Published online Feb 18, 2020. doi: 10.5312/wjo.v11.i2.107
Peer-review started: October 3, 2019
First decision: October 13, 2019
Revised: October 15, 2019
Accepted: November 28, 2019
Article in press: November 28, 2019
Published online: February 18, 2020
Processing time: 138 Days and 18.6 Hours
Airborne sports have become more popular in recent years. The number of accidents has increased linearly as athletes take increasingly greater risks to experience the adventurous spirit of this kind of sports.
To investigate the variety of injuries in airborne sport accidents, as well as which acute treatment these patients receive, both before and after admission to a level-one-trauma center.
We performed a retrospective chart analysis at a major level-one-trauma center in Switzerland for 235-patients who were admitted following airborne sports injuries between 2010 and 2017. Patients’ demographic data, injury patterns, emergency primary care procedures and intra-hospital care were recorded.
Overall, 718-injuries in 235-patients were identified; the spine was the most commonly affected region with 46.5% of injuries (n = 334/718) in 143-patients. In 69-patients (15.5%), the (non-spine) thorax was affected, followed by the lower and upper extremity, pelvis, head/face and abdominal injuries. Eleven-patients had to be intubated at the trauma site. Three patients were resuscitated after onset of pulseless-electrical-activity. Two-patients died in the resuscitation room. In 116-cases, surgery was indicated including 55-emergency surgeries. Another 19 patients (8.1%) were transferred to the intensive care unit.
Paragliders are most commonly affected, although the highest injury severities were identified for Building, Antenna, Span and Earth-jumping athletes. First responders, treating physicians and pilots should be aware of the risk for potentially serious and life-threatening injury with an in-hospital mortality of 0.9%.
Core tip: We describe the different severities and types of injuries in individual airborne sports in one cohort. This study will improve the pre- and intra-/hospital management especially in the emergency department to accelerate and simplify the diagnostics and allow prompt and early initiation of the treatment. Furthermore, pilots will be more aware of injuries and injury patterns, which may help to develop new prevention programs.
- Citation: Bäcker HC, Vosseller JT, Exadaktylos AK, Perka C, Benneker LM, Krause FG, Deml MC. Epidemiology and injury patterns of aerial sports in Switzerland. World J Orthop 2020; 11(2): 107-115
- URL: https://www.wjgnet.com/2218-5836/full/v11/i2/107.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i2.107
Due to Switzerland’s mountainous landscape, many different airborne sports [Paragliding, skydiving, Building, Antenna, Span and Earth (BASE)-jumping, Delta flying and speed flying] are commonly performed. One of the most popular and famous venues for these sports is Lauterbrunnen (Berne, Switzerland), where about 15000 jumps and flights are performed annually[1].
The most common airborne sport in Switzerland is paragliding, a sport that requires a delicate and deft touch to maintain appropriate balance even in calm conditions. Paragliding can become exponentially less safe and more difficult in more turbulent weather conditions. Due to its popularity in Switzerland, the Swiss Paragliding Association was established in 1974 with about 15200 members currently registered[2]. Paragliding is responsible for the highest number of injuries amongst these types of sports, especially during the launching and landing phase with mortality rates up to 22% described. In Switzerland, 13.7% of paragliding pilots were severely injured (54/398) when performing paragliding between 2013 and 2017[2-4]. Spine injuries are the most commonly reported injuries, followed by talus and calcaneus fractures[1,5]. Other extreme sports include skydiving, BASE jumping, parachuting and Speed flying. In skydiving approximately 5.5 million jumps in over 40 countries were recorded in 2009. In BASE jumping pilots require a wingsuit, which can aerodynamically be controlled by the body, and a parachute for landing[6,7]. Speed flying on the other hand is comparable to paragliding where pilots try to keep up in the air as long as possible with a high risk of severe injuries due to higher speed[8,9]. The orthopaedic and trauma literature have a relative dearth of information on injuries that can result from these extreme sports.
Therefore, the aim of this study is to investigate (1) the pre- and in-trauma-center management of these potentially high impact injuries; (2) the severity of injuries based on the injury severity score; and (3) the different injury patterns according to the different types of airborne sports.
After local ethic approval, we performed a retrospective chart analysis on all patients admitted to a single trauma-center between February 2010 and May 2017. Our emergency department database was searched for airborne sport injuries. Patients who got re-admitted because of a complication after primary treatment in another center or abroad were excluded from this study.
The emergency department at our university hospital is a level I trauma center with a commuter area of about 1.5 million people. Approximately 45000 trauma patients are treated there every year. The database provides information on basic demographics, the means of admission (i.e., ambulance, air ambulance or self-admission) and in hospital acute care unit (such as resuscitation room or normal emergency department), diagnosis and co-morbidities, status of consciousness (GCS-Score), primary/secondary survey according to advanced traumatic life support protocol, as well as diagnostics performed. The short-term outcome was recorded by further procedures performed (discharged/outpatient, inpatient, transferred to intensive care unit (ICU), emergency surgery, early elective surgery or no surgical procedures).
To classify the injury severities, we used the injury severity score (ISS)[10]. Therefore, the injuries were summarized according their location to upper and lower extremity, thoracic, abdominal trauma, spine, pelvis and head/face injuries using the abbreviated injury codes as has been done previously[11]. All data are presented in absolute numbers and percentages.
We used Microsoft Excel spreadsheet and Origin Lab, using a t-test for mean and standard deviation for all calculations and graphs. Statistical significances are expressed as P < 0.05, P < 0.01 and P < 0.005.
A total of 237 patients suffering from airborne injuries were admitted to the emergency department between February 2010 and June 2017. Two patients were readmitted due to complications after the previous hospitalization. These patients were excluded due to missing acute trauma care data, leaving 235. In most cases paragliding (n = 192; 82.6%; including 13 tandem-Paraglider) was the cause of injury, followed by BASE-jumping (n = 25), skydiving (n = 10; one tandem-skydiver), speed flying (n = 4) and finally Delta flying (n = 2) as shown in Table 1. The mean age was 38.7 years (Min/Max 18 - 74) with a predominance in male 198 (84.3%) patients and a mean injury severity score of 16.5 (SD 14, range from 0 to 75). However, this varied according to the airborne sport performed. For BASE-jumping the ISS was higher although no significance was identified (P = 0.1).
| Overall | Paragliding | BASE-jumping | Skydiving | Delta flying | Speed flying | |
| Total numbers | 235 (100) | 194 (82.6) | 25 (10.6) | 10 (4.2) | 2 (0.9) | 4 (1.7) |
| Male | 198 (84.3) | 162 (83.5) | 23 (92) | 9 (90) | 2 (100) | 2 (50) |
| Injury severity score, n (SD) | 16.5 (14.0) | 16.0 (13.9) | 21.1 (13.9) | 13.3 (15.2) | 18 (14) | 19.75 (8.8) |
| Age (yr, range) | 38.7 (18-74) | 39.8 (18-74) | 30.8 (21-45) | 37.2 (20-59) | 51 (49-53) | 33.3 (27-45) |
| Air rescue | 155 (67.0) | 129 (66.5) | 19 (76.0) | 2 (20.0) | 1 (50) | 4 (100) |
| Ambulance | 6 (2.6) | 5 (2.6) | 1 (4.0) | - | - | |
| Self-admission | 28 (11.9) | 21 (10.8) | 1 (4.0) | 5 (50.0) | 1 (50) | - |
| Transferred from other hospitals | 44 (18.7) | 37 (19.1) | 4 (16.0) | 3 (30.0) | - | - |
| Not otherwise specified | 2 (0.9) | 2 (1.0) | - | - | - | - |
| Resuscitation room | 162 (68.9) | 133 (68.6) | 21 (84.0) | 3 (30.0) | 1 (50) | 4 (100) |
| Normal trauma ward | 72 (30.6) | 60 (30.9) | 4 (16.0) | 7 (70.0) | 1 (50) | - |
| Not otherwise specified | 1 (0.4) | 1 (0.5) | - | - | - | - |
In total, 11 patients had to be intubated at the trauma site by the prehospital emergency physician (4.7%). One hundred fifty-five patients (67.0%) were admitted by air rescue. Sixty-two of these patients’ (68.9%) primary diagnostics were performed in the resuscitation room and in three cases a manual resuscitation was required due to onset of a pulseless electrical activity. Two of these patients died. One had a severe pelvis fracture, femoral fracture with liver laceration and haemo-pneumothorax, whereas the other patient suffered from a severe cranio-cerebral injury. In both cases, only whole body low dose X-ray was performed without a computed tomography. The overall intra-hospital mortality in our cohort was 0.9%. Our database does not include the pre-hospital mortality. All details of the type of admission and airborne sport details are summarized in Table 1.
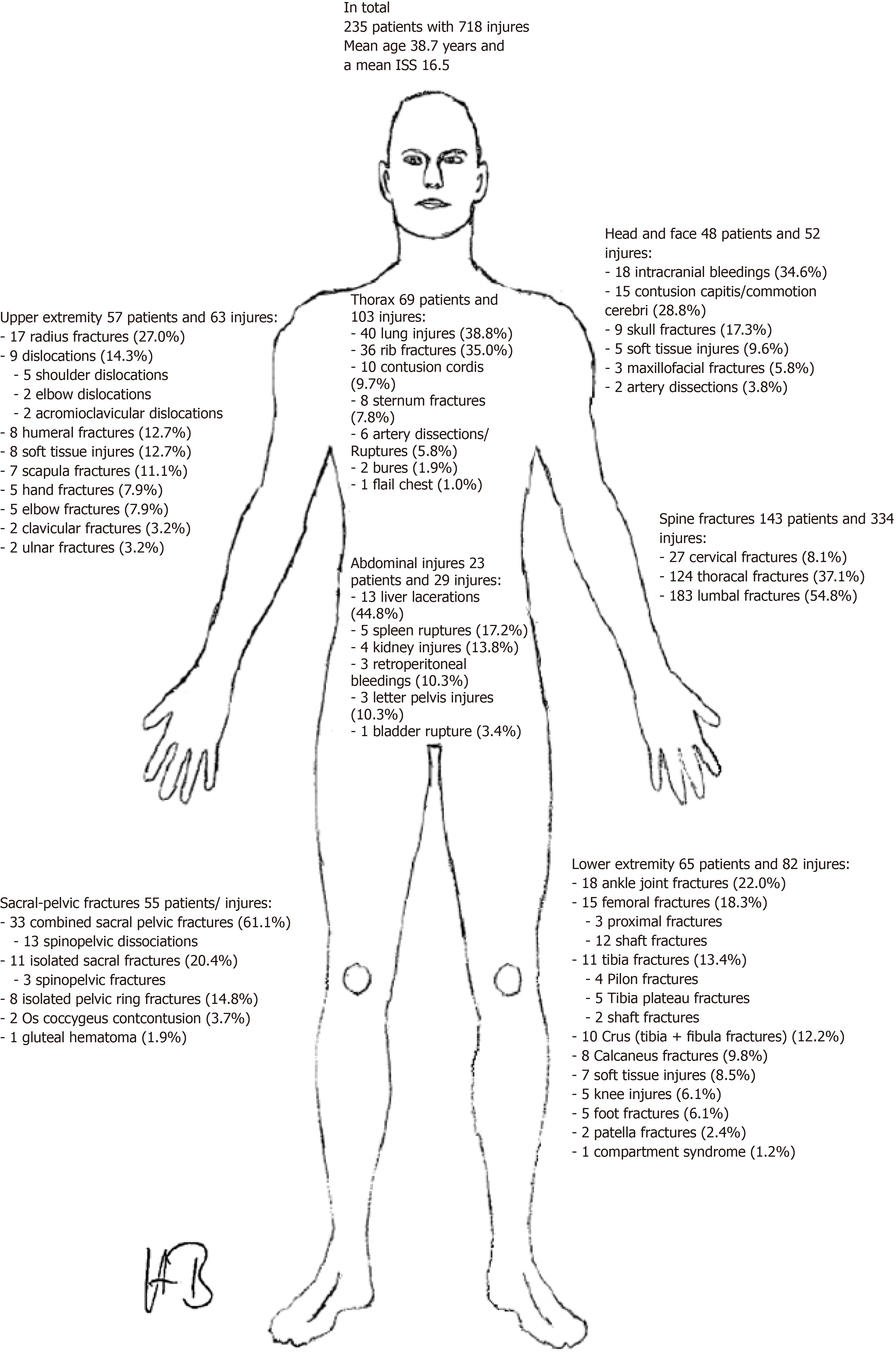
Two hundred thirty-five patients suffered 718 injuries (mean 2.8 injuries/per patient). The most commonly affected location was the spine within 143 patients (143/235, or 60.9%) and in total 334 individual spine injuries (334/718, or 46.5%), followed in incidence by thorax injuries (69/235, or 29.4%). The most commonly affected vertebral body was L1 (68/334, or 20.4%), followed by L2 (47/334, or 14.1%). Neurologic impairment was identified in 31 patients accompanied by spinal injury (31/143, or 21.7%); seven type A, two type B, seven type C (including cauda equina syndrome), 15 type D according to ASIA grading. Most injuries were defined as serious with a mean abbreviated injury code of 2.77. In patients who suffered from thorax injuries the most commonly affected organ was the lung – including lung laceration, lung contusion or edema (32/69, or 46.4%), followed by rib fractures (17/69, or 24.6%). Fifteen subjects suffered from cardiac contusion, sternum fracture, or thoracic skin burning. With respect to abdominal injuries (23/235, or 9.8%), the most common injured organ was the liver (11 cases (47.8%). Other abdominal organs were less commonly damaged (Figure 1). For ISS both thorax and abdomen were serious, although the mean code was higher for abdomen with 3.18 than thoracic with 3.04.
The extremities were injured at a high rate as well, with 122 (51.9%) patients in total. The lower extremity (65/235, or 27.7%) had a few more injuries than the upper extremity (57/235, or 24.3%). The ankles were the most commonly fractured individual part of the extremities (16/122, or 13.1%), followed by femoral fractures in 15 (12.3%) patients. Four (3.3%) patients suffered from combined fractures of the lower extremity. The individual types of injuries are summarized in Figure 1. All injuries were defined as moderate with an abbreviated injury codes (AIC) of 2.09 for the upper and 2.34 for the lower extremities.
The sacrum and pelvis were fractured in 52 cases. Most of the injuries were combined sacro-pelvic fractures (33/52, or 63.5%), followed by isolated sacral (11/52, or 21.2%) and pelvic fractures (8/52, or 15.4%). Hereby, the highest AIC was observed among all locations with severe injuries and a mean AIC of 3.52. Finally, when looking at the face and head trauma we observed 48 patients (48/235, or 20.4%) with 52 injuries. The most common type of injuries were intracranial bleeds which occurred in 16 patients (16/48, or 33.3%), followed by concussions (15/48, or 31.3%). Skull fractures were present in nine patients (18.8%). The mean AIC was 2.57 and therefore defined as serious. All individual injuries and the percentages are summarized in Figure 1. Table 2 and Table 3 gives an overview of the distribution of injuries according to the different airborne sports, respectively the abbreviated injury codes among location of injuries.
| Total | Spine | Extremity | Sacro/pelvis | Abdomen | Thorax | Head/face | |
| Paragliding | 532 (74.1) | 274 (51.5) | 92 (17.3) | 41 (7.7) | 22 (4.1) | 66 (12.4) | 37 (7.0) |
| BASE-jumping | 134 (18.7) | 48 (35.8) | 33 (24.6) | 12 (9.0) | 5 (3.7) | 26 (19.4) | 10 (7.5) |
| Parachuting | 20 (2.8) | 1 (5) | 10 (50) | 2 (10) | 1 (5) | 2 (10) | 4 (20) |
| Speedflying | 24 (3.3) | 11 (45.8) | 2 (8.3) | - | 1 (4.2) | 9 (37.5) | 1 (4.2) |
| Delta | 8 (1.1) | - | 8 (100) | - | - | - | - |
| Total | 718 (100) | 334 (46.5) | 145 (20.2) | 55 (7.7) | 29 (4.0) | 103 (14.4) | 52 (7.2) |
| Mean | 1 -minor | 2 - moderate | 3 - serious | 4 - severe | 5 - critical | 6 - maximal | Not within 3 most severe AIC | Total | |
| Head/face | 2.57 | 10 | 13 | 13 | 8 | 1 | 1 | 2 | 48 |
| Thoracic | 3.04 | 3 | 17 | 28 | 12 | 7 | 0 | 2 | 69 |
| Abdomen | 3.18 | 1 | 2 | 7 | 7 | 0 | 0 | 6 | 23 |
| Spine | 2.77 | 24 | 36 | 28 | 48 | 2 | 0 | 5 | 143 |
| Pelvis | 3.52 | 3 | 8 | 16 | 8 | 13 | 2 | 5 | 55 |
| Upper extremity | 2.09 | 7 | 29 | 11 | 0 | 0 | 0 | 10 | 57 |
| Lower extremity | 2.34 | 16 | 16 | 23 | 7 | 0 | 0 | 3 | 65 |
After performing the primary assessment at the emergency department, 15 chest tubes and three invasive intracranial pressure sensors were inserted in the resuscitation room. Emergency surgery was immediately indicated in 55 patients (55/235, or 23.4%, Table 4). Sixty-one patients (61/235, or 26.0%) underwent surgery in the following days. Nineteen patients were transferred to the intensive care unit (19/235, or 8.1%), in addition to 55 patients who underwent emergency surgery and were observed in the intensive care unit (55/235, or 23.4%). Furthermore, 111 patients were hospitalized on the general ward (111/235, or 47.2%) and in total, 47 patients were treated as outpatient (47/235, or 20%) and were discharged from the emergency department within 24 hours. In terms of injury severity score, the ISS was significantly higher for the emergency surgery group (22.9) and the intensive care unit group (24.8) compared to all other patients (13.3; both P < 0.005).
| Emergency surgeries | Procedure | |
| Total | 55 (100) | |
| Extremities | 18 (32.7) | 10 external fixations, 4 plate osteosynthesis, 4 internal fixations with intramedullar nail |
| Open fractures | 12 | |
| Closed fractures | 6 | |
| Spine surgery | 23 (41.8) | 16 decompressions and pedicle screw fixation, 7 percutaneous stabilizations |
| With neurology | 16 (69.6) | |
| Without neurology | 7 (30.4) | |
| Pelvic fixation | 7 (12.7), including one with Urinary bladder rupture | 7 plate osteosynthesis and in one case direct suturing of the bladder |
| Vascular surgery | 3 (5.5) | 2 arterial bypasses, 1 coronary artery angiography |
| Others (visceral, plastic, neuro, maxillo fascial) | 4 (7.3), each 1 | 1 explorative laparotomy, 1 debridement (after burn), 1 cerebral decompression, 1 maxillofacial fixation |
| Additionally interventions | 15 thoracic trauma, 3 cerebral trauma | 15 thoracic drainages, 3 ICP probe insertion |
For the patients who were transferred from the resuscitation room to the operating room it took 2:34 h in mean respectively 4:18 h to the ICU.
In the literature, the mortality rate was found to be approximately 45/100000 paragliding jumps[12] with one fatality in every 2317 BASE-jumps of which all deaths occurred on the scene and were not admitted to a hospital[13]. Since January 2013, all deaths of pilots who crashed during paragliding are reported to the Swiss Paragliding Association. Less severe injuries from paragliding incidents are reported by the pilots on a voluntary basis, and so it is very possible that the real incidence of injury is even higher than is recognized here. Furthermore, no equivalent register for skydiving, BASE-jumping, speed flying or Delta flying exists[2]. From about 15000 members of the Swiss paragliding association only 398 pilots reported an accident while paragliding between 2013 and 2017. Most of them had no injury (128/398, or 32.2%), while one third had severe injuries (125/398, or 31.4%). Unfortunately, there were 54 fatalities from paragliding over this time period[2]. The ’BFU – Swiss Council for Accident Prevention’ has given a total number of 132 flying sports related deaths from 2010 to 2016 for the whole of Switzerland with a mean of 19 patients per year. In 2015 eight pilots died when paragliding, and three when skydiving[14]. However, this data is not stratified regionally, thus we cannot correlate these data to our regional data. In our cohort, the overall intra-hospital mortality was 0.9% (n = 2; both paraglider), although our database does not include the pre-hospital mortality. Three patients had to be resuscitated due to onset of a pulseless electrical activity; only one survived.
Regarding the severity of injury related to the different sports, the most severe injuries were identified in BASE-jumping athletes as assessed by the injury severity score, followed by speed FLYING, Delta flying and paragliding. Our data show that less severe injuries are related to Skydiving among the cohort that was admitted alive to the hospital, although only ten patients were skydiving at the time of injury. For location, the pelvis was at greatest risk followed by the abdomen and thorax, which showed the highest abbreviated injury codes.
Emergency surgery and/or transfer to the intensive care unit was necessary in 55 cases (23.4%). In those patients who suffered from pelvis fractures, plate fixation was performed as all of them were medically stable. After adequate surveillance, 47 patients were treated as outpatient (20%) and were discharged within 24 h. It took a mean 2:34 h to transfer the patients from the resuscitation room to the operating room versus 4:18 h to the ICU. According to the German Trauma society register, in 2016, the mean time between initial assessment and emergency surgery was slightly higher in our center, compared with the average time in German clinics (1:14 h ± 0:59 h), likewise the transfer from the resuscitation room to the intensive care unit (1:22 h ± 1:12 h)[15].
This study also shows the importance of the prehospital management in assessing and treating the most severe, life-threatening injuries. Overall, 11 patients were intubated at the site of the accident. There is a well-established air rescue system with an emergency physician on board in Switzerland, which allows early rescue and admission to the hospital while providing maximal pre-hospital treatment, which potentially increases the survival rate. However, according to the air rescue database, only a small percentage (4.9%, or 544/11,055 in 2016) of helicopter missions in total are related to traumatic injuries. This emergency rescue setting may also explain a far lower death rate compared to data from another country (22%)[4,16]. In our subjects, more than half of the cases – 67.0% - were admitted by air ambulance and most patients got admitted through the resuscitation room – 68.9% - to avoid any delay for primary diagnostics and early onset of treatment according to advanced traumatic life support guidelines.
Comparing the injury patterns with those published in the literature, we see that the spine is by far more often affected in our cohort - especially paragliding (51.5%) and speed flying pilots (45.8%)[17,18]. The second most common location was the thorax, followed by the lower extremity. This difference may be related to the fact that skydivers usually hang in the parachute, whereas paragliders sit and most of the cases in our cohort were paragliders (82.6%). Ball et al[18] reported in their cohort, that the lower extremity was affected most (65%) followed by the head (22%) and spine (22%). This orientation of the body may also explain the high incidence of sacral-pelvic injuries due to the higher percentage of paragliders in our cohort compared to others[18]. Interestingly, in previous reports, injuries in those who performed BASE-jumping and survived were generally minor from a musculoskeletal perspective, including sprained ankles or knees, with only few moderate injuries, although concussions were common[13,19]. Delta flyers suffer more from extremity injuries (100%). In parachuting the extremities (50%) are affected most, followed by the highest percentage of head and face injuries (20%). Our data show a shift towards more spine injuries than extremity injuries compared with the pre-existing literature[1].
Compared to other high energy trauma, like motorcycle injuries, the mean age in our group is slightly younger, 38.7 years versus 40.5 years from an historical cohort. The mean ISS is by far lower in an historical motorcycle injury cohort, 7.7 ± 6.7 vs 16.5 ± 14.0 and the most common types of injuries are rib fractures and maxillofacial trauma (2.5%, respectively 11.6%) according to Liang et al[20]. Rust et al[21] assessed the injury patterns of snowboarders and described that especially the lower and upper extremities are at risk, which include anterior cruciate ligament tears, distal radius fractures and knee sprains. Closed head injury is less likely, whereas only few lumbar strains without fractures were reported[21]. These injuries stand in contradistinction to those seen in airborne sports which affected mainly the spine with pelvis and lumbosacral junction and the thorax followed by extremities.
In the literature few publications on vascular injuries such as rupture or dissection exist – mainly as case reports[22], however according to our data it may be more common than suspected. In total, we identified eight vascular injuries – two dissections of the cranial vessels (vertebral artery, carotid artery), four aortic ruptures or dissections and one coronary artery dissection, combining for an incidence of 3.4%. This relatively high incidence may also be due to the strict full body computed tomography-scan done in high ISS-Scores, which has not historically been done.
When looking for the causes of paragliding injuries, about 53.5% are related to pilot errors, followed by weather conditions in 10.1%[23]. As the paragliding parachute is fragile, it may collapse and it is difficult to re-inflate and re-balance. In paragliding most common injuries occur during take-off which includes the running and inflation phase (35.1%) or landing (48.7%)[24,25]. Likewise in skydiving where a proper landing technique is pivotal to avoid injuries[18].
As Westman et al[17] stated for skydiving, general instructions for students to activate reserve parachutes should be given, even though in paragliding this may not help in most cases as most injuries occur during the start and landing phase from less height. In addition, training courses and special gliders (wider ones, which allow more stability) should be provided for beginners and for intermediate. To reduce the incidence of pelvic and sacral injuries, harnesses have become safer over time, due to new robust, replaceable Polyvinyl plastics as a protector. Once an accident has occurred, one of the most important parts in mitigating injury seems to be the level in life support training of the first responder, to identify severe injuries and reduce the risk of further complications from unnecessary or inappropriate movement.
Shortcomings of this study are the retrospective, descriptive study design and the focus on patients who were admitted to the emergency department of a level-one-trauma-center. Patients with mono-trauma or less severe injuries may present to the general practitioner or were admitted to smaller hospitals, which therefore may be missed in our study. We are also not able to report the overall mortality, as some patients died before admission to the hospital. Furthermore, no information is given about the long-term survival rate and treatment outcome of severely injured patients presented in this cohort.
In conclusion, this study shows the clinical impact and severity of airborne injuries. In total, 235 patients suffered from paragliding, speed flying, Delta flying, skydiving or BASE-jumping injuries with a total of 718 injuries. More than half of the patients were admitted by the air ambulance and through the resuscitation room. Contrary to the literature, not the lower extremities but the spine and thorax were most commonly affected in our cohort. The overall intra-hospital mortality was 0.9%. Optimal treatment likely involves both maximizing safety on the front end to decrease the incidence of injury and continued vigilance to swiftly treat those that do get injured in order to minimize morbidity and mortality.
Airborne sports are becoming more popular in recent years especially in Switzerland due to its landscape.
The number of accidents has increased linearly with the increased popularity as athletes take increasingly greater risks to experience the adventurous spirit of the sport. To assess potential changes in injury patterns over the years due to different trends and changes sports men mentalities.
Our purpose was to investigate the variety of injuries in airborne sport accidents, as well as what acute treatment these patients receive, both before and after admission to a trauma center.
We performed a retrospective chart analysis at a major level-one-trauma center in Switzerland for patients who were admitted due to airborne injury between 2010 and 2017.
A total of 237-patients were admitted to our center, having suffered an airborne sport accident. Two patients were excluded as they were a readmission from a previous injury. Overall, 718-injuries in 235-patients were identified; the spine was the most commonly affected region with 46.5% of injuries (n = 334/718) in 143-patients. In 69-patients (15.5%) the (non-spine) thorax was affected, followed by the lower and upper extremity, pelvis, head/face and abdominal injuries. Eleven patients had to be intubated at the trauma site, three patients were resuscitated after onset of pulseless-electrical-activity. Two-patients died in the resuscitation room. In 116-cases, surgery was indicated including 55 emergency surgeries. Other 19-patients (8.1%) were transferred to the intensive care unit.
There is a high potential for serious and sometimes life-threatening injuries in airborne sports. Contrary to the current literature, the spine was the most commonly affected body region in our cohort and not lower extremities as cited before.
Athletes, as well as first responders and ultimately the treating physicians, must be aware of the risk for potentially serious injury.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Switzerland
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Llompart-Pou JA, Ju SQ S-Editor: Wang JL L-Editor: A E-Editor: Liu MY
| 1. | Hasler RM, Hüttner HE, Keel MJ, Durrer B, Zimmermann H, Exadaktylos AK, Benneker LM. Spinal and pelvic injuries in airborne sports: a retrospective analysis from a major Swiss trauma centre. Injury. 2012;43:440-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Stocker B. Schweizerischer Hängegleiter-Verband. Available from: Http://www.shv-fsvl.ch. |
| 3. | Schulze W, Richter J, Schulze B, Esenwein SA, Büttner-Janz K. Injury prophylaxis in paragliding. Br J Sports Med. 2002;36:365-369. [PubMed] |
| 4. | Canbek U, İmerci A, Akgün U, Yeşil M, Aydin A, Balci Y. Characteristics of injuries caused by paragliding accidents: A cross-sectional study. World J Emerg Med. 2015;6:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Gauler R, Moulin P, Koch HG, Wick L, Sauter B, Michel D, Knecht H. Paragliding accidents with spinal cord injury: 10 years' experience at a single institution. Spine (Phila Pa 1976). 2006;31:1125-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Riksinstruktören. Grundläggande bestämmelser in Swedish regulations for sport parachuting [SFF Bestämmelser Fallskärmsverksamhet; in Swedish]. Svenska Fallskärmsförbundet, 2011. |
| 7. | Laver L, Pengas IP, Mei-Dan O. Injuries in extreme sports. J Orthop Surg Res. 2017;12:59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Bisharat A. Why are so many BASE Jumpers Dying? Available from: https://www.nationalgeographic.com/adventure/features/why-are-so-many-base-jumpers-dying/. |
| 9. | Blake S. Speedflying in the Lake District. Suwanee: Publisher Services Inc, 1988. |
| 10. | Ebrahimi M, Pirazghandi H, Reihani HR. How is the injury severity scored? a brief review of scoring systems. Review Clin Med. 2015;42:125-128. [DOI] [Full Text] |
| 11. | Markogiannakis H, Sanidas E, Messaris E, Koutentakis D, Alpantaki K, Kafetzakis A, Tsiftsis D. Motor vehicle trauma: analysis of injury profiles by road-user category. Emerg Med J. 2006;23:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Fasching G, Schippinger G, Pretscher R. Paragliding accidents in remote areas. Wilderness Environ Med. 1997;8:129-133. [PubMed] |
| 13. | Soreide K, Ellingsen CL, Knutson V. How dangerous is BASE jumping? An analysis of adverse events in 20,850 jumps from the Kjerag Massif, Norway. J Trauma. 2007;62:1113-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Beratungsstelle für Unfallverhütung. Prevention b-SCfA. Fatalities, by type of sports group and residential location (accident location: Switzerland), 2012-2017 ed. Available from: https://www.bfu.ch/en. |
| 15. | Berlin GTSDaA. Annual report 2017 of the TR-DGU. Available from: http://www.traumaregister.de. |
| 16. | Rega. Rega missions 2001-2016. Available from: http://www.rega.ch/en/about-us/in-brief.aspx. |
| 17. | Westman A, Björnstig U. Injuries in Swedish skydiving. Br J Sports Med. 2007;41:356-64; discussion 364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Ball VL, Sutton JA, Hull A, Sinnott BA. Traumatic injury patterns associated with static line parachuting. Wilderness Environ Med. 2014;25:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Søreide K. The epidemiology of injury in bungee jumping, BASE jumping, and skydiving. Med Sport Sci. 2012;58:112-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 20. | Liang CC, Liu HT, Rau CS, Hsu SY, Hsieh HY, Hsieh CH. Motorcycle-related hospitalization of adolescents in a Level I trauma center in southern Taiwan: a cross-sectional study. BMC Pediatr. 2015;15:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Rust DA, Gilmore CJ, Treme G. Injury patterns at a large Western United States ski resort with and without snowboarders: the Taos experience. Am J Sports Med. 2013;41:652-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Go MR, Barbato JE, Dillavou ED, Gupta N, Rhee RY, Makaroun MS, Cho JS. Thoracic endovascular aortic repair for traumatic aortic transection. J Vasc Surg. 2007;46:928-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Feletti F, Goin J. Accidents and injuries related to powered paragliding: a cross-sectional study. BMJ Open. 2014;4:e005508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Rekand T. The epidemiology of injury in hang-gliding and paragliding. Med Sport Sci. 2012;58:44-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Zeller T, Billing A, Lob G. Injuries in paragliding. Int Orthop. 1992;16:255-259. [PubMed] |