Published online Nov 18, 2020. doi: 10.5312/wjo.v11.i11.507
Peer-review started: February 29, 2020
First decision: April 25, 2020
Revised: May 26, 2020
Accepted: September 1, 2020
Article in press: September 1, 2020
Published online: November 18, 2020
Processing time: 259 Days and 3.9 Hours
Müller-Weiss disease (MWD) is an idiopathic foot condition characterized by spontaneous tarsal “scaphoiditis” in adults. Frequently bilateral and affecting females during the 4th-6th decades of life, the pathogenesis of MWD remains unclear: It has been traditionally considered a spontaneous osteonecrosis of the navicular. The typical presentation of MWD is a long period of subtle discomfort followed by prolonged standing, atraumatic, disabling pain. Currently, there is no gold standard for the treatment of patients with MWD. Most support initial conservative therapy. Operative treatment should be considered for failure of conservative therapies longer than 6 months. The indication for surgery is severity of symptoms rather than severity of deformities. Operative treatment options include core decompression, internal fixation of the tarsal navicular, open or arthroscopic triple fusion, talo-navicular or talo-navicular-cuneiform arthrodesis, and navicular excision with reconstruction of the medial column.
In this study, we report four patients affected by MWD. Clinical and radiographic assessment, follow-up and treatment are reported.
As it is frequently misdiagnosed, MWD is challenging for orthopedic surgeons. Early diagnosis and effective treatment are mandatory to avoid sequelae.
Core tip: Müller-Weiss is a subtle disease of the foot, rarely described in the literature. This study describes four cases, examines in detail the etiopathogenesis reported in the literature and describes available treatments. We believe that these findings could assist orthopedic surgeons in the successful management of this foot disorder.
- Citation: Volpe A, Monestier L, Malara T, Riva G, La Barbera G, Surace MF. Müller-Weiss disease: Four case reports. World J Orthop 2020; 11(11): 507-515
- URL: https://www.wjgnet.com/2218-5836/full/v11/i11/507.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i11.507
Müller-Weiss disease (MWD) is a dysplasia of the tarsal navicular that develops during childhood and becomes symptomatic around the fifth decade. Although first reported by Schimdt in 1925, the disorder was described by Müller[1] in 1927 who proposed a relationship with forceful compression laterally and in the varus, and osteonecrosis of this tarsal bone. He proposed that the condition was due to a congenital defect. At the same time, Konrad Weiss described a similar disorder but suggested osteonecrosis as the cause for the condition[2]. Given the frequent misdiagnosis, affected patients by MWD are disabled for a very long time. Details of four cases and those found in the literature are described.
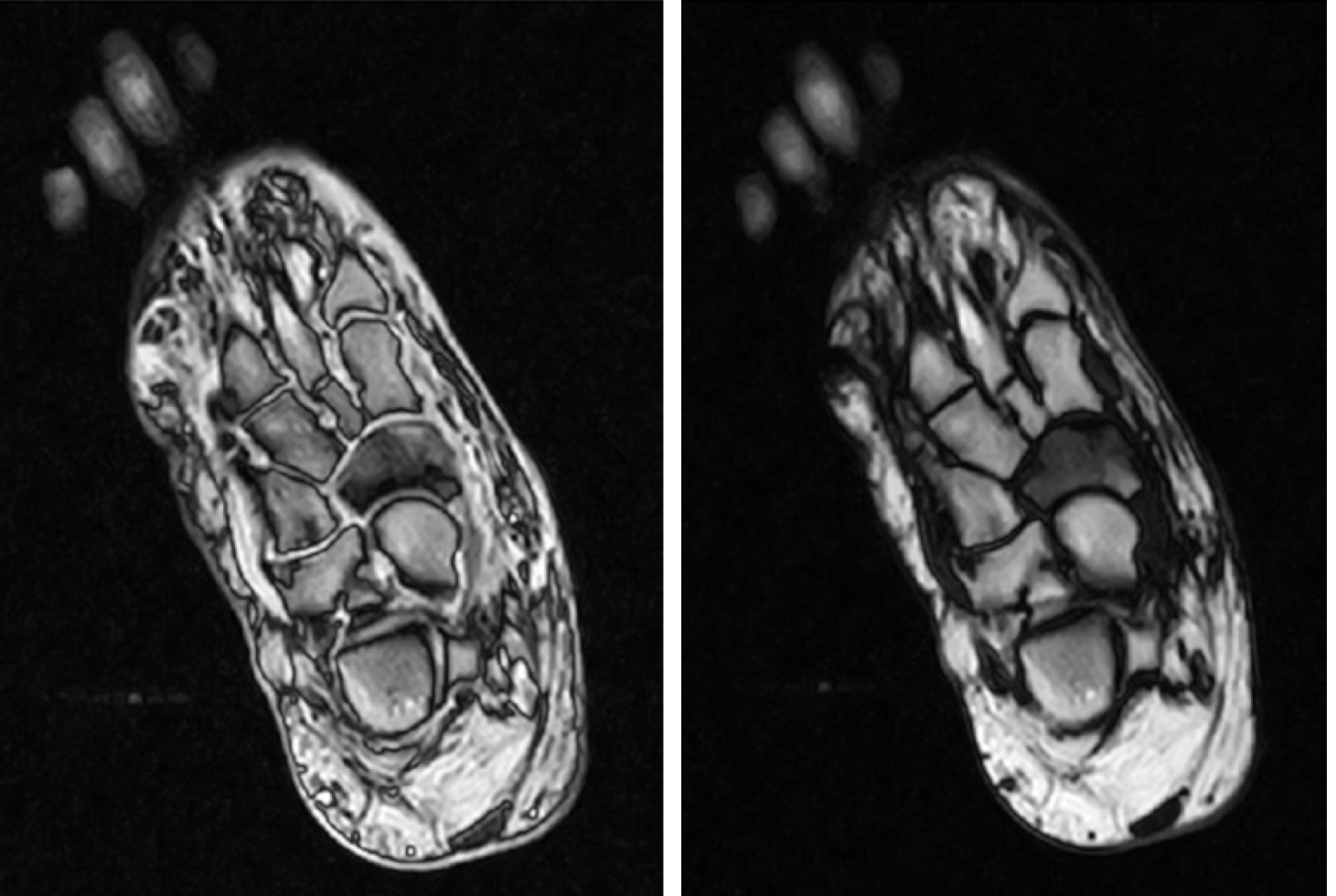
A 56-year-old female reported mild dorsomedial pain in the right midfoot, exacerbated by longstanding. The discomfort was initially managed only by nonsteroidal anti-inflammatory drugs (NSAIDs) (diclofenac, ibuprofen). Given her persistent pain, the patient decided to undergo our evaluation and tenderness and mild swelling over the dorsomedial aspect was assessed. She presented a plantigrade foot, slight range of motion (ROM) reduction of her ankle and normal hindfoot ROM [American Orthopedic Foot and Ankle Score (AOFAS) score 80/100]. Rx showed minimal arthritic deformity. Magnetic resonance imaging (MRI) demonstrated alteration of the navicular bone in both T1- and T2-weighted images (Figure 1).
A 63-year-old female reported dorsomedial pain in her left midfoot of two years duration. She could not go up and down stairs and needed a single crutch for long walks. There was no history of trauma. She occasionally took acetaminophen for pain. Prominence of the medial navicular and valgus hindfoot were evaluated. The patient had pain at palpation of the dorsomedial midfoot. Her AOFAS score was 59/100. MRI images demonstrated alteration and fragmentation of the navicular bone (Figure 2).
A 58-year-old male underwent arthrodesis of the left subtalar joint three years previously for posterior tibial tendon dysfunction. At post-operative follow-up, he reported severe limitation of daily and recreational activities due to persistent dorsal pain at the right ankle. He could only walk with two crutches. The foot was flat with a positive single-heel-raise test. A mild prominence at the talo-navicular joint was present and the ankle presented moderate restriction of dorsi-plantarflexion. His AOFAS score was 23/100. X-rays demonstrated sclerosis of the talo-navicular joint and deformity of the scaphoid (Figure 3). MRI demonstrated necrosis of the scaphoid.
A 62-year-old female practiced ballet in her youth. She reported a persistent dorsomedial pain in the left midfoot without trauma. She used custom-made orthoses and occasionally took NSAIDs (ibuprofen). During the last few months, she could not take part in recreational activity and her daily life was strictly limited. She presented with a flatfoot, pain at the talo-navicular and hallux valgus, very restricted ROM of the ankle and subtalar joint, and dorsal hard prominence at the talus. Her AOFAS score was 25/100. X-rays showed narrowing of the joint and subchondral geodes. A computed tomography (CT) scan demonstrated advanced arthritis (Figure 4).
Case 1: Stage-1 MWD; Case 2: Stage-2 MWD; Case 3: Stage-4 MWD; Case 4: Stage-4 MWD.
The patient was treated with conservative therapies: magnetotherapy (8 h/d), bisphosphonates (intramuscular Chlodronate 200 mg: Once a day for two weeks, and then once a week for six subsequent weeks) and custom-made foot orthoses. The patient returned to normal life with no restrictions after eighty days (AOFAS score 98/100).
The patent was treated with magnetotherapy (8 h/d) and used custom-made foot orthoses. She returned to normal life with minimal restrictions after four months (AOFAS score 84/100).
Talo-navicular arthrodesis with two screws was performed. Weight-bearing was allowed at two months. At five months, the patient showed moderate improvement and partial return to daily activities (AOFAS score 71/100).
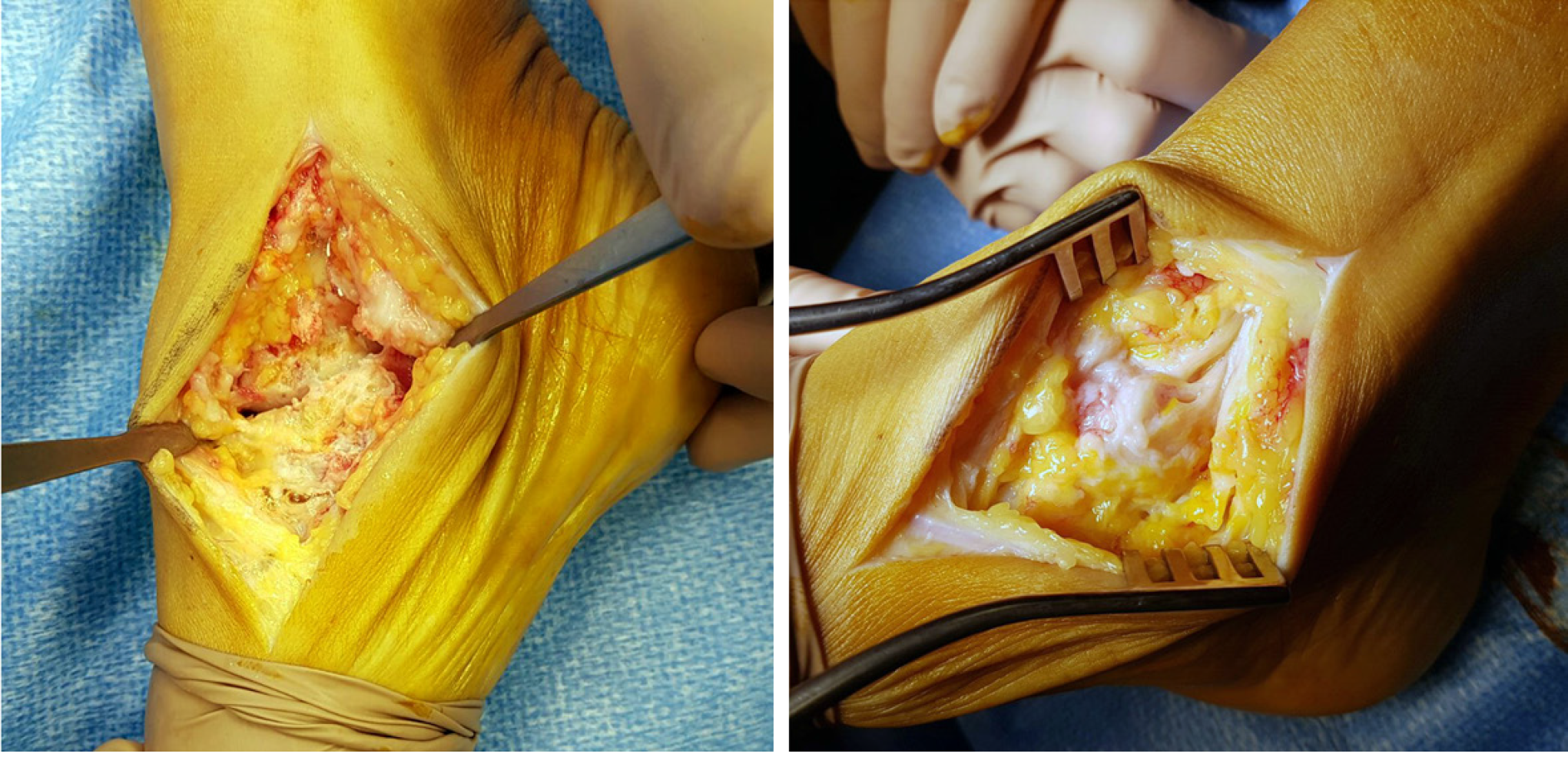
Talo-navicular arthrodesis with two cross screws was performed (Figure 5). Weight-bearing was allowed at two months. At six months, the patient showed occasional symptoms and she did not need any crutches for long walks; she returned to recreational activities such as swimming and cycling (AOFAS score 75/100).
The patients had uneventful clinical courses after conservative or operative treatment. At follow-up visits, the four patients were either asymptomatic or had occasional symptoms. They returned to their daily and recreational activities [AOFAS score (71-98)/100].
MWD is an idiopathic osteonecrosis of the tarsal navicular that is symptomatic in adulthood.
The true incidence of MWD is unknown. The disease is frequently bilateral and affects females during the 4th-6th decades of life[3,4]. Patients are usually overweight, the condition is more common in Europe than in America, and is probably related to nutritional or environmental factors. Nutritional deficiencies may cause disturbances in the ossification process. MWD is associated with tooth enamel hypoplasia, loss of teeth and the tertiary dentition process[5]. Its incidence is higher in populations under stressful conditions (war or famine) and in manual workers: however, these postulations have recently been refuted by Doyle et al[6].
Its pathogenesis remains unclear. MWD has been traditionally considered a spontaneous osteonecrosis of the navicular, but Maceira et al[5] recently disproved this theory, as patients’ histopathologic specimens demonstrated normal bone, inconsistent with osteonecrosis. In addition, Haller et al[7] stated that MRI findings were compatible but not specific to osteonecrosis. Mohiuddin et al[4] suggested that MWD is a sequelae of repetitive shear stress fractures of the navicular: However, this theory has not yet been proved.
MWD is commonly referred to an abnormal force distribution throughout the foot which alters navicular vascularization and delays its ossification (clamp-like mechanism)[5]. Thus, any condition resulting in lateralization of excessive compressive forces leads to deformity and, in late stages, fragmentation of the dorsolateral navicular. Moreover, shifting of the talar head occurs laterally over the calcaneus, driving the subtalar joint into the varus[8]. This occurs as the central navicular has a poor blood supply and local or generalized disturbance (endocrinopathies or malabsorption diseases) and this may disturb bone ossification. Mohiuddin et al[4] stated that MWD corresponds to the sequelae of undiagnosed navicular stress fractures, as lateral compressive force leads to the formation of a cleft along the sagittal plane, dividing the bone in two[4]. Navicular osteonecrosis could be related to polyarthritis, rheumatoid arthritis, kidney insufficiency or lupus erythematosus. Trauma is indeed considered to an unlikely contributing factor as bilateral disease is usually found in patients with a history of unilateral trauma[6].
MWD is often misdiagnosed. The typical presentation is a long period of mild and subtle discomfort followed by longstanding, atraumatic, disabling pain in the dorsomedial midfoot or/and hindfoot. Physical examination may reveal a hindfoot varus with low-arched, normal or a high-arched foot, depending on the severity of disease. The lateral malleolus is posteriorly placed due to extra-rotation of the tibia. A false impression of hindfoot varus is caused by the medial prominence of the navicular tuberosity, but the head of the talus is displaced laterally to the hindfoot axis. This situation, known as paradoxical pes planus varus, suggests an advanced stage of disease and is usually associated with a posteriorly prominent calcaneus. Monteagudo et al[8] asserts that failure to identify paradoxical flatfoot may lead to misdiagnosis and incorrect management. Swelling and tenderness are present over the dorsomedial aspect of the midfoot; tenderness may also exist over the lateral sinus tarsi. Subtalar movements may be reduced. Patients frequently complain of anterior knee pain due to patellar maltracking[3,4].
Weightbearing x-rays form the mainstay for diagnosis. Basic views are anteropos-terior, lateral and oblique of the foot; anteroposterior, lateral and mortise view of the ankle. It is important to obtain imaging of the contralateral foot for comparison. The examiner should assess the extent of navicular fragmentation as the presence of associated deformity or arthritic evolution.
Hetsroni et al[9] revealed significant differences in foot pressure distribution in MWD compared to non-MWD. They recorded increased plantar pressures at the midfoot and lower values in the toe segments. Hindfoot varus deformity leads to decreased mean pressure on the medial heel. Maceira and Rochera[5] also noted that the decreased pressure of the forefoot could lead to a low incidence of hallux valgus. As comprehensively illustrated by Welck et al[10], imaging is fundamental for diagnosis while exposing many parameters (Table 1).
| Radiological features in Müller-Weiss disease |
| Anteroposterior weightbearing |
| Hindfoot |
| Talocalcaneal divergence (reduced Kite angle) |
| Short cyma line: Talar head is no longer than the anterior process of the calcaneus |
| Widened talar head due to rotation |
| Midfoot |
| Comma or hourglass-shaped navicular |
| Lateral compression of the navicular with hyperdensity |
| Difficulty in distinguishing the lateral navicular from the underlying cuboid |
| Contact between the talar head and lateral cuneiforms |
| Medial column shortening |
| Cuboid sign: Subluxation of the cuboid |
| Forefoot |
| Parallelism of metatarsals with variable atrophy of 1st, 3rd, 4th and 5th |
| Second tarsal-metatarsal joint rotation |
| True or apparent (due to shortening of medial column) 1st metatarsal shortening |
| Second metatarsal cortical hypertrophy related to increased load |
| Lateral weightbearing |
| Hindfoot |
| Sinus-tarsi “see-through” sign |
| Increased calcaneal pitch |
| Abnormal cyma line |
| Posterior and middle subtalar facet visible in the same view |
| Double talar dome shadow |
| Midfoot |
| Anteroposterior shortening of the navicular |
| Meary’s line |
| Splitting with extrusion of the navicular |
| Surrounding arthritis |
A computed tomography scan allows accurate assessment of fracture lines, deformities, bone stock and density of tarsal navicular and surrounding arthritis. Furthermore, measurement of medial column shortening and pre-operative planning are permitted. MRI shows homogeneous hypointense signals in dorsolateral bone marrow on T1-weighted images, edema on STIR sequences and effusion in the surrounding joints. Hyperperfusion around the tarsal navicular is shown by technetium-99m polyphosphate bone scintigraphy. The same paper also illustrated a new method of tridimensional CT imaging with full weightbearing[10].
