a significant inverse relationship between radiographic instability and the presence of an OLT. This is the second study to evaluate the inverse relationship seen between instability and OLTs.
In evaluating stress radiographs as they relate to associated conditions, we found several areas of significance. Increasing instability was associated with a statistically significant higher prevalence of peroneal tendinopathy and peroneal tendon tears. We also demonstrated an inverse relationship between the presence of OLTs and higher degrees of instability. The broad application of these findings to clinical practice is limited as demonstrated with low sensitivity, specificity, and predictive values for the thresholds measured. Ankle instability remains a complex diagnosis with known associated conditions. While stress radiographs may assist the surgeon in defining mechanical instability, this imaging study alone cannot be utilized to rule out or rule in concomitant pathology that is associated with ankle instability.
Once patients were diagnosed with instability based upon stress radiographs, the surgical procedure was delayed due to the need to obtain a magnetic resonance imaging in order to define which patients had associated conditions. Prior to this study, the surgeons involved felt that higher degrees on instability were associated with the incidence of associated conditions that could result from instability.
In general, we hoped to avoid a delay in treatment due to the need to obtain advanced imaging. We assumed that patients with higher degrees of instability would have osteochondral lesions or peroneal pathology and would require diagnostic arthroscopy or peroneal exploration while patients with a lesser degree of instability could be addressed with a limited surgical procedure focused on the lateral ligaments.
We aimed to determine a degree of instability that could predict the incidence of peroneal pathology or osteochondral defects.
A retrospective analysis of patients who had previously been diagnosed with ankle instability was performed. We stratified the patients based upon their degree of instability as defined by stress radiographs and evaluated the incidence of peroneal pathology and osteochondral defects as related to the varying degrees of instability.
Increasing degrees of instability was associated with a statistically significant increased prevalence of peroneal pathology. An inverse relationship was found between increasing degrees of instability and the presence of osteochondral defects. While we did confirm the association of ligamentous instability to peroneal pathology and the inverse relationship found between osteochondral defects and instability, we did not find a degree of instability that was predictive of peroneal pathology or osteochondral defects.
Stress radiographs were not found to be predictive of peroneal tendon pathology or osteochondral defects of the talus.
This is only the second study to demonstrate an inverse relationship between ankle instability and osteochondral defects of the talus. This is a novel discovery, but the injury mechanism that leads to ligamentous instability without chondral injury is unclear. Potentially axial load injuries are more likely to result in chondral injuries as opposed to rotational injuries that may lead to ankle instability. Further work is required to better understand this injury pattern.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gantaguru A S-Editor: Wang JL L-Editor: A P-Editor: Ma YJ
| 1. | Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44:123-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 692] [Cited by in RCA: 564] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 2. | Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669-677. [PubMed] |
| 3. | Jolman S, Robbins J, Lewis L, Wilkes M, Ryan P. Comparison of Magnetic Resonance Imaging and Stress Radiographs in the Evaluation of Chronic Lateral Ankle Instability. Foot Ankle Int. 2017;38:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Taljanovic MS, Alcala JN, Gimber LH, Rieke JD, Chilvers MM, Latt LD. High-resolution US and MR imaging of peroneal tendon injuries. Radiographics. 2015;35:179-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (1)] |
| 5. | O'Neil JT, Pedowitz DI, Kerbel YE, Codding JL, Zoga AC, Raikin SM. Peroneal Tendon Abnormalities on Routine Magnetic Resonance Imaging of the Foot and Ankle. Foot Ankle Int. 2016;37:743-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma. 2016;30:232-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 182] [Cited by in RCA: 234] [Article Influence: 26.0] [Reference Citation Analysis (1)] |
| 7. | Scranton PE Jr, McMaster JG, Kelly E. Dynamic fibular function: a new concept. Clin Orthop Relat Res. 1976;76-81. [PubMed] |
| 8. | Strauss JE, Forsberg JA, Lippert FG 3rd. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int. 2007;28:1041-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Aicale R, Tarantino D, Maffulli N. Overuse injuries in sport: a comprehensive overview. J Orthop Surg Res. 2018;13:309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 141] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 10. | Miura K, Ishibashi Y, Tsuda E, Kusumi T, Toh S. Split lesions of the peroneus brevis tendon in the Japanese population: an anatomic and histologic study of 112 cadaveric ankles. J Orthop Sci. 2004;9:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Davda K, Malhotra K, O'Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT Open Rev. 2017;2:281-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 12. | Grant TH, Kelikian AS, Jereb SE, McCarthy RJ. Ultrasound diagnosis of peroneal tendon tears. A surgical correlation. J Bone Joint Surg Am. 2005;87:1788-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Wang XT, Rosenberg ZS, Mechlin MB, Schweitzer ME. Normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics. 2005;25:587-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 14. | Chang SH, Morris BL, Saengsin J, Tourné Y, Guillo S, Guss D, DiGiovanni CW. Diagnosis and Treatment of Chronic Lateral Ankle Instability: Review of Our Biomechanical Evidence. J Am Acad Orthop Surg. 2021;29:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Calhoun JH, Li F, Ledbetter BR, Viegas SF. A comprehensive study of pressure distribution in the ankle joint with inversion and eversion. Foot Ankle Int. 1994;15:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 115] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | de Asla RJ, Wan L, Rubash HE, Li G. Six DOF in vivo kinematics of the ankle joint complex: Application of a combined dual-orthogonal fluoroscopic and magnetic resonance imaging technique. J Orthop Res. 2006;24:1019-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 383] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 18. | Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, Hyung JW. Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg. 2012;4:293-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 143] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 20. | Park BS, Chung CY, Park MS, Sung KH, Choi Y, Park C, Koo S, Lee KM. Inverse Relationship Between Radiographic Lateral Ankle Instability and Osteochondral Lesions of the Talus in Patients With Ankle Inversion Injuries. Foot Ankle Int. 2019;40:1368-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |