Published online May 18, 2021. doi: 10.5312/wjo.v12.i5.310
Peer-review started: January 10, 2021
First decision: February 15, 2021
Revised: February 15, 2021
Accepted: March 28, 2021
Article in press: March 28, 2021
Published online: May 18, 2021
Processing time: 121 Days and 12.9 Hours
The majority of published data report the results of biomechanical tests of various design pedicle screw performance. The clinical relevance and relative contribution of screw design to instrumentation stability have been insufficiently studied.
To estimate the contribution of screw design to rate of pedicle screw loosening in patients with degenerative diseases of the lumbar spine.
This study is a prospective evaluation of 175 patients with degenerative diseases and instability of the lumbar spine segments. Participants underwent spinal instrumentation employing pedicle screws with posterior only or transforaminal interbody fusion. Follow-up was for 18 mo. Patients with signs of pedicle screw loosening on computed tomography were registered; logistic regression analysis was used to identify the factors that influenced the rate of loosening.
Parameters included in the analysis were screw geometry, type of thread, external and internal screw diameter and helical pitch, bone density in Hounsfield units, number of levels fused, instrumentation without anterior support, laminectomy, and unilateral and bilateral total facet joint resection. The rate of screw loosening decreased with the increment in outer diameter, decrease in core diameter and helical pitch. The rate of screw loosening correlated positively with the number of fused levels and decreasing bone density. Bilateral facet joint removal signifi
Screw parameters had a significant impact on the loosening rate along with bone quality characteristics, the number of levels fused and the extensiveness of decompression. The significance of the influence of screw parameters was comparable to those of patient- and surgery-related factors. Pedicle screw loosening was influenced by helical pitch, inner and outer diameter, but screw geometry and thread type were insignificant factors.
Core Tip: The published data on the contribution of pedicle screw design to pedicle screw stability remain controversial. According to the study results, the influence of screw parameters was comparable to that of patient- and surgery-related factors. The rate of pedicle screw loosening was influenced by helical pitch, inner, and outer diameter, but the influence of screw geometry and thread type was not significant.
- Citation: Bokov A, Pavlova S, Bulkin A, Aleynik A, Mlyavykh S. Potential contribution of pedicle screw design to loosening rate in patients with degenerative diseases of the lumbar spine: An observational study. World J Orthop 2021; 12(5): 310-319
- URL: https://www.wjgnet.com/2218-5836/full/v12/i5/310.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i5.310
Severe symptomatic degenerative diseases of the lumbar spine are frequently encountered morbid conditions, for which clinically significant improvement can only be achieved by pedicle screw fixation and fusion. Pedicle screw fixation, however, is associated with frequent complications, notably screw loosening, which has an overall reported rate of from 0.8% to 27% and over 50% in patients with osteoporosis[1-4]. Taking into account complication-related concerns, several strategies have been suggested to reduce the risk of implant failure, among which optimal screw design might play a considerable role[5].
Although the potential impact of screw design on pedicle screw instrumentation failure is a topic of interest in the literature, the pros and cons of each design alteration are still unresolved[5]. The most frequently used strategy is an increase in external diameter with an optimal thread depth[6,7]. Also, it is widely assumed that a conical screw geometry provides additional pullout resistance[8-10]. While some authors expect that an optimal screw shape and helical thread pitch may provide additional bone purchase benefit, screw performance in normal and osteoporotic models remains controversial[5,8,9].
Among the many factors that affect pedicle screw fixation stability, the most thoroughly studied is bone quality. At present, there is growing evidence that bone radiodensity in Hounsfield units (HUs) can be used to predict implant failure and pseudoarthrosis[4,11,12]. The extension of fixation, anterior support with interbody cages, screw insertion technique including depth and angulation may strongly influence the pedicle screw loosening rate, potentially blurring the results of ex-vivo studies[3,13-15]. Applying the results of ex-vivo experiments is problematic, because in the vast majority of studies, pullout tests barely mimic the biomechanics of screw loosening[7,16]. Finally, the reported data on pedicle screw loosening remain controversial because of differences in the criteria used as indicators for implant loosening and heterogeneity of the enrolled groups[3].
The study aim was to estimate the contribution of screw design to the rate of pedicle screw loosening and its interrelation with other risk factors in patients with degenerative diseases of the lumbar spine.
This study was a single-center prospective evaluation of 175 nonconsecutive patients with degenerative diseases of the lumbar spine with instability of spinal segments including 60 men and 115 women with a male-to-female ratio of 0.52. The average age of the participants at the time of surgery was 54 years (standard deviation = 14.12; range 28-76 years). Patients with only axial pain and those who presented with neurological symptoms associated with spinal stenosis were enrolled. Participants underwent spinal instrumentation employing pedicle screw fixation with posterior fusion stand-alone or with transforaminal interbody fusion supplementation during the years 2012 to 2017. The duration of follow-up was 18 mo. Radiographic criteria of pedicle screw loosening were used to assess outcomes as numeric scores can be biased by causes not associated with the surgery. The study was reviewed and approved by the local institutional review board, given that no additional risks were anticipated.
The inclusion criterion was presence of degenerative disease of the lumbar spine with unstable spinal segments and confirmed by functional radiograms or the presence of low-grade symptomatic unstable spondylolisthesis. Indications for spinal instrumentation were: (1) Neurological deficit associated with spinal stenosis; (2) Neuro
The exclusion criteria were: (1) High-grade spondylolisthesis (grades 3 and 4); (2) Degenerative deformities that required fixation of more than five segments or spinopelvic fixation; (3) Tumor-related lesions of the lumbar spine; (4) Sagittal and frontal imbalance and spinopelvic parameter mismatches that required more than five-segment fixation and spinopelvic fixation; (5) Hospitalization for revision surgery; (6) Screw malposition and redirection detected on postoperative computed tomography (CT) images; (7) Different types of fusion applied on different levels; and (8) Different screw designs and sizes applied for pedicle screw fixation. This exclusion criterion was the reason why the study cohort was not consecutive.
Before the procedure, all patients underwent functional X-ray imaging and CT evaluation. The criterion for spinal instability was anterior translation greater than 3 mm or rotation more than 10°[17]. CT was used as a part of the preoperative work-up. The CT scans were performed from the T12-L5 levels using a single CT scanner (Aquilion 32, Toshiba Corporation). The scans used a slice thickness of 0.5 mm and covered a scan area of 50 cm. The scan parameters included tube voltage 120 kV, tube current 300 mA, auto mAs range 180 to 400; 1.0 s/3.0 mm/0.5 × 32, helical pitch 21.0. Integrated software was used for calculations of bone density (Vitrea Version 5.2.497.5523) incorporating a window width/window level ratio of 2000/500. During CT evaluations, measurements of a vertebral body cancellous bone radiodensity in HU were obtained at standard level of L3 in the sagittal, axial, and coronal planes; those measurements were taken by two independent radiologists. Measurements in the axial plane were taken at the level of the middle of the pedicles while those in the sagittal and coronal planes were taken along the geometric center of the vertebral body. Oval-shaped trabecular bone samples were selected using the maximal achievable diameters without traversing into cortical bone to calculate bone density in each plane. Using those values, an average radiodensity was calculated for each case.
Pedicle screw fixation with different types of polyaxial screws was used, either to augment posterolateral fusion alone or with interbody fusion. Screws with a conical core and thread (con/con), cylindrical core and thread (cyl/cyl), or cylindrical thread and conical core (cyl/con), with either V-shaped or buttress threads were used. The size of the pedicle screws was 6, 6.5, 7, or 7.5 mm. The applied technique was a standard strait trajectory for screw placement and either Wiltse or conventional open screw placement. The surgeon qualification was at least 7 years of experience. Pedicle screws were introduced at least to the anterior third of a vertebral body; bicortical screw placement was not used in the enrolled patients. Transforaminal lumbar interbody fusion (TLIF) with a single cage, or posterior fusion only were used in this study. Only autografts of locally harvested bone was used to perform TLIF and posterior fusion. If indicated, decompression of the nerve roots and spinal cord was performed. The extent of the applied decompression was classified by structures removed (i.e. unilateral facet joint removal, bilateral facet joints with interspinous ligament removal, and laminectomy).
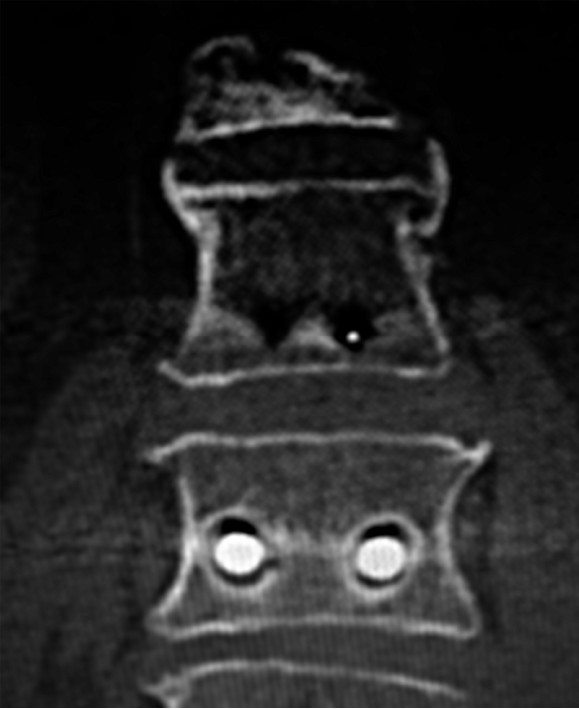
The duration of follow-up was 18 mo. All patients underwent CT evaluation at the 6, 12, and 18 mo after surgery. Patients with pedicle screw loosening detected on CT images were registered. The criterion for screw loosening was a 1 mm or greater radiolucent zone around the screw, a double halo sign, or both[3]. Figure 1 includes a CT image in a patient with signs of pedicle screw loosening. Finally, patient outcomes were reported in a dichotomized scale either with the presence signs of pedicle screw loosening regardless the number of the involved screws, or absence of this compli
Power analysis employing a Monte-Carlo method with 2000 simulations was used to calculate the required sample size (NCSS PASS 2008 v8). The association between screw loosening rate (dichotomized scale) and potential risk factors (both, continuous and dichotomized) was assessed with a general multivariate logistic regression model (Statistica 12, SPSS 22).
The characteristics of the enrolled group are shown in Table 1. By the end of the follow-up period, CT signs of pedicle screw loosening were present in 71 (40.6%) patients, 29 (16.6%) of whom presented with axial pain and Oswestry Disability Index scores over 40; the other 29 patients underwent revision surgery. The high prevalence of CT loosening signs can be explained by a considerable proportion of patients with radiodensities below 110 HU, which has a 90% specificity of osteoporosis detection. The screw parameters used in the analysis were con/con, cyl/cyl, cyl/con designs, V-shaped vs buttress thread, external, internal screw diameter, and helical pitch. The characteristics of screws used in this study are shown in Table 2.
| Characteristic | Patients, n (%) |
| Number of levels fused | |
| 1 level | 115 (65.7) |
| 2 levels | 47 (26.9) |
| 3 levels | 16 (9.1) |
| 4 levels | 1 (0.6) |
| 5 levels | 1 (0.6) |
| Fusion type | |
| Posterior fusion only | 25 (14.3) |
| TLIF | 150 (85.6) |
| Amount of decompression | |
| No resection of posterior structures | 18 (10.3) |
| Laminectomy | 46 (26.3) |
| Unilateral total facet joint removal | 108 (61.7) |
| Bilateral total facet joint removal on at least one level | 46 (26.3) |
| Bone characteristics | |
| Radiodensity, HU | M = 126.25 ± 3.20 SD = 42.31, range 43.17-282.07 |
| Design | External diameter (max) | Internal diameter (max) | Helical pitch | Type of thread | n (%) |
| cyl/cyl | 6.5 | 4.0 | 3.0 | Buttress | 6 (3.4) |
| cyl/cyl | 7.5 | 4.5 | 3.0 | Buttress | 9 (5.1) |
| cyl/con | 6.5 | 4.0 | 2.5 | Buttress | 40 (22.9) |
| cyl/con | 7.5 | 5.0 | 2.5 | Buttress | 4 (2.3) |
| con/con | 6.0 | 4.0 | 3.0 | V-shape | 48 (27.4) |
| con/con | 7.0 | 4.5 | 3.0 | V-shape | 5 (2.9) |
| con/con | 6.0 | 4.5 | 2.5 | V-shape | 49 (28.0) |
| con/con | 7.0 | 5.5 | 2.5 | V-shape | 14 (8.0) |
Patient- and surgery-related factors were bone density measured in HU, number of fused levels (the extension of fixation), posterior fusion performed without anterior support vs anterior support applying TLIF, and the extent of decompression (from no decompression performed, to laminectomy, unilateral and bilateral total facet joint resection). The parameters included in the general multivariate logistic regression model with highest explanatory value are shown in Table 3.
| Parameter | Regression coefficient | OR per unit change with 95%CI |
| Intercept | −4.819065; Р = 0.3617 | - |
| Radiodensity, HU | −0.0271586; P < 0.0001 | 0.9732 (0.9623-0.9842) |
| Number of fused levels | 1.111651; P < 0.0001 | 3.0394 (1.7566-5.2590) |
| Bilateral total facet joints removal (at least one level) | 1.124871; Р = 0.4359 | 3.0798 (1.0023-9.2781) |
| Laminectomy | 0.4418158; Р = 0.5333 | 1.5555 (0.5090-4.7533) |
| Posterior fusion performed without interbody fusion | −0.4247137; Р = 0.4550 | 0.6540 (0.2128-2.0097) |
| Maximal external screw diameter | −5.966555; Р = 0.3798 | 0.0026 (0.000009-0.7153) |
| Maximal internal screw diameter | 6.430714; P = 0.0253 | 620.61 (2.2363-172234.6) |
| Helical pitch | 4.611687; Р = 0.0081 | 100.6538 (3.3668-3009.1310) |
| Thread type (buttress vs V-shape) | −1.034237; Р = 0.9949 | 0.1070 (0.0090-1.2659) |
| Design cyl/cyl | 0.1446205; P = 0.8568 | 1.1566 (0.2378-5.6156) |
| Design cyl/con | −1.731799; Р = 0.2767 | 0.1769 (0.0077-4.0602) |
| Design con/con | 0.2718265; P = 0.7594 | 1.3124 (0.2282-7.5451) |
The most significant non-implant-related factors contributing to pedicle screw loosening were the number of fused levels and radiodensity. The rate of screw loosening correlated positively with the number of fused levels and decreasing bone density. Bilateral facet joint removal significantly contributed to pedicle screw loosening and the impact of laminectomy was not significant. Technical solutions with pedicle screw fixation and posterior fusion only vs cases supplemented with TLIF were not significantly associated with the loosening rate.
We found that screw parameters also strongly influenced the frequency of loosening. The rate of pedicle screw loosening decreased with increase in outer diameter and decrease in core diameter. A small helical pitch was associated with a decrease in the pedicle screw loosening rate. Neither thread type or screw design (con/con, cyl/con, cyl/cyl) had a significant influence on pedicle screw loosening. The overall goodness of fit of estimated general multivariate model was χ2 = 64.5554, P < 0.0001. The model correctly classified 78.86% of cases and had a 86.54% specificity and 67.61% sensitivity.
Among the few surgical means of achieving clinically significant results, pedicle screw fixation is associated with various implant-related complications, and one of the most frequently reported is pedicle screw loosening[3]. Along with degenerative diseases of the spine, osteoporosis is also a frequently encountered morbid condition in older-adult populations. Even though altered bone quality is not an absolute contraindication for spinal surgery with pedicle screw fixation, it may increase the risk of implant instability, with reported rates as high as 50%-60%[1,3]. One of the approaches intended provide maximal stability of pedicle screw fixation is an alteration of screw design including differences in geometry, type of thread and helical pitch, and in the ratio of internal to external diameter[5,8-10,18]. Despite a considerable amount of research published on this topic, the reported results remain controversial[5].
It has been shown in ex-vivo experiments that an increase in external diameter enhances the pullout strength of a screw although pedicle size and the risk of pedicle fracture limit application of this strategy[5,18-20]. By additionally increasing the depth of thread the interface of bone and screw can be considerably strengthened, however this effect can be achieved only if internal diameter is decreased[19]. The results of our study are in agreement with previously reported data and demonstrate that the rate of pedicle screw loosening declined with increase in outer diameter and decrease in core diameter. Surprisingly, helical pitch turned out to be a parameter that had a statistically significant influence on the pedicle screw loosening rate. According to the regression analysis results, a decrease of the helical pitch was associated with a decline in the pedicle screw loosening rate. The potential influence of helical pitch on bone and screw interface strength is still debated in the literature. In theory, pedicle screws with a small helical pitch provide a maximal contact area between the screw thread and bone[5,10,18,19]. On the other hand, it has been reported that pedicle screws with a small helical pitch sometimes have a decreased resistance to pullout forces[5,21]. The explanation for the observed discrepancies is that a smaller helical pitch results in an increase in coverage between bone and thread enhancing pullout strength only until the bone is damaged[5,21].
The potential influence of thread type and screw geometry is frequently discussed in the literature, but the results remain controversial to some extent. It has been reported that conical screws are superior to cylindrical screws because of additional compression of the surrounding bone[5,9,10]. Some studies have reported that pedicle screws with a cylindrical thread and conical core provided maximal pullout resistance[8]. Screws with a buttress thread might be expected to provide increased strength at the bone-screw interface because of its geometry, however pedicle screws with a V-shaped thread were found to have superior pullout strength in foams that mimic osteoporotic bone[8]. On the other hand, buttress and V-shaped threads had about the same pullout strength in foam that reproduced normal bone density[8]. The results of those studies demonstrate that the effect of different thread types might depend on bone quality. The results of our study demonstrate, that in a cohort of patients with having nonstandardized bone quality, the geometry of screw and thread type turned out to be insignificant factors.
A potential source of controversies related to screw design is the way screws are tested ex-vivo. Even though the most frequently used pullout test can be easily standardized and reproduced, it has limited relevance to screw loosening mechanisms in vivo because cases with pullout failure account for only 0%-1.3% of the causes[7]. The surgical technique may also interfere with the results of screw testing in clinical trials. It has been reported that multilevel fusion may favor pedicle loosening because of an increased load on the pedicle screws[1,3,14]. It has been clearly shown that excessive resection of ligaments, facet joints, and laminectomy are associated with the increased range of movements in a spinal segment[22,23]. Taking into account that the most reliable mechanisms of screw loosening were considered cyclic caudocephalad toggling and rotational stress causing micromovements between the vertebral body and screws, extensive decompression may favor screw loosening[16,24]. It has been reported that the lack of anterior support and even fusion type may also impact the stability of spinal instrumentation[3,25,26]. For those reasons, those factors were also taken into account to assess their relative contribution to pedicle screws loosening. Finally anterior support did not significantly influence the screws loosening rate in our study.
Measurements of bone density in HU was used in this study as a predictor because of growing evidence that those figures can be used to predict implant failure and pseudoarthrosis. Furthermore if a 120 kV tube is used, then HU values can be converted to mineral density[4,11,12,27,28]. The results of our study demonstrate that the radiodensity of vertebral body cancellous bone and the extensiveness of fixation were the most significant nonimplant-related contributing factors to pedicle screw loosening. The rate of screw loosening was positively correlated with the number of fused levels and with decreasing bone density, which is in agreement with previously reported data. The results of this analysis confirmed that total removal of bilateral facet joints slightly increased the pedicle screw loosening rate and that the impact of laminectomy was not significant. The influence of fusion by TLIF vs posterior fusion only on the pedicle screw loosening rate was not significant.
Finally the study results demonstrate the clinical relevance of previously reported biomechanical findings and provide additional evidence that screw parameters may have a considerable influence on the loosening rate. The significance of the contribution of screw parameters was comparable to that of patient- and surgery-related factors.
This study limitations include enrollment of a nonconsecutive patient cohort because individual patients with different screw types and sizes were excluded. The prevalence and significance of pseudoarthrosis was not studied because that aim would have required a different study design. Collinearity of some screw parameters may have influenced the results of the analysis. On the other hand, the study provides evidence sufficient to conclude that screw parameters strongly influenced the rate of pedicle screw loosening.
Screw parameters have a significant impact on pedicle screw loosening rate along with bone quality characteristics, the number of levels fused, and the extent of decompression. The significance of the impact of screw parameters was comparable to the influence of patient and surgery-related factors. The complication rate is influenced by helical pitch and inner and outer screw diameter. The impact of screw geometry and thread type was not significant.
Because of aging populations worldwide the number of spinal instrumentations performed annually is increasing dramatically. The most frequently encountered comorbidity in elderly adults is osteoporosis, which is a main reason for development of pedicle screw instability. Strategies to increase pedicle screw fixation stability include changes in pedicle screw design, but evaluations of pedicle screw loosening are controversial because of differences in the criteria used as indicators for implant loosening and heterogeneity of study groups.
It has be assumed that pedicle screw design influences the stability of the bone-screw interface and it has been extensively studied. The weak points of those studies is in the extrapolation of mechanical data and the results of pullout tests that to clinical practice. It is clear that pullout forces cause minority of cases of pedicle screw instability and that and bone characteristics influence the performance of screws. The strong point of our study is that the influence of screw parameters were tested.
The study aim was to test the impact of a screw design on loosening rate and to assess how screw parameters interfere with patient- and surgery-related factors.
This study was a prospective evaluation of 175 patients with degenerative bone diseases and instability of lumbar spine segments. Participants underwent spinal instrumentation employing pedicle screws with posterior only or transforaminal interbody fusion. Follow-up was for 18 mo. Patients with signs of pedicle screw loosening signs on CT were registered; logistic regression analysis was used to identify the factors associated with loosening, including screw parameters, bone characteristics, and surgery-related factors.
Parameters included in the analysis were screw geometry, thread type, external and internal screw diameter and helical pitch, bone density in HUs, the number of levels fused, instrumentation without anterior support, laminectomy, and unilateral and bilateral total facet joint resection. The rate of screw loosening decreased with an increase in outer diameter, decrease in core diameter, and helical pitch. The rate of screw loosening was positively correlated with the number of fused levels and with decreasing bone density. Bilateral facet joint removal significantly favored pedicle screw loosening. The influence of other factors was not significant. The overall contribution of screw design to loosening rate was comparable to that of patient and surgery-related factors.
Screw parameters had a significant impact on loosening rate along with bone quality characteristics, the number of levels fused, and the extent of decompression. The significance of the influence of screw parameters was comparable to that of patient- and surgery-related factors. The pedicle screw loosening rate was influenced by helical pitch, inner, and outer screw diameter. The influence of screw geometry and thread type was not significant.
We assume that the rational application of implants of various designs can result in a decrease in implant-related complications, but the design characteristics may interfere with patient- and surgery-related factors. To identify additional effects, including those of higher order, and to address the potential bias relevant to collinearity, a cohort study with enrollment of more patients is required. Multivariate analysis can help in the design of randomized case-control trials that can address potential sources of study bias.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berra LV, Li Y S-Editor: Zhang L L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Röllinghoff M, Schlüter-Brust K, Groos D, Sobottke R, Michael JW, Eysel P, Delank KS. Mid-range outcomes in 64 consecutive cases of multilevel fusion for degenerative diseases of the lumbar spine. Orthop Rev (Pavia). 2010;2:e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Wu ZX, Gong FT, Liu L, Ma ZS, Zhang Y, Zhao X, Yang M, Lei W, Sang HX. A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg. 2012;132:471-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24:1005-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 270] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 4. | Bredow J, Boese CK, Werner CM, Siewe J, Löhrer L, Zarghooni K, Eysel P, Scheyerer MJ. Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg. 2016;136:1063-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 137] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 5. | Shea TM, Laun J, Gonzalez-Blohm SA, Doulgeris JJ, Lee WE 3rd, Aghayev K, Vrionis FD. Designs and techniques that improve the pullout strength of pedicle screws in osteoporotic vertebrae: current status. Biomed Res Int. 2014;2014:748393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 6. | Bianco RJ, Arnoux PJ, Wagnac E, Mac-Thiong JM, Aubin CÉ. Minimizing Pedicle Screw Pullout Risks: A Detailed Biomechanical Analysis of Screw Design and Placement. Clin Spine Surg. 2017;30:E226-E232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Kueny RA, Kolb JP, Lehmann W, Püschel K, Morlock MM, Huber G. Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: pullout vs fatigue testing. Eur Spine J. 2014;23:2196-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 91] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Kim YY, Choi WS, Rhyu KW. Assessment of pedicle screw pullout strength based on various screw designs and bone densities-an ex vivo biomechanical study. Spine J. 2012;12:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Chao CK, Hsu CC, Wang JL, Lin J. Increasing bending strength and pullout strength in conical pedicle screws: biomechanical tests and finite element analyses. J Spinal Disord Tech. 2008;21:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Tsai WC, Chen PQ, Lu TW, Wu SS, Shih KS, Lin SC. Comparison and prediction of pullout strength of conical and cylindrical pedicle screws within synthetic bone. BMC Musculoskelet Disord. 2009;10:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93:1057-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 620] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 12. | Matsukawa K, Abe Y, Yanai Y, Yato Y. Regional Hounsfield unit measurement of screw trajectory for predicting pedicle screw fixation using cortical bone trajectory: a retrospective cohort study. Acta Neurochir (Wien). 2018;160:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Matsukawa K, Yato Y, Hynes RA, Imabayashi H, Hosogane N, Yoshihara Y, Asazuma T, Nemoto K. Comparison of Pedicle Screw Fixation Strength Among Different Transpedicular Trajectories: A Finite Element Study. Clin Spine Surg. 2017;30:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Kim JB, Park SW, Lee YS, Nam TK, Park YS, Kim YB. The Effects of Spinopelvic Parameters and Paraspinal Muscle Degeneration on S1 Screw Loosening. J Korean Neurosurg Soc. 2015;58:357-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 15. | Varghese V, Saravana Kumar G, Krishnan V. Effect of various factors on pull out strength of pedicle screw in normal and osteoporotic cancellous bone models. Med Eng Phys. 2017;40:28-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 16. | Mizuno T, Kasai Y, Sakakibara T, Yoshikawa T, Inaba T. Biomechanical study of rotational micromovement of the pedicle screw. Springerplus. 2016;5:1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 2007;245:62-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 193] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Biswas JK, Sahu TP, Rana M, RoyS, Karmakar SK, Majumder S, Roychowdhury A. Design factors of lumbar pedicle screws under bending load: A finite element analysis. Biocybern Biomed Eng. 2019;39:52-62. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Cho W, Cho SK, Wu C. The biomechanics of pedicle screw-based instrumentation. J Bone Joint Surg Br. 2010;92:1061-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 159] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 20. | Hirano T, Hasegawa K, Washio T, Hara T, Takahashi H. Fracture risk during pedicle screw insertion in osteoporotic spine. J Spinal Disord. 1998;11:493-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Krenn MH, Piotrowski WP, Penzkofer R, Augat P. Influence of thread design on pedicle screw fixation. Laboratory investigation. J Neurosurg Spine. 2008;9:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 22. | Bisschop A, van Engelen SJ, Kingma I, Holewijn RM, Stadhouder A, van der Veen AJ, van Dieën JH, van Royen BJ. Single level lumbar laminectomy alters segmental biomechanical behavior without affecting adjacent segments. Clin Biomech (Bristol, Avon). 2014;29:912-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Lee KK, Teo EC. Effects of laminectomy and facetectomy on the stability of the lumbar motion segment. Med Eng Phys. 2004;26:183-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Pearson HB, Dobbs CJ, Grantham E, Niebur GL, Chappuis JL, Boerckel JD. Intraoperative biomechanics of lumbar pedicle screw loosening following successful arthrodesis. J Orthop Res. 2017;35:2673-2681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Niemeyer TK, Koriller M, Claes L, Kettler A, Werner K, Wilke HJ. In vitro study of biomechanical behavior of anterior and transforaminal lumbar interbody instrumentation techniques. Neurosurgery. 2006;59:1271-6; discussion 1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Peck JH, Kavlock KD, Showalter BL, Ferrell BM, Peck DG, Dmitriev AE. Mechanical performance of lumbar intervertebral body fusion devices: An analysis of data submitted to the Food and Drug Administration. J Biomech. 2018;78:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Schwaiger BJ, Gersing AS, Baum T, Noël PB, Zimmer C, Bauer JS. Bone mineral density values derived from routine lumbar spine multidetector row CT predict osteoporotic vertebral fractures and screw loosening. AJNR Am J Neuroradiol. 2014;35:1628-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 28. | Zaidi Q, Danisa OA, Cheng W. Measurement Techniques and Utility of Hounsfield Unit Values for Assessment of Bone Quality Prior to Spinal Instrumentation: A Review of Current Literature. Spine (Phila Pa 1976). 2019;44:E239-E244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 132] [Article Influence: 22.0] [Reference Citation Analysis (0)] |