Published online Aug 18, 2021. doi: 10.5312/wjo.v12.i8.604
Peer-review started: April 26, 2021
First decision: June 16, 2021
Revised: June 20, 2021
Accepted: July 20, 2021
Article in press: July 20, 2021
Published online: August 18, 2021
Processing time: 106 Days and 13.7 Hours
Femoral head fractures (FHFs) are considered relatively uncommon injuries; however, open reduction and internal fixation is preferred for most displaced fractures. Several surgical approaches had been utilized with controversial results; surgical hip dislocation (SHD) is among these approaches, with the reputation of being demanding and leading to higher complication rates.
To determine the efficacy and safety of SHD in managing FHFs by reviewing the results reported in the literature.
Major databases including PubMed, Embase, Web of Science, and Cochrane Central Register of Controlled Trials were searched to identify studies reporting on outcomes of SHD utilized as an approach in treating FHFs. We extracted basic studies data, surgery-related data, functional outcomes, radiological outcomes, and postoperative complications. We calculated the mean differences for continuous data with 95% confidence intervals for each outcome and the odds ratio with 95% confidence intervals for binary outcomes. P < 0.05 was considered significant.
Our search retrieved nine studies meeting our inclusion criteria, with a total of 129 FHFs. The results of our analysis revealed that the average operation time was 123.74 min, while the average blood loss was 491.89 mL. After an average follow-up of 38.4 mo, a satisfactory clinical outcome was achieved in 85% of patients, with 74% obtained anatomical fracture reduction. Overall complication rate ranged from 30% to 86%, with avascular necrosis, heterotopic ossification, and osteoarthritis being the most common complications occurring at an incidence of 12%, 25%, and 16%, respectively. Trochanteric flip osteotomy nonunion and trochanteric bursitis as a unique complication of SHD occurred at an incidence of 3.4% and 3.8%, respectively.
The integration of SHD approach for dealing with FHFs offered acceptable functional and radiological outcomes with a wide range of safety in regards to the hip joint vascularity and the development of avascular necrosis, the formation of heterotopic ossification, and the development of posttraumatic osteoarthritis; however, it still carries its unique risk of trochanteric flip osteotomy nonunion and persistent lateral thigh pain.
Core Tip: In the past few years, surgical hip dislocation had been adopted by many trauma surgeons as an approach for femoral head fractures management. The current systematic review and metanalysis collected data from the most recent literature showed the efficacy of this approach in regards to obtaining acceptable functional and radiological outcomes as well as resulting in relatively low complication rates when compared with other approaches reported in the literature. However, it carries some unique complications such as trochanteric bursitis and trochanteric flip osteotomy nonunion.
- Citation: Khalifa AA, Haridy MA, Fergany A. Safety and efficacy of surgical hip dislocation in managing femoral head fractures: A systematic review and meta-analysis. World J Orthop 2021; 12(8): 604-619
- URL: https://www.wjgnet.com/2218-5836/full/v12/i8/604.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i8.604
Femoral head fractures (FHFs) are considered rare injuries resulting from high energy trauma, which is usually associated with posterior hip dislocation and rarely anterior subluxation [1,2]. The rarity of this injury makes it difficult to report on large numbers of patients, and the performance of high quality prospective randomized studies is even more challenging [1,3].
The commonly used classification system for this injury is the Pipkin classification, where four types were identified according to the fracture location and the presence of associated injuries (Type I where the fracture fragment is distal to the fovea, Type II where the fracture fragment including or above the fovea, Type III if the fracture is associated with a femoral neck fracture, and Type IV if it was associated with aceta
The management of FHFs follows a broad spectrum of options (primarily based on its Pipkin type), where conservative management is kept for the minimally displaced Pipkin I fracture, and at the end of the spectrum, total hip arthroplasty could be offered for older patients with highly comminuted fractures[5].
The basic principles of intraarticular fracture management still apply to FHFs, where obtaining anatomical reduction and stable fixation [achieved by open reduction and internal fixation (ORIF)] is mandatory for good long-term results. The controversy exists regarding the optimum approach that should be used safely for ORIF[2,3,6], either anterior, lateral, or posterior based approaches including the use of safe surgical hip dislocation (SHD), which was initially described by Ganz et al[7] as a safe approach for management of different intraarticular hip pathologies with no or few complications especially those related to femoral head vascularity[3,7].
One of the significant complications occurring either due to the trauma itself or as a consequence of surgical management is avascular necrosis (AVN) of the femoral head[2,3]. After Ganz popularized the safety of SHD in regard to hip vascularity preservation[7], this encouraged more trauma surgeons to introduce this approach in the armamentarium of approaches in the management of FHFs[2,3,6,8].
As a trial to collect large data on these injuries, a systematic review was performed by Giannoudis et al[2] in 2009, pooling the data from 29 studies that constituted a total of 453 FHFs treated through different approaches, where they evaluated various aspects related to management; however, one drawback of this review was the heterogenicity of the reported studies, and the inclusion of relatively few numbers of patients (36 FHFs) treated through SHD[2].
Recently, more studies with a larger number of patients reported the utilization of SHD in the management of FHFs; this encouraged us to carry out this systematic review and metanalysis to update the knowledge regarding the clinical and radio
We conducted a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist[9]. PubMed, Embase, Web of Science, and Cochrane Central Register of Controlled Trials databases were searched for the last 20 years (until January 2021) using a combination of the following search terms: Femoral head fracture, Pipkin fracture, surgical hip dislocation, Ganz.
Retrieved results were imported into Endnote X9 software (Thomson Reuters, New York, NY, United States), where a check for duplicates was conducted. The titles and abstracts of the remaining articles were then screened, and the selection was based on the following exclusion criteria: (1) Articles published in languages other than English; (2) Reviews, guidelines, or classifications; (3) Letters to the editor, case reports, or conference papers; (4) In vitro and animal experiment studies; and (5) Irrelevant studies.
Subsequently, full-text articles of potentially relevant studies were obtained and assessed for eligibility. We included studies that met the following inclusion criteria: (1) Prospective or retrospective cohorts or case series investigating SHD via a trochanteric flip osteotomy (TFO) (as described initially by Ganz et al[7]) as an approach to treat FHFs in adult populations or studies from which data could be extracted independently; (2) A minimum sample size of 5 patients; and (3) The ability to extract data related to the outcomes of interest (data should be genuine and not reported in another study).
Two independent reviewers reviewed the list of potentially eligible articles (they also performed data extraction), and a third reviewer was consulted, when necessary, to decide any uncertainties regarding eligibility. The following information was extracted from studies that met the inclusion criteria: The name of the first author, year of publication, study design, number of cases, patients age and gender, classification of the fracture according to Pipkin classification system, the strategy of management (ORIF or fragment excision), type of the implant used for fixation, operation time, blood loss, length of follow-up time, and outcomes of interest including functional outcome, radiological outcome, complication rate, and reoperation or revision surgery details.
When mean or standard deviation values were not available in the publications, we used statistical methods described in previous literature to derive the needed numerical values[10]. We performed all data analyses using Review Manager version 5.4.1. (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). We calculated the odds ratio with a 95% confidence interval (CI) for binary outcomes, while the mean difference with 95%CI for continuous outcomes was calculated. To calculate the overall effect estimate with 95%CI, we used a fixed-effect model with the method of Mantel-Haenszel when there was no evidence of heterogeneity between studies. Otherwise, a random-effects model with the method of DerSiomonian and Laird was chosen. Heterogeneity between studies was evaluated using the Q statistic and I² test, which describes the percentage of variability in the effect estimates. A P value of < 0.05 was considered significant.
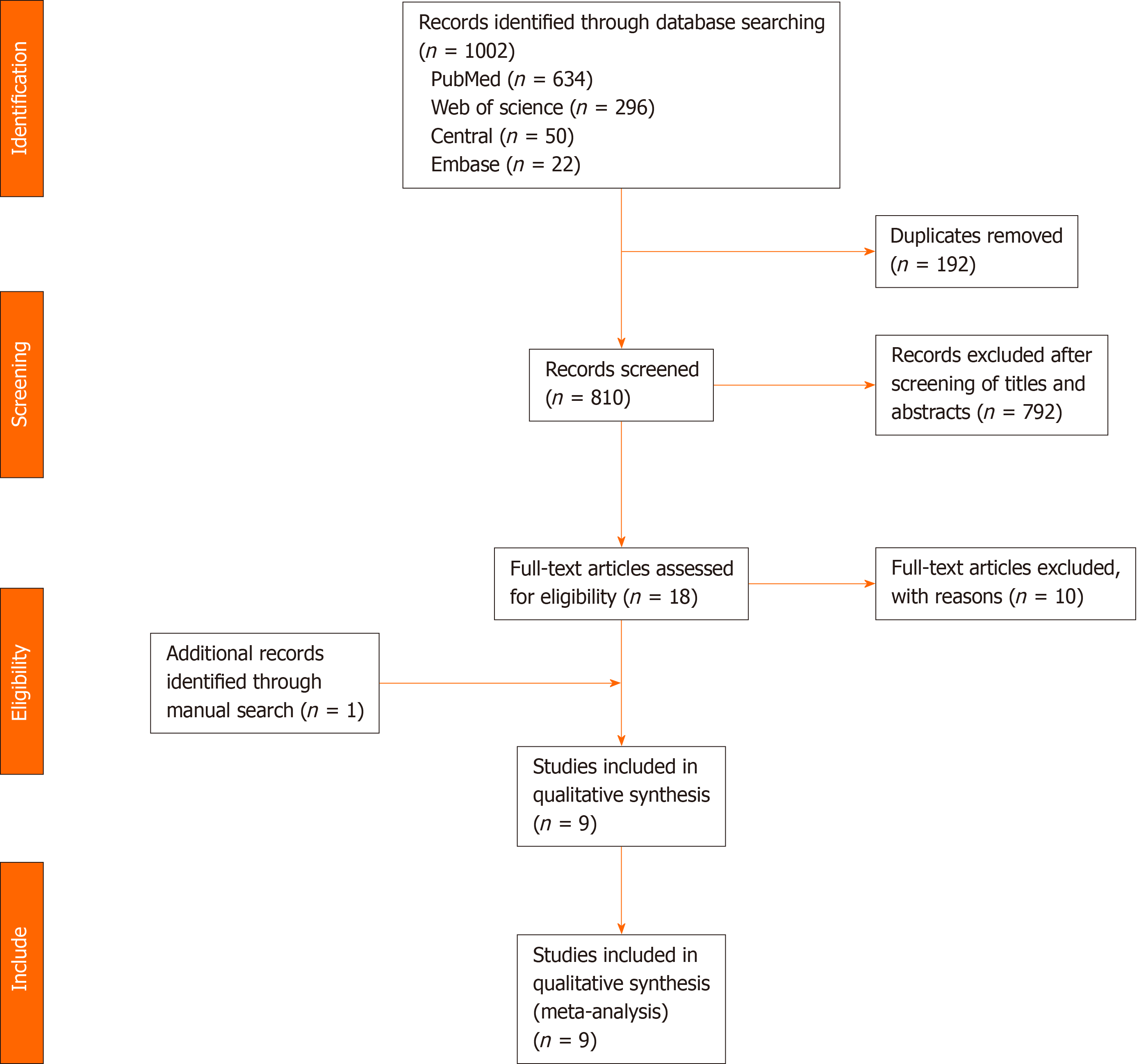
The electronic search yielded 1002 references from the four databases. After excluding 192 duplicates, 810 records remained for a title and abstract screening. We had 18 relevant articles for full-text screening: Eight fulfilled the inclusion criteria, and ten were excluded (one article not in English, six articles were case reports or included less than five cases, two articles the data of interest could not be extracted, and in one article the same data was reported in one of the included articles). The manual search of the included articles references imported one additional article. Nine studies[11-19] were ultimately included in the qualitative and quantitative analyses. The flow diagram of the study selection process is shown in Figure 1.
Nine studies included a total of 129 FHFs from which basic demographic data were extracted (the data on outcomes were extracted from 127 FHFs, as in one study[15], the authors reported missing the assessment of two patients in their results section). Two studies[15,16] were prospective, while seven[11-14,17-19] were retrospective. Across studies, the mean age was 38.2 years (range from 17 to 64). The average follow-up period was 38.4 mo (ranged from 10.8 to 77.0). The majority of participants were males (76.4%). In one study[18], the fracture classification was not reported, while in the remaining eight studies, the fracture classification according to Pipkin was as follows, 77 (62.6%) type I and II, while 46 (37.4%) were type IV, and none (0%) were Pipkin type III. All patients underwent fixation (96.9%) except four (3.1%) patients who underwent fragment excision; no patient underwent total hip arthroplasty as the primary management. Details for included studies are summarized in (Table 1).
| Ref. | Study design | Sample size | Age1, yr | Sex | Pipkin classification (I/II/III/IV) | Management | Implant | Follow up1, mo | ||
| M | F | Fixation | Excision | |||||||
| Henle et al[11], 2007 | Retrospective | 12 | 39.8 (26-71) | 10 | 2 | 1/3/0/8 | 12 | 0 | Mini or small fragment cortical screws (2.0-2.7 mm) or Herbert screws or absorbable pins | 31.1 (3-96) |
| Solberg et al[12], 2009 | Retrospective | 12 | - | 10 | 2 | 0/0/0/12 | 11 | 1 | Headless variable-pitch screws or Herbert screws | 47 (24-71) |
| Mostafa et al[13], 2014 | Retrospective | 12 | - | - | - | 12/0/0 | 12 | 0 | Partially threaded cancellous screws or Herbert headless screws | 31 (24-84) |
| Massè et al[14], 2015 | Retrospective | 13 | 34 (22-54) | 11 | 2 | 5/2/0/6 | 13 | 0 | 2.7 mm nonabsorbable screws | 77 (26-122) |
| Gavaskar et al[15], 2015 | Prospective | 28 | - | - | - | 6/22/0/0 | 26 | 2 | 2.4 mm headless screws (Synthes-India). | 36 (25-46) |
| Wang et al[16], 2019 | Prospective | 12 | 39.9 ± 12.2 | 8 | 4 | 4/3/0/5 | 12 | 0 | 3.2 mm Herbert screws or partially threaded screws | 35 (25-48) |
| Engel et al[17], 2020 | Retrospective | 7 | 39.57 (17-64) | 4 | 3 | 0/0/0/7 | 6 | 1 | Buried headless screw | 29.8 (11.6-67.2) |
| Rana et al[18], 2020 | Retrospective | 6 | 42 (32-54) | 4 | 2 | - | 6 | 0 | Herbert (headless) screw | 10.8 (8-18) |
| Khalifa et al[19], 2020 | Retrospective | 27 | 33.8 (18-45) | 21 | 6 | 6/13/0/8 | 27 | 0 | 4 mm partially threaded cancellous screws or Herbert headless screws | 48 (24-72) |
Associated intraarticular injuries: Regarding the intraarticular associated injuries (other than the primary fractures either in the femoral head or the acetabulum), in four studies[12,14,15,19], the authors reported intraoperative diagnosis of Labral injuries at an incidence of 41.3% (33 out of 80 hips). Head impaction injury was reported in three studies[14,15,19], which occurred at an incidence of 23.5% (16 out of 68 hips).
Operation time: It was reported in five studies[12-14,16,18]. However, we were able to pool the results of four studies[12-14,16] due to incomplete data from the fifth study. No significant heterogeneity was detected (I² = 41.33%, P = 0.164) using the fixed-effect model for analysis. The mean operation time ranged from 120.0 to 155.2 min, with the pooled estimate being 123.7 (95%CI: 116.58–130.89). The result was statistically significant (Z = 33.91, P = 0.000). Details of operation time in included studies are shown in (Table 2).
| Ref. | Operation time | Blood loss |
| Solberg et al[12], 2009 | 121.0 ± 28.3 (102-215) | 350.00 ± 125.00 (250-750) |
| Mostafa et al[13], 2014 | 120.0 ± 19.7 | 283.00 ± 124.90 |
| Massè et al[14], 2015 | 155.2 ± 53.1 | 1436.90 ± 663.80 |
| Wang et al[16], 2019 | 124.2 ± 22.1 | 437.50 ± 113.10 |
| Engel et al[17], 2020 | NR | 503.00 ± 181.25 |
| Rana et al[18], 2020 | 90.0 | 450.00 |
Blood loss: It was reported in six studies[12-14,16-18]. However, we were able to pool the results of five studies[12-14,16,17] due to incomplete data from the sixth study. We used the random effect model for analysis as significant heterogeneity was detected (I² = 91.52%, P = 0.000). The mean amount of blood loss ranged from 283.0 to 1436.9 mL, with the pooled estimate being 491.9 (95%CI: 347.01–636.77). The result was statistically significant (Z = 6.66, P = 0.000). Details of blood loss in included studies are shown in (Table 2).
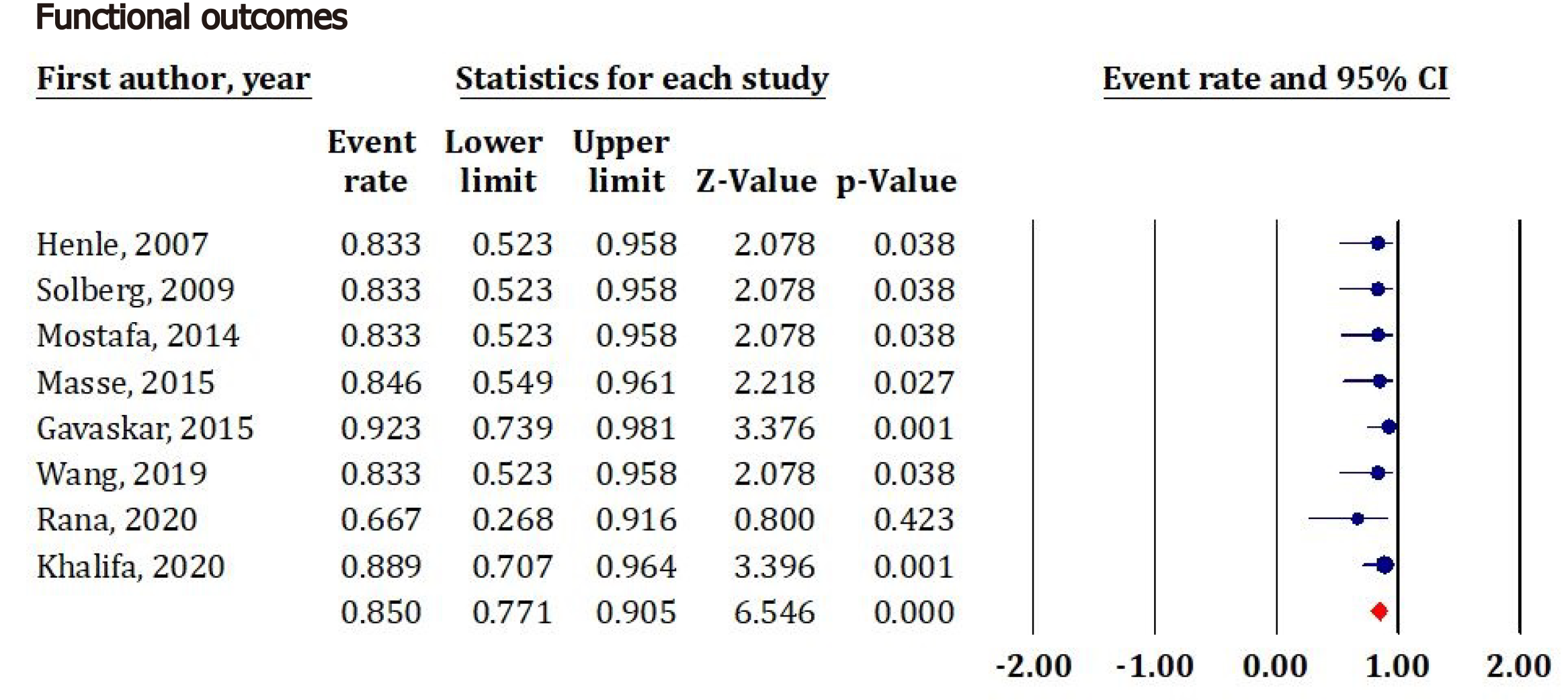
Functional outcomes (Figure 2) of the hip were reported in eight studies[11-16,18,19], but the assessment methods used were different. The Harris Hip Score (HHS) was used in three studies[14,18,19], in six studies[11-13,15,16,19] Merle d’Aubigne-Postel score was used, Thompson–Epstein scale was used in three studies[11-13], and the Oxford Hip Score was used in one study[15]. In the current meta-analysis, a satisfactory functional outcome was defined as HHS or Merle d’Aubigne-Postel score graded as excellent or good. No significant heterogeneity was detected (I² = 0%, P = 0.893) using the fixed-effect model for analysis. The event rates of satisfactory outcome ranged from 0.62 to 0.98, with the pooled estimate being 0.85 (95%CI: 0.77-0.91). The result was statistically significant (Z = 6.55, P = 0.000). According to individual assessment score or scale, excellent or good results were obtained in 87.9% (29 of 33 hips), 87.1% (88 of 101 hips), and 83.3% (30 of 36 hips) according to HHS, Merle d’Aubigne-Postel score, and Thompson–Epstein scale, respectively.
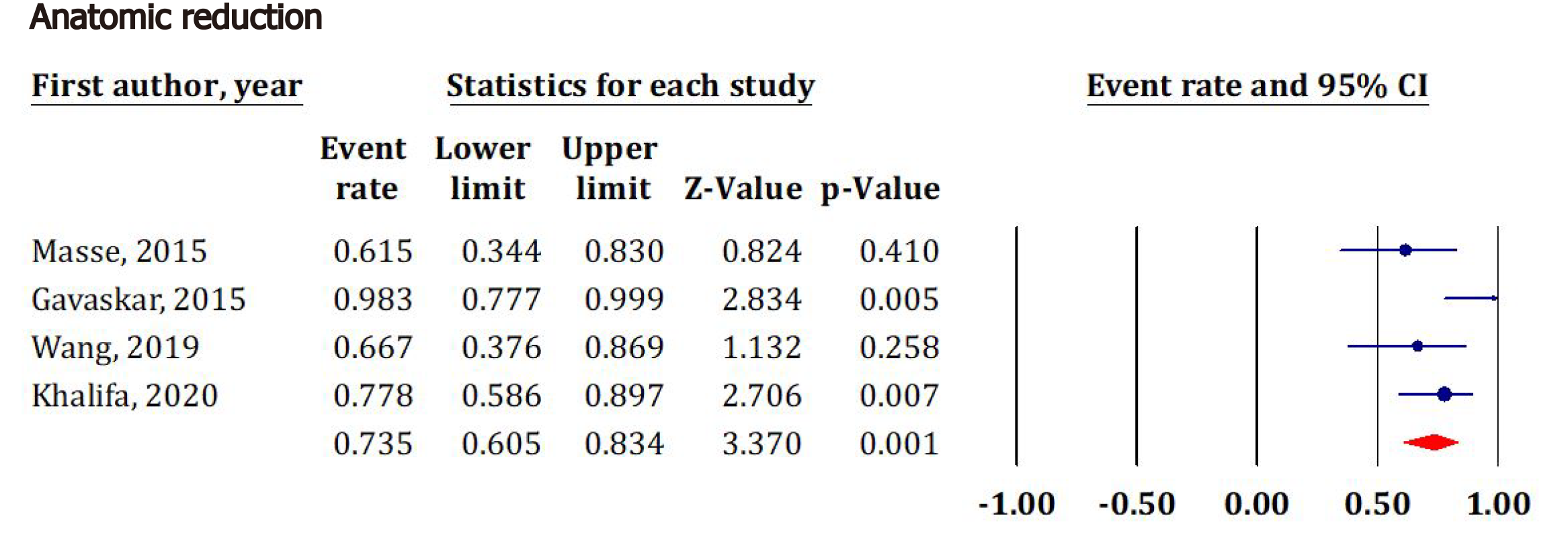
Four studies[14-16,19] reported radiological outcomes in terms of obtaining fracture anatomical reduction. No significant heterogeneity was detected (I² = 49.66%, P = 0.114) using the fixed-effect model for analysis. The overall incidence of anatomic reduction ranged from 0.30 to 0.86, with the pooled estimate being 0.74 (95%CI: 0.61–0.83). The result was statistically significant (Z = 3.37, P = 0.001, Figure 3).
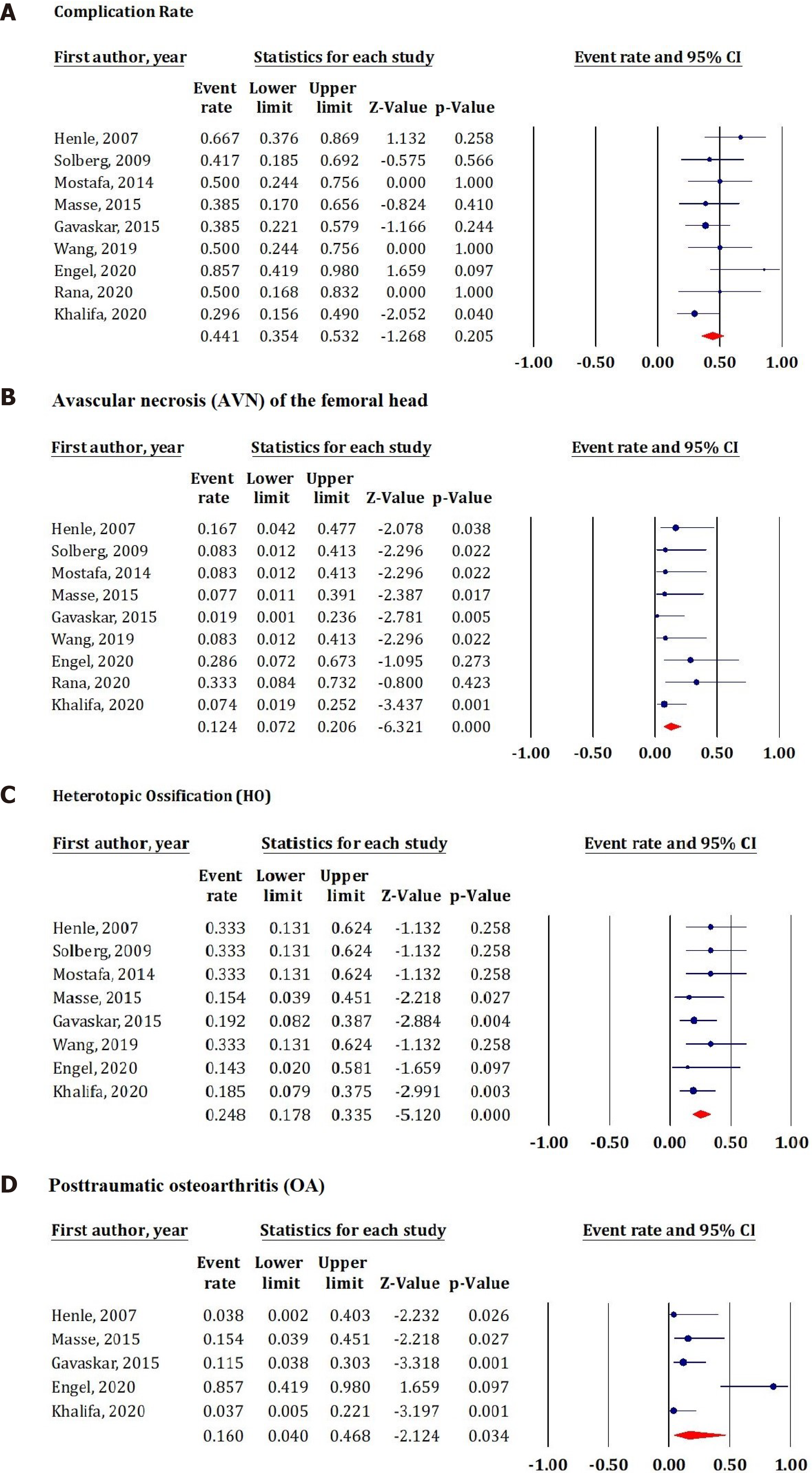
All nine studies[11-19] reported on the postoperative complications, namely AVN of the femoral head, heterotopic ossification (HO) formation, posttraumatic osteoarthritis (OA), deep infection, trochanteric bursitis, and nonunion of the TFO. No significant heterogeneity was detected (I² = 11.18%, P = 0.342) using the fixed-effect model for analysis. The overall incidence of postoperative complications ranged from 0.30 to 0.86, with the pooled estimate being 0.44 (95%CI: 0.35–0.53). The result was statistically insignificant (Z = -1.27, P = 0.205) (Figure 4A).
AVN of the femoral head: AVN was reported in all nine studies[11-19]. No significant heterogeneity was detected (I² = 0%, P = 0.509) using the fixed-effect model for analysis. The incidence of AVN ranged from 0.02 to 0.33, with the pooled estimate being 0.12 (95%CI: 0.07–0.21). The result was statistically significant (Z = -6.32, P = 0.000) (Figure 4B).
HO formation: HO was reported in eight studies[11-17,19]. No significant heterogeneity was detected (I² = 0%, P = 0.798) using the fixed-effect model for analysis. The incidence of HO ranged from 0.14 to 0.33, with the pooled estimate being 0.25 (95%CI: 0.18–0.34). The result was statistically significant (Z = -5.12, P = 0.000) (Figure 4C). According to the Brooker classification system[20], there was grade I in ten (33.3%) patients, grade II in 13 (43.3%), grade III in six (20%), and grade IV in one (3.4%). Excision was required in three (10%) patients.
Posttraumatic OA: OA was reported in five studies[11,15,17,19]. We used the random effect model for analysis as significant heterogeneity was detected (I² = 71.82%, P = 6.696). The incidence of OA ranged from 0.04 to 0.86, with the pooled estimate being 0.16 (95%CI: 0.04–0.47). The result was statistically significant (Z = -2.12, P = 0.034) (Figure 4D).
Other complications: Further complications that were not included in the meta-analysis were presented as follows. Nonunion of the TFO was reported in five studies[11,13-16,19] and occurred at an incidence of 3.4% (3 out of 89 hips). Presence of infection was reported in six studies[13-17,19] and occurred at an incidence of 2.1% (2 out of 97 hips). Trochanteric bursitis was reported in one study[15], which occurred at an incidence of 3.8% (1 out of 26 hips).
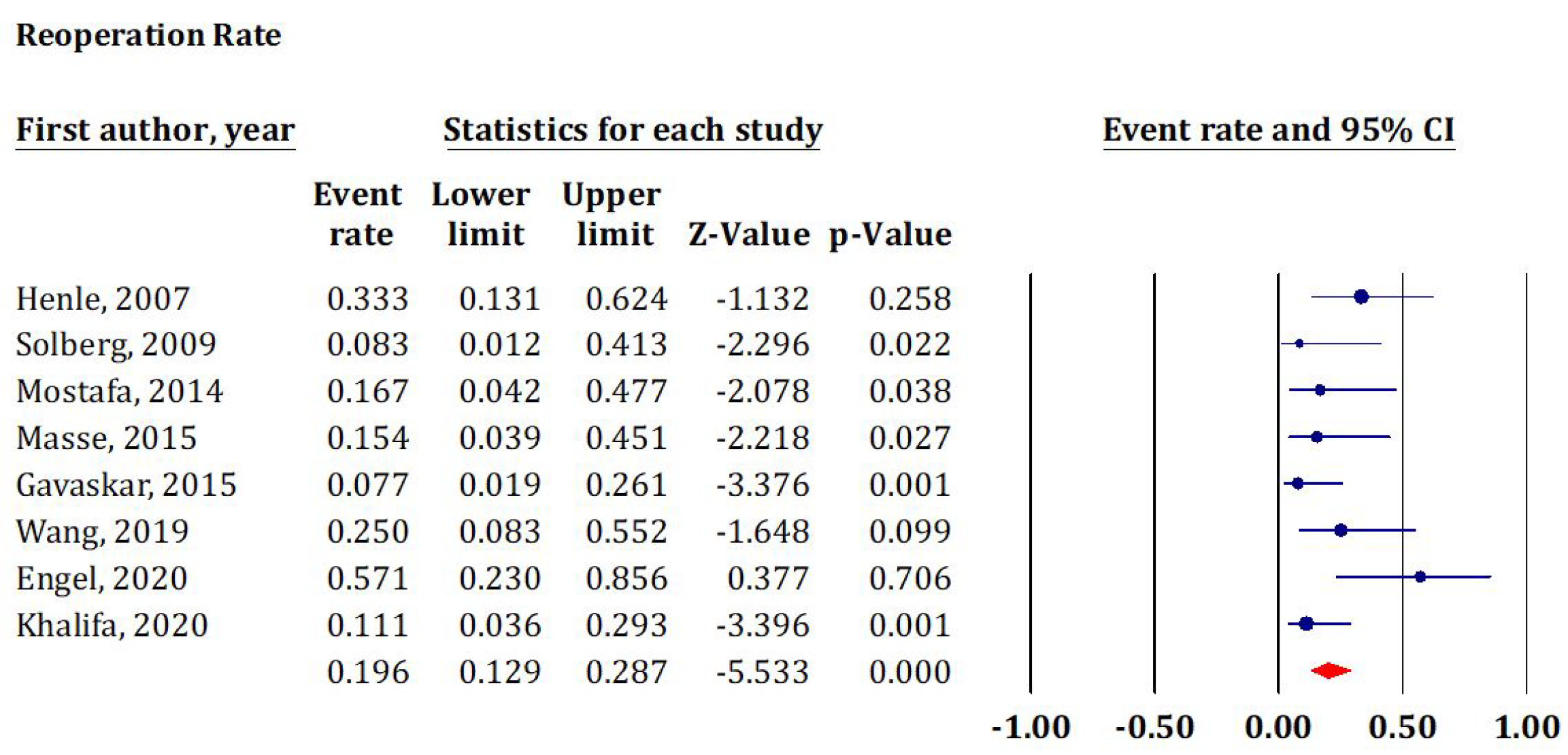
Reoperation rate was reported in eight studies[11-17,19]. No significant heterogeneity was detected (I² = 36.16%, P = 0.140) using the fixed effect model for analysis. The event rate for reoperation ranged from 0.08 to 0.57, with the pooled estimate being 0.20 (95%CI: 0.13–0.29) (Figure 5). The result was statistically significant (Z = -5.53, P = 0.000). Details of the reoperations required are in Table 3.
| Ref. | Indication of reoperation | Intervention |
| Henle et al[11], 2007 | 2 AVN | THA |
| 2 HO | Excision | |
| Solberg et al[12], 2009 | 1 AVN | THA |
| Mostafa et al[13], 2014 | 1 AVN | THA |
| 1 TFO Nonunion | Revision of fixation | |
| Massè et al[14], 2015 | 1 AVN | THA |
| 1 OA | THA | |
| Gavaskar et al[15], 2015 | 1 Infection | Debridement |
| 1 Bursitis | Screw removal | |
| Wang et al[16], 2019 | 1 AVN | THA |
| 1 HO | Excision | |
| 1 TFO Nonunion | Revision of fixation | |
| Engel et al[17], 2020 | 2 OA/ AVN | THA |
| 1 OA/HO | THA | |
| 1 OA/Metal failure/Infection | Revision/Girdlestone/THA | |
| Khalifa et al[19], 2020 | 2 AVN | THA |
| 1 OA | THA |
FHFs possess a challenge to the trauma surgeon, owing to the lack of a standard protocol for management and the various controversial issues around the best management option. The surgeon has to choose between conservative and surgical management. If the latter was chosen, then the surgeon must decide whether will it be excision or ORIF and through which approach it would be carried out[16,21,22]. Various surgical approaches have been utilized, including medial (Ludloff), anterior Smith-Petersen (S-P), posterior Kocher-Langenbeck (K-L), and anterolateral (Watson-Jones) approaches. Even hip arthroscopy was reported to be a way of management; SHD has emerged in the past few years and gained popularity as an option to approach and treat FHFs[2,3,6,23].
The most important findings in the current systematic review and metanalysis are that a large percentage of patients with FHFs obtained proper postoperative hip joint function after being managed through SHD; this approach enabled the surgeon to achieve anatomical fracture reduction and an acceptable rate of postoperative complications, mainly femoral head AVN, HO formation, and posttraumatic OA develop
In the systematic review by Giannoudis et al[2], the data regarding the surgical approaches were collected from 14 articles forming 177 surgical cases and was distributed as follows: The K-L was the most commonly used in 72 (40.7%) cases, followed by the S-P in 44 (24.9%), in third place was the SHD through TFO, which was used in 36 (20.3%). The remaining were other approaches reported in fewer numbers (lateral, anterolateral, medial, and dual approach). Thirty-six FHFs were treated through SHD, which was driven from four studies[2], while in the current systematic review, we included data of 129 FHFs from nine studies, meaning that in the past 10 years, the cases treated through SHD nearly tripled, indicating that this approach is gaining popularity among trauma surgeons.
In the current systematic review, the reported average operative time was 123.7 minutes, which is considered to be shorter than the operative time reported with the K-L approach but longer than the S-P. In a study by Wang et al[24], the authors compared managing Pipkin type I and II FHFs (21 through S-P and 18 through K-L). The average operative time for the S-P approach group was 96.9 ± 14.8 min, which was significantly shorter than the K-L approach group where the average operative time was 131.8 ± 21.2 min (P < 0.001)[24]. Many factors could affect the operative time, such as the presence of a concomitant injury that needed further management, such as an acetabular fracture (which was present in the current systematic review in 37.4% of the patients) or the presence of intra-articular injuries, mainly labral and head impaction injuries that were reported in the current systematic review in 41.3% and 23.5% of patients, respectively. Another factor that might play a role is the surgical skill and familiarity of the surgeon with the SHD approach and the learning curve needed to master managing such injuries through SHD, which we were unable to assess.
The relatively prolonged operative time and the presence of associated injuries led to an increase in the blood loss, as the reported average blood loss in the current systematic review was 491.9 mL, with a maximum blood loss of 1436.9 mL as reported in one study[14]. In Wang et al[24] study, the average blood loss was lower in both approaches than what was reported with SHD in the current review, and the S-P approach group was even significantly lower than the K-L group, 103.3 ± 28.5 vs 334.5 ± 58.9, respectively (P < 0.001).
Many fixation devices could be used when ORIF is decided, such as headless subchondral screws, countersinking lag screws, bioabsorbable pins or screws, and suture fixation[15,25-27]. The same diversity was reported in the current systematic review, as various implants were used for fracture fixation, as reported in (Table 1). Some of the fixation devices had been criticized for causing foreign body reactions such as biodegradable screws or pins[26]; metal implants may lead to stress shielding besides causing an allergic reaction in susceptible patients[28].
Although there was diversity in reporting the functional outcomes among the studies included in this meta-analysis owing to implementing different assessment scales and scores, an overall satisfactory functional outcome (defined as excellent or good according to HHS or Merle d’Aubigne-Postel) was reported in 85% of the patients. Giannoudis et al[2] studied the relation between the functional outcomes and the utilized approach in 119 cases from nine studies. Excellent and good results according to the Thompson–Epstein scale was reported in 83.4% of patients treated through SHD compared to 65.4% and 49% in patients who received S-P or K-L approaches, respectively. In the current systematic review, we found nearly the same result as 83.3% of the patients where the Thompson–Epstein scale was used for functional assessment reported being excellent or good. However, the functional results obtained in patients treated through SHD were better than what was reported in other studies using the K-L or S-P approaches. In a study by Del Core et al[29], they retrospectively reviewed the results of 22 patient managed for FHFs (five Pipkin I, three Pipkin II, 0 Pipkin III, and 14 Pipkin IV). Surgical intervention was needed in 18 (82%) patients: S-P approach was used in 5 (28%) patients, and K-L approach in 13 (72%). Overall functional results (regardless of the approach used) according to the Thompson and Epstein scale were excellent and good in 12 (54%) patients, fair and poor in 10 (46%)[29]. In a systematic review and meta-analysis carried out by Wang et al[21] comparing the S-P vs K-L approaches for managing Pipkin type I and II fractures, five case-control trials were evaluated, including data of 68 patients (34 in each approach). An acceptable hip function (excellent or good) according to Thompson and Epstein scale was achieved in 67.6% (23/34) treated through the S-P approach, and this was not different from the K-L approach (P = 0.82)[21].
There is no agreement on a scale or specific criteria to assess the quality of FHF reduction (as what is to be considered as non-anatomical or mal-reduction) in the postoperative period and follow-up radiographs, which makes comparison across studies difficult. However, Massè et al[14] was the first to describe using the Matta criteria[30] (originally described for acetabular fracture quality of reduction assessment) and applied it to the FHFs. In the current systematic review, a postoperative anatomic reduction was reported in about 74% of the patients reported from four studies. Three of them[14,16,19] reported using the Matta criteria, while in the fourth study[15], the authors did not report a specific method of assessment. As the SHD allows for 360 degrees of head exposure, it is postulated that it will allow a better anatomical reduction of the fracture compared with the limited visualization offered by other approaches[7].
The three major reported complications after FHF management had been alternating between AVN of the femoral head, HO formation, and posttraumatic OA as reported in many studies regardless of the approach used for surgery[1-3,25]. Controversy exists as to whether the trauma incident itself or the surgical intervention (including the surgical approach) is the cause leading to these complications; for example, the timing of reduction (if the patient presented with a dislocated hip) could affect the complication incidence[8,11,31], and disruption of the femoral head vascularity (leading to AVN) can occur at the time of trauma rather than being a consequence of surgical intervention[32].
The overall incidence of postoperative complications in the current systematic review was 44%; however, only half of those patients needed further intervention. This incidence was higher than what was reported in the initial series by Ganz et al[7] (treating non-traumatic conditions), where they reported a major complication rate of 3.3% in 213 patients. However, the incidence was lower than the overall complications reported in the Giannoudis et al[2] systematic review, where the major three complications were reported to occur at an incidence of 68%, which reached 84.4% when cases treated through SHD were excluded.
Ganz et al[7] reported 0% of AVN in their study; however, the cases they reported were non-traumatic conditions. The authors proved the safety of SHD in regard to hip vascularity preservation. In the systematic review by Giannoudis et al[2], after a mean follow-up of 59.7 mo, AVN was reported in 2 (5.3%) out of 38 patients treated through the S-P approach, 3 (8.3%) out of 36 patients treated through SHD, and 11 (16.9%) patients out of 65 treated through the K-L approach. The authors reported that the chance of a patient to develop AVN when treated through a K-L approach was 3.67 and 2.24 times higher compared to S-P or SHD approach, respectively (P > 0.05)[2]. In the current systematic review, we reported an incidence of AVN of 12%, which was better than the K-L approach and higher than the S-P approach, as reported in the previous study.
The same previous finding was confirmed in further studies as follows. In a study by Scolaro et al[1] on 147 FHFs classified according to Pipkin classification into type I (27%), II (42%), III (4.7%), IV (15%), and as others which included impaction injuries (10%). ORIF was performed in 78 (53.1%) fractures; 97% of these were approached through the S–P approach. After a mean follow-up of 12.4 months, 6 (8.7%) patients developed AVN, mostly all Pipkin III fractures (n = 5) had AVN[1]. In a study by Stannard et al[33] where they surgically treated 17 patients diagnosed with FHFs, in 6 patients (35%) the S-P approach was used, 10 (59%) underwent the K-L approach, and 1 (6%) underwent dual anterior and posterior approaches. The authors reported that 4 of the 5 patients who had AVN were managed through the K-L approach. They reported that the odds ratio was 3.2 times higher for AVN when the K-L approach was used compared to the S-P approach[33].
In a retrospective analysis by Swiontkowski et al[34] of 24 patients presented with Pipkin types I and II (12 patients were treated through the K-L approach and 12 through the S-P approach), the authors reported an incidence of AVN of 16.7% with the K-L approach compared to 0% when the surgery was performed through the S-P approach[34]. In the systematic review by Guo et al[35], they included studies from 1980 to April 2009 to evaluate the relation of the surgical approach to the development of AVN; ten studies were eligible to be included with a total of 176 cases. The incidence of AVN was more with the K-L approach (16.9%) than the S-P (7.9%); however, the difference was not significant[35].
It is not clearly defined if HO formation relates to the surgical approach or the traumatic muscle injury[25]. The exact pathogenesis is still unclear, but other factors rather than the type of the approach have been accused such as being a polytrauma patient, concomitant craniocerebral or thoracoabdominal trauma, male sex, the time to hip reduction (if dislocated), delay to surgery, and associated fractures as in type III and IV injuries[36-38]. In the current systematic review, SHD was associated with HO formation at an incidence of 25%; surprisingly, this incidence was lower than the incidence reported with treating non-traumatic conditions as Ganz et al[7] reported 37% of their patients having HO formation.
In another study by Kargin et al[39] where they evaluated 44 patients who underwent SHD for non-traumatic causes with a mean follow up of 66 mo, they reported an incidence of HO formation of 36.5%. The incidence reported in the current systematic review was lower than what was reported by Giannoudis et al[2], as they noted that HO of any grade occurred in 44.7% of patients treated with the S-P approach and in 32.3% of patients treated through the K-L approach. However, the difference between approaches was not significant (P > 0.05). The authors reported an incidence of 47.2% in the patients treated through SHD included in their review (which was nearly double the incidence in the current review). They estimated a 1.87 times higher rate of HO following SHD; however, they noted that this higher incidence did not affect the functional outcomes[2].
In the systematic review by Guo et al[35], HO formation was lower in the SHD group (33.3%) compared to the S-P or K-L approaches (42.1% and 36.9%), although the difference was not statistically significant. In a study by Peng et al[40] reporting their results of treating FHFs at an average follow up of 3.3 years, 18 patients treated through the S-P approach, and 6 through the K-L approach, the overall incidence of HO was 43%. No surgical intervention was needed.
In the current systematic review, lower grades of HO (Brooker I and II) occurred in 76.5 % of the patients, while higher grades (III and IV) occurred in 23.4 %. This was nearly similar to the results obtained from the study by Scolaro et al[1] where low-grade HO developed in 74% of the patients, while higher grades developed in 24%. However, they had a lower incidence of surgical intervention for HO in only 2.9% of patients who required surgical excision compared to 10% of the patients in the current systematic review. The lower incidence of HO formation in the current systematic review compared to the previous reports may be attributed to the advancement in HO prophylaxis techniques, more orientation about the problem, which was gained from previous studies, and to increasing experience of surgeons with the SHD technique paying more respect to soft tissues.
This complication could develop due to improper fracture reduction or as a consequence of AVN, as in some studies the authors reported AVN and OA as a single entity[1]. In the current systematic review, we reported an incidence of posttraumatic OA of 16% after SHD, which is considered higher than the incidence reported with cases managed through SHD in the Giannoudis et al[2] systematic review, where the authors reported 0% incidence. However, the incidence reported with SHD was still lower than other approaches, as Giannoudis et al[2] reported an incidence of 21.0% and 29.2% in patients treated through the S-P and K-L approaches, respectively. They estimated a 20.3 (P = 0.04) and 30.6 (P = 0.018) times higher incidence of posttraumatic OA development when the S-P or K-L approach was used, respectively, compared to SHD[2]. An increased incidence with other approaches was reported in other studies, as in the study by Wang et al[24] the authors reported a posttraumatic OA incidence of 14.3% and 16.7% with the S-P and K-L approaches, respectively. The difference was insignificant (P = 1.000). Del Core et al[29] reported an overall incidence of 23% in their patients. In the current systematic review, the increased incidence of OA development could be attributed to the fact that 6 of the 12 patients who developed posttraumatic OA were reported from Engel et al[17] study, where all the included cases were Pipkin type IV with an incidence of OA of 85.7% (6 out of 7 patients), owing to the severity and complexity of this type of injury.
This was the lowest reported complication in the current systematic review, which occurred at an incidence of 2.1%. Only 2 patients required further surgical inter
The possibility of TFO nonunion and the development of trochanteric bursitis with lateral thigh pain secondary to irritation by the screws used to fix the TFO are unique complications to the SHD approach[7,13,41,42]. An incidence of TFO nonunion was reported in five studies in the current review giving an incidence of 3.4%, and two patients required refixation. The incidence was even lower in the studies reported on non-traumatic conditions, as in a multicentre study by Sink et al[43]. They evaluated 334 hips from eight different North American centres with a minimum of 12 months follow-up. TFO nonunion was reported in six hips (1.8%), all united after revision of the internal fixation. Ganz et al[7] reported three (1.4%) cases with TFO nonunion. In the current systematic review, we reported an incidence of trochanteric bursitis with lateral thigh pain in 1 (3.8%) patient out of 26 hips, which required screw removal. In the study by Kargin et al[39], lateral thigh pain was reported to occur in 28.8% of their patients.
Trauma surgeons were encouraged to incorporate SHD in the management of FHFs as it offered many advantages. Firstly, the wide exposure (360 degrees) of both the femoral head and the acetabulum makes it possible to treat both pathologies if present (as in Pipkin Type 4) at the same time. Secondly, it enables the detection and dealing with other intraarticular injuries such as labrum injury or head impaction injuries, which may be difficult to diagnose in preoperative imaging studies[44-46]. Thirdly, the ability of the approach allows the surgeon to perform better reduction and fixation of the fractured fragments. Lastly, it enables the ability to check the vascularity of the femoral head intraoperatively by using the drill test [7,8].
First, we did not compare the results obtained from SHD with other approaches, which might be due to the lack of comparative studies in this field. Second, one crucial point that was not assessed is the experience of the surgeon with this approach. Some authors reported having no familiarity with this approach[40]. On the other hand, in two studies[14,19] included in the meta-analysis, the authors reported having previous experience with the SHD approach; however, we found it unmeasurable and challenging to state the learning curve needed to master this technique. Lastly, limiting the article search to the past 20 years might lead to missing some earlier articles; however, we aimed at presenting as updated data as possible.
Incorporating SHD as an optional approach in the armamentarium of approaches in dealing with FHFs enables trauma surgeons to properly manage these intraarticular fractures and detect and deal with additional intraarticular injuries. It offered acceptable functional and radiological outcomes with a wide range of safety in regards to the hip joint vascularity and the development of AVN, the formation of HO, and the development of posttraumatic OA; however, it still carries its unique risk of complications such as TFO nonunion and persistent lateral thigh pain.
Surgical hip dislocation (SHD) was introduced as a safe approach for managing various hip pathologies. It gained popularity among trauma surgeons as a new approach for the management of femoral head fractures (FHFs). Several studies were published on this subject. However, no systematic reviews were carried pooling these data together to generate stronger evidence of this approach utility.
FHFs are considered as intraarticular fractures. Anatomical reduction and preservation of its vascularity are two mandatory perquisites for obtaining optimum outcomes; SHD was introduced for the management of these fractures with the advantage of preserving femoral head vascularity and providing 360 degree visualization of the femoral head.
We carried out this systematic review and meta-analysis to evaluate the efficacy (functional and radiological outcomes) as well as the safety (complications incidence) of using the SHD approach for management of FHFs, which could help encourage more surgeons to widely adopting this approach in their practice.
Four major databases were searched (PubMed, Embase, Web of Science, and Cochrane Central Register of Controlled Trials) to collect eligible studies reporting on various outcomes (functional, radiological, and complications) after utilizing SHD as described by Ganz in the management of FHFs. Articles basic, surgical, functional, radiographic, and complications data were collected from the included articles.
Nine studies were eligible and included in the analysis, forming a total of 129 FHFs with an average follow up of 38.4 mo. The average operative time and blood loss were 123.74 min and 491.89 mL, respectively. Excellent and good functional outcomes were obtained in 85% of the patients, while anatomical fracture reduction could be obtained in 74%. The overall complication rate was 44%; the main reported complications were femoral head avascular necrosis, heterotopic ossification, and osteoarthritis, which occurred at an incidence of 12%, 25%, and 16%, respectively. A unique complication to SHD was trochanteric flip osteotomy nonunion and trochanteric bursitis, which occurred at an incidence of 3.4% and 3.8%, respectively. The issue of surgeon experience and its relation to the results and utilization of this approach is still to be studied.
We believe that this was the most recent systematic review collecting and reporting the data regarding the efficacy and safety of SHD as an approach for management of FHFs; the results of this systematic review suggest the high safety profile of this approach with acceptable functional outcomes.
We believe that there is a need for further studies and systematic reviews comparing the SHD approach to conventional approaches (anterior and posterior) in the management of FHFs to prove its safety and efficacy.
We would like to thank Dr. Ahmed M Ahmed for his great effort in performing the statistical analysis for the current systematic review and metanalysis.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maslennikov R S-Editor: Wang JL L-Editor: Filipodia P-Editor: Li JH
| 1. | Scolaro JA, Marecek G, Firoozabadi R, Krieg JC, Routt MLC. Management and radiographic outcomes of femoral head fractures. J Orthop Traumatol. 2017;18:235-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Giannoudis PV, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009;40:1245-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 3. | Giordano V, Giordano M, Glória RC, de Souza FS, di Tullio P, Lages MM, Koch HA. General principles for treatment of femoral head fractures. J Clin Orthop Trauma. 2019;10:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am. 1957;39-A:1027-42 passim. [PubMed] |
| 5. | Kim TS, Oh CW, Kim JW, Park KH. an Irreducible Hip dislocation with femoral Head fracture. J Trauma Injury. 2018;31:181-188. |
| 6. | Johal H, Axelrod D, Bhandari M. Femoral Head Fractures. In: Giannoudis PV, editor. Fracture Reduction and Fixation Techniques. Cham: Springer International Publishing, 2020: 183-191. |
| 7. | Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 633] [Cited by in RCA: 651] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 8. | Keel M, Eid K, Isler B, Trentz O, Ertel W. The role of surgical hip dislocation in the treatment of acetabular and femoral head fractures. Eur J Trauma. 2005;31:138-147. |
| 9. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47200] [Article Influence: 2950.0] [Reference Citation Analysis (0)] |
| 10. | Weir CJ, Butcher I, Assi V, Lewis SC, Murray GD, Langhorne P, Brady MC. Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol. 2018;18:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 250] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 11. | Henle P, Kloen P, Siebenrock KA. Femoral head injuries: Which treatment strategy can be recommended? Injury. 2007;38:478-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Solberg BD, Moon CN, Franco DP. Use of a trochanteric flip osteotomy improves outcomes in Pipkin IV fractures. Clin Orthop Relat Res. 2009;467:929-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Mostafa MF, El-Adl W, El-Sayed MA. Operative treatment of displaced Pipkin type I and II femoral head fractures. Arch Orthop Trauma Surg. 2014;134:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Massè A, Aprato A, Alluto C, Favuto M, Ganz R. Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop Relat Res. 2015;473:3744-3751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 15. | Gavaskar AS, Tummala NC. Ganz Surgical Dislocation of the Hip Is a Safe Technique for Operative Treatment of Pipkin Fractures. Results of a Prospective Trial. J Orthop Trauma. 2015;29:544-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Wang J, Cai L, Xie L, Chen H, Guo X, Yu K. 3D printing-based Ganz approach for treatment of femoral head fractures: a prospective analysis. J Orthop Surg Res. 2019;14:338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Engel JL, Johnsen P, Patel NK, Satpathy J, Mounasamy V. Pipkin type IV femoral head fractures: a case series and review of literature. Eur J Orthop Surg Traumatol. 2021;31:791-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Rana R, Verma D Jr, Behera S 2nd, Behera H, Raulo B. Irreducible Femur Head Fracture-Dislocation Treatment With Kocher-Langenbeck Approach With Flip Trochanteric Osteotomy: A Novel Approach. Cureus. 2020;12:e11969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Khalifa AA, Refai O, Farouk O, Abdelnasser MK. Management of femoral head fractures through surgical hip dislocation (SHD): a demanding but safe technique. Arch Orthop Trauma Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629-1632. [PubMed] |
| 21. | Wang CG, Li YM, Zhang HF, Li H, Li ZJ. Anterior approach versus posterior approach for Pipkin I and II femoral head fractures: A systemic review and meta-analysis. Int J Surg. 2016;27:176-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Oransky M, Martinelli N, Sanzarello I, Papapietro N. Fractures of the femoral head: a long-term follow-up study. Musculoskelet Surg. 2012;96:95-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Niroopan G, de Sa D, MacDonald A, Burrow S, Larson CM, Ayeni OR. Hip Arthroscopy in Trauma: A Systematic Review of Indications, Efficacy, and Complications. Arthroscopy. 2016;32:692-703.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Wang S, Li B, Li J, Zhang Z, Yang H, Liu L. Comparison of the modified Heuter approach and the Kocher-Langenbeck approach in the treatment of Pipkin type I and type II femoral head fractures. Int Orthop. 2019;43:2613-2620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Henriques R, Ramalho D, Soares do Brito J, Rocha P, Spranger A, Almeida P. Management of Pipkin Fractures Using a Safe Surgical Hip Dislocation. Case Rep Orthop. 2019;2019:3526018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Gagała J, Tarczyńska M, Gawęda K. Fixation of femoral head fractures with autologous osteochondral transfer (mosaicplasty). J Orthop Trauma. 2014;28:e226-e230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Ross JR, Gardner MJ. Femoral head fractures. Curr Rev Musculoskelet Med. 2012;5:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Hermus JP, Laan CA, Hogervorst M, Rhemrev SJ. Fixation of a Pipkin fracture with bio-absorbable screws. Case report and a review of the literature. Injury. 2005;36:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Del Core MA, Gross B, Ahn J, Wallace SB, Starr A. Clinical and Radiographic Outcomes of Femoral Head Fractures Associated with Traumatic Hip Dislocations. Strategies Trauma Limb Reconstr. 2019;14:6-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Matta JM, Tornetta P 3rd. Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res. 1996;129-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 298] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 31. | Prokop A, Helling HJ, Hahn U, Udomkaewkanjana C, Rehm KE. Biodegradable implants for Pipkin fractures. Clin Orthop Relat Res. 2005;226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Stirma GA, Uliana CS, Valenza WR, Abagge M. Surgical treatment of femoral head fractures through previously controlled hip luxation: four case series and literature review. Rev Bras Ortop. 2018;53:337-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Stannard JP, Harris HW, Volgas DA, Alonso JE. Functional outcome of patients with femoral head fractures associated with hip dislocations. Clin Orthop Relat Res. 2000;44-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 142] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 34. | Swiontkowski MF, Thorpe M, Seiler JG, Hansen ST. Operative management of displaced femoral head fractures: case-matched comparison of anterior versus posterior approaches for Pipkin I and Pipkin II fractures. J Orthop Trauma. 1992;6:437-442. [PubMed] |
| 35. | Guo JJ, Tang N, Yang HL, Qin L, Leung KS. Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: a systematic review. Int Orthop. 2010;34:319-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Firoozabadi R, O'Mara TJ, Swenson A, Agel J, Beck JD, Routt M. Risk factors for the development of heterotopic ossification after acetabular fracture fixation. Clin Orthop Relat Res. 2014;472:3383-3388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 37. | Marecek GS, Scolaro JA, Routt ML Jr. Femoral Head Fractures. JBJS Rev. 2015;3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 38. | Marchetti ME, Steinberg GG, Coumas JM. Intermediate-term experience of Pipkin fracture-dislocations of the hip. J Orthop Trauma. 1996;10:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 72] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 39. | Kargin D, Albayrak A, Atici Y, Yapici F, İlvan G, Balioğlu MB. The complications after open hip dislocation in hip surgery. Acta Orthop Belg. 2017;83:74-80. [PubMed] |
| 40. | Peng SH, Wu CC, Yu YH, Lee PC, Chou YC, Yeh WL. Surgical treatment of femoral head fractures. Biomed J. 2020;43:451-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 41. | Schoeniger R, LaFrance AE, Oxland TR, Ganz R, Leunig M. Does trochanteric step osteotomy provide greater stability than classic slide osteotomy? Clin Orthop Relat Res. 2009;467:775-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Ross JR, Schoenecker PL, Clohisy JC. Surgical dislocation of the hip: evolving indications. HSS J. 2013;9:60-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Sink EL, Beaulé PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J. Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am. 2011;93:1132-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 44. | Brooks RA, Ribbans WJ. Diagnosis and imaging studies of traumatic hip dislocations in the adult. Clin Orthop Relat Res. 2000;15-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 45. | Laorr A, Greenspan A, Anderson MW, Moehring HD, McKinley T. Traumatic hip dislocation: early MRI findings. Skeletal Radiol. 1995;24:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 51] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Chen Z, Liang X, Wu J, Cui J, Tang Z, Fan W, Li C, Wu W, Dai Z. [Diagnosis and treatment of acetabular labrum injury in pipkin fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2015;29:14-18. [PubMed] |