MWD should not be confused with Kohler’s disease as the latter is a spontaneous osteochondrosis that occurs in children, with a generally benign and self-limited course. These two disorders differ in epidemiology, clinical features and imaging. Köhler’s disease affects children 3-to-7 years old and is usually asymptomatic. The scaphoid appears hypoplastic at X-ray. MWD affects adults with pain and progressive navicular deformity. Koehler's disease is unilateral in 75%-80% and has a male preponderance of 4 or 6:1, while MWD is usually bilateral and seen predominately in women with a ratio of approximately 6:4. The most common imaging features are a flattened navicular bone, with irregular central sclerosis and eventual uniform reconstitution[10].
Other pathologies to consider as a possible differential diagnosis are osteomyelitis, Paget’s disease, healing fracture of the navicular, osteonecrosis secondary to renal failure, rheumatoid arthritis or systemic lupus erythematosus. In these cases, diagnosis is based on the patient’s history and laboratory values. Navicular stress fractures should also be considered, particularly in athletes. CT depicts stress-adaptive sclerosis and fracture morphology. These fractures are typically incomplete and involve the dorsal aspect of the navicular bone. Lastly, diabetic Charcot foot may also develop with subtle midfoot/hindfoot pain, swelling, fragmentation and sclerosis of the navicular. Destructive joint changes at later stages of the disease, followed by sclerotic and reparative changes, result in both joint subluxations/dislocation and foot deformities. However, the fragmentation in Charcot arthropathy is periarticular and associated with joint debris, whereas sclerotic changes are usually found over a disorganized joint. Vascular calcifications are an adjunctive finding in up to 90% of patients with Charcot foot[11].
In 2004 Maceira and Rochera[5] introduced a classification based on the compression/ fragmentation of the navicular bone and Meary’s line, on lateral radiographs (Table 2). Mayich[12] suggested the addition of stage 5 to include subtalar degeneration.
| Radiological staging | |
| Stage 1 | Normal or minimal bone changes on radiographs. Subtle subtalar varus. Intra-osseus edema on MRI. Positive CT scan |
| Stage 2 | Initial cavovarus: Subtalar varus and dorsal angulation of Meary’s line, dorsal and lateral subluxation of the talar head |
| Stage 3 | Subtalar varus. Medial column shortened. Neutral Meary’s line |
| Stage 4 | Subtalar varus. Plantarwards Meary’s line. Paradoxical pes planus with varus and calcaneal equinus |
| Stage 5 | Degeneration of the subtalar joint. Formation of talo-cuneiform articulation, complete extrusion of the navicular |
Currently, there is no gold standard for the treatment of patients with MWD. A wide variety of options have been described in a limited number of papers. Most of the options for early stages of the disease suggest initial conservative therapy with ankle foot orthoses, cast immobilization and NSAIDs[13]. The use of rigid insoles with a support of the medial arch and an anti-supination wedge for os calcis has been shown to be effective[8].
Operative treatment should subsequently be considered for failed conservative therapies longer than 6 months. The indication for surgery should be based on the severity of symptoms rather than the severity of deformities. Basics of intervention are arthrodesis of symptomatic degenerative joints to relieve pain and restoration of the medial longitudinal arch or Meary-Tomeno axis[4].
Operative treatment options include core decompression, internal fixation of the tarsal navicular, open or arthroscopic triple fusion, talo-navicular or talo-navicular-cuneiform arthrodesis, and navicular excision with reconstruction of the medial column[4,13-15]. Other procedures such as Achilles tendon lengthening or calcaneal osteotomy can also be considered. Some authors have suggested that calcaneal osteotomy is fundamental, as maldistribution of forces and biomechanical impairment are present in the MWD foot, and surgical treatment of the hindfoot should be considered to correct the varus deformity[3,13,16]. Monteagudo et al[8] suggested performing the Dwyer calcaneal osteotomy with lateral displacement, due to good outcomes and preservation of talar joints. The use of autologous tricortical iliac crest or allogenic femoral head grafts to reconstruct the excised navicular fragment was also described[3,17].
Although core decompression and autologous bone grafting has been widely used to treat the early stages of osteonecrosis of the femoral head, there is no consensus among investigators for the indications on this procedure or its efficacy[14].
Internal fixation of the navicular is considered appropriate for acute fractures, but with MWD, particularly in the later stages, morphological deformation precludes anatomic restoration of the navicular and its joint surfaces. Furthermore, fixation is not possible due to loss of bone stock in advanced stages of the disease. Maceira et al[5] and Fernandez de Retana et al[13] reported poor results in the presence of peri-navicular arthritis.
Isolated talo-navicular arthrodesis usually fails to resolve the incongruence of the navicular-cuneiform joint and carries a high risk of non-union[13,18]. This complication is due to poor vascularity of the bone and curved surfaces of the joint which can hinder internal fixation. As calcaneal-cuboid degeneration has been shown to be significant (83.3%), Lui recommended adding a calcaneal-cuboid arthrodesis instead of an isolated talo-navicular fusion because of potential pain in this joint[19]. Although isolated talo-navicular arthrodesis involves only a single joint, biomechanically it results in an almost complete loss of motion in the subtalar and transverse tarsal joints[20]. Finally, standard techniques with screw fixation may not be able to withstand the remaining forces resulting from the external rotation of the talar head and adduction forces of the navicular, respectively: Fornaciari et al[21] recommended, in addition to medial screw fixation, a lateral tension band technique to control these forces.
Talo-navicular-cuneiform arthrodesis (TNC) effectively corrects the deformity, eliminates the medial column arthritis that is the major source of pain, and maintains ROM in the remaining joints. Metal screws, staples or low contact plates can be used to stabilize the graft and for the arthrodesis. Fernandez de Retana et al[13] described medial-approach TNC arthrodesis using a trapezoid autologous graft to achieve the desired medial arch length. Cao proposed dorsal-approach TNC arthrodesis with a reverse V shaped osteotomy, and a dorsal based closing wedge osteotomy, through the talo-navicular joint. The graft was held in place with cannulated 4.0 mm titanium screws[18]. Yu et al[22] reported good results using a locking screw-plate system for TNC arthrodesis.
Triple fusion may deliver better consolidation but does not solve the problem of pain with the navicular-cuneiform joints; additionally, the subtalar joint motion is severely and unnecessarily restricted[17]. Triple arthrodesis can provide medial and lateral control, resulting in good stabilization. Lui proposed an arthroscopic fusion[19] which was performed through lateral, dorsolateral, dorsomedial and medial portals. Fixation was obtained by 4.0 cannulated screws. Compared to the open procedure, arthroscopic triple arthrodesis can minimize the soft tissue dissection and wound complications. Finally, Tan described excision of the diseased navicular and medial column reconstruction with either autologous cancellous bone or a remodeled femoral head allograft, stabilized with an AO low-contact plate[23].
The treatment of Müller-Weiss disease depends on the gravity of this disorder. Conservative therapies often succeed in the early stages while surgical treatment is indicated in patients with collapsed navicular bone or advanced osteoarthritis.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Taheri S S-Editor: Yan JP L-Editor: Webster JR P-Editor: Xing YX
| 1. | Müller W. Über eine typische gestalte Veränderung beim ös naviculare pedis und ihre klinische Bedeutung. ROFO. 1928;37:38-42. |
| 2. | Weiss K. Über die ‘‘Malazie’’ des os naviculare pedis. FortschritteaufdemG ebieteder Röntgenstrahlen. 1927;45:63-67. |
| 3. | Ahmed AA, Kandil MI, Tabl EA, Elgazzar AS. Müller-Weiss Disease: A Topical Review. Foot Ankle Int. 2019;40:1447-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Mohiuddin T, Jennison T, Damany D. Müller-Weiss disease - review of current knowledge. Foot Ankle Surg. 2014;20:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 5. | Maceira E, Rochera R. Müller-Weiss disease: clinical and biomechanical features. Foot Ankle Clin. 2004;9:105-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Doyle T, Napier RJ, Wong-Chung J. Recognition and management of Müller-Weiss disease. Foot Ankle Int. 2012;33:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Haller J, Sartoris DJ, Resnick D, Pathria MN, Berthoty D, Howard B, Nordstrom D. Spontaneous osteonecrosis of the tarsal navicular in adults: imaging findings. AJR Am J Roentgenol. 1988;151:355-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 69] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Monteagudo M, Maceira E. Management of Müller-Weiss Disease. Foot Ankle Clin. 2019;24:89-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Hetsroni I, Nyska M, Ayalon M. Plantar pressure distribution in patients with Müller-Weiss disease. Foot Ankle Int. 2007;28:237-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Welck MJ, Kaplan J, Myerson MS. Müller-Weiss Syndrome: Radiological Features and the Role of Weightbearing Computed Tomography Scan. Foot Ankle Spec. 2016;9:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Baker JC, Demertzis JL, Rhodes NG, Wessell DE, Rubin DA. Diabetic musculoskeletal complications and their imaging mimics. Radiographics. 2012;32:1959-1974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Mayich DJ. The treatment of Mueller-Weiss disease: a systematic approach. Tech Foot Ankle Surg. 2016;15:59-73. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Fernández de Retana P, Maceira E, Fernández-Valencia JA, Suso S. Arthrodesis of the talonavicular-cuneiform joints in Müller-Weiss disease. Foot Ankle Clin. 2004;9:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Lieberman JR. Core decompression for osteonecrosis of the hip. Clin Orthop Relat Res. 2004;(418):29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Viladot A, Viladot A Jr. Osteochondroses: aseptic necrosis of the foot. In: Disorders of the Foot and Ankle. WB Saunders, Philadelphia, 1991: 607-619. |
| 16. | Li SY, Myerson MS, Monteagudo M, Maceira E. Efficacy of Calcaneus Osteotomy for Treatment of Symptomatic Müller-Weiss Disease. Foot Ankle Int. 2017;38:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Nelson EW, Rivello GJ. Müller-Weiss disease of the tarsal navicular: an idiopathic case. J Foot Ankle Surg. 2012;51:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Cao HH, Tang KL, Xu JZ. Peri-navicular arthrodesis for the Stage III Müller-Weiss disease. Foot Ankle Int. 2012;33:475-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Lui TH. Arthroscopic triple arthrodesis in patients with Müller Weiss disease. Foot Ankle Surg. 2009;15:119-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Mann RA, Coughlin MJ. Surgery of the foot and ankle, vol II. Mosby, St Louis, 1999: 675-678. |
| 21. | Fornaciari P, Gilgen A, Zwicky L, Horn Lang T, Hintermann B. Isolated talonavicular fusion with tension band for Müller-Weiss syndrome. Foot Ankle Int. 2014;35:1316-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Yu G, Zhao Y, Zhou J, Zhang M. Fusion of talonavicular and naviculocuneiform joints for the treatment of Müller-Weiss disease. J Foot Ankle Surg. 2012;51:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Tan A, Smulders YC, Zöphel OT. Use of remodeled femoral head allograft for tarsal reconstruction in the treatment of müller-weiss disease. J Foot Ankle Surg. 2011;50:721-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |