Published online Oct 18, 2020. doi: 10.5312/wjo.v11.i10.465
Peer-review started: May 19, 2020
First decision: July 21, 2020
Revised: July 23, 2020
Accepted: September 4, 2020
Article in press: September 4, 2020
Published online: October 18, 2020
Processing time: 152 Days and 4.3 Hours
Patients with a shoulder arthrodesis generally experience restriction in range of motion and limitations in activities of daily living. In addition, up to one-third of the patients deals with serious peri scapular pain. The conversion of a shoulder arthrodesis in a reverse shoulder arthroplasty (RSA) has been described as an effective treatment to achieve better function and decreased pain, although literature is sparse. We present the case of a conversion from a painful shoulder arthrodesis to RSA, after a 51 years interval.
A 71-year-old male presented with severe peri scapular pain and limited function 51 years after shoulder arthrodesis. Preoperative workup showed a normal bone stock of the glenoid and an intact axillary nerve, but atrophic posterior part of the deltoid muscle. The shoulder arthrodesis was successfully converted to RSA. Twelve months postoperative the patient was very satisfied. He has no pain at rest, nor with exercise and experienced definite improvements in activities of daily living, despite his limited range of motion.
Conversion from shoulder arthrodesis to a RSA can be performed safely, with a high chance of peri scapular pain relief; even after a longstanding arthrodesis.
Core Tip: To the best of our knowledge, this unique presentation of a conversion from shoulder arthrodesis to reverse shoulder arthroplasty is the sixth reported case. This treatment should be considered in patients with a painful shoulder arthrodesis. Requirements for a successful procedure are adequate bone stock and a functional deltoid muscle. The treatment can be performed safely, with a high chance of peri scapular pain relief; even after a longstanding arthrodesis. Improvements of activities of daily living are noticed, with varying results of shoulder function.
- Citation: Dogger MN, Bemmel AFV, Alta TDW, van Noort A. Conversion to reverse shoulder arthroplasty fifty-one years after shoulder arthrodesis: A case report. World J Orthop 2020; 11(10): 465-472
- URL: https://www.wjgnet.com/2218-5836/full/v11/i10/465.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i10.465
Shoulder arthrodesis is a salvage procedure for patients with shoulder dysfunction when other surgical options are limited. Indications include post-traumatic brachial plexus injuries, paralysis of the deltoid muscle and the rotator cuff, chronic infections, failed arthroplasties, and recurrent instability[1,2]. A shoulder arthrodesis may involve an acromiohumeral fusion, a glenohumeral fusion, or a combination of both[1-3]. The shoulder function of a well-positioned arthrodesis is limited and allows the patient to reach his back pocket, groin, and mouth. Generally, only scapulothoracic movements, like elevation and minimal rotations, after an arthrodesis are possible[1,2]. Most patients experience a reduction in pain but few are pain free, with up to one-third experiencing substantial peri scapular pain[1,2,4].
A treatment for a painful arthrodesis is conversion to reverse shoulder arthroplasty (RSA), which has been described as effective for pain relief and promising functional improvements[5,6]. Based on the literature review conducted by the authors of this report, only two reports were found that describe a total of five cases in which the patients received a conversion to RSA[5,6].
Here we present the case and surgical technique of a conversion from a painful shoulder arthrodesis to RSA in a 71-year-old male patient after a 51 years interval. The patient was informed that data concerning the case would be submitted for publication, and written patient consent was obtained. Table 1 outlines a timeline of the patient presentation.
| Timeline | Patient situation |
| 1967 | Posttraumatic posterior instability both shoulders; underwent arthrodesis right shoulder |
| 2017 | Underwent reverse shoulder arthroplasty left shoulder |
| Mai 2018 | Conversion of arthrodesis to reverse shoulder arthroplasty right shoulder |
| Mai 2019 | At twelve months follow-up; complete disappearance of his peri scapular pain and improvements in activities of daily living |
A 71-year-old male patient presented to the orthopedics outpatient department of our hospital with complaints of severe peri scapular pain and limited shoulder function, 51 years post arthrodesis of the right shoulder.
Since the shoulder arthrodesis, the patient has been experiencing peri scapular pain. There was no history of new preceding trauma or injury. Pain progressed throughout the years, present at rest and with activity. Due to the limited range of shoulder motion, the patient experienced problems in activities of daily living. He was unable to reach above shoulder level and particularly the loss of internal rotation bothered him in self-care. Conservative treatment including analgesics and physical therapy was ineffective.
Indication for arthrodesis in the past was persistent posttraumatic posterior instability of both shoulders after failed open stabilizing procedures. In 2017, the patient was treated with a RSA on the left side because of development of a rotator cuff arthropathy. Due to a very good functional outcome of the left shoulder, he had the expressed wish for conversion of the fused right shoulder into RSA as well.
At physical examination the actively achieved elevation was 100º, external rotation and internal rotation to lateral side of his leg. Notable was the peri scapular pain which he experienced during physical examination. He had an Oxford Shoulder Score of 38 (the best score: 12; the lowest score: 60). Sensibility of the axillary nerve was intact and despite general atrophy of the deltoid muscle (in particular the posterior part), contraction of the deltoid muscle was still possible.
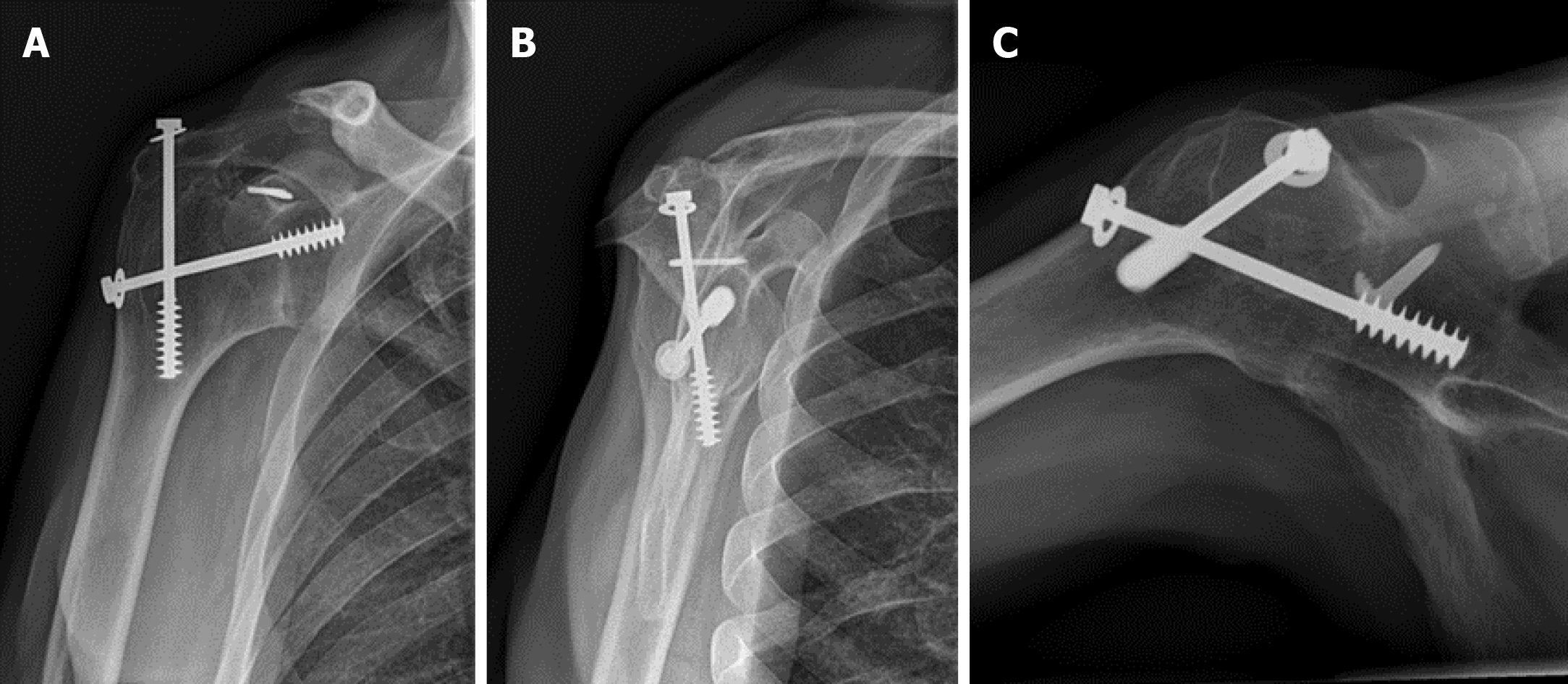
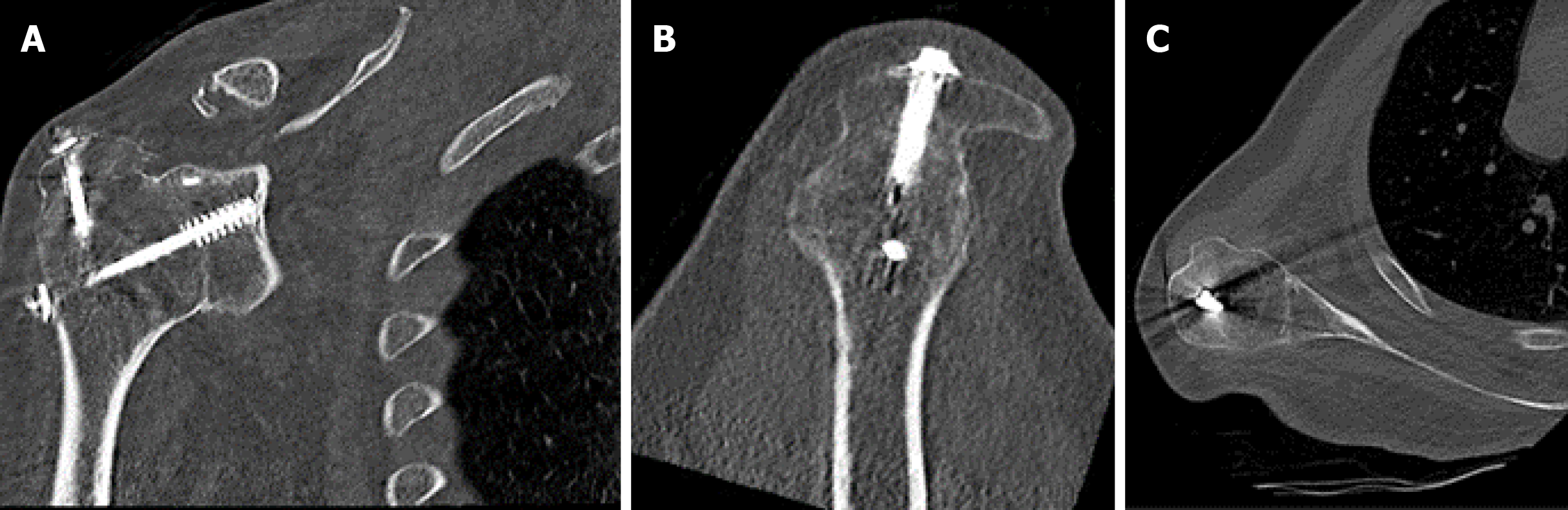
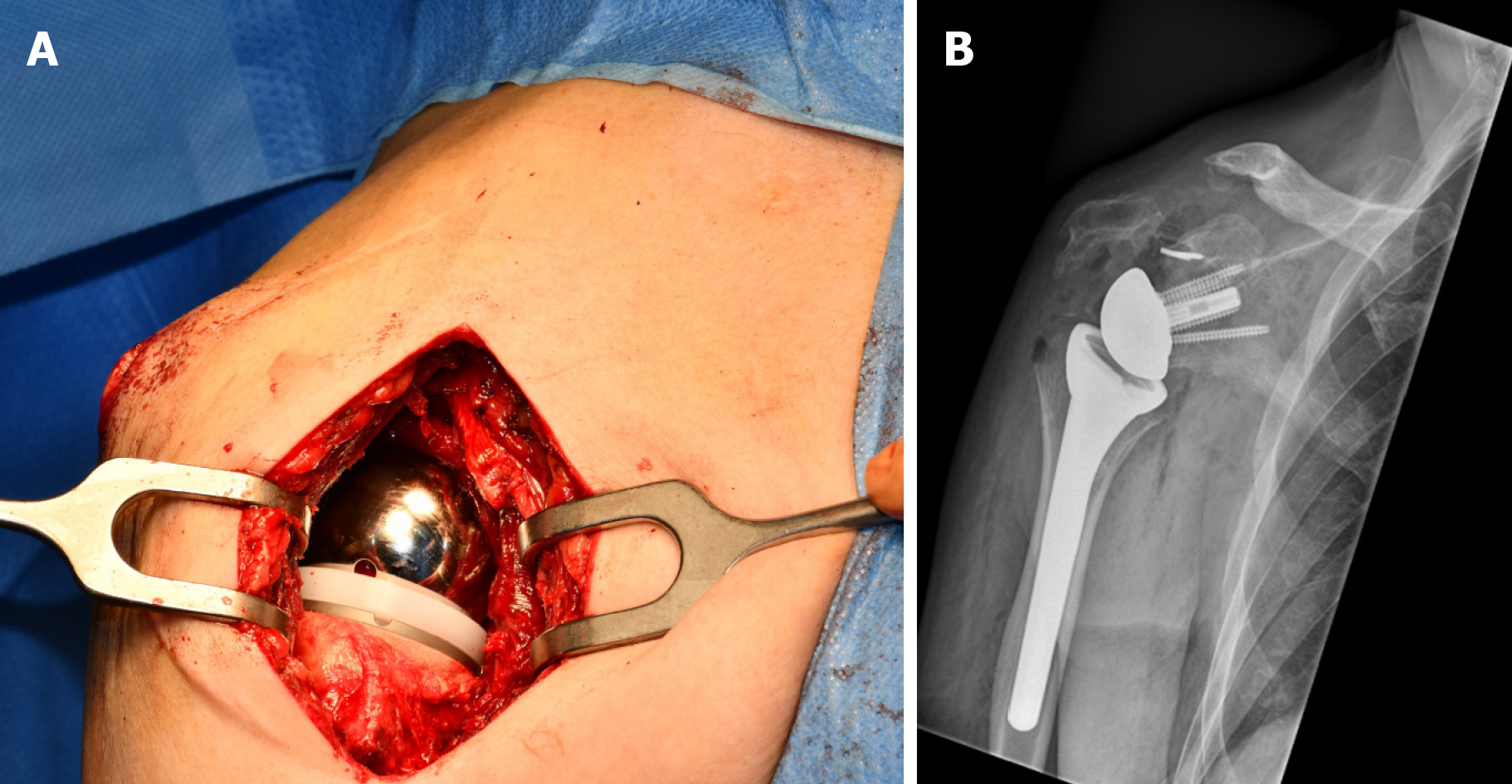
Conventional radiographs (Figure 1) and computed tomography (Figure 2) showed a shoulder arthrodesis with glenohumeral and acromiohumeral consolidation and normal bone stock of the glenoid. As part of the preoperative workup, electromyography (EMG) was performed and showed normal motor unit activity and recruitment in all three parts of the deltoid muscle.
Complete cessation of peri scapular pain and structural improvements in daily activity after conversion of shoulder arthrodesis to RSA, after a 51 years interval.
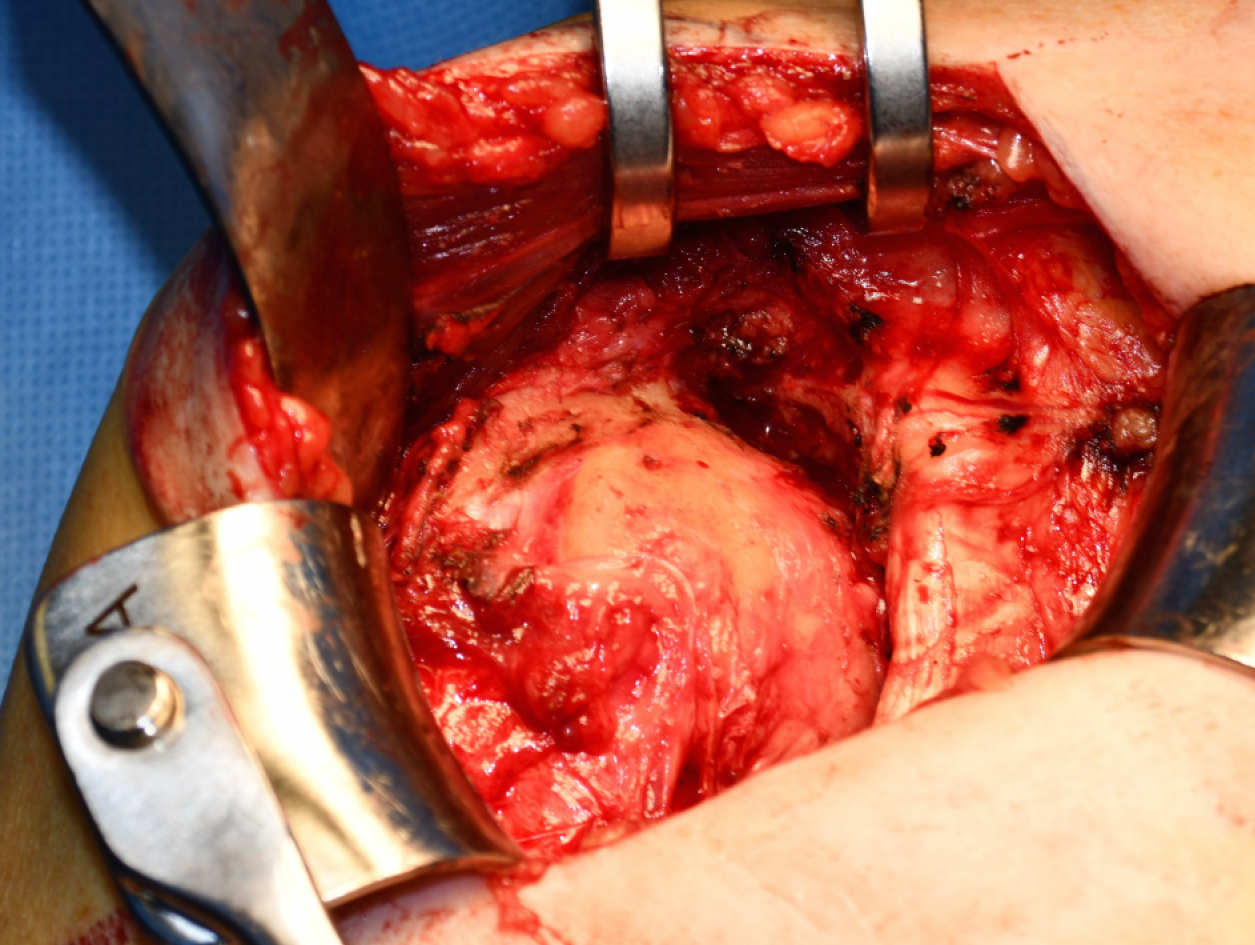
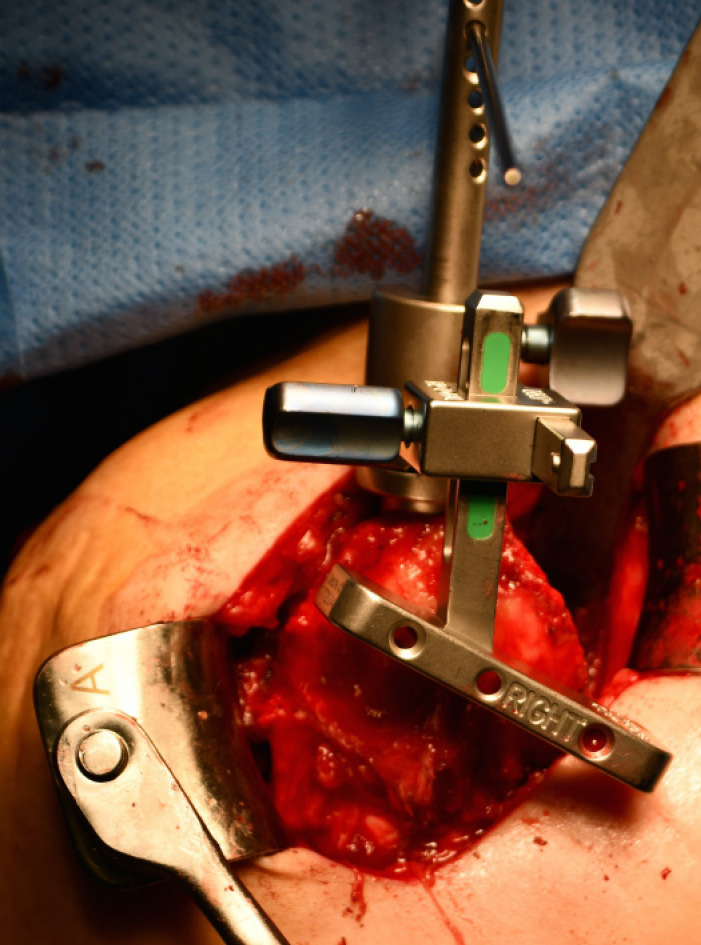
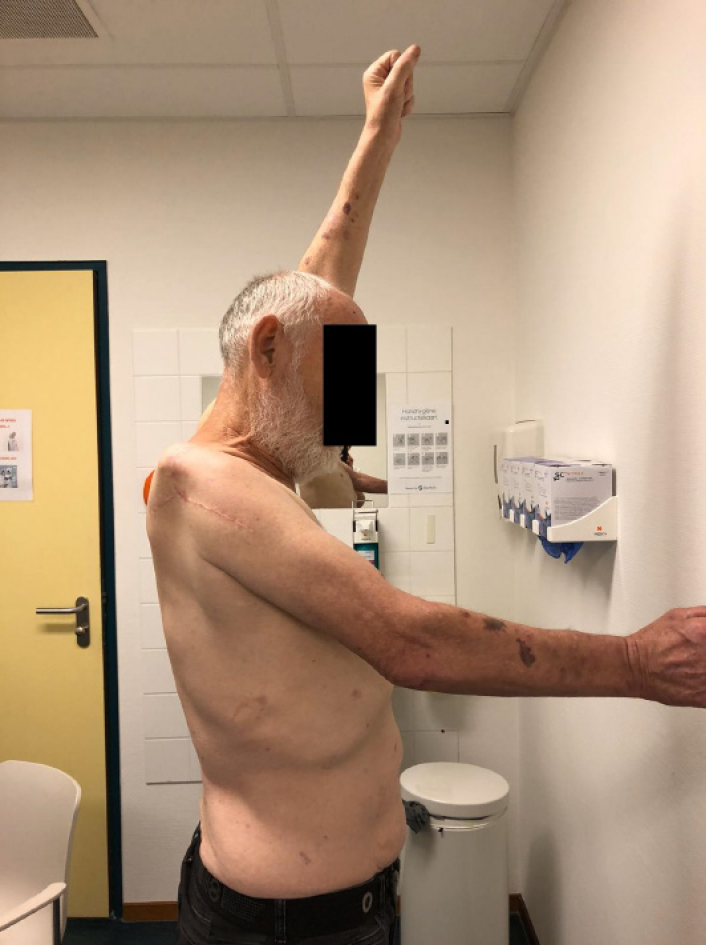
At the time of surgery, the patient had an interscalene block with general anesthesia, and was positioned semi-inclined in the beach chair position. After a stab incision the superior screw, through the acromion into the humeral head, was removed. The original anterior incision was used and a deltopectoral approach performed. The layers could nicely be mobilized without obstruction of an excessive amount of fibrosis. In contrast with a sufficient deltoid muscle (Figure 3), the quality of the rotator cuff was very poor with an absent superior cuff and a fibrotic, very thin subscapularis muscle. After removal of the screw which penetrated the formal glenohumeral joint, an osteotome was used to split the acromion from the humeral head. The “glenohumeral” osteotomy was performed under 10º of caudal inclination, a neutral version and one centimeter lateral from the original joint line, creating a long-necked scapula (Figure 4) in order to minimize scapular notching and improve rotations. An uncemented RSA (DELTA XTEND, DePuy Synthes, Raynham, Massachusetts, United States) was now implanted in a standard fashion (Figure 5).
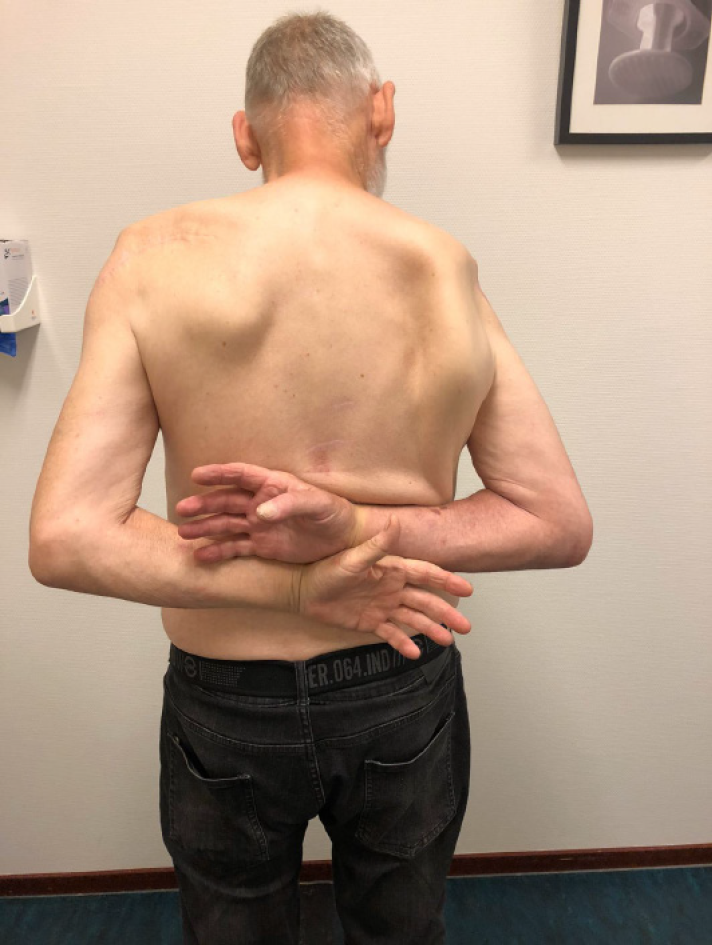
Postoperatively the patient was placed in a shoulder immobilizer for 6 wk. The patient was allowed to move passively and actively guided for 6 wk direct postoperatively. The postoperative course was otherwise uneventful. At 12 mo follow-up, the patient was very happy with respect to the outcome, with complete disappearance of his peri scapular pain (visual analogue scale score 0 in rest and exercise) and structural improvements in activities of daily living like eating with knife and fork, wiping his buttocks with his right hand, carrying more heavy objects with his right hand. Nevertheless, his shoulder function was rather poor with an active forward elevation of 50º, internal rotation to Th12 and absence of external rotation (neutral position) (Figures 6-8). The deltoid muscle had an intact function in the anterior and lateral part, the posterior part was atrophic (Figure 6). He had an Oxford Shoulder Score of 23, and a Subjective Shoulder Value of 60%. Conventional radiographs showed a correct position of the RSA (Figure 5B). The patient was very satisfied with the outcome and assured the necessity of the surgery.
Shoulder arthrodesis for recurrent instability is a salvage procedure to regaining stability and some degree of function[1,2]. However, after the arthrodesis not all patients are pain free. Our patient still experienced peri scapular pain and severe limitation of active range of motion. The conversion of a shoulder arthrodesis into a RSA, has been described as an alternative and promising treatment for managing pain and achieve better functional results[5,6].
In patients with a RSA, the deltoid muscle becomes the primary mover of the shoulder. Due to fibrosis and atrophy after arthrodesis, the function of the rotator cuff muscles is absent[4,6]. Therefore, the deltoid muscle function is critical to shoulder function after RSA[7,8]. Li et al[8] have suggested that preoperative EMG measurements of the deltoid muscle will help to predict the postoperative outcome of RSA. They found that postoperative shoulder strength after RSA was increased in patients with greater EMG activity of the middle deltoid. In an EMG study of Walker et al[4], an important role for the anterior part of the deltoid is suggested. Lädermann et al[9] concluded that if partial deltoid function remains, RSA can produce reliable improvements in functional outcomes without an increased risk of dislocation. To obtain preoperative information of the activity and the quality of the deltoid muscle, we performed an EMG, which showed normal motor unit activity and recruitment in all three parts of the deltoid muscle.
A few previous case reports described conversion of a shoulder arthrodesis into hemiarthroplasty and total shoulder arthroplasty[10-13]. Patients achieved minimal functional improvement and mild to moderate pain remained. To the best of our knowledge, only two case reports of conversion of a shoulder arthrodesis into RSA are published[5,6]. No cases reported such a long interval (51 years) between arthrodesis and conversion to RSA.
Table 2 shows the patient characteristics and functional outcomes at different follow-up of patients from both studies[5,6]. Alta et al[6] found that activity in two-thirds of the deltoid was sufficient to create a stable arthroplasty, with impairment of the anterior part in three of the four patients. Only one patient preoperatively had a completely intact deltoid muscle. Nevertheless, after conversion to RSA the elevation of that patient improved with 40 degrees but postoperative elevation did not reach above shoulder height[6]. The young patient in Toney et al[5] achieved excellent elevation of 160 degrees after conversion to RSA, with an intact deltoid muscle. However, this patient was not free of pain. In Alta et al[6], all patients experienced decreased pain, but only one patient noted a pain score of zero. Most important for our patient was his complete ceasing of peri scapular pain, and he was very pleased with the improvement in internal rotation. Despite an intact axillary nerve and anterior part of the deltoid, he lost postoperatively active forward elevation, which could be related with the timeframe between arthrodesis and reverse arthroplasty. However, the patient is a highly motivated patient who continued in a determined way with active exercises.
| Toney et al[5] | Alta et al[6] | ||||
| Patient characteristics | Female, 41 yr | Female, 63 yr | Male, 46 yr | Female 66, yr | Male, 58 yr |
| Arthrodesis indication | Brachial plexus injury with recurrent instability | Post-traumatic arthritis | Glenohumeral arthritis | Failed surgeries for proximal humeral fracture | Failed surgeries for proximal humeral fracture |
| Years after arthrodesis | 5 | 11 | 5 | 6 | 11 |
| Preoperative EMG | Deltoid intact | 2/3 deltoid intact | 2/3 deltoid intact | Deltoid intact | 2/3 deltoid intact |
| Follow-up (mo) | 12 | 36 | 6 | 48 | 22 |
| Preoperative/postoperative | |||||
| Forward elevation | 60/160 | 60/70 | 70/110 | 50/90 | 40/40 |
| External rotation | 0/60 | 0/15 | 0/20 | 0/15 | 0/10 |
| Internal rotation | Trochanter/Th12 | Trochanter/L5 | Trochanter/L5 | Trochanter/L5 | Trochanter/sacrum |
| VAS pain scores | 6 | 2 | 0 | 4 | 1 |
The importance of a complete intact deltoid muscle and the role of the anterior part seems debatable. In our opinion, the activity of the deltoid muscle can be assessed by judging the tension of the muscle during physical examination. Additional information on the deltoid muscle by performing an EMG can be considered. More cases with conversion of arthroplasty to RSA are needed to predict the outcome of shoulder function from the activity of the three parts of the deltoid muscle.
Conversion from shoulder arthrodesis to a RSA can be performed safely, with a possibility for peri scapular pain relief; even after a longstanding arthrodesis. Improvements in activities of daily living were noticed by our patient despite loss of active forward elevation.
We would like to thank the patient for being so willing to participate in the case report. Thanks are also due to Schager M, our native speaker, for her help with the language and grammar.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koumantakis GA S-Editor: Gao CC L-Editor: A P-Editor: Li JH
| 1. | Safran O, Iannotti JP. Arthrodesis of the shoulder. J Am Acad Orthop Surg. 2006;14:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Clare DJ, Wirth MA, Groh GI, Rockwood CA. Shoulder arthrodesis. J Bone Joint Surg Am. 2001;83:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Lädermann A, Denard PJ. Arthroscopic glenohumeral arthrodesis with o-arm navigation. Arthrosc Tech. 2014;3:e205-e209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Walker D, Wright TW, Banks SA, Struk AM. Electromyographic analysis of reverse total shoulder arthroplasties. J Shoulder Elbow Surg. 2014;23:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Toney CB, Thompson MJ, Barnes BJ, Boardman ND. Conversion of Glenohumeral Fusion to Reverse Total Shoulder Arthroplasty: A Case Report. JBJS Case Connect. 2017;7:e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Alta TD, Willems WJ. Once an arthrodesis, always an arthrodesis? J Shoulder Elbow Surg. 2016;25:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Smith RA, Woolley K, Mazzocca A, Feinn R, Cote M, Gomlinski G, Garbalosa J, Myrick KM. Kinematics and EMG activity in Reverse Total Shoulder Arthroplasty. J Orthop. 2020;22:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Li H, Yoon SH, Lee D, Chung H. Relation between preoperative electromyographic activity of the deltoid and upper trapezius muscle and clinical results in patients treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Lädermann A, Walch G, Denard PJ, Collin P, Sirveaux F, Favard L, Edwards TB, Kherad O, Boileau P. Reverse shoulder arthroplasty in patients with pre-operative impairment of the deltoid muscle. Bone Joint J. 2013;95-B:1106-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Nho SJ, Garbis N, Reiff S, Terry A, Shindelar S, Romeo AA. Conversion of glenohumeral fusion to total shoulder arthroplasty for scapulothoracic pain: case report and surgical technique. HSS J. 2010;6:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Cofield RH, Briggs BT. Glenohumeral arthrodesis. Operative and long-term functional results. J Bone Joint Surg Am. 1979;61:668-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 109] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Sperling JW, Cofield RH. Total shoulder arthroplasty after attempted shoulder arthrodesis: report of three cases. J Shoulder Elbow Surg. 2003;12:302-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Hertel R, Ballmer FT. Shoulder arthroplasty after glenohumeral fusion. J Shoulder Elbow Surg. 1994;3:407-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |