Published online Mar 18, 2021. doi: 10.5312/wjo.v12.i3.129
Peer-review started: December 21, 2020
First decision: January 7, 2021
Revised: January 7, 2021
Accepted: January 28, 2021
Article in press: January 28, 2021
Published online: March 18, 2021
Processing time: 80 Days and 12 Hours
Malleolar ankle fractures have been classified using plain radiographs, and there is no consensus regarding the role of computed tomography (CT) scans in preoperative planning. We analyzed critical aspects, such as limits of standard radiographs, types of injury, classification methods and cost/benefit evaluations. CT scans allow a 3D analysis of the fracture to be obtained and consequently assess the indication for surgical procedure, surgical access and the type of fixation devices required. This exam is useful for detecting lesions that may go unnoticed on radiographs and will help surgeons to clarify the pathoanatomy of ankle fractures. According to Arbeitsgemeinschaft fur Osteosynthesefragen/ Orthopaedic Trauma Association (AO/OTA) classification, CT scan is recommended in medial malleolar fractures with vertical rim, type 44B fractures with posterior malleolar involvement and all type 44C fractures (according to AO/OTA). Also Tillaux-Chaput fractures (43-B1 according to AO/OTA), malleolar fractures in the presence of distal tibial fractures (43 according to AO/OTA) and distal tibia fractures in adolescents should be studied with CT scans.
Core Tip: Computed tomography scan is recommended in medial malleolar fractures with vertical rim, type 44B fractures [according to Arbeitsgemeinschaft fur Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification] with posterior malleolar involvement. All type 44C fractures (according to AO/OTA), Tillaux-Chaput fractures (43-B1 according to AO/OTA), malleolar fractures in the presence of distal tibial fractures (43 according to AO/OTA) and distal tibia fractures in adolescents should be studied with computed tomography scans.
- Citation: Tarallo L, Micheloni GM, Mazzi M, Rebeccato A, Novi M, Catani F. Advantages of preoperative planning using computed tomography scan for treatment of malleolar ankle fractures. World J Orthop 2021; 12(3): 129-139
- URL: https://www.wjgnet.com/2218-5836/full/v12/i3/129.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i3.129
Ankle fractures represent 10.2% of all fractures[1] and are the most common fractures of the lower extremity after proximal femur fractures[2]. The incidence number is approximately 1000 out of 1000000 people per year[3] with higher rates reported in the European literature[3,4]. Single malleolar fractures are the most frequent followed by bimalleolar fractures (25% of ankle fractures) and trimalleolar fractures (5%-10%)[5].
Isolated posterior malleolar fractures are rare[6] because they are usually associated with other bone or ligament injuries[7]. Ankle syndesmosis injury occurs in 10%-13% of cases, and 20% of cases require surgical treatment[8,9]. Malleolar fractures, in some cases, are associated with tibial pilon injuries[10-13].
The Arbeitsgemeinschaft fur Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) fracture and dislocation classification is one of the most used classifications. Malleolar segments are categorized as 44 and are based on the direction of the fracture lines and of the fracture degree of comminution (A-C)[14]. This classification is based on standard plain radiographs, although often this diagnostic assessment can underestimate the nature, extent and severity of the injury because of the complex three-dimensional anatomy of the joint[15].
Compute tomography (CT) scan is used in some cases in order to obtain a 3D analysis of the fracture and to consequently assess the indication for the surgical procedure, surgical access and type of fixation devices required. The anatomical reduction of fractures demonstrated higher functionality and improved long-term outcomes[16].
However, approximately one-third of patients aged 10-21 years with bimalleolar and trimalleolar fractures presented clinical signs of post-traumatic arthritis, and more than 97% showed pathological radiological findings[17-19]. Possible causes are due to minor inconsistencies, axial malalignment and syndesmosis instability. This study aims to identify the cases in which a CT scan is recommended in order to avoid or reduce the risk of long-term complications.
Radiological assessment, usually performed in the emergency room, presents noncanonical projections because of patient pain or the presence of immobilization devices[2,16]. Furthermore, it is subject to the variable accuracy of the action and the scarce penetration of the radiations. Therefore, it is difficult to determine if the diagnostic assessment is adequate to perform a surgical fixation procedure with satisfying results. CT scan study does not replace an adequate plain radiograph study. Instead, it can provide precious information regarding the assessment of the fracture lines pattern and the number of fragments.
CT is fundamental to determine if surgical treatment is required due to the increase of the energy of the injury, which consequently increases the possibility of associated dislocations as well as complex injuries secondary to rotation flexion. Kumar et al[16] reported that in ankle fracture cases the increase of malleolar involvement and the increase of the severity of the injury led to a different type of treatment strategy (that is surgical procedure) after CT scan study was performed. Hence, the presence of occult fractures and complex fracture lines is more likely in such injuries. The severity of the fracture is predictive of the increased risk of intra-articular abnormality[20,21], and in such cases preoperative CT scan assessment could identify additional lesions and mobile bodies requiring surgical treatment. The global change of the management plan rate was 23.2%, which was comparable with another retrospective study[2].
The most used classifications in the literature are AO/OTA, Weber or Lauge-Hansen classifications and are all based on standard plain radiographs. Clinical studies report that such classifications are not correlated with the fracture mechanism[22,23] and are not predictive of the sequence of bone and ligament injuries like CT, magnetic resonance imaging and surgical exploration are[24,25].
Currently, CT scan studies represent the standard of care for all lower extremity joint fractures, especially acetabular fractures[26], femoral head fractures[27], distal femur fractures[28], tibial plateau fractures[29], tibial pilon fractures[30], talar fractures[31], calcaneal fractures[32], metatarsal fractures[33] and tarsometatarsal fractures[34]. Therefore, the CT scan study is by definition higher and larger than radiological analysis, although it is not assumed that it is required in all types of malleolar fractures[2].
CT requires higher costs, timing and exposure to radiation. Medical facilities are unfortunately more sensitive to cost and timing containment due to the constant increase of the demand for services; for this reason, it is essential to determine when a CT scan assessment is required. Radiation exposure is a sensitive aspect, particularly in pediatric patients. It was reported that the actual dose of an ankle CT scan study (0.07 mSv) was low and equivalent to a plain radiograph with anterior-posterior planes of the chest[35]. This value is ten times lower than the required dose of a CT scan study of the chest, abdomen and pelvis. It could be further reduced by limiting the exposed body segment or using a cone-beam CT scan and other protocols without the risk of losing essential information[36-38].
The advantages of using CT in the preoperative planning of malleolar fractures are: more accurate planning to determine the conservative/surgical approach and the type of fixation device required (and this is the major advantage because of the long-term results in spite of the surgical treatment[17-19]); the identification of unknown lesions in order to obtain a more accurate prognosis, including the detection of tibial pilon fractures; and more diffuse use of CT in the preoperative planning could clarify some unresolved biomechanical aspects regarding the relationship between the mechanism of injury and the pattern of fracture.
The most used classification, among the studies regarding the use of CT in the preoperative planning is the Danis Weber–AO classification, limited only to the three main categories: infrasyndesmotic (44-A according to AO/OTA classification), transsyndesmotic (44-B according to AO/OTA classification) and suprasyndesmotic (44-C according to AO/OTA classification). However, there is no absolute consensus among the authors[2,16,39]. This classification is attractive for clinicians because it is simple. The disadvantage of this system is that it does not incorporate a staging system to allow the degree of injuries falling only under one heading in terms of severity[40].
In our opinion this system is extremely simple and does not allow the differentiation of significant varieties within each group. Therefore, we reassessed the published system in order to determine a more detailed algorithm specifically referring to the Danis Weber subclassifications.
In our revision of the literature, the Lauge-Hansen classification was useful and significant in the evaluation of the importance of CT in the preoperative planning[7,41]. The classification is based on the rise of the mechanic forces, and there is a direct correlation between the increase of the energy of the injury and the usefulness of the preoperative CT study[2].
Isolated lateral malleolar fractures [type 44-A1; Lauge-Hansen supination adduction (SA) stage I] and isolated medial malleolar fractures (type 44-A2.1/2; Lauge-Hansen SA stage II) are largely caused by injuries with no associated lesions. The use of CT is not recommended in this type of case. In a retrospective study[2] of 100 patients, no significant changes were noted regarding the treatment option (only 1 patient out of 24 cases of infrasyndesmotic fractures) following a CT scan study compared to the plain radiograph analysis[2].
The vertical medial malleolar fracture (Lauge-Hansen SA stage II) represents a particular condition because a medial tibial pilon injury can occur in the case of persistent energy of injury in adduction[11,42]. This type of lesion was described in 61% of SA stage II in the retrospective study conducted on 120 patients by Alluri et al[43]. In such cases, CT is recommended because the ideal treatment should provide the specific approach with elevation and bone grafting to significantly improve the prognosis[44]. In our opinion, the angulation of the line of fracture increases or decreases the suspected rate of tibial pilon injuries.
The above described subjects regarding the study of medial malleolus can be applied to bimalleolar fractures type 44-A2.3 (Lauge-Hansen stage II). In fracture type 44-A3 with a medial malleolus involvement associated with part of the posterior malleolus, a CT scan study is always recommended.
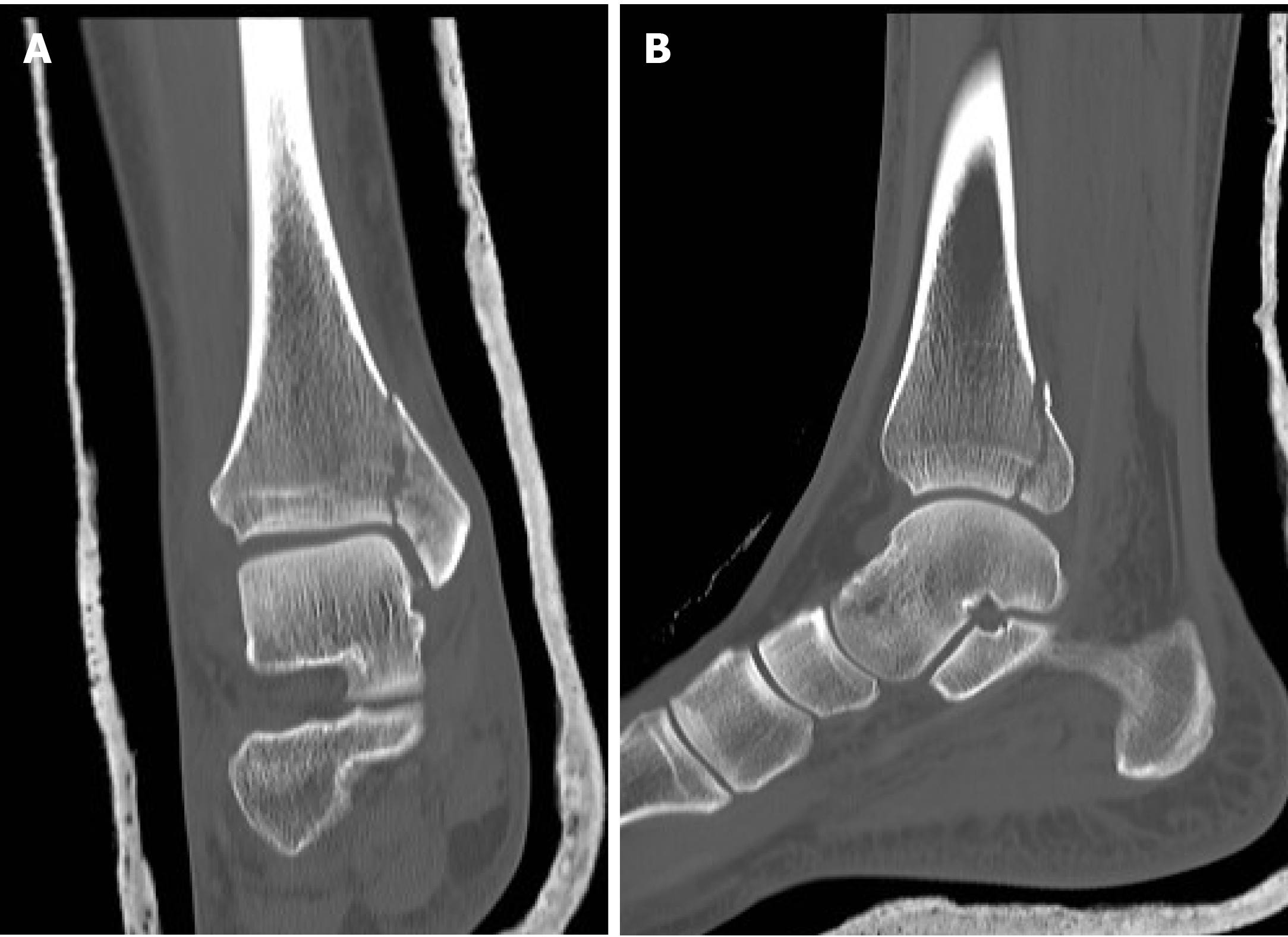
The importance of the preoperative CT scan study in the case of posterior malleolus fractures is documented by numerous publications in the literature. In fact, classifications based on CT scan studies have been proposed[13,45,46]. CT images allow the identification of impacted fracture fragments not visualized with conventional plain radiographs and with possible changes to the preoperative planning.
Black et al[2] and Magid et al[47] demonstrated that the use of CT scan study varies between 24.0% and 38.7% of the treatment planning compared to simple plain radiographs in cases of trimalleolar fracture[2,47]. Donohoe et al[48] and Palmanovich et al[49] reported that CT scan images increased the diagnostic accuracy and the intraobserver and interobserver agreement compared to conventional radiographs[48,49]. Furthermore, Evers et al[50] showed that in 25.1% of cases (430/1710), the planning was revised after CT scan study was performed with an increase of surgical indications and fixation device technique[50].
In transsyndesmotic fractures of isolated fibular fractures (type 44-B1 and B2) or bimalleolar fractures, the preoperative CT scan study does not significantly change the surgical treatment option[11,51]. This could be related to the fact that the standard radiographs are sufficient to adequately detect this type of fracture.
This assumption cannot be applied to transsyndesmotic fracture of posterior malleolar fracture (type 44-B3). In this case the study of posterior malleolus, as in fractures type 44-A3, cannot be based only on plain radiographs (Figures 1-3).
In suprasyndesmotic fractures, despite the degree of fracture (C1, C2, C3 Lauge-Hansen PER stage 1-4), CT is always recommended. This study allows the evaluation of the syndesmosis and the possible involvement of the Tillaux-Chaput fragment[52,53]. Plain radiographs are not sufficient for syndesmosis evaluation because of the extreme variability among the individuals[54,55], whereas axial CT scan images allow a correct diagnosis as well as a determination of the best direction of the transsyndesmotic screw placement.
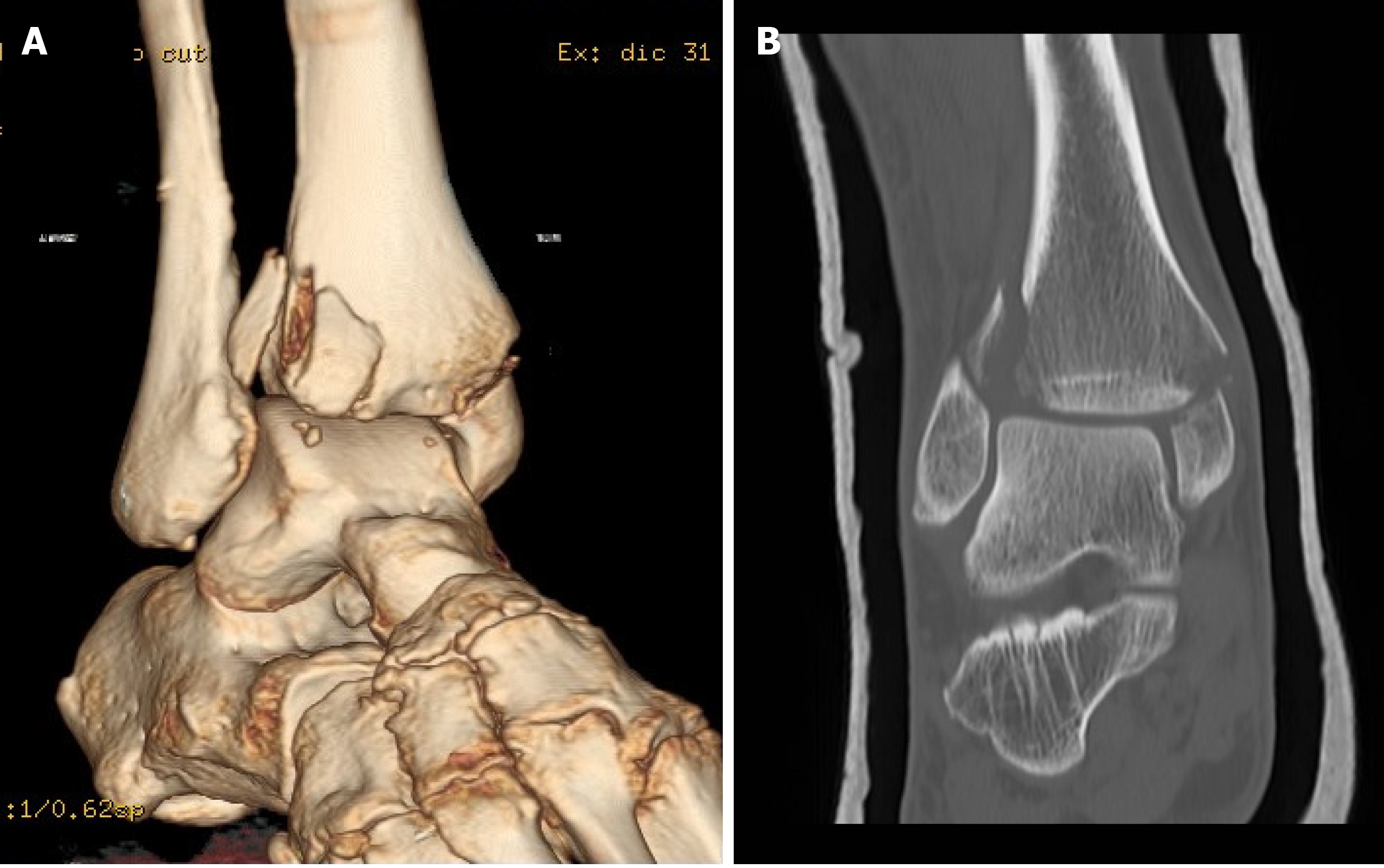
Conventional plain radiographs did not detect the Tillaux-Chaput fragment, which is more frequently present in fractures type B and C according to AO/OTA classification, in the studies conducted by Black et al[2] and Kumar et al[16]. This suggests an absolute advantage of the use of CT in fractures involving the anterior tibial tubercle[44] or in suspected cases considering the above-mentioned posterior malleolus fractures. The fixation of the anterolateral fragments re-establishes the anterior incisure and provides the stability of the anterior syndesmosis[56] (Figures 4 and 5).
The presence of occult fractures of the medial malleolus in fractures of the distal shaft of the tibia are described by some authors[57-60]. In the study by Jung et al[57], 89% of patients with distal tibia spiral fracture (type 43 according to AO/OTA) associated with malleolar fracture underwent surgical fixation. The importance of the preoperative identification derives from the risk of intraoperative decomposition during a surgical procedure of nailing with a consequent increase of surgical difficulties and duration of surgical treatment.
CT is additionally recommended in distal fracture of the leg because the line of fracture (even closed fracture) involves the epiphyseal/malleolar regions.
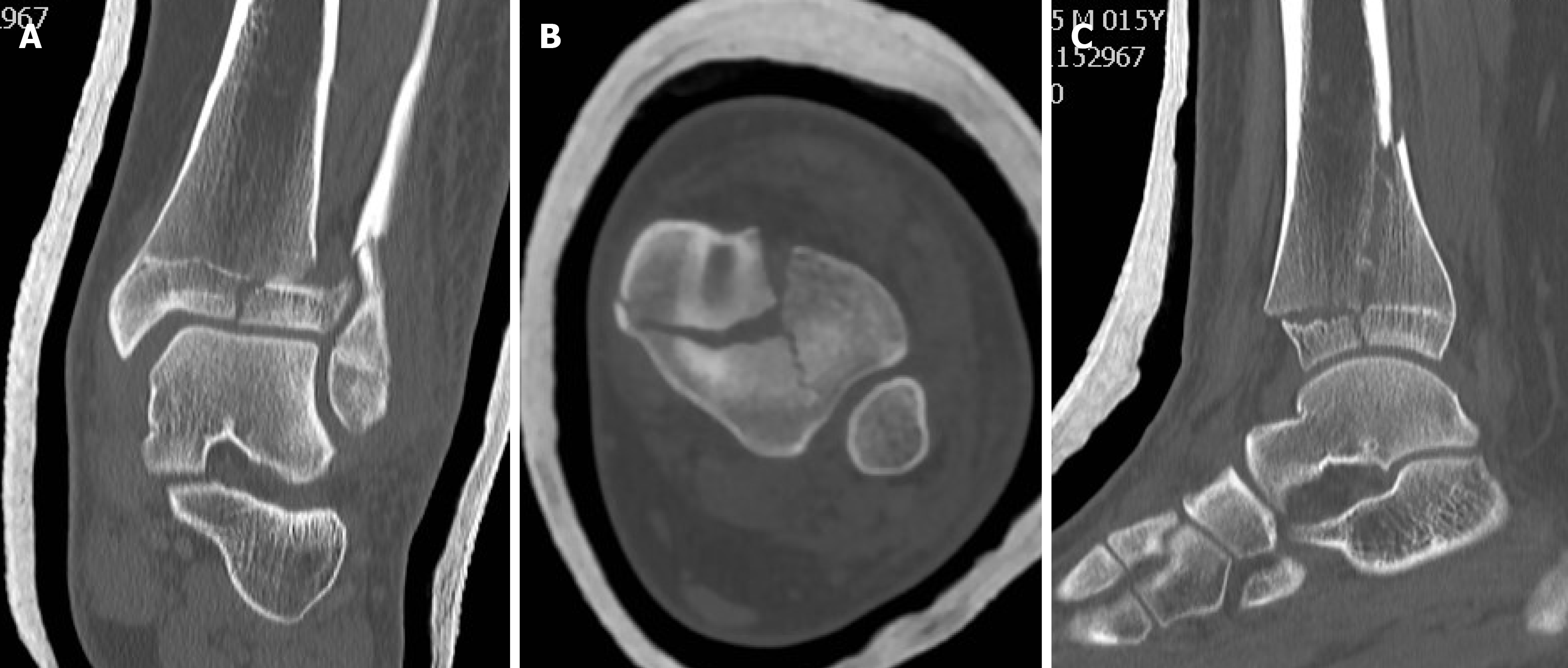
The preoperative CT scan study represents the gold standard in malleolar ankle fractures in adolescents. Plain radiographs tend to underestimate this type of fracture. It is noted that consolidating fractures of the distal tibia present some features because the ossification of the growing cartilage is medial-lateral and posterolateral. This implies extraordinarily complex patterns of fractures (i.e. triplane fractures) and only with axial, sagittal and coronal planes is it possible to obtain adequate treatment planning[11,61] (Figures 6-8).
The aim of malleolar fracture treatment is the anatomical reduction of the articular surfaces and of the syndesmosis. The use of CT in the preoperative planning could improve the clinical outcomes and reduce the risk of intraoperative difficulty and surgical duration in vertical medial malleolar fractures, in fractures type 44B with posterior malleolus involvement and in fractures type 44C. A CT scan study is mandatory in cases of Tillaux-Chaput fracture, malleolar fractures associated with the distal third of the leg and in adolescent patients. Additional large-scale clinical studies with cost/benefit analysis are required to confirm this hypothesis.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zaman MU S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
| 1. | Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018;42:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 124] [Article Influence: 15.5] [Reference Citation Analysis (1)] |
| 2. | Black EM, Antoci V, Lee JT, Weaver MJ, Johnson AH, Susarla SM, Kwon JY. Role of preoperative computed tomography scans in operative planning for malleolar ankle fractures. Foot Ankle Int. 2013;34:697-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1916] [Cited by in RCA: 2176] [Article Influence: 114.5] [Reference Citation Analysis (0)] |
| 4. | Jensen SL, Andresen BK, Mencke S, Nielsen PT. Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. Acta Orthop Scand. 1998;69:48-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 199] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Driesman AS, Egol KA. An update on the treatment of malleolar fractures. Fuss Sprungg. 2016;14:55-65. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Comat G, Barbier O, Ollat D. The posterior malleolar fracture: a parachute injury not to be overlooked. Orthop Traumatol Surg Res. 2014;100:419-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Vosoughi AR, Jayatilaka MLT, Fischer B, Molloy AP, Mason LW. CT Analysis of the Posteromedial Fragment of the Posterior Malleolar Fracture. Foot Ankle Int. 2019;40:648-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Ntalos D, Rupprecht M, Grossterlinden LG, Hamurcu A, Regier M, Klatte TO, Rueger JM, Spiro AS. Incidence and severity of malreduction of the tibiofibular syndesmosis following surgical treatement of displaced ankle fractures and impact on the function -Clinical study and MRI evaluation. Injury. 2018;49:1220-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Andersen MR, Frihagen F, Hellund JC, Madsen JE, Figved W. Randomized Trial Comparing Suture Button with Single Syndesmotic Screw for Syndesmosis Injury. J Bone Joint Surg Am. 2018;100:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 10. | Weber M. Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int. 2004;25:716-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Rammelt S, Zwipp H. Ankle fractures. In: Bentley G. European instructional lectures. Berlin: Springer; 2012: 205-219. [DOI] [Full Text] |
| 12. | Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. 2013;34:189-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg. 2015;135:505-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 177] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 14. | Fonseca LLD, Nunes IG, Nogueira RR, Martins GEV, Mesencio AC, Kobata SI. Reproducibility of the Lauge-Hansen, Danis-Weber, and AO classifications for ankle fractures. Rev Bras Ortop. 2018;53:101-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 15. | Carrozzo M, Vicenti G, Pesce V, Solarino G, Rifino F, Spinarelli A, Campagna C, Bizzoca D, Moretti B. Beyond the pillars of the ankle: A prospective randomized CT analysis of syndesmosis' injuries in Weber B and C type fractures. Injury. 2018;49 Suppl 3:S54-S60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Kumar A, Mishra P, Tandon A, Arora R, Chadha M. Effect of CT on Management Plan in Malleolar Ankle Fractures. Foot Ankle Int. 2018;39:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Bagger J, Hølmer P, Nielsen KF. The prognostic importance of primary dislocated ankle joint in patients with malleolar fractures. Acta Orthop Belg. 1993;59:181-183. [PubMed] |
| 18. | Donken CC, Verhofstad MH, Edwards MJ, van Laarhoven CJ. Twenty-one-year follow-up of supination-external rotation type II-IV (OTA type B) ankle fractures: a retrospective cohort study. J Orthop Trauma. 2012;26:e108-e114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Day GA, Swanson CE, Hulcombe BG. Operative treatment of ankle fractures: a minimum ten-year follow-up. Foot Ankle Int. 2001;22:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 93] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 143] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 21. | Loren GJ, Ferkel RD. Arthroscopic assessment of occult intra-articular injury in acute ankle fractures. Arthroscopy. 2002;18:412-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 110] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Rodriguez EK, Kwon JY, Herder LM, Appleton PT. Correlation of AO and Lauge-Hansen classification systems for ankle fractures to the mechanism of injury. Foot Ankle Int. 2013;34:1516-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Boszczyk A, Fudalej M, Kwapisz S, Klimek U, Maksymowicz M, Kordasiewicz B, Rammelt S. Ankle fracture - Correlation of Lauge-Hansen classification and patient reported fracture mechanism. Forensic Sci Int. 2018;282:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Nielsen JO, Dons-Jensen H, Sørensen HT. Lauge-Hansen classification of malleolar fractures. An assessment of the reproducibility in 118 cases. Acta Orthop Scand. 1990;61:385-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: an MRI study. J Orthop Trauma. 2006;20:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Scheinfeld MH, Dym AA, Spektor M, Avery LL, Dym RJ, Amanatullah DF. Acetabular fractures: what radiologists should know and how 3D CT can aid classification. Radiographics. 2015;35:555-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 27. | Collinge CA, Mir H, Reddix R. Fracture morphology of high shear angle "vertical" femoral neck fractures in young adult patients. J Orthop Trauma. 2014;28:270-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 28. | Xie X, Zhan Y, Dong M, He Q, Lucas JF, Zhang Y, Wang Y, Luo C. Two and Three-Dimensional CT Mapping of Hoffa Fractures. J Bone Joint Surg Am. 2017;99:1866-1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 29. | Millán-Billi A, Gómez-Masdeu M, Ramírez-Bermejo E, Ibañez M, Gelber PE. What is the most reproducible classification system to assess tibial plateau fractures? Int Orthop. 2017;41:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. J Orthop Trauma. 2013;27:e152-e156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 144] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 31. | Rammelt S, Zwipp H. Talar neck and body fractures. Injury. 2009;40:120-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 32. | Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: long-term (10-20 Years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma. 2014;28:551-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 134] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 33. | Rammelt S, Schepers T. Chopart Injuries: When to Fix and When to Fuse? Foot Ankle Clin. 2017;22:163-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 34. | Preidler KW, Peicha G, Lajtai G, Seibert FJ, Fock C, Szolar DM, Raith H. Conventional radiography, CT, and MR imaging in patients with hyperflexion injuries of the foot: diagnostic accuracy in the detection of bony and ligamentous changes. AJR Am J Roentgenol. 1999;173:1673-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91:1882-1889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 338] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 36. | Yi JW, Park HJ, Lee SY, Rho MH, Hong HP, Choi YJ, Kim MS. Radiation dose reduction in multidetector CT in fracture evaluation. Br J Radiol. 2017;90:20170240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 37. | Konda SR, Goch AM, Haglin J, Egol KA. Ultralow-Dose CT (REDUCTION Protocol) for Extremity Fracture Evaluation Is as Safe and Effective as Conventional CT: An Evaluation of Quality Outcomes. J Orthop Trauma. 2018;32:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Pugmire BS, Shailam R, Sagar P, Liu B, Li X, Palmer WE, Huang AJ. Initial Clinical Experience With Extremity Cone-Beam CT of the Foot and Ankle in Pediatric Patients. AJR Am J Roentgenol. 2016;206:431-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 39. | Leung KH, Fang CX, Lau TW, Leung FK. Preoperative radiography vs computed tomography for surgical planning for ankle fractures. J Orthop Surg (Hong Kong). 2016;24:158-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | Harper MC. Ankle fracture classification systems: a case for integration of the Lauge-Hansen and AO-Danis-Weber schemes. Foot Ankle. 1992;13:404-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Palmanovich E, Ohana N, Yaacobi E, Segal D, Iftach H, Sharfman ZT, Vidra M, Atzmon R. Preoperative planning and surgical technique for optimizing internal fixation of posterior malleolar fractures: CT vs standard radiographs. J Orthop Surg Res. 2020;15:119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Weber BG. Die Verletzungen des oberen Sprunggelenkes. Aktuelle Probl Chir. 1973;50:1898-1902. [DOI] [Full Text] |
| 43. | Alluri RK, Hill JR, Donohoe S, Fleming M, Tan E, Marecek G. Radiographic Detection of Marginal Impaction in Supination-Adduction Ankle Fractures. Foot Ankle Int. 2017;38:1005-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Rammelt S, Boszczyk A. Computed Tomography in the Diagnosis and Treatment of Ankle Fractures: A Critical Analysis Review. JBJS Rev. 2018;6:e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 45. | Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88:1085-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 191] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 46. | Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle. Foot Ankle Int. 2017;38:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 47. | Magid D, Michelson JD, Ney DR, Fishman EK. Adult ankle fractures: comparison of plain films and interactive two- and three-dimensional CT scans. AJR Am J Roentgenol. 1990;154:1017-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 58] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 48. | Donohoe S, Alluri RK, Hill JR, Fleming M, Tan E, Marecek G. Impact of Computed Tomography on Operative Planning for Ankle Fractures Involving the Posterior Malleolus. Foot Ankle Int. 2017;38:1337-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 49. | Palmanovich E, Brin YS, Laver L, Kish B, Nyska M, Hetsroni I. The effect of minimally displaced posterior malleolar fractures on decision making in minimally displaced lateral malleolus fractures. Int Orthop. 2014;38:1051-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 50. | Evers J, Barz L, Wähnert D, Grüneweller N, Raschke MJ, Ochman S. Size matters: The influence of the posterior fragment on patient outcomes in trimalleolar ankle fractures. Injury. 2015;46 Suppl 4:S109-S113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 51. | Egol KA, Koval KJ, Zuckerman JD. Handbook of fractures. PA: Lippincott Williams & Wilkins; 2010. |
| 52. | Ebraheim NA, Lu J, Yang H, Rollins J. The fibular incisure of the tibia on CT scan: a cadaver study. Foot Ankle Int. 1998;19:318-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 53. | Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 365] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 54. | Cherney SM, Spraggs-Hughes AG, McAndrew CM, Ricci WM, Gardner MJ. Incisura Morphology as a Risk Factor for Syndesmotic Malreduction. Foot Ankle Int. 2016;37:748-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 55. | Boszczyk A, Kwapisz S, Krümmel M, Grass R, Rammelt S. Correlation of Incisura Anatomy With Syndesmotic Malreduction. Foot Ankle Int. 2018;39:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 56. | Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. 2015;41:601-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 57. | Jung KJ, Chung CY, Park MS, Chung MK, Lee DY, Koo S, Lee KM. Concomitant Ankle Injuries Associated With Tibial Shaft Fractures. Foot Ankle Int. 2015;36:1209-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 58. | Purnell GJ, Glass ER, Altman DT, Sciulli RL, Muffly MT, Altman GT. Results of a computed tomography protocol evaluating distal third tibial shaft fractures to assess noncontiguous malleolar fractures. J Trauma. 2011;71:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 59. | Boraiah S, Gardner MJ, Helfet DL, Lorich DG. High association of posterior malleolus fractures with spiral distal tibial fractures. Clin Orthop Relat Res. 2008;466:1692-1698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 60. | Hou Z, Zhang Q, Zhang Y, Li S, Pan J, Wu H. A occult and regular combination injury: the posterior malleolar fracture associated with spiral tibial shaft fracture. J Trauma. 2009;66:1385-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 61. | Schneidmueller D, Sander AL, Wertenbroek M, Wutzler S, Kraus R, Marzi I, Laurer H. Triplane fractures: do we need cross-sectional imaging? Eur J Trauma Emerg Surg. 2014;40:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |