Published online Apr 18, 2020. doi: 10.5312/wjo.v11.i4.222
Peer-review started: December 10, 2019
First decision: February 20, 2020
Revised: February 21, 2020
Accepted: March 12, 2020
Article in press: March 12, 2020
Published online: April 18, 2020
Processing time: 125 Days and 4.2 Hours
Orthopedic surgery in children with cerebral palsy (CP) aims to improve function and prevent deformities. Each child’s condition in CP is unique and many co-variables influence surgical decision-making including a patient's age and their functional level. Little is known about the frequency of different types of orthopedic surgery in children with CP who have varied functional levels, particularly in countries from Latin America.
To assess the type of orthopedic surgical procedures in relation to age and gross motor function in children with CP.
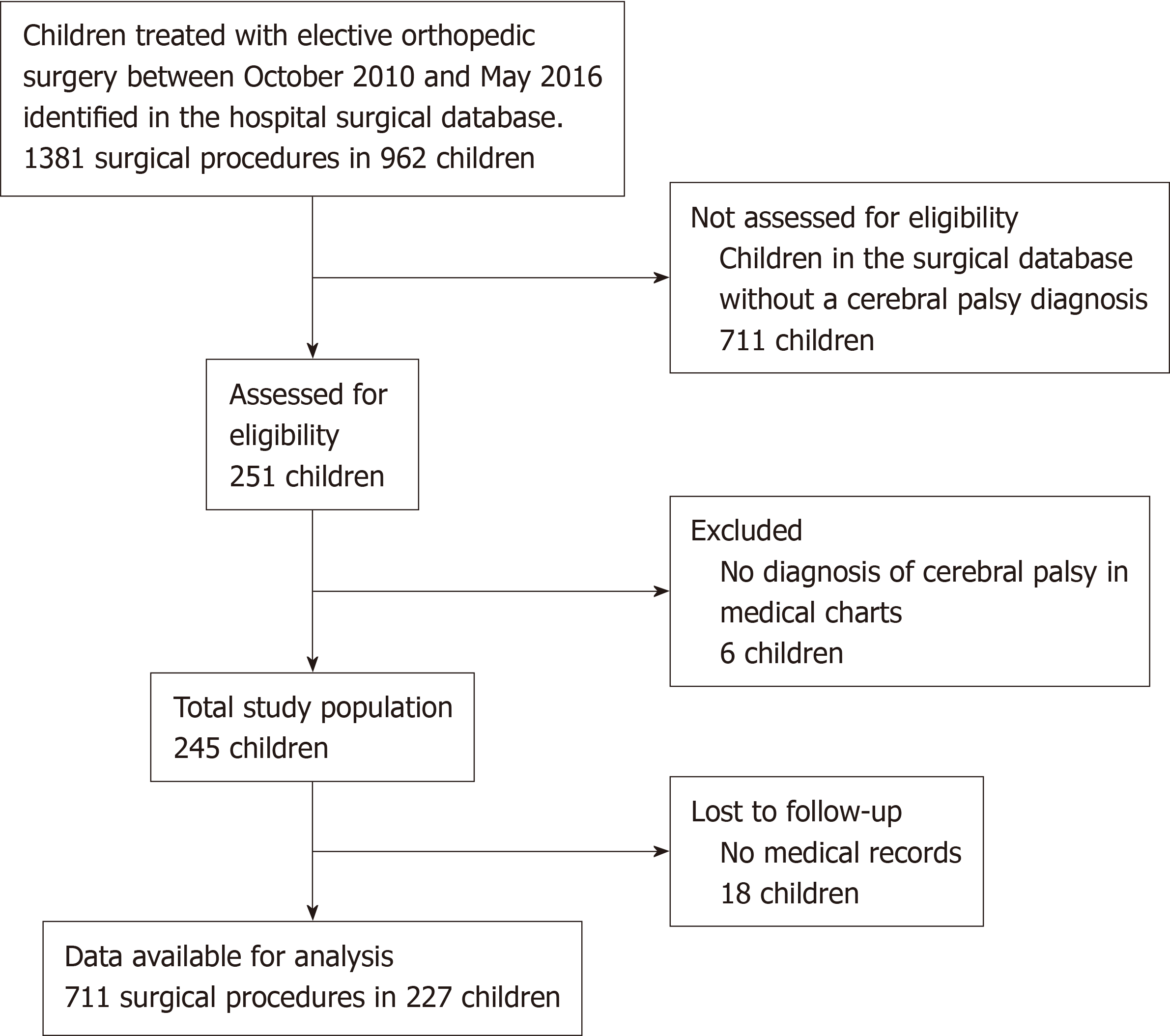
This retrospective study included all children with CP (n = 245) treated with elective orthopedic surgery at a Uruguayan university hospital between October 2010 and May 2016 identified from a surgical database. Eighteen children (7%) were lost to follow-up due to missing medical charts. Demographics, gross motor function classification (GMFCS), and orthopedic surgeries were obtained from the medical records of 227 children. Chi-squared tests and analysis of variance were used to assess the frequency of surgery, accounting for GMFCS levels. Mean age for soft tissue vs bone surgery was compared with the independent samples t-test.
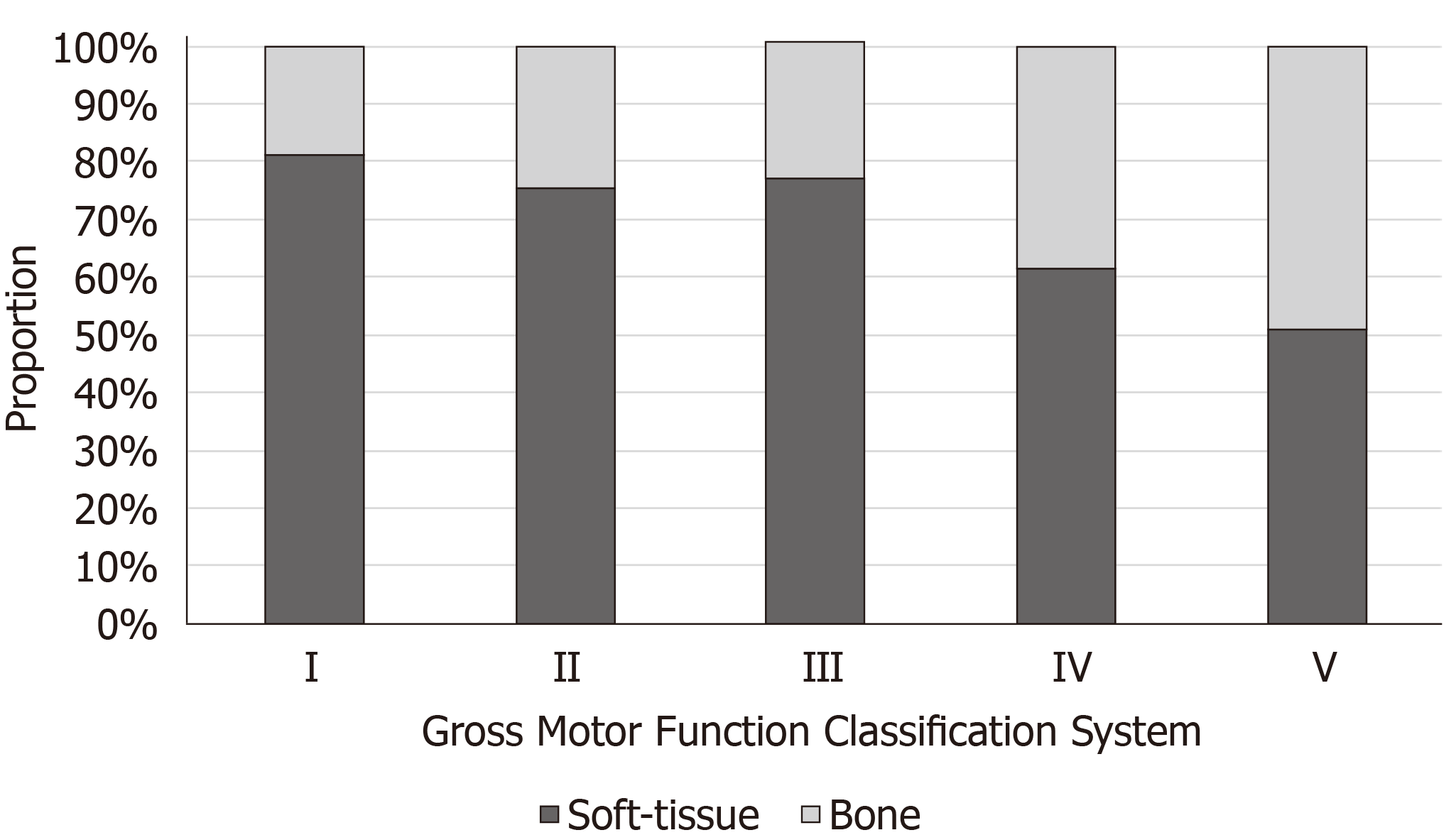
A total of 711 surgical procedures were performed between 1998 and 2016. On average, children had 3.1 surgical procedures and the mean age at first surgery was 8.0 years. There were no significant differences in age at first surgery among GMFCS levels (P = 0.47). The most common procedures were lower leg soft tissue surgery (n = 189, 27%), hip tenotomy (n = 135, 19%), and hamstring tenotomy (n = 104, 14%). For children with GMFCS level I, the mean number of surgeries per child [1.8 (range 1-9)] differed significantly at P < 0.05 in children with GMFCS levels II [3.2 (1-12)], III [3.2 (1-8)], IV [3.3 (1-13)], and V [3.6 (1-11)]. Within II, III, IV, and V, there was no significant difference in mean number of surgeries per child when comparing across the groups. The proportion of soft tissue surgery vs bone surgery was higher in GMFCS levels I-III (80%-85%) compared to levels IV (68%) and V (55%) (P < 0.05).
The frequency of surgical procedures per child did not increase with higher GMFCS level after level I. However, the proportion of bone surgery was higher in GMFCS levels IV-V compared to I-III.
Core tip: Little is known about the frequency of different types of orthopedic surgery in children with cerebral palsy, particularly in Latin America, as most studies related to orthopedic surgery are retrospective case series describing a specific surgery. This paper illustrated that among Uruguayan children with cerebral palsy, the number of corrective surgeries performed did not differ by functional motor ability (gross motor function classification levels) after level I, but the types of surgeries did differ by gross motor function classification levels. The proportion of soft tissue surgery vs bone surgery was higher in ambulatory children compared to non-ambulatory children.
- Citation: Rehbein I, Teske V, Pagano I, Cúneo A, Pérez ME, von Heideken J. Analysis of orthopedic surgical procedures in children with cerebral palsy. World J Orthop 2020; 11(4): 222-231
- URL: https://www.wjgnet.com/2218-5836/full/v11/i4/222.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i4.222
Cerebral palsy (CP) is the most common neurologic disorder causing motor impairment in children and affects 2-3 of 1000 children[1]. In Uruguay, this amounts to roughly 100 children diagnosed with CP annually. CP is commonly classified not only by the dominant symptom, but by functional motor ability, according to the Gross Motor Functional Classification Scale (GMFCS)[2].
Orthopedic surgery is common in children with CP. A Danish registry study concluded that 41% of children between 8 and 15 years with GMFCS level I, 54% with level II, and 62% with levels III, IV or V had received orthopedic surgery[3]. Orthopedic surgery aims to improve the child’s quality of life by controlling pain, optimizing independence and self-care, maximizing movement, balance and coordination, and maintaining functionality[4]. Another primary indication for orthopedic surgery is to prevent future complications such as contractures, hip dislocations, and scoliosis progression[5]. Each child’s condition in CP is unique making it difficult to establish guidelines about when is the best age for different types of orthopedic surgery. Several factors affect the timing for a surgical procedure: the change of spasticity over time which in general is most severe in preschoolers[6], the development of joint contractions[7], hip migration[8], pain[9], the GMFCS level and comorbidities[4,7].
There is a trend towards single event multilevel surgery (SEMLS), which can be defined as two or more soft tissue or bony surgical procedures performed at two or more anatomical levels during a single surgery[10]. Avoiding repeated operations has many advantages, including fewer hospital admissions and periods of rehabilitation. Little is known about the frequency of different types of orthopedic surgery in children with CP. Most studies related to orthopedic surgery are retrospective case series describing a specific surgery. We are only aware of one published study in the literature that has described the frequency of orthopedic surgical procedures in children with CP[11] and to the best of our knowledge, there are no studies of this kind in Latin America.
The aim of this retrospective cohort study was to analyze the frequency, anatomic location, and type of orthopedic surgical procedures in relation to age and gross motor function in children with CP. We hypothesized that the frequency of surgical procedures per child would increase with higher GMFCS level.
Institutional Human Subjects approval was obtained for this study from our local Board (Centro Hospitelario Pereira Rossell).
We retrospectively reviewed the charts of all patients with CP treated with orthopedic surgery at a public university hospital providing care to children of lower socioeconomic status in Montevideo between October 2010 and May 2016. Patients were identified from the hospital surgical electronic database for elective orthopedic surgery. As the surgical registry became computerized in October 2010 this date was chosen as the start date for the study. Among the 251 patients retrieved from the surgical database, 6 did not have a CP diagnosis recorded in the medical charts and were excluded. Thus, 245 patients with CP treated with orthopedic surgery were included in this study. The flow of the patients through the study is illustrated in Figure 1.
CP subtype was classified according to the Surveillance of Cerebral Palsy in Europe into Bilateral Spastic, Unilateral Spastic, Dyskinetic, Ataxic, and Non classifiable CP[12]. GMFCS level was established based on findings in the medical history from the treating physician or rehabilitation physician. Because this classification system was not used in our hospital from the beginning of the study period, we chose to use the last recorded GMFCS level in the medical charts. During phase one of the data collection, all orthopedic surgeries recorded in the patients’ medical history were collected and confirmed by reading the surgical history in the medical chart. The type of surgery was noted, soft tissue or bone, and classified according to the most affected anatomical location as follows: Spine, upper extremity, pelvic osteotomy, proximal femur osteotomy, hip tenotomy, distal femur osteotomy, surgery for patella alta, hamstring tenotomy, osteotomy lower leg, soft tissue lower leg, and foot. Soft tissue lower leg surgery included: slide and Z lengthening of the Achilles tendon and soleus and gastrocnemius aponeurotic lengthening such as Vulpius to treat foot equinus. Orthopedic surgeries that could not be classified into this system were defined as “other” types of surgery. For example, “other” included implant removal, wound infection requiring a reoperation, or correction of cast. Bilateral procedures of the same type and on the same date were counted as one surgery. The surgical procedure with two or more soft tissue or bony surgical procedures at two or more anatomical levels during one operative procedure was classified as an SEMLS[10]. Pelvic osteotomies with proximal femur osteotomy and hip tenotomy were not classified as a single event multi-level surgery. A database was constructed using data extracted from the charts.
Descriptive statistics such as counts, percentages, means and standard deviations or medians with ranges were used to characterize the sample. Age at first surgery, surgeries per patient, and mean number of surgical sessions was compared among GMFCS levels using one-way analysis of variance (ANOVA). Number of surgeries classified by type of surgery (soft tissue and bone surgery) was compared using the chi-squared test. Mean age for soft tissue vs bone surgery was compared with the independent samples t-test. P values of 0.05 or less were considered statistically significant. Statistical analysis was performed with the statistical program SPSS for Mac 23.0 (http://www.spss.com, SPSS Inc., Chicago, IL, United States).
The statistical methods of this study were reviewed by Dr. Maura Daly Iversen, Professor of Public Health and Physical Therapy Sacred Heart University.
Of the 245 patients included in the study, 18 (7%) were lost due to missing charts. Thus, data on 227 patients with CP (46% female) were obtained from the medical records. The mean age of the patients at the first surgery was 8.1 years (range 2-19) and the mean follow-up from first surgery was 52 mo (range 0-219 mo). Most children were classified as having spastic diplegia (80%) or spastic hemiplegia (17%). In 1% of children, the CP subtype was not possible to classify. The proportion of children within the different GMFCS levels was I = 14%, II = 22%, III = 18%, IV = 23, and V = 23% (Table 1).
| Variable | Value |
| Mean age at first surgery, yr (range) | 8.1 (2-19) |
| Mean age at end of study period, yr (range) | 12.5 (4-27) |
| Female, n (%) | 105 (46) |
| Cerebral Palsy subtype, n (%) | |
| Bilateral spactic | 180 (80) |
| Unilateral spactic | 38 (17) |
| Dyskinetic | 5 (2) |
| Ataxic | 1 (0) |
| Non classifiable | 3 (1) |
| GMFCS level, n (%) | |
| I | 33 (14) |
| II | 51 (22) |
| III | 40 (18) |
| IV | 52 (23) |
| V | 51 (23) |
Table 2 illustrates surgical characteristics of the 227 children. There were 711 total surgical procedures performed on these children between 1998 and 2016. The mean number of surgeries per patient was 3.1 (range 1-13). An ANOVA on the mean number of surgeries per child between different GMFCS levels yielded significant variation, F (4, 222) = 3.69, P = 0.006. A post hoc Tukey test showed that for children with GMFCS level I, the mean number of surgeries per child [1.8 (range 1-9)] differed significantly at P < 0.05 with children with GMFCS levels II [3.2 (1-12)], III [3.2 (1-8)], IV [3.3 (1-13)], and V [3.6 (1-11)]. Within GMFCS levels II, III, IV, and V, there was no significant difference in the mean number of surgeries per child. Taken together, these results suggest that children with GMFCS level I have significantly fewer surgeries than children with more limited ability to ambulate. However, the frequency of surgical procedures per child did not increase with higher GMFCS level after level I.
| Variable | Value |
| Total number of surgeries | 711 |
| Mean number of surgeries per patient (range) by GMFCS | |
| I | 1.8 (1-9) |
| II | 3.2 (1-12) |
| III | 3.2 (1-8) |
| IV | 3.3 (1-13) |
| V | 3.6 (1-11) |
| Total number of visits to the surgical theater | 413 |
| Mean number of visits to the surgical theater per patient (range)1 | 1.8 (1-10) |
| Mean number of visits to the surgical theater per patient (range) by GMFCS | |
| I | 1.4 (1-5) |
| II | 1.9 (1-6) |
| III | 1.7 (1-4) |
| IV | 1.8 (1-7) |
| V | 2.1 (1-10) |
| Number of single event multilevel surgeries2 (% of all visits to the surgical theater) | 140 (34%) |
| Number of hip salvage procedures (% of patients) | 4 (1.7%) |
| Number of deep infections (% of all surgeries not including revisions for infections) | 2 (0.3%) |
The ANOVA test demonstrated no significant differences in age at first surgery among GMFCS levels [F (4, 222) = 1.71, P = 0.47]. Not including surgeries classified as other, 441 surgeries were classified as soft tissue surgery and 217 as bone surgery. The mean age for soft tissue surgery was 8.3 years compared to 11.0 years for bone surgery (P < 0.05). The proportion of soft tissue surgery was higher in GMFCS levels I-III (77%) compared to levels IV-V (59%) (P < 0.05) (Figure 2).
The total number of visits to the surgical theater for children in this study was 413. The mean number of surgeries per child was 1.8 (1-10). ANOVA on the mean number of surgeries per child between different GMFCS levels yielded no significant variation [F (4, 222) = 1.71, P = 0.149]. Of the 413 times a child was in the surgical theater, SEMLS was performed 140 times (34%) with an average of 2.6 (range 2-5) procedures. The distribution of children who underwent SEMLS based on GMFCS level was I = 5%, II = 25%, III = 26%, IV = 26%, and V = 18%.
The most common procedures performed were soft tissue surgery of lower leg [number of procedures = 189 (27%)], adductor psoas tenotomy [n = 135 (19%)], and hamstring tenotomy (n = 102 (14%)) (Table 3). Of all the surgeries, 8% were classified as other including removal of osteosynthesis material, correction of casts and in two children, surgical treatment due to post-operative infection. The most common soft tissue surgery of the lower leg was unilateral or bilateral Vulpius (78%). In 22% of the children with soft tissue surgery of the lower extremity, the procedure was repeated 1-3 times on the same side. Hip surgery, regardless of the type, was more common in GMFCS levels IV and V. The mean age for pelvic osteotomies was 8 years (range 3-16) and hip tenotomies was 8 years (range 2-16). Among the 227 patients, hip salvage procedures were performed in 4 children (1.7% of the patients). The mean age at surgery for soft tissue lower leg, hamstring tenotomy, hip tenotomy, and pelvic osteotomy was under 10 years. The mean age at surgery was 10 years or more for foot, lower leg osteotomy, surgery for patella alta, distal femur osteotomy, proximal femur osteotomy, upper extremity surgery, and spine surgery.
| Type of surgery | Gross Motor Function Classification System | Total | ||||||||||
| I | II | III | IV | V | ||||||||
| n (%) | Years (range) | n (%) | Years (range) | n (%) | Years (range) | n (%) | Years (range) | n (%) | Years (range) | n (%) | Years (range) | |
| Spine | 0 | NA | 1 (1) | 10 (10-10) | 1 (1) | 14 (14-14) | 3 (2) | 11 (11-11) | 5 (3) | 13 (11-15) | 9 (1) | 13 (10-15) |
| Upper extremi-ty | 1 (2) | 10 (10-10) | 0 | NA | 1 (1) | 10 (10-10) | 1 (1) | 12 (12-12) | 0 | NA | 3 (0) | 11 (10-12) |
| Pelvic osteo-tomy1 | 2 (3) | 13 (12-12) | 1 (1) | 13 (13-13) | 2 (2) | 7 (6-8) | 7 (4) | 8 (5-13) | 21 (12) | 7 (3-16) | 33 (5) | 8 (3-16) |
| Proxi-mal femur osteo-tomy | 4 (7) | 12 (7-15) | 15 (9) | 10 (5-15) | 14 (11) | 11 (5-16) | 22 (13) | 11 (3-20) | 42 (23) | 8 (1-23) | 98 (14) | 10 (1-23) |
| Hip teno-tomy | 4 (7) | 7 (4-8) | 22 (13) | 7 (0-14) | 31 (24) | 8 (4-15) | 32 (19) | 8 (3-15) | 46 (24) | 7 (1-16) | 135 (19) | 8 (0-16) |
| Distal femur osteo-tomy | 0 | NA | 6 (4) | 15 (14-18) | 7 (5) | 13 (12-15) | 18 (11) | 14 (10-20) | 5 (3) | 15 (12-18) | 36 (5) | 15 (10-20) |
| Surgery for Patella alta | 0 | NA | 5 (3) | 16 (13-18) | 2 (1) | 13 (13-13) | 2 (1) | 12 (10-15) | 0 | NA | 9 (1) | 15 (10-18) |
| Hamstr-ing tenoto-my | 2 (3) | 11 (7-15) | 22 (13) | 8 (0-15) | 24 (19) | 7 (5-15) | 33 (19) | 8 (4-15) | 21 (12) | 8 (2-16) | 102 (14) | 8 (0-16) |
| Osteo-tomy lower leg | 0 | NA | 2 (1) | 10 (10-11) | 1 (1) | 19 (19-19) | 1 (1) | 10 (10-10) | 0 | NA | 4 (1) | 13 (10-19) |
| Soft tissue lower leg | 41 (67) | 8 (4-15) | 65 (39) | 8 (0-16) | 38 (30) | 8 (0-17) | 32 (19) | 9 (4-16) | 14 (8) | 7 (3-12) | 189 (27) | 8 (0 -17) |
| Foot | 5 (8) | 10 (7-13) | 13 (8) | 13 (9-17) | 3 (2) | 13 (12-14) | 11 (7) | 13 (9-16) | 8 (4) | 11 (2-18) | 40 (6) | 12 (2-18) |
| Other2 | 2 (3) | 6 (0-13) | 13 (8) | 14 (7-19) | 6 (5) | 13 (5-21) | 10 (6) | 13 (8-18) | 22 (12) | 10 (2-18) | 53 (8) | 12 (0-21) |
| Total | 61 | 9 (0-15) | 165 | 10 (0-19) | 130 | 9 (3-21) | 172 | 10 (3-20) | 183 | 8 (1-23) | 711 | 9 (0-23) |
This study analyzed the frequency, anatomic location, and type of orthopedic surgical procedures in relation to age and gross motor function in children with CP in a public university hospital providing care to children of lower socioeconomic status. We hypothesized that the frequency of surgical procedures per child would increase with higher GMFCS level. This hypothesis could not be confirmed with our data, as the frequency of surgical procedures per child did not increase with higher GMFCS level after level I. This result could partly be explained by the indication and goal of the surgery in an ambulatory child, which is to improve gait, compared to the goal of surgery in a non-ambulatory child where the goal of treatment is often related to pain relief, greater comfort with positioning, improved basic care, correction of severe foot deformities, prevention of hip dislocation, and/or to halt progression of scoliosis[5]. Another reason is that the benefit of surgery in non-ambulatory children needs to be judged against the increased risk of major complications due to the presence of comorbidities such as malnutrition and decreased pulmonary and cardiac function[7]. Additionally, there is also an increased risk of complications from surgery such as nerve palsies and neuropathic pain in this patient group[5].
We identified only one published study that described the frequency of orthopedic surgical procedures in children with CP[11]. This study examined data from 127 children and only classified lower extremity surgeries. The researchers did not include children with GMFCS level V and children with hemiplegia who had isolated tendo-achilles lengthening surgery. The average age at first operation was 6.9 years compared to 8.0 years in our study. These researchers also found no significant differences among GMFCS levels for the number of procedures performed, but children at GMFCS level II underwent significantly more surgical sessions than those at level I. Since there are few data reported, it is hard to draw any conclusion about whether children in our cohort received similar numbers of surgeries compared to other parts of the world.
Few children in our study had surgery at a very young age, because in preschool children with CP, orthopedic issues are normally treated without surgery[5]. However, children with more severe forms of CP often receive adductor-psoas tenotomies at young age to prevent hip subluxation[13]. In our study, surgery among ambulatory children aged 6 to 10 years focused on limb alignment, often as SEMLS in GMFCS level higher than I. Among non-ambulatory children aged 6 to 10 years, surgery focused on prevention of hip subluxation or dislocation. Among adolescents, surgeries focus more on preventing recurrence of lower extremity deformities.
Among all surgeries performed, roughly one-third of the surgeries were SEMLS. However, the complexity of the SEMLS varied between lengthening of two tendons on two different anatomic levels and advanced surgery combining both soft tissues and bony procedures in more than two different anatomic levels.
Even though orthopedic surgery in children with CP focuses primarily on the lower extremities, one might expect a higher prevalence of upper extremity surgeries in this cohort. However, we found only three upper extremity surgeries in our data. One possible explanation for this small number of upper extremity surgeries in our study is that in Uruguay plastic surgeons are responsible for correcting wrist and hand deformities. We did not have access to these medical charts and therefore, the real number of upper extremity surgeries in our study population is probably higher.
Among the nine children in our study who had scoliosis surgery, none developed a wound infection, while Samdini et al[14] reported 4.7% of spine surgeries in 127 children with CP resulted in wound infections requiring re-operation. Since we did not include unplanned surgeries performed outside surgical hours (evenings and weekends), we may be under-estimating the post-operative infections requiring surgery. However, we did not find any indication of under-reporting in the medical charts.
As with all retrospective research, this study had several limitations. One is that it was conducted by reviewing medical charts at a single hospital including only children with at least one orthopedic surgery. Therefore, these results may have limited generalizability. Since we did not know the total number of children with CP we could not determine the incidence of orthopedic surgery in this sample of patients. Additionally, there could be patients with CP that were not registered for elective surgery with a CP diagnosis in the hospital surgical electronic database and therefore, were not included in the study. However, to minimize this selection bias, we examined medical records to determine whether any patients without a CP diagnosis had a surgical procedure that could indicate that the child had CP. We also examined medical charts of children from the neuropediatric department to identify whether any children had a CP diagnosis and could not identify any new patients with CP. The fact that 7% of the medical records could not be located demonstrates a weakness of the hospital’s non-electronic medical chart archive system. This supports the advantage for functioning national databases in order to adequately follow-up regarding the outcomes of these patients. The literature strongly supports the effectiveness of specifically designed follow-up programs for the prevention of hip dislocation in children with CP[8,15,16].
There is always a risk of information bias. In this study, data could be misclassified according to CP subtype, GMFCS level, and type of surgery. To lessen the impact of misclassification, we searched the entire medical chart including radiographs. We did not analyze change in functional level over time for these children. However, the children’s rehabilitation doctors also confirmed GMFCS level and CP-subtype recorded in the medical charts.
The orthopedic care of children with CP in Uruguay is carried out by both public and private institutions with approximately 50% of all orthopedic surgeries in children with CP performed at the public pediatric university hospital in Uruguay, the location of this study. There is a potential for random error due to the fact that some children might have been operated at other hospitals in Uruguay. We did not find any indication of this occurring in the medical charts. However, there is always the possibility that the children subsequently had orthopedic surgery in another hospitals outside Montevideo or changed to private health care or were transferred to an adult hospital at the age of 15 years. In this study, we did not have access to the medical charts of other hospitals. The mortality during childhood is high in GMFCS level V[17] and this is another random error that we could not adjust for in our analysis, as we could not confirm whether some of the children died during the study period.
Spasticity reduction treatment might in some cases postpone surgery[18] and we did not look at these potential confounders. Children with CP in Uruguay have limited access to botulinum toxin and selective dorsal rhizotomy. However, the access to gait analysis and spasticity reduction treatment in the form of oral Baclofen, regular physiotherapy and orthotic devices probably increased over the study period with the increased availability of rehabilitation centers like Teleton and increased resources in the health care system due to economic growth in Uruguay during the past 15 years. For example, the number of soft tissue surgeries in the lower limb to correct foot equinus might be affected by this as well as by a change in surgical technique over time.
Many co-variables beyond a patient's age and their functional level influence decision making for surgery. For example, surgical technique, accepted indications, and co-morbidities of the child. However, analyzing the different indication for surgery was beyond the scope of this paper. The indication for surgery changes over time and in the beginning of the study period very few patients had spine surgery partly due to a belief that the risk of major complication was too high. The Uruguayan health system has also changed during the study period and a higher proportion of children with CP in Uruguay are probably operated today in other non-public hospitals.
Despite these limitations this study had numerous strengths. To the best of our knowledge, this is the first study to describe the frequency of different orthopedic surgical procedures in children with CP in relation to GMFCS level and age group. It is also the first study to report the frequency of orthopedic surgical procedures performed in children with CP at a public University Clinic in Uruguay. Another strength is that the number of children in this study is large and the surgical procedures were confirmed by medical chart reviews.
In conclusion, these results suggest that children with GMFCS level I have significantly fewer surgeries than children with a more limited ability to ambulate but the frequency of surgical procedures per child did not increase with higher GMFCS level after level I. However, the proportion of soft tissue surgery was higher in GMFCS levels I-III compared to IV-V. Even though each individual’s condition is unique in children with CP, information from this study may help to predict future orthopedic surgical interventions based on the GMFCS level and age and can be useful as a basis for comparison for future studies.
Little is known about the frequency of different types of orthopedic surgery in children with cerebral palsy (CP), particularly in Latin America.
The aim of this retrospective cohort study was to analyze the frequency, anatomic location, and type of orthopedic surgical procedures in relation to age and gross motor function classification (GMFCS) in children with CP in a public university hospital providing care to children of lower socioeconomic status.
We hypothesized that the frequency of surgical procedures per child would increase with higher GMFCS level. Information from this study may help to predict future orthopedic surgical interventions based on the GMFCS level and age and can be useful as a basis for comparison for future studies.
This retrospective study included all children with CP (n = 245) treated with elective orthopedic surgery at a Uruguayan university hospital between October 2010 and May 2016 identified from a surgical database. Demographics, GMFCS, and orthopedic surgeries were obtained from the medical records of 227 children.
This study examined surgical procedures among children with CP, with a total of 711 surgical procedures performed between 1998 and 2016. On average, children had 3.1 surgical procedures and no differences existed regarding age at first surgery. The most common procedures were: lower leg soft tissue surgery, hip tenotomy, and hamstring tenotomy. For children with GMFCS level I the mean number of surgeries per child differed significantly with children with GMFCS levels II, III, IV and V. Within II, III, IV, and V there was not a significantly significant difference of mean number of surgeries per child when comparing across the groups. The proportion of soft tissue surgery vs bone surgery was significantly higher in GMFCS levels I-III, compared to levels IV and V. This study provides a rich description of orthopedic procedures performed in children with CP. However, we do not know the prevalence of surgery in all patients with CP.
This is to our knowledge the first study to describe the frequency of different orthopedic surgical procedures in children with CP in relation to GMFCS level and age group. Our hypothesis that the frequency of surgical procedures per child would increase with higher GMFCS level could not be confirmed with our data, as the frequency of surgical procedures per child did not increase with higher GMFCS level after level I. This result could partly be explained by the indication and goal of the surgery in an ambulatory child which is to improve gait, compared to the goal of surgery in a non-ambulatory child where the goal is often related to pain relief, greater comfort with positioning, improved basic care, correction of severe foot deformities, prevention of hip dislocation, and/or to halt scoliosis progression. Additionally, the benefit of surgery in non-ambulatory children needs to be judged against the increased risk of major complications due to the presence of comorbidities. There is also an increased risk of complications from surgery.
Few studies describe the panorama of different surgical procedures used in an entire population of children with CP or investigate differences in orthopedic surgical treatment between different CP-subtypes.
We thank Professor Maura Daly Iversen for using her expertise in biostatistical analysis to review the final statistical methods used in the study. We thank Dr Magdalena Cibils and Dr Claudia Gonzalez for their contribution to the research.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Uruguay
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emara KM S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Liu MY
| 1. | Himmelmann K. Epidemiology of cerebral palsy. Handb Clin Neurol. 2013;111:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214-223. [PubMed] |
| 3. | Rackauskaite G, Uldall PW, Bech BH, Østergaard JR. Management of cerebral palsy varies by healthcare region. Dan Med J. 2015;62:A5152. [PubMed] |
| 4. | Sharan D. Orthopedic surgery in cerebral palsy: Instructional course lecture. Indian J Orthop. 2017;51:240-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Miller F. Cerebral palsy. New York: Springer-Verlag, 2005. |
| 6. | Hägglund G, Wagner P. Development of spasticity with age in a total population of children with cerebral palsy. BMC Musculoskelet Disord. 2008;9:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet. 2014;383:1240-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 363] [Article Influence: 33.0] [Reference Citation Analysis (1)] |
| 8. | Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J. 2014;96-B:1546-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 182] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 9. | Parkinson KN, Gibson L, Dickinson HO, Colver AF. Pain in children with cerebral palsy: a cross-sectional multicentre European study. Acta Paediatr. 2010;99:446-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | McGinley JL, Dobson F, Ganeshalingam R, Shore BJ, Rutz E, Graham HK. Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2012;54:117-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 139] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 11. | Yu S, Rethlefsen SA, Wren TA, Kay RM. Long-term ambulatory change after lower extremity orthopaedic surgery in children with cerebral palsy: a retrospective review. J Pediatr Orthop. 2015;35:285-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Gainsborough M, Surman G, Maestri G, Colver A, Cans C. Validity and reliability of the guidelines of the surveillance of cerebral palsy in Europe for the classification of cerebral palsy. Dev Med Child Neurol. 2008;50:828-831. [PubMed] |
| 13. | Presedo A, Oh CW, Dabney KW, Miller F. Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J Bone Joint Surg Am. 2005;87:832-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Samdani AF, Belin EJ, Bennett JT, Miyanji F, Pahys JM, Shah SA, Newton PO, Betz RR, Cahill PJ, Sponseller PD. Major perioperative complications after spine surgery in patients with cerebral palsy: assessment of risk factors. Eur Spine J. 2016;25:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Elkamil AI, Andersen GL, Hägglund G, Lamvik T, Skranes J, Vik T. Prevalence of hip dislocation among children with cerebral palsy in regions with and without a surveillance programme: a cross sectional study in Sweden and Norway. BMC Musculoskelet Disord. 2011;12:284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Kentish M, Wynter M, Snape N, Boyd R. Five-year outcome of state-wide hip surveillance of children and adolescents with cerebral palsy. J Pediatr Rehabil Med. 2011;4:205-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Westbom L, Bergstrand L, Wagner P, Nordmark E. Survival at 19 years of age in a total population of children and young people with cerebral palsy. Dev Med Child Neurol. 2011;53:808-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Heinen F, Desloovere K, Schroeder AS, Berweck S, Borggraefe I, van Campenhout A, Andersen GL, Aydin R, Becher JG, Bernert G, Caballero IM, Carr L, Valayer EC, Desiato MT, Fairhurst C, Filipetti P, Hassink RI, Hustedt U, Jozwiak M, Kocer SI, Kolanowski E, Krägeloh-Mann I, Kutlay S, Mäenpää H, Mall V, McArthur P, Morel E, Papavassiliou A, Pascual-Pascual I, Pedersen SA, Plasschaert FS, van der Ploeg I, Remy-Neris O, Renders A, Di Rosa G, Steinlin M, Tedroff K, Valls JV, Viehweger E, Molenaers G. The updated European Consensus 2009 on the use of Botulinum toxin for children with cerebral palsy. Eur J Paediatr Neurol. 2010;14:45-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |