Published online Feb 18, 2021. doi: 10.5312/wjo.v12.i2.69
Peer-review started: September 16, 2020
First decision: December 1, 2020
Revised: December 14, 2020
Accepted: January 21, 2021
Article in press: January 21, 2021
Published online: February 18, 2021
Processing time: 140 Days and 4.1 Hours
A fracture of the acetabulum is an uncommon, but serious injury. Established outcome tools do not reflect the patient’s perspective after fracture of the hip joint. Originally designed for post-arthroplasty patients, the Forgotten Joint Score (FJS) is a patient-reported outcome measurement (PROM) tool evaluating the disease-specific health-related quality of life (HR-QoL).
To validate the FJS in patients after acetabular fracture.
In a prospective mono-centric cohort study, we evaluated 100 patients at mean 5.2 ± 3.6 years after a fracture of the acetabulum. The validation study followed the complete COSMIN checklist protocol. For calculation of convergent validity, we used the Tegner-Activity Scale, the Western Ontario and McMaster Universities Osteoarthritis Index, the EuroQol-5D, and a subjective rating of change as an anchor variable.
We confirmed good internal consistency with a Cronbach‘s alpha of 0.95. With an intraclass correlation coefficient of 0.99 (95%CI: 0.97, 0.99), test-retest reliability of the FJS was excellent. Correlation coefficients between the questionnaires were moderate to high ranging from |0.56| to |0.83| (absolute value). No relevant floor or ceiling effects occurred. Standard error of measurement was 3.2 and smallest detectable change (SDC) was 8.8. Thus, changes greater than 8.8 points between two assessments denote a real change in FJS.
The FJS is a valid and reliable tool for evaluation of patient-reported outcome in posttraumatic condition after acetabular fracture. The SDC indicating a real clinical improvement was 8.8 points in the FJS. We could confirm responsiveness of the FJS and found no relevant floor- or ceiling effects.
Core Tip: A fracture of the acetabulum is a rare but serious medical condition. Patient-reported outcome measurement has rising impact on clinical decision-making and is of extraordinary value in research. Validation of measurement tools is an essential scientific contribution for further research. This study evaluates psychometric properties of the Forgotten Joint Score in posttraumatic condition after acetabular fractures.
- Citation: Freigang V, Weber J, Mueller K, Pfeifer C, Worlicek M, Alt V, Baumann FM. Evaluation of joint awareness after acetabular fracture: Validation of the Forgotten Joint Score according to the COSMIN checklist protocol. World J Orthop 2021; 12(2): 69-81
- URL: https://www.wjgnet.com/2218-5836/full/v12/i2/69.htm
- DOI: https://dx.doi.org/10.5312/wjo.v12.i2.69
A fracture of the acetabulum is an uncommon but severe injury to the hip joint. Initial management of these injuries is crucial regarding long-term outcome[1-7]. Persistent immobilizing pain and post-traumatic osteoarthritis are typical consequences in cases where the integrity of the acetabulum is not adequately reconstructed. Open reduction and internal fixation (ORIF) is the standard treatment for displaced acetabular fractures. Risk factors for a poor radiographic outcome like residual articular surface gaps and steps as well as involvement of the posterior wall and the quadrilateral surface are well known[2,4,8,9]. However, the impact of these radiographic parameters on Patient-reported outcome (PRO) is unclear. Conventional scoring systems like the Merle d’Aubigne-Postel Score are rather surgeon-based neglecting the patient’s perception of the outcome[10].
The “Forgotten Joint Score” (FJS) was developed in 2012 as a PRO measurement tool in patients after arthroplasty of the knee or hip joint[11]. The concept that the patient rates the loss of awareness of the hip joint is revolutionary in patient-reported outcome measurement (PROM). Joint awareness in everyday life is seen as an important criterion in activity of daily living (ADL)[11-13]. The forgotten joint, a condition where the patient has no distracting sensation of the joint, is seen as the ultimate goal resulting in maximum patient satisfaction[11]. Currently, the Merle d’Aubigne-Postel Score and the Western Ontario and McMaster Universities Osteoarthritis Index-Visual Analog Scale (WOMAC-VAS) Score are most frequently used in functional outcome evaluation after acetabular fractures[2,4,8,9,14]. Other scales like the EuroQol-5D (EQ-5D-3L) and the Tegner Activity Scale (TAS) are tools to rate global health-related quality of life and sports activity for characterization of a patient population.
Studies on psychometric properties of outcome tools should meet highest standards regarding methodological quality[15]. The COSMIN checklist is based on an international Delphi study in 2010 reporting on a consensus-based checklist evaluating the quality of studies on psychometric properties of HR-QoL instruments[16]. The COSMIN checklist consists of ten items giving recommen-dations for design, conduction and interpretation of medical validation studies. Relevant characteristics are study design, content validity, structural validity, internal consistency, cross-cultural validity/measurement invariance, reliability, measurement error, criterion validity, hypotheses testing for construct validity, and responsiveness.
Purpose of this study was to validate the FJS for mid- and long-term condition after acetabular fractures and to investigate the relation between perioperative parameters and score values of the FJS.
The ethics committee at the University of Regensburg approved this study in December 2015 (Institutional Review Board Number 15-101-0241). We obtained written informed consent from all study participants. The study was carried out in accordance with the Declaration of Helsinki.
In this prospective, mono-centric validating study, we identified 100 consecutive German-speaking patients with a history of an acetabular fracture between 07/2002 and 06/2016.
Inclusion criteria were: (1) Mid- and long-term condition after acetabular fracture; (2) Minimum follow up was 12 mo after trauma; (3) Age between 18 and 70 years; and (4) Sufficient German reading and comprehension capacity.
Exclusion criteria were: (1) Relevant concomitant injuries (e.g., a fracture of the lower extremity or neurovascular injury leading to prolonged immobilization); (2) Preexisting mental disorder; and (3) Lack of consent to participate in this study.
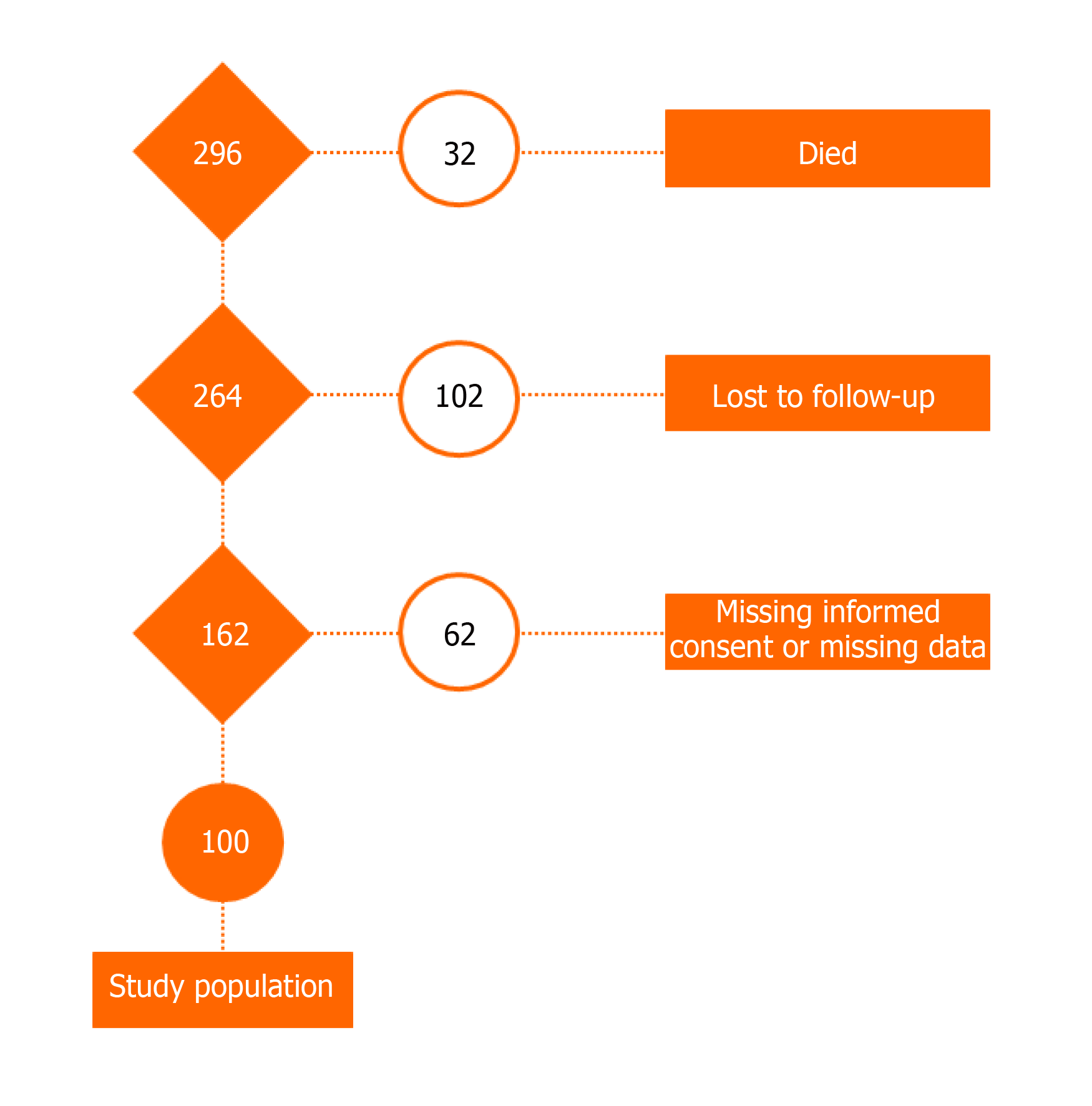
Of initial 296 patients who were treated in a single institution for an acetabular fracture between 07/2002 and 06/2016, 32 patients had died until follow-up, 102 patients were lost to follow-up, 58 patients refused to give their informed consent. Four patients were excluded due to missing data. The patients were asked to complete the questionnaire at follow-up evaluation at mean 5.2 ± 3.6 years after the injury (time point T1). The patients received the questionnaire two weeks after the first questionnaire (time point T2) to evaluate the test-retest reliability and responsiveness. If the patients did not return the questionnaire form within four weeks, the patients were reminded at intervals of two weeks’ time. 55 of 100 patients completed the questionnaire twice on average after 32 ± 71.4 d. Figure 1 shows the patient flow chart.
The Forgotten Joint score is a self-administrated questionnaire comprising of 12 items concerning on the patient’s ability to forget the hip joint in everyday life[11]. Meanwhile, the loss of awareness of a joint is seen as the ultimate goal leading to maximum patient satisfaction. The FJS was developed in 2012. Several studies have proven high internal consistency, responsiveness, and construct validity in mid- and long term conditions after arthroplasty[11,13,17-19]. Originally, it was developed to evaluate PRO in patients after arthroplasty of the knee or hip.
The patients were asked to return the forms by mail. For evaluation of test–retest reliability, the patients were supposed to complete a second questionnaire after a minimum of two weeks. The patients received a reminding call if they did not answer within two weeks.
The WOMAC-VAS is a well-established standardized questionnaire to evaluate the disease-specific health-related quality of life of patients with osteoarthritis of the knee and hip comprising of 24 questions each rated on a VAS (0-100 mm)[20]. Following scores were computed: Subscale pain (0-500 mm), subscale stiffness (0-200 mm), subscale functional limitation (0-1700 mm), and a summary score (0-2400 mm). A WOMAC-VAS score of 0 indicates no pain, no stiffness, and full function. The higher the score is, the more problems the patient is facing. The WOMAC-VAS is validated in German[21].
The TAS is a well-established score reflecting the patient’s highest level of physical activity on a 10 level scale[22]. The TAS is the most commonly reported tool for physical activity in patients with lower extremity disorders. A TAS score of ten reflects the functional capacity of a top-level athlete, a score of 0 reflects the inability to walk. A German adaption is available[23].
The EQ-5D-3L is a HR-QoL questionnaire consisting of subscales regarding mobility, self-care, usual activities, pain/discomfort, and anxiety/depression[24,25]. Responses to each dimension were transformed into EQ index ranging from -0.21 (worst health) to 1.00 (best health). Additionally, the EQ-5D reports the patient’s assessment of the current HR-QoL in a 100 mm visual analogue scale. This scale ranges from 0 (the worst health you can imagine) to 100 (the best health you can imagine).
We asked the patients to evaluate whether the condition of their hip joint had changed since primary evaluation (much better, somewhat better, unchanged, somewhat worse, much worse). For calculation of the responsiveness, the anchor variable was summarized to ‘better’, ‘unchanged’, or ‘worse’.
We reviewed all digital patient charts to record relevant clinical data. Our institution is a level-one trauma-center specialized on management of pelvic injuries. Standard diagnostics at time of injury was a clinical evaluation and a computed tomography (CT) scan of the pelvis. The initial degree of initial and postoperative dislocation was rated according to the Matta scoring system for evaluation of dislocation after acetabular fracture[8]. There was an indication for conservative treatment in cases with no relevant dislocation (less than 2 mm and no involvement of the dome area) measured in the initial CT scan. We recorded clinical parameter like treatment modality (operative vs non-operative/fracture classification according to Letournel/surgical approach) and compared mean values of the FJS between the groups.
Statistical analysis was performed using the software package SPSS (Version 25, SPSS Inc, Chicago, IL, United States). The level of significance was defined at P < 0.05 for all tests. Analyses were exploratory, thus no adjustments of P values for multiple testing were conducted. Questionnaires were computed in accordance with guidelines. If not stated in questionnaire guidelines, missing values were not imputed.
Descriptive data were given as frequencies (n) and percentage (%) for categorical variables, mean ± SD or median and interquartile range (IQR) for continuous variables.
We evaluated the reliability (internal consistency, test-retest reliability, and measurement error), validity (convergent validity and clinical validity), responsiveness to change, and interpretability (data completeness and response distribution) of the FJS based on the COSMIN checklist.
Reliability is the degree to which the measurement is free from measurement error[16].
Internal consistency is the degree of interrelatedness among items[16]. Sufficient internal consistency iukrs assumed for a Cronbach’s α ≥ 0.70[15].
Test–retest reliability is the degree of which an outcome of the same patient in the same health condition remains unchanged over time. As the time interval between first and second testing were heterogeneous (0 to 385 d), intraclass correlation coefficient (ICC, two-way mixed model with absolute agreement, average measures) and its 95%CI was estimated indicating an unchanged health condition regarding their hip function compared to the primary evaluation. For an ICC ≥ 0.70 sufficient test-retest reliability was assumed.
The measurement error is the systematic and random error of a patient’s score that is not attributed to true changes in the construct to be measured[16]. For patients indicating no change in the condition of their hip joint, standard error of measurement (SEM) and smallest detectable change (SDC) were computed to estimate how much a score needs to change to be sure that a true change has occurred (sensitivity to change). SEM was computed by multiplying the standard deviation (SD, all assessments of patients with unchanged condition) by the square root of 1 minus reliability (ICC): SD × (1-ICC)1/2 . SDC was computed by SEM × 1.96 × 21/2[15].
Validity is the degree to which a questionnaire measures the construct it purports to measure[16]. There is no gold standard in the measurement of PRO. Therefore, we rated validity as convergent and clinical validity. Convergent validity is the degree to which the score of the FJS is comparable with the scores of other functional questionnaires (TAS, WOMAC-VAS, EQ Index, EQ VAS). We measured convergent validity by Spearmen’s rank correlation. With a correlation coefficients |≥ 0.60| (absolute value), convergent validity was rated positive. Based on previous results, it is expected that FJS correlates negative and high ≤ -0.60 with WOMAC-VAS subscales and WOMAC-VAS summary score[11], correlates positive and moderate between 0.30 and 0.50 with EQ Index, EQ VAS and TAS[13]. We measured clinical validity of FJS by known-groups comparison using U-test to assess differences between patients with and without articular displacement. Just the first FJS measurement of patients without total hip arthroplasty was assessed.
Responsiveness is the ability of a questionnaire to detect a change over time in the construct to be measured[16]. Changes in FJS were assessed by Wilcoxon tests separate for patients indicating improvement, no change or worsening of hip functioning. Moreover, Cohan’s d effect size (ES) was computed for each patient group by the mean difference between measurement at T1 and T2 by the SD of measurement A: mean difference measure A and B/SD measure A. ES values of 0.2, 0.5, and 0.8 indicate small, moderate and large changes/ responsiveness[15,16]. To assess whether patients with different hip function development (improvement, no change, worsening) differed in baseline FJS, Kruskal-Wallis H-Test was computed.
Interpretability is the ability to transform a qualitative effect into a quantitative score[16]. Interpretability of the FJS was assessed by presenting data completeness and response distribution (floor and ceiling effects). Extreme outcome values might not be represented adequately if more than 15% of patients score lowest (0) value (floor effect) or highest (100) (ceiling effect) levels in the FJS. In cases of floor- or ceiling effects, the questionnaire might also not be able to reflect changes[15].
Table 1 shows mean score values at initial assessment and demographic data. The cohort comprised of 79% men and 21% women. All patients had sustained an acetabular fracture 1 to 14 years before. 22% of these patients were treated conservatively; 78% required surgical treatment. Of 78 patients with surgical treatment, 55 patients required open reduction and internal plate fixation. In 37 cases, an anterior approach (25 × ilio-inguinal and 12 × intrapelvic approach) was necessary. 18 patients required posterior fixation via a Kocher-Langenbeck approach. We carried out operative management according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) principles (Figure 2). According to these recommendations, we aimed for anatomic reduction of the articular surface and internal fixation of the fragments. Aftercare was equal for all patients. We advised the patients to partial weight-bearing of 15 kg for 6 weeks and a step-wise increase of load of 10 kg per week until the patient’s normal weight was reached. For patients with an involvement of the posterior wall, internal rotation of the hip was limited for 6 weeks postoperative. 54/100 patients had an initial articular surface step of more than 3 mm and 46 patients had an initial articular surface step of 3 mm or less. Regarding long-term complications, 4 of 100 patients required a total hip arthroplasty (THA) due to rapid progressive joint degeneration after the acetabular fracture. There were 2/54 patients in the displacement group and 2/46 patients in the other group requiring THA until follow-up evaluation. The time between accident (T0) and follow-up (T1) was 5.2 ± 3.6 years (range 0.2-13.5). The mean age at follow up (T1) was 57.9 ± 17.6 years (range 22-88). The second questionnaire (T2) was completed on average 31.2 ± 71.4 d (range 0-385) after the first.
| n = 100 | Total |
| Sex | 21 female/79 male |
| Mean age at follow up T1 | 57.9 ± 17.6 yr |
| Intra-articular step | 54 > 3 mm/46 < 3 mm |
| Treatment | 78 operative/22 conservative |
| Approach (open reduction only) | 37 anterior/18 posterior |
| FJS | 41.4 ± 29.7 |
| WOMAC-VAS | 60.6 ± 63.3 |
| EQ-5D Index | 0.90 ± 0.09 |
| EQ-5D VAS | 67.8 ± 23.0 |
| TAS | 3.6 ± 1.8 |
The internal consistency of the questionnaire is satisfying, with Cronbach’s alpha = 0.95 for measurement at T1 (n = 83) and 0.97 for measurement at T2 (n = 50). Even with deleting an item, Cronbach’s alpha was high raging between 0.95 and 0.97.
The test-retest reliability was excellent with an ICC = 0.99 (95%CI = 0.97-0.99). We included only patients indicating an unchanged functional condition regarding their hip joint (n = 24).
SEM was 3.2 and SDC was 8.8. Thus, changes > 8.8 points between two assessments denote real change in FJS and changes ≤ 8.8 denote for measurement errors and subject variability.
In both assessments, convergent validity between FJS and WOMAC-VAS, TAS, EQ Index as well as EQ VAS could be confirmed. Correlation coefficients were moderate to high ranging from |0.56| to |0.83| (absolute value). The higher the WOMAC-VAS (pain, stiffness, functional limitation and summary score), the lower the forgetting of the joint. The higher the TAS, EQ index and EQ VAS, the higher the forgetting of the joint (Table 2).
| FJS | WOM I | WOM II | WOM III | WOM total | EQ Index | EQ VAS | TAS |
| r | -0.69 | -0.68 | -0.70 | -0.73 | 0.72 | 0.60 | 0.56 |
| P value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| n | 96 | 96 | 96 | 96 | 96 | 95 | 94 |
Clinical validity was assessed by comparing FJS scores between patients with articular displacement (> 3 mm, n = 54) and patients without articular displacement (≤ 3 mm, n = 46). Patients with (median = 3 8.6, IQR = 12.5/72.9) and without (median = 3 7.5, IQR = 16.6/67.8) articular displacement did not differ in FJS at follow-up evaluation T1 (Z = 0.005, P = 0.996).
We also evaluated clinical validity by comparing the different fracture patterns according to the Letournel classification. We found highest median values for anterior column and posterior hemi-transverse fractures (median = 12.5, n = 11), and lowest levels of the FJS in T-type fractures (median = 72.9, n = 3). However, there were only three patients with a T-type fracture within the study population. There was no significant difference in the FJS between the fracture types according to the Letournel classification (P = 0.795).
There was also no significant difference between the surgical approaches (P = 0.477). Lowest FJS levels (median = 15.6, n = 24) were found in patients undergoing ORIF via an ilio-inguinal approach whereas patients with a Kocher-Langenbeck approach reported highest FJS levels (median 33.3, n = 18).
There was a significant difference in FJS (P = 0.019) comparing patients after conservative treatment (median 68.7, n = 22) to surgically managed patients (median 33.3, n = 78).
Patients with different hip function development did not significantly differ in FJS at initial assessment (H2, 55 = 0.336, P = 0.845). In patients indicating improvement of hip function, the FJS significantly increased (mean difference = 9.4, Z = 3.465, P = 0.001, n = 21). This increase was higher than the SDC of 8.8 and had a small ES of 0.28. In patients indicating worsening of hip function, the FJS significantly decreased (mean difference = 17.1, Z = -2.402, P = 0.016, n = 10). This decrease was higher than the SDC of 8.8 and had a moderate ES of 0.59. Patients indicating no change in hip function did not show differences in FJS (mean difference = 1.1, Z = -0.328, P = 0.743, n = 24, ES = 0.03). Table 3 presents responsiveness data of the FJS.
| n | FJS first assessment | FJS second assessment | Difference FJS first-second assessment | P value | SEM | SDC | ES | ||||
| m | SD | m | SD | m | 95%CI | ||||||
| Function improved | 21 | 46.9 | 34.1 | 56.2 | 34.9 | -9.4 | -13.6–(-5.1) | 0.001 | 0.28 | ||
| Function unchanged | 24 | 43.8 | 31.6 | 42.7 | 32.6 | 1.1 | -1.9–4.1 | 0.743 | 3.2 | 8.8 | 0.03 |
| Function worsened | 10 | 37.7 | 29.0 | 20.2 | 13.1 | 17.1 | 0.7–33.4 | 0.016 | 0.59 | ||
The proportion of missing FJS item responses was 3.9% (47/1200) at first assessment and 1.2% (8/660) at second assessment. For four patients, the FJS at first assessment could not be computed as they had more than four missing responses and thus, these patients were excluded from data analyses.
There was no relevant floor effect [minimum score of 0: first assessment T1: n = 1 (1%), second assessment T2: n = 1 (1%)] and no relevant ceiling effect [maximum score of 100: first assessment T1: n = 1 (1%), second assessment T2: n = 2 (2%)] for the FJS.
The main result of this study is that the FJS is a valid and reliable tool for evaluation of PRO in posttraumatic condition after acetabular fracture. The SDC indicating a real clinical improvement after a change of 8.8 points between FJS assessments. We could confirm responsiveness of the FJS and found no relevant floor- or ceiling effects. This is the first study validating FJS in fractures of the hip joint according to the COSMIN checklist.
An acetabular fracture is an uncommon but serious injury to the hip joint[2,6,8,9,14,26]. The surgeon-based view on clinical and functional outcomes after acetabular fracture is well documented in literature[1,4,5,26-29]. Operative management has become the standard treatment for displaced fractures[2,6,8,26,28,30]. Even though technical advancements have led to major improvements in management of these injuries, there is still a relevant number of cases leading to poor clinical outcomes[5,6]. The presented outcome studies mainly reflect short-term outcomes with a focus on risk factors leading to early failure with posttraumatic rapid-progressive joint degeneration like quality of reduction or stability of the osteosynthetic fixation[2,4,5,7]. However, there is a variety of symptoms sensed by the patient and the patient’s perspective are neglected by most studies on QoL after acetabular fracture[1,2,5,7,8,31]. We chose to include patients with a mid-term result as well as long-term condition in this validating study to represent as many conditions as possible. Demographic data of our patient population is comparable to other studies on acetabular fractures with an average age of 57.9 years at time of injury[2,32,33]. Again, our population represents the broad spectrum regarding age distribution seen in acetabular fracture patients[33]. The FJS was originally designed for patients after arthroplasty of the knee and hip[11]. Therefore, it is compiled for an older, physically less active patient population. However, recent studies have proven reliability in younger patients[12,13,17-19,34]. The FJS measures the patient’s ability to forget the joint in everyday life, which is seen as ultimate goal resulting in maximum patient satisfaction[11]. This concept seems to be a valid construct not just post arthroplasty. We found a mean FJS of 41.6 points in our patient population. Recently, Baumann et al[34] published a validation study on the FJS in long-term results of patients in a posttraumatic condition after tibial head fracture in 77 skiers. They found an increased joint awareness of 70.7 points in the FJS 9-13 years after injury. The mean score in the present study was 41 at first assessment indicating that the level of forgetting the joint after acetabular fracture is lower than in patients after tibial head fracture (70.7)[13], anterior cruciate ligament repair (70.1)[12] or even total hip arthroplasty (59.8)[11]. We included patients of all age groups and operative and non-operative treatment. The distribution of our population’s Letournel classification of acetabular fractures reflects also typical fracture patterns. Therefore, we assume generalizability for this type of injury.
There is ongoing discussion about methodical standards in validation studies[15,16,35]. The validation process in the present study was processed following the COSMIN checklist[16]. Along with the prospective multicenter design, the study meets high methodological standards with a level of evidence Ib.
The FJS has been validated in English and has been adapted in French, Dutch, Danish, Japanese, and German language[11,13,17,18,35,36]. All of these publications gave a positive rating on internal consistency with a Cronbach’s alpha of 0.95-0.97. We measured a Cronbach’s alpha of at least 0.95 in our study. According to Terwee et al[15] internal consistency can be confirmed if Cronbach’s alpha is greater than 0.70 and below 0.95. Greater values reflect higher correlations among the items and might be an indication for a redundancy of two or more items[15]. Cronbach’s alpha is also dependent on the number issues a questionnaire contains; higher values for scores with a higher number of items. The FJS consists of only 12 items. Therefore, it seems that the concept of the FJS with measurement of the joint awareness for every question could be the reason for a high level of internal consistency.
Prior studies reported a test-retest reliability of the FJS between 0.80 and 0.97[13,18,36]. We found perfect test-retest reliability with an ICC of 0.99. We intended to include also patients with a long-term result years after injury. In these cases, we assumed a stable medical condition making the ICC robust. The long period of time between time points T1 and T2 in some cases leading to a SD of 71.4 days is a potential source of bias. However, the anchor-based method to include only patients with a subjective steady medical condition should lead to reliable results from a statistical point of view.
We expected the WOMAC-VAS, TAS, and EQ-5D-3L to be appropriate for evaluation of construct validity, because these scores are widely used and a German language version of all scores was validated for sports related injuries and arthroplasty patients[23,24,37]. We decided to use the WOMAC-VAS score as tool for evaluation of validity because it was used in the original publication of the FJS as well[11]. The FJS showed good correlation to the total score of the WOMAC-VAS as well as to the WOMAC-VAS subscales.
To investigate if a risk factors for rapid-progressive joint degeneration like a residual joint surface step of more than 3 mm might have an impact on patient-centered HR-QoL, we collected data from the initial CT scan in cases of conservative treatment and the post-operative CT scan in operatively treated patients. We expected that a complex fracture pattern or a residual articular step would lead to a lower level of forgetting the joint because of inflammation of the joint. However, we did not find any impact of the fracture pattern according to Letournel or an articular surface step of more than 3 mm in the CT scan on the FJS at time of the validation study. This is probably due to the long period mean time between injury and mean follow-up of more than 5 years. It is likely that the patients with a clinically relevant joint step develop joint degeneration within the first two years after injury (n = 4/100). The other patients with an initial articular step might have sustained a consolidation in functional joint kinetics to a sub-clinical degree. From our perspective, this is an interesting finding and is worth further investigating.
However, we did find a difference between surgical and conservative management. Patients after conservative management reported higher levels in the FJS than surgically treated patients. We recommended conservative management with partial weight bearing only in cases with no dislocation of the fragments. We suspect that this reflects a potential selection bias for conservatively treated patients.
Another important issue for the use of PROMs for further prospective trials is responsiveness to change in medical condition. With a lack of gold standard, defining responsiveness is difficult. According to the COSMIN checklist, we assessed responsiveness in patients by Wilcoxon tests and ES[16]. The FJS score has shown good responsiveness in post-arthroplasty conditions longer than 12 mo post-operatively[11,13,38]. In this study, patients indicating no change in function of the hip, FJS scores did not significantly differ, and the mean differences was with 1.1 below the SDC of 8.8. In patients indicating a change in medical condition of the hip, FJS scores significantly differed between both assessments and the mean differences were above the computed SDC. Therefore, we could give a positive rating for responsiveness.
According to the guidelines of the original FJS publication in 2012, we refused to calculate the FJS if more than four items were missing. The overall proportion of missing items of the FJS was 4% at first assessment. Concordant to all prior studies on the FJS, there was no relevant floor- or ceiling effect[11,12,17,18,35,36,38].
The findings of this study have to be seen in the light of some limitations. First of all, the limited number of cases. Acetabular fractures are uncommon and treatment is concentrated to large trauma centers. We assume that our population can be seen as reference population for most centers, since our age distribution is relatively broad and we included conservatively and operatively treated patients to reflect clinical reality. Another limitation is that the time span between first and second evaluation showed quite some variability. Although we put major efforts on guidance of the patients to assure highest methodical quality, there is a natural variation in the recorded data. Finally, calculation of ICC was based on only 24 patients. This was the number of patients who indicated no relevant clinical change in medical condition of their hip joint between T1 and T2. Further studies are needed to confirm the results based on longitudinal data.
This is the first study validating FJS in fractures of the hip joint according to the COSMIN checklist. The FJS is a valid and reliable tool for evaluation of PRO in posttraumatic condition after acetabular fracture. With a Cronbach’s alpha of 0.95, internal consistency of the questionnaire was good. Test-retest reliability was excellent with an ICC of 0.99. Based on the anchor variable, the SDC indicating a real clinical improvement was 8.8 points in the FJS. We could confirm responsiveness of the FJS and found no relevant floor- or ceiling effects. Clinicians are suggested to use the FJS for evaluation of PRO after fractures of the acetabulum.
Patient-reported outcome (PRO) measurement is gaining more and more importance in clinical decision-making. Evaluation of psychometric properties of PRO tools is essential to assure validity.
A fracture of the acetabulum is an uncommon but serious injury. Outcome evaluation tools in patients after acetabular fractures are outdated. However, research based on large registries are dependent on valid outcome tools to allow the comparability.
Aim of the study was to validate the Forgotten Joint Score (FJS) according the COSMIN checklist. The FJS is a novel PRO tool to disease-specific quality of life in musculo-skeletal disorders.
The COSMIN checklist is a standard protocol to assure methodical quality of validation studies. The COSMIN checklist consists of ten items giving recommendations for design, conduction and interpretation of medical validation studies. Relevant characteristics are study design, content validity, structural validity, internal consistency, cross-cultural validity/measurement invariance, reliability, measurement error, criterion validity, hypotheses testing for construct validity, and responsiveness.
We found the FJS to be a valid and reliable tool for evaluation of PRO in posttraumatic condition after an acetabular fracture. With a Cronbach’s alpha of 0.95, internal consistency of the questionnaire was good. Test-retest reliability was excellent with an ICC of 0.99. Based on the anchor variable, the smallest detectable change indicating a real clinical improvement was 8.8 points in the FJS. We could confirm responsiveness of the FJS and found no relevant floor- or ceiling effects.
Clinicians are suggested to use the FJS for evaluation of PRO after fractures of the acetabulum.
Further studies are needed to confirm the study results, especially concerning longitudinal data. Based on the study results, the FJS can now be used for further clinical studies on post-traumatic conditions after fractures of the acetabulum.
We thank all participants for contributing to this study. The authors wish to thank the German Pelvic Multicenter Study Group (http://www.dgu-online.de) for their support in the conception of the study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kuo YL, von Engelhardt LV S-Editor: Zhang H L-Editor: A P-Editor: Xing YX
| 1. | Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. J Bone Joint Surg Br. 2011;93:229-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 173] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 2. | Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94:1559-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 283] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 3. | Piazzolla A, Baglioni M, Solarino G, Vicenti G, Panella A, Moretti B. Acetabular fractures: Is it possible to regain the same patient's related quality of life before trauma? Injury. 2018;49 Suppl 3:S74-S76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Busch A, Stöckle U, Schreiner A, de Zwaart P, Schäffler A, Ochs BG. Total hip arthroplasty following acetabular fracture: a clinical and radiographic outcome analysis of 67 patients. Arch Orthop Trauma Surg. 2020;140:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Meena UK, Tripathy SK, Sen RK, Aggarwal S, Behera P. Predictors of postoperative outcome for acetabular fractures. Orthop Traumatol Surg Res. 2013;99:929-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 385] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 7. | García-Rey E, Sirianni R, García-Cimbrelo E, Sedel L. Total hip arthroplasty after acetabular fracture: does initial treatment make any difference to the outcome? Hip Int. 2020;30:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 886] [Cited by in RCA: 883] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 9. | Verbeek DO, van der List JP, Tissue CM, Helfet DL. Predictors for Long-Term Hip Survivorship Following Acetabular Fracture Surgery: Importance of Gap Compared with Step Displacement. J Bone Joint Surg Am. 2018;100:922-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 10. | d'Aubigné RM, Postel M. The classic: functional results of hip arthroplasty with acrylic prosthesis. 1954. Clin Orthop Relat Res. 2009;467:7-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Behrend H, Giesinger K, Giesinger JM, Kuster MS. The "forgotten joint" as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 2012; 27: 430-436. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 577] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 12. | Behrend H, Zdravkovic V, Giesinger JM, Giesinger K. Joint awareness after ACL reconstruction: patient-reported outcomes measured with the Forgotten Joint Score-12. Knee Surg Sports Traumatol Arthrosc. 2017;25:1454-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Baumann F, Ernstberger T, Loibl M, Zeman F, Nerlich M, Tibesku C. Validation of the German Forgotten Joint Score (G-FJS) according to the COSMIN checklist: does a reduction in joint awareness indicate clinical improvement after arthroplasty of the knee? Arch Orthop Trauma Surg. 2016;136:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Baumann F, Schmitz P, Mahr D, Kerschbaum M, Gänsslen A, Nerlich M, Worlicek M. A guideline for placement of an infra-acetabular screw based on anatomic landmarks via an intra-pelvic approach. J Orthop Surg Res. 2018;13:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5565] [Cited by in RCA: 7299] [Article Influence: 384.2] [Reference Citation Analysis (0)] |
| 16. | Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19:539-549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2083] [Cited by in RCA: 2762] [Article Influence: 184.1] [Reference Citation Analysis (0)] |
| 17. | Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H, Yuasa T, Behrend H, Kaneko K. Validation study of the Forgotten Joint Score-12 as a universal patient-reported outcome measure. Eur J Orthop Surg Traumatol. 2015;25:1141-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | Shadid MB, Vinken NS, Marting LN, Wolterbeek N. The Dutch version of the Forgotten Joint Score: test-retesting reliability and validation. Acta Orthop Belg. 2016;82:112-118. [PubMed] |
| 19. | Baumann F, Krutsch W, Worlicek M, Kerschbaum M, Zellner J, Schmitz P, Nerlich M, Tibesku C. Reduced joint-awareness in bicruciate-retaining total knee arthroplasty compared to cruciate-sacrificing total knee arthroplasty. Arch Orthop Trauma Surg. 2018;138:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833-1840. [PubMed] |
| 21. | Stucki G, Meier D, Stucki S, Michel BA, Tyndall AG, Dick W, Theiler R. [Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index]. Z Rheumatol. 1996;55:40-49. [PubMed] |
| 22. | Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985: 43-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1649] [Cited by in RCA: 1898] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 23. | Swanenburg J, Koch PP, Meier N, Wirth B. Function and activity in patients with knee arthroplasty: validity and reliability of a German version of the Lysholm Score and the Tegner Activity Scale. Swiss Med Wkly. 2014;144:w13976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3307] [Cited by in RCA: 4085] [Article Influence: 170.2] [Reference Citation Analysis (0)] |
| 25. | Greiner W, Claes C, Busschbach JJ, von der Schulenburg JM. Validating the EQ-5D with time trade off for the German population. Eur J Health Econ. 2005;6:124-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 288] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 26. | Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003: 173-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 239] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 27. | Baker G, McMahon SE, Warnock M, Johnston A, Cusick LA. Outcomes of conservatively managed complex acetabular fractures in the frail and elderly one year post injury. Injury. 2020;51:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | de Palma L, Santucci A, Verdenelli A, Bugatti MG, Meco L, Marinelli M. Outcome of unstable isolated fractures of the posterior acetabular wall associated with hip dislocation. Eur J Orthop Surg Traumatol. 2014;24:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Wenzel L, von Rüden C, Thannheimer A, Becker J, Brand A, Augat P, Perl M. The Pararectus Approach in Acetabular Surgery: Radiological and Clinical Outcome. J Orthop Trauma. 2020;34:82-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 30. | LETOURNEL E. [Fractures of the cotyloid cavity, study of a series of 75 cases]. J Chir (Paris). 1961;82:47-87. [PubMed] |
| 31. | Nicholson JA, Scott CEH, Annan J, Ahmed I, Keating JF. Native hip dislocation at acetabular fracture predicts poor long-term outcome. Injury. 2018;49:1841-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 32. | Ochs BG, Marintschev I, Hoyer H, Rolauffs B, Culemann U, Pohlemann T, Stuby FM. Changes in the treatment of acetabular fractures over 15 years: Analysis of 1266 cases treated by the German Pelvic Multicentre Study Group (DAO/DGU). Injury. 2010;41:839-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 33. | Herath SC, Pott H, Rollmann MFR, Braun BJ, Holstein JH, Höch A, Stuby FM, Pohlemann T. Geriatric Acetabular Surgery: Letournel's Contraindications Then and Now-Data From the German Pelvic Registry. J Orthop Trauma. 2019;33 Suppl 2:S8-S13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 34. | Baumann F, Weber J, Mahr D, Bäumlein M, Kerschbaum M, Müller K, Rillmann P, Nerlich M, Loibl M. Joint awareness in posttraumatic osteoarthritis of the knee: validation of the forgotten joint score in long term condition after tibial plateau fracture. Health Qual Life Outcomes. 2017;15:233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Thienpont E, Vanden Berghe A, Schwab PE, Forthomme JP, Cornu O. Joint awareness in osteoarthritis of the hip and knee evaluated with the 'Forgotten Joint' Score before and after joint replacement. Knee Surg Sports Traumatol Arthrosc. 2016;24:3346-3351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 36. | Thomsen MG, Latifi R, Kallemose T, Barfod KW, Husted H, Troelsen A. Good validity and reliability of the forgotten joint score in evaluating the outcome of total knee arthroplasty. Acta Orthop. 2016;87:280-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 106] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 37. | Wirth B, Liffert F, de Bruin ED. [Development and evaluation of a German version of the Lysholm score for measuring outcome after anterior cruciate ligament injuries]. Sportverletz Sportschaden. 2011;25:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Giesinger JM, Behrend H, Hamilton DF, Kuster MS, Giesinger K. Normative Values for the Forgotten Joint Score-12 for the US General Population. J Arthroplasty. 2019;34:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |