Published online Oct 18, 2020. doi: 10.5312/wjo.v11.i10.431
Peer-review started: April 18, 2020
First decision: August 9, 2020
Revised: August 18, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 18, 2020
Processing time: 184 Days and 3.2 Hours
New implants for total knee arthroplasty (TKA) are continuously introduced with the proposed benefit of increased performance and improved outcome. Little information exists on how the introduction of a novel arthroplasty implant affects the perioperative and surgical outcome immediately after implementation.
To investigate how surgery-related factors and implant positioning were affected by the introduction of a novel TKA system.
A novel TKA system was introduced at our institution on 30th November 2015. Seventy-five TKAs performed with the Persona TKA immediately following its introduction by 3 different surgeons (25 TKAs/surgeon) were identified as the Introduction Group. Moreover, the latest 25 TKAs performed by each surgeon prior to introduction of the Persona TKA were identified as the Control Group. A Follow-up Group of 25 TKAs/surgeon was identified starting 1-year after the end of the introduction period. Demographics, surgery-related factors and alignment data were recorded, and intergroup differences compared.
Following introduction of the novel implant, Persona TKA was utilized in 69% (71%), 53% (54%), and 45% (75%) of primary TKA procedures by the three surgeons, respectively (Follow-up Group). Mean surgery time was increased by 28% (P < 0.0001) and mean intra-operative blood loss by 25% (P = 0.002) in the Introduction Group, while only the mean surgery time was increased in the Follow-up Group by 18% (P < 0.0001). Overall alignment was similar between the groups apart from femoral flexion (FF) and tibial slope (TS). The number of FF outliers was reduced in the Introduction Group with a more pronounced decrease in the Follow-up Group.
Introduction of the new TKA implant increased surgical time and intraoperative blood loss immediately after its introduction. These differences diminished one year after introduction of the new implant. Fewer outliers with respect to FF and TS were seen when using the novel TKA implant. Further studies are needed to investigate if these differences persist over time and correlate with patient reported outcomes.
Core Tip: Limited information exists in the literature on how the introduction of a novel total joint arthroplasty (TKA) system translates to improvements in early surgical outcome and component alignment in first adopters. The introduction of a novel TKA implant increased surgical time and intraoperative blood loss immediately after its introduction, but diminished one year after introduction of the implant. As only minor improvements with respect to optimal TKA alignment were observed following its introduction, surgeons should take increased care when introducing new procedures and consider logistics when selecting novel implants, as small gains in alignment should be balanced against inferior peri-operative outcomes.
- Citation: Omari A, Troelsen A, Husted H, Nielsen CS, Gromov K. Early clinical outcome and learning curve following unilateral primary total knee arthroplasty after introduction of a novel total knee arthroplasty system. World J Orthop 2020; 11(10): 431-441
- URL: https://www.wjgnet.com/2218-5836/full/v11/i10/431.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i10.431
The use of total knee arthroplasty (TKA) has risen globally throughout the last 2-3 decades and is projected to increase even further[1]. New implants for TKA are constantly introduced with the proposed benefit of increased performance and improved outcome for patients. In recent years, this rapidly advancing trend concurrently necessitated a stricter scrutiny of the regulatory environment around the introduction of novel medical devices with ambitions of strengthening patient safety and monitoring claimed effects[2-4]. A focus on the long-term outcome after TKA introduction, which is gained through prospective and registered studies, is critical in its own right, and the introduction is similarly accompanied by more immediate changes in relation to learning curves and early clinical outcomes. Little information exists on how early surgical outcome is affected following the introduction of a novel TKA system[5,6]. One study found significant variations in model-specific learning curves for new TKA systems, with some systems showing a learning curve with an increase in early revisions[7].
The expectation of improvements offered by the new systems in comparison to the former established systems, is unfortunately sometimes contradicted by evidence of undesirable effects on revision rates[8,9] and patient-perceived outcomes[10]. Furthermore, novel TKA systems are generally priced higher compared to older systems[11].
The Persona® (Zimmer-Biomet, Warsaw, Indiana, United States) TKA was introduced in our department as a supplement to two older established TKA systems. The aim of this study was to investigate how surgery-related factors as well as implant positioning were affected by the introduction of the novel TKA system. Furthermore, we aimed to investigate the utilization rate of the novel system, and how surgical experience with the implant affected the procedure.
On the 30th November 2015, the Persona TKA was introduced in our institution (Copenhagen University Hospital Hvidovre, Denmark).
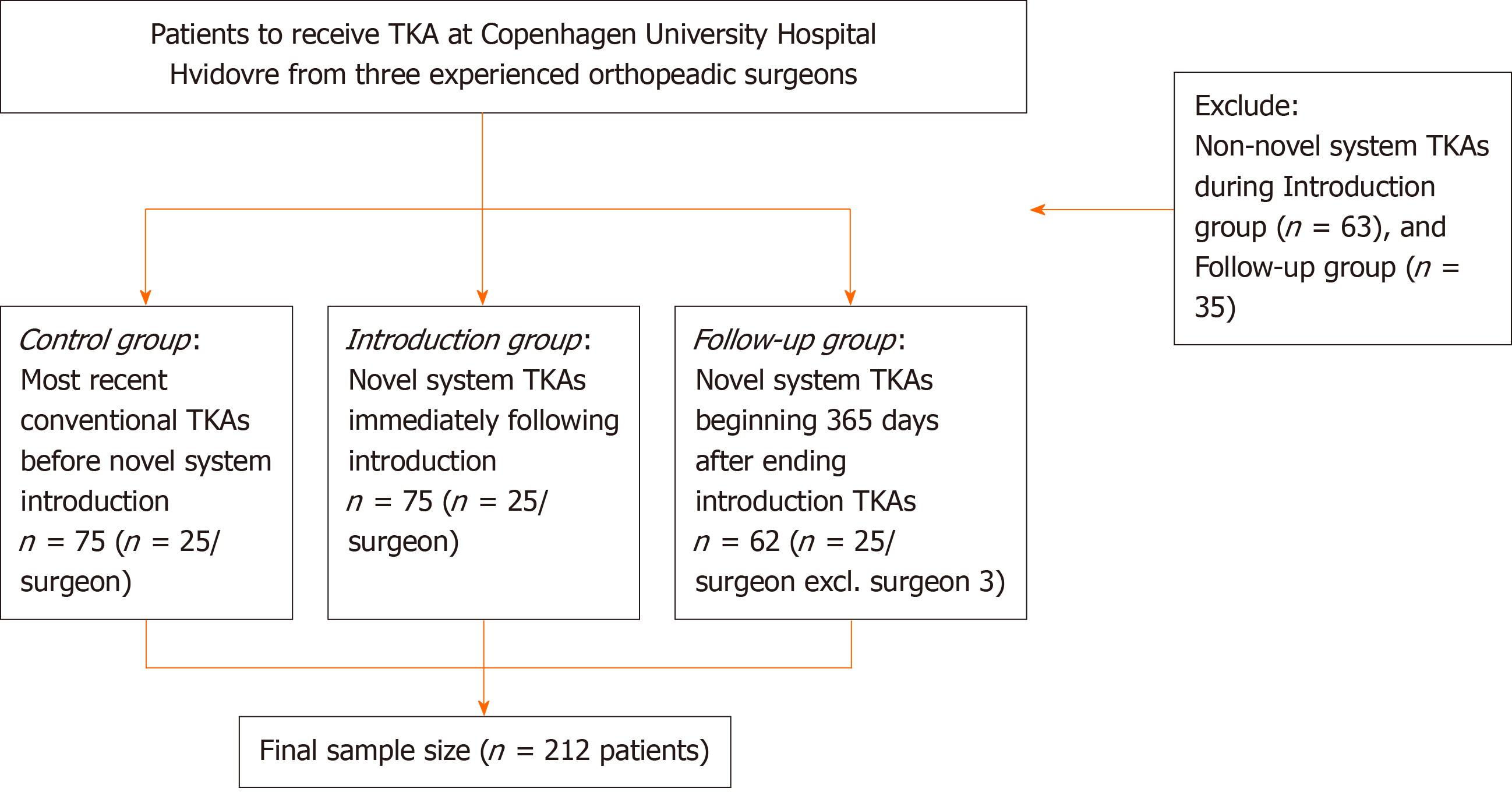
We included 75 consecutive knees treated with the Persona TKA in the introduction period starting from 30th November 2015 immediately following implementation by three experienced surgeons (25 TKAs/surgeon) (Introduction Group), along with a Control Group (n = 75) consisting of the most recent consecutive TKAs performed by the same surgeons prior to introduction of the Persona TKA (25 TKAs/surgeon). Finally, a Follow-up Group of 62 consecutive knees starting from 365-d after each respective surgeon ended their initial 25 Persona TKAs was included. In the Follow-up Group, two of the three surgeons managed to complete 25 TKAs, while the third surgeon only completed 12 TKAs due to a recent change in the first choice of TKA system at our institution. In summary, we retrospectively identified a total of 212 patients who underwent primary unilateral TKA surgery at our institution (Figure 1). The patients were operated between 11th August 2015 (the first patient in the Control Group) and 3rd December 2018 (the last patient in the Follow-up Group). However, it should be noted that the three orthopedic surgeons’ individual timeframes were shorter which was ascribed to differences in volume and utilization frequency of the novel system following its introduction. From start to finish, surgeon 1 spent approximately 3.2 years, surgeon 2 spent approximately 2.5 years and surgeon 3 spent approximately 2.8 years. In these individual timeframes, the orthopedic surgeons performed a total of 96, 118 and 96 TKAs, respectively. As surgical skill, experience and caseload varies across orthopedic surgeons we ensured a study design which accounted for these variances by studying the same experienced orthopedic surgeons throughout the study. Patients were registered and included in this study through use of the institution’s patient registry. Only cruciate retaining (CR) implants were included in the analysis.
The patients were pooled into three cohorts for data analysis purposes: Control Group, Introduction Group and the Follow-up Group. The patients were included based on their primary unilateral CR TKA, surgeon and timeframe, and as such unselected for all other factors. All patients were monitored for 90-d after surgery, and any readmissions or deaths were recorded. No patients were lost due to follow-up or died within the 90-d period.
Following the introduction of the Persona system, a company representative was present during surgery for as long as the surgeon deemed necessary. All patients were operated in a well described standardized fast-track setup[12]. A standard medial parapatellar incision was used. Femoral and tibial surfaces were prepared using standard cutting guides using a measured resection technique. All surgeons aimed for neutral anatomical alignment[13]. Resurfacing of the patella was performed in all cases. The novel system (Persona) differed with respect to the anatomical baseplate, option for 1 mm increment adjustment for tibial bearing size, option for adjusting gaps through anteriorized and posteriorized instrumentation of the femur, option to adjust distal femoral resection in 1 mm increments and option to adjust distal femoral resection angle in 1-degree increments. Blood loss management was similar across TKA systems with bone plugging of the femoral canal, 1 g tranexamic acid administered at the start of the operation and re-administered 3 h later. No drain or tourniquet was applied, and spinal anesthesia was given to all patients.
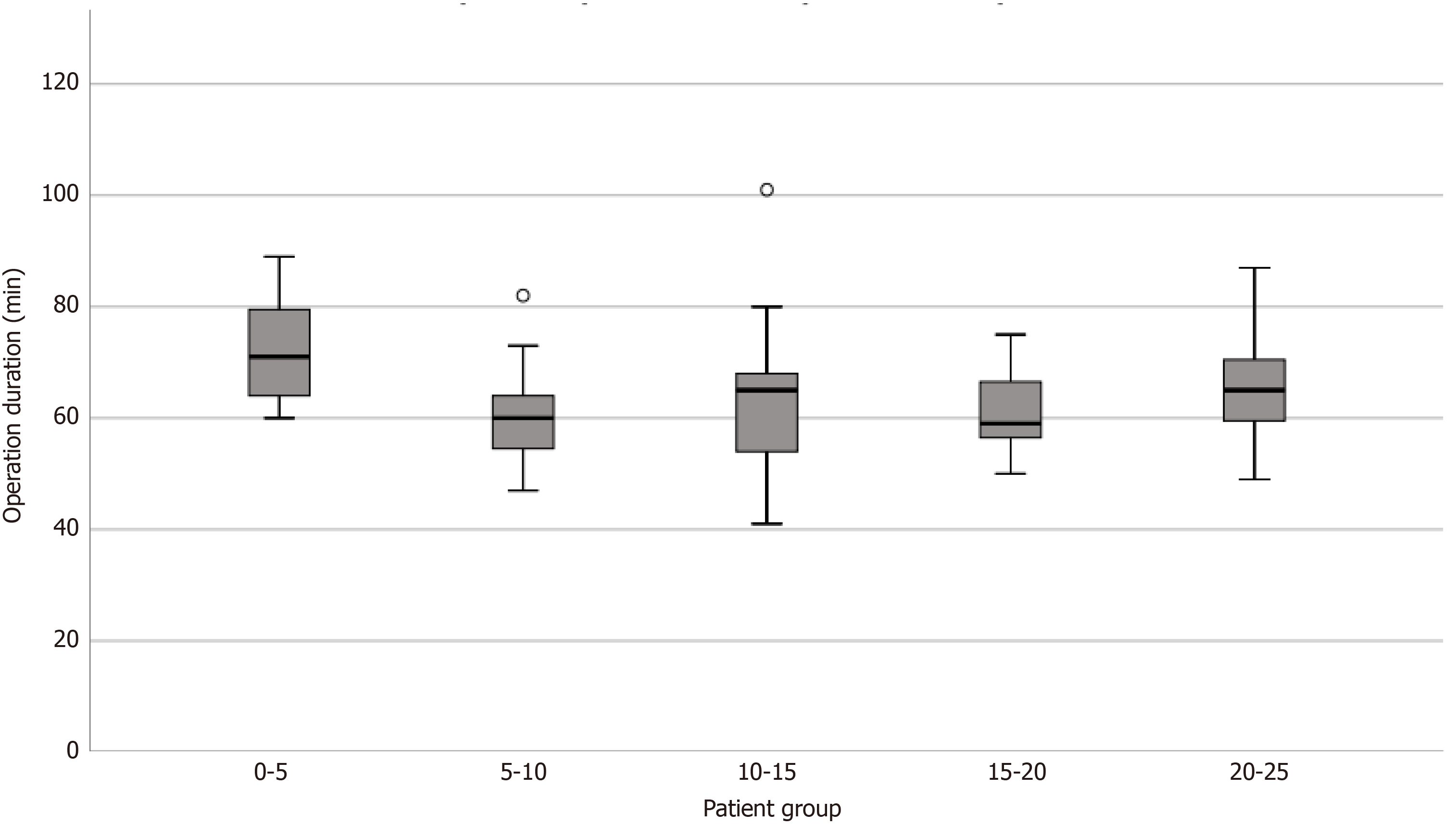
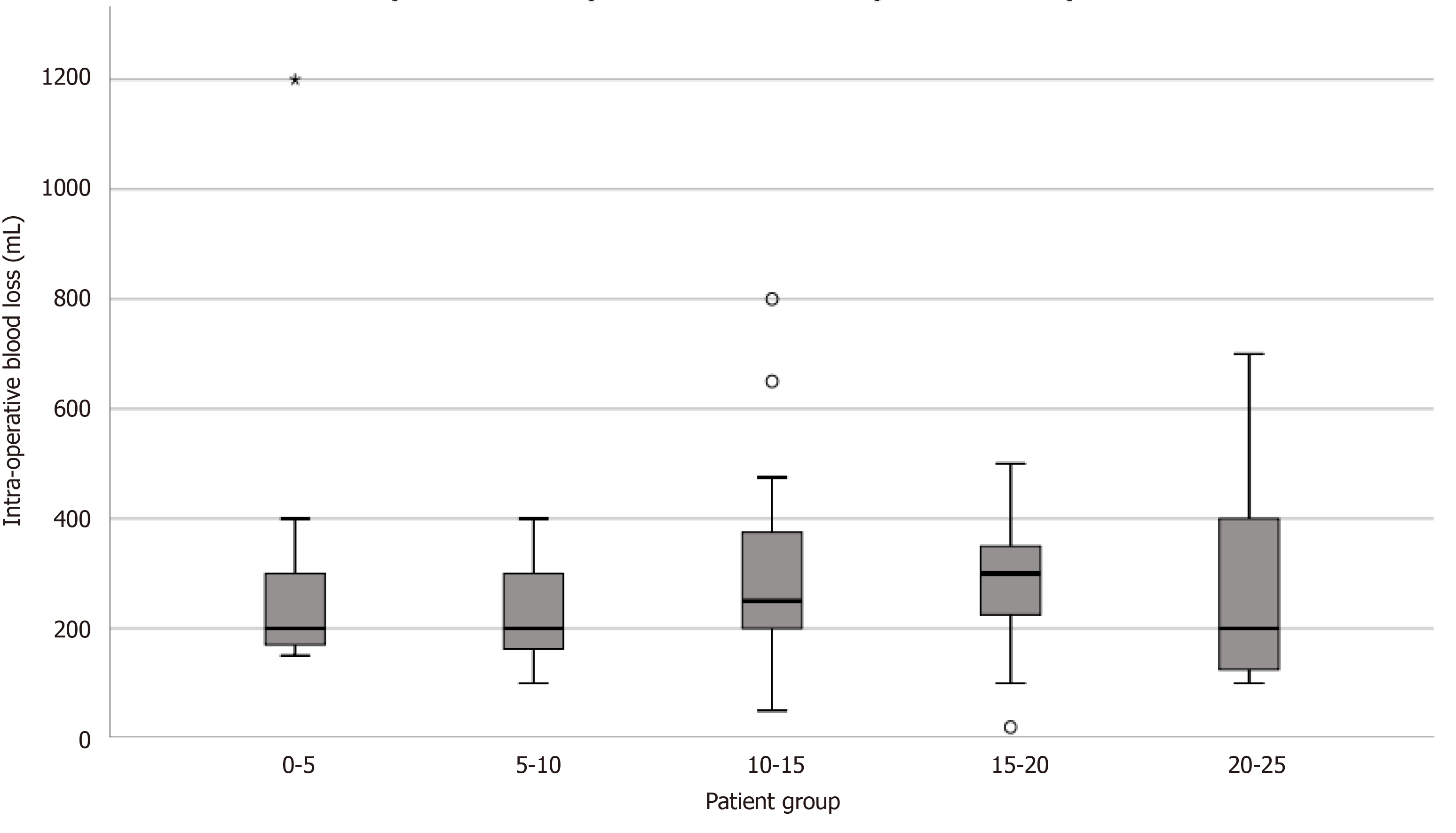
Demographic parameters such as age, gender, length of operation, body mass index (BMI), levels of pre-operative American Society of Anaesthesiologists score (ASA score) were recorded (Table 1). Radiological parameters including AP alignment of tibial and femoral components, femoral flexion (FF), tibial slope (TS), post-operative tibio-femoral angle (TFA), pre-operative TFA, lateral and medial tibial overhang were recorded (Table 2). Perioperative factors constituting measured blood loss, any intraoperative complications, length of operation, length of stay (LOS), and readmissions within 90 d were recorded (Table 3). For blood loss and length of operation, patients in the Introduction Group were pooled into five chronologically ordered patient groups from earliest (0-5) to latest (20-25) TKA by each surgeon, to detect any initial improvements due to the learning curve (Figure 2 and Figure 3).
| Control group | Introduction group | P value (Control vs Introduction) | Follow-up group | P value (Control vs Follow-up) | Test | |
| Subjects count, n (%) | 75 (100) | 75 (100) | 62 (100) | |||
| Age, mean (range) | 65.6 (49-84) | 61.1 (39-81) | 0.009 | 65.1 (45-86) | 0.90 | Mann-Whitney U test |
| Gender, male/female (%) | 31/44 (m = 41%, f = 59%) | 38/37 (m = 51%, f = 49%) | 0.25 | 24/38 (63.2) | 0.76 | χ2 |
| BMI, median (range) | 29.4 (17.3-45.1) | 29.4 (19.4-46.9) | 1.0 | 28.8 (20.3-51.9) | 1.0 | Mann-Whitney U test |
| ASA Score, median | 2 | 2 | 0.23 | 2 | 0.80 | χ2 |
| ASA Score I, n (%) | 11 (14.7) | 14 (18.7) | 7 (11.3) | |||
| ASA Score II, n (%) | 46 (61.3%) | 49 (65.3%) | 38 (61.3) | |||
| ASA Score III, n (%) | 18 (24%) | 10 (13.3%) | 17 (27.4) | |||
| Pre-operative TFA, mean (95%CI) | 1.2 valgus (0.5 varus–2.4 valgus) | 0.1 varus (1.2 varus–1.0 valgus) | 0.12 | 0.4 varus (1.7 varus–0.9 valgus) | 0.076 | Unpaired T-test |
| Varus Outliers, n (%) | 47 (62.7) | 55 (73.3) | 50 (80.6) | |||
| Valgus Outliers, n (%) | 5 (6.7) | 2 (2.7) | 2 (3.3) |
| Control group | Introduction group | P value (Control vs Introduction) | Follow-up group | P value (Control vs Follow-up) | Test | |
| Tibial AP-alignment, mean (95%CI) | 88.5 (88.1-88.9) | 88.5 (88.1-88.9) | 0.68 | 88.5 (88.1-88.8) | 1.0 | Mann-Whitney U test |
| Outliers, n (%) | 11 (14.7) | 10 (13.3) | 0.81 | 10 (16.1) | 0.81 | χ2 |
| Femoral AP-alignment, mean (95%CI) | 96.0 (95.5-96.5) | 95.4 (95.0-95.8) | 0.06 | 95.6 (95.2-96.0) | 0.22 | Unpaired T-test |
| Outliers, n (%) | 21 (28) | 14 (18.7) | 0.18 | 11 (17.7) | 0.16 | χ2 |
| Post-operative TFA, mean (95%CI) | 4.4 valgus (3.8-5.0) | 3.8 valgus (3.3-4.4) | 0.16 | 4.2 valgus (3.6-4.8) | 0.62 | Unpaired T-test |
| Outliers, n (%) | 25 (33.3) | 26 (34.7) | 0.86 | 23 (37.1) | 0.65 | χ2 |
| Medial Tibial Overhang, n (%) | 5 (6.7) | 8 (10.7) | 0.38 | 6 (9.7) | 0.52 | χ2 |
| Lateral Tibial Overhang, n (%) | 6 (8.0) | 7 (9.3) | 0.77 | 4 (6.5) | 0.73 | χ2 |
| Tibial Slope, mean (95%CI) | 88.8 (88.2-89.4) | 85.1 (84.4-85.8) | < 0.0001 | 84.9 (84.2-85.5) | < 0.0001 | Unpaired T-test |
| Outliers, n (%) | 21 (28.0) | 13 (17.3) | 0.12 | 12 (19.4) | 0.24 | χ2 |
| Femoral Flexion (FF), mean (95%CI) | 86.2 (85.3-87.0) | 88.2 (87.8-88.7) | < 0.0001 | 88.2 (87.8-88.6) | < 0.0001 | Unpaired T-test |
| Outliers, n (%) | 44 (58.7) | 28 (37.3) | 0.009 | 16 (25.8) | < 0.0001 | χ2 |
| Control group | Introduction group | P value (Control vs Introduction) | Follow-up group | P value (Control vs Follow-up) | Test | |
| Length of operation, mean (95%CI) | 50 min (48-52) | 64 min (62-67) | < 0.0001 | 59 min (57-61) | < 0.0001 | Unpaired T test |
| Length of stay, median (range) | 2 d (0-5) | 1 d (0-3) | 0.24 | 1 d (0-9) | 0.032 | Mann-Whitney U test |
| Intra-operative blood loss, median (range) | 200 mL (0-500) | 250 mL (20-1200) | 0.002 | 200 mL (50-1150) | 0.84 | Mann-Whitney U test |
| Intra-operative complications, n (%) | 0 (0) | 1 (1.3) | 1.0 | 0 (0) | 1.0 | Fisher’s exact t-test |
| Readmissions within 90 d, n (%) | 9 (12) | 12 (16) | 0.56 | 7 (11.3) | 0.83 | χ2 |
| Deaths within 90 d, n (%) | 0 (0) | 0 (0) | 1.0 | 0 (0) | 1.0 | Fisher’s exact t-test |
Changes in the mentioned surgery-related factors and early outcome were compared between the three groups. The alignment measurements were compared and analyzed with respect to the gold standard of optimal component placement[13]. Optimal alignment was therefore characterized as follows: TFA = 3-7.5° valgus, femoral component AP alignment: 83-88°, tibial component AP alignment: 87-93°, femoral flexion: 87-90°, and tibial slope: 83-90°. For AP alignment, femoral and tibial components, < 90 degrees corresponds to varus placement and > 90 degrees corresponds to valgus placement. Any alignment outside the optimal alignment interval was considered an outlier. Tibial overhang was recorded if overhang measured 1 mm. All measurements were performed by the main authors using Orthopedic Tools add-on built into Impax Client software.
The use of knee systems other than the newly introduced system (AGC Total Knee System or Vanguard CR Total Knee System, Zimmer Biomet, Warsaw, Indiana, United States) for patients receiving primary unilateral TKAs during the time period encompassing either the Introduction Group or Follow-up Group was registered. The data on the use of alternative TKA systems were subsequently used to develop a perspective on the surgeon-specific adaptation rate to the novel system (Table 4).
| Introduction group | Follow-up group | |
| Orthopedic Surgeon 1, n (%) | 25 out of 36 (69.4) | 25 out of 35 (71.4) |
| Orthopedic Surgeon 2, n (%) | 25 out of 47 (53.2) | 25 out of 46 (54.3) |
| Orthopedic Surgeon 3, n (%) | 25 out of 55 (45.4) | 12 out of 16 (75) |
Continuous data were presented as means with standard deviations (SD) or as medians with range, and categorical data as absolute numbers and percentages (%) or medians. For comparison of variables between age groups, the Student’s t-test, Pearson’s Chi squared test (χ²-test) or the Mann Whitney U test were applied when appropriate. SPSS Statistics Software version 25.0 was used. P values less than 0.05 were considered statistically significant.
No approval from the National Ethics Committee was necessary as this was a non-interventional observational study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Permission to store and review patient data was obtained from the Danish Data Protection Agency Jr, No. 2007-58-0015.
No significant demographic differences between the three groups were found, aside from a significant discrepancy in the mean age of patients in the Introduction Group, who were 4.5 years younger than the controls (P = 0.009) (Table 1).
Immediately after introduction of the novel implant, the Persona TKA system was utilized in 69%, 53%, and 45% of primary TKA procedures by the three surgeons at our institution. In the Follow-up Group the Persona TKA was utilized in 71%, 54%, and 75% by the respective surgeons (Table 2). Remaining knees in either period were treated with one of the former TKA standards (AGC- or Vanguard TKA).
Mean operation time significantly increased from 50 to 64 min subsequent to introduction of the Persona TKA system (P < 0.0001), and this increase was still evident in the Follow-up Group (P < 0.0001) although it decreased to 59 min (Table 3). Median intraoperative blood loss significantly increased from 200 mL to 250 mL following the introduction (P = 0.002). This difference disappeared in the Follow-up Group (P = 0.84) (Table 3). Length of stay (LOS) was significantly reduced from 2 d to 1 d (median) exclusively in the Follow-up Group compared with the Control Group (P = 0.032) (Table 3).
The initial learning curve effect on operation time in the first 25 novel TKAs showed signs of a reduction after the initial 5 TKAs in the Introduction Group for each surgeon, with a decline from 70 min (median) in the initial 5 patients for each surgeon to between 65-58 min (Figure 2). However, no signs of an initial learning curve were observed in the first 25 novel TKAs regarding improvements in blood loss management as a function of the surgeon’s experience in the novel system (Figure 3).
Alignment measurements on digital X-rays showed significant differences with respect to the lateral component alignment. Tibial slope (TS) was 88.8-, 85.1- and 84.9 degrees (mean) for the Control, Introduction, and Follow-up Group, respectively (Table 2), with a significantly increased posterior slope for both the Introduction and Follow-up Groups.
Mean FF was 86.2 degrees for the Control Group vs 88.2 degrees for both the Introduction and Follow-up Groups. The number of outliers with respect to FF was reduced in the Introduction Group (37% outliers) and reduced further in the Follow-up Group (26% outliers) when compared to patients in the Control Group (59% outliers). No significant changes in TS outliers were observed. No differences in medial- and lateral tibial overhang were found (Table 2).
In this study, 212 patients were investigated regarding the implementation of a novel TKA and its influence on perioperative and surgical outcomes. An increase in operation time of 14 min (from 50 min to 64 min) was seen immediately after the introduction of this novel TKA system. This increase was still evident, but lower, 1 year after its introduction. Intraoperative blood loss showed a transient rise following its introduction with 50 mL blood loss (+25%), with no difference recorded 1 year after introduction of the system (Table 3).
A reduction in femoral flexion (FF) of 2.0 degrees (from 88.2 to 86.2) resulted in improved optimal overall component placement compared to the Control Group, and significantly reduced the number of FF outliers in the Introduction Group (from 58.7% to 37.3% outliers). The observed reduction in FF outliers was even more pronounced in the Follow-up Group (25.8% outliers). We also found a significantly increased posterior TS following introduction of this system (TS: 85.1 degrees) and Follow-up Group (TS: 84.9 degrees) compared to the Control Group (TS: 88.8 degrees). This also caused a reduction in the number of TS outliers in both groups receiving novel TKAs compared to the Control Group, although the reduction was not significantly different (Table 2).
Appropriate surgical training in the new procedure could help resolve the inexpedient increase in time and blood loss, although Weber et al[14] found no significant differences in outcome between senior and trainee surgeons in TKA surgeries. Their study was, however, a retrospective study with a risk of selection bias, and all trainee surgeons had 2 years of surgical education prior to performing the surgery and were supervised throughout the operation by senior surgeons. Relatedly, a multicenter study examining the learning curve of a novel TKA introduction found no difference in intraoperative outcome and patient reported outcome measures (PROMs), and only a slight increase in operation time[15]. All surgeons in our study were very experienced at performing knee arthroplasty, thus limiting the learning curve. Nevertheless, the changes in surgery time and intraoperative blood loss found in this study do suggest that a learning curve is present even for experienced knee surgeons following the introduction of a novel knee system. Evidence suggesting rapid improvement was observed specifically for surgery time after the first 5 TKAs for each surgeon, while blood loss management showed no signs of improvements in the first 25 TKAs for each surgeon. This suggests that the orthopedic surgeons experience with specific TKA systems affects intraoperative outcome indicators at a different pace (Figure 2 and Figure 3).
Other studies have investigated the role that the introduction of a novel knee system may play on early outcome. A Swedish study found that a poor routine by the surgeon affected surgical outcome and was especially pronounced for technically challenging implants[16]. A nationwide register-based Finnish study examined the ten most common TKA implants at introduction and found large differences in survival and revision risk, and interestingly, 4 of the 10 systems appeared to show a surgeon learning curve at the expense of the first patients who received inferior results[7]. Besides substantiating the plausibility that a wide degree of variance exists between TKA system designs and their ease of use, the study supports our findings as our Follow-up Group showed superiority in both intra- and early postoperative outcomes when compared with the Introduction Group.
It appears that our findings on cemented TKAs were not mirrored when compared to early outcomes following the introduction of a novel cementless TKA system. A small American study by Cohen et al[17] looked at how the introduction of a cementless TKA compared with a conventional cemented TKA system, and found no significant difference in intra-operative blood loss and a 5 min shorter (-11%) operating time for the newly introduced cementless TKA. Their results are in line with available literature on existing TKA systems[18,19], although it should be noted that Cohen et al merely changed the means of fixation of the implants, while our study investigated a complete change of the entire TKA system.
In terms of clinical relevance, we believe our findings of an increase in mean operation time of 14 min in the Introduction Group is clinically significant as it constitutes a 28% mean increase. With 3 and 5 cases daily, this difference adds up to 42 min and 1 h and 10 min, respectively. We believe this to be a direct consequence of more complex instrumentation. The median increase in intra-operative blood loss of 50 mL has little clinical significance for patients, and may partly be the result of increased operation time as it shows a positive correlation with increased blood loss[20].
In recent times the utilization of guides and other navigation have increased the opportunity to intraoperatively control alignment and osseous resections during TKA[21,22]. The Persona implant introduced in this study makes use of bespoke instrumentation and as such offers inherent advantages regarding fit and placement of the femoral and tibial components as opposed to the former AGC and Vanguard systems. This provides an advantage for the surgeon which could explain the improved TS and FF alignment and an approximately 35% reduction in outliers even directly following introduction of the novel TKA system, as several of the critical elements during the procedure have been made easier.
Length of stay (LOS) was significantly shorter only in the Follow-up Group with the median length of stay of 1 d compared to 2 d in the Control Group. However, this finding is most likely unrelated to the implant, as continuous evolvement of the fast-track setup in our institution with continuously decreasing LOS may explain the differences in LOS between the groups[23].
Limitations of this study include the unavailability of PROMs; thus, the longer term outcome of patients in the three groups remains unclear, as we have no reports or evidence to support any viewpoint. Also, the sample size of patients was fundamentally determined by the number of Persona TKAs at our institution, and an orderly power analysis was consequently not applied in the study design. Our study included three surgeons from the same institution as our point of reference, and it is possible that results may vary between hospitals, although a large American study found similar overall readmission rates, LOS and postoperative adverse outcomes in TKA operations between top rated and other hospitals[24].
BMI, gender, pre-operative ASA score and pre-operative tibiofemoral angle were the same for all three groups suggesting homogeneous patient demographics and thus limited selection bias, apart from patients in the Introduction Group who were 4 years (mean) younger that the others, suggesting that surgeons do tend to select a novel (and more expensive system) for younger patients. The strengths of this study lie in the use of the secure local registries which ensure that data is collected unbiasedly. Individual surgeons vary in performance, and by including three surgeons it enabled more general data to be obtained in which the individual surgeon’s performance plays a smaller role.
The introduction of a new TKA implant at our institution increased surgical time and intraoperative blood loss immediately after introduction. These differences decreased one year after introduction of the new implant. Only minor differences were observed with respect to alignment, which mainly constituted improvements in lateral component alignment following introduction of the new system, and these were further pronounced in the follow-up. Further studies are needed to investigate if these differences persist over time and correlate with patient reported outcomes. Surgeons should take increased care when introducing new procedures and consider the logistics when choosing a novel implant as small gains in alignment should be balanced against inferior peri-operative outcomes.
Globally, the use of total knee arthroplasty (TKA) has risen throughout the last 2-3 decades and is projected to increase even further. The introduction of novel implants for TKA is a frequent occurrence with proposed benefits for patients, but is unfortunately sometimes contradicted by evidence of undesirable effects with regard to revision rates, costs, and patient-perceived outcomes. Little information exists on how early surgical outcome and implant positioning are affected following the introduction of a novel TKA system.
This study focused on the early logistical challenges posed by the introduction of a novel TKA system. In particular, the short-term clinical outcomes in patients with emphasis on how surgery-related factors and implant positioning are affected following the introduction of a novel TKA system. The utilization rate across surgeons and how surgical experience with the implant affects outcome were investigated.
This short-term study showed that a learning curve is present even for experienced knee surgeons following the introduction of a novel knee system. Information from this study may help to increase care when introducing new procedures and logistical considerations when choosing a novel implant, as small gains in alignment should be balanced against inferior peri-operative outcomes. These findings will be useful as a basis for comparisons for future studies and correlations with patient reported outcomes.
This retrospective study included 212 TKA patients undergoing surgery at Copenhagen University Hospital Hvidovre. We included 75 consecutive knees treated with the novel TKA system in the introduction period starting from November 30th 2015 immediately following implementation by three experienced surgeons (25 TKAs/surgeon), along with a control group of 75 patients. A Follow-up Group consisting of 62 consecutive knees starting from 365-d after each respective surgeon ended their initial 25 novel TKAs was also included. Patient demographics, surgery-related factors and alignment data were recorded using the institution’s patient registry.
This study examined how early clinical outcome, implant positioning and utilization rate were affected by the introduction of a novel TKA system between August 2015–December 2018, and how increased surgical experience with the implant affected patient outcome. The novel TKA system was utilized in 69% (71%), 53% (54%), and 45% (75%) of primary TKA procedures by the three surgeons, respectively (Follow-up Group). Mean surgery time was increased by 28% and mean intra-operative blood loss by 25% in the Introduction Group, whereas only the mean surgery time was increased in the Follow-up Group by 18%. Small improvements were observed in alignment. FF outliers were reduced in the Introduction Group with a more pronounced decrease in the Follow-up Group.
Little information exists on how early surgical outcome is affected following the introduction of a novel TKA system. This study brings a unique view on short-term outcome following the introduction of a novel TKA system in relation to implant positioning, early clinical outcome and the learning curve. It accounts for variances between surgeons by studying the same experienced orthopedic surgeons throughout the study, as surgical skill, experience, and caseload varies across surgeons. Increased surgical time and intraoperative blood loss was observed immediately after introduction of the new system. These differences diminished one year after introduction of the new implant. Our findings suggest that surgeons should take increased care when introducing new procedures and consider the logistics when choosing a novel implant, as small gains in alignment should be balanced against inferior peri-operative outcomes.
Further studies are needed to investigate if these differences persist over time and correlate with patient reported outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: Denmark
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): E
P-Reviewer: Cui Q, DeSousa K, Emara KM, Prudhon JL S-Editor: Wang DM L-Editor: Webster JR P-Editor: Xing YX
| 1. | Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J. 2011;5:80-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 247] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 2. | Martelli N, Eskenazy D, Déan C, Pineau J, Prognon P, Chatellier G, Sapoval M, Pellerin O. New European Regulation for Medical Devices: What Is Changing? Cardiovasc Intervent Radiol. 2019;42:1272-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Klar E. Medical Device Regulation as current challenge for the legally safe introduction of new technologies. Chirurg. 2018;89:755-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Melvin T, Torre M. New medical device regulations: the regulator's view. EFORT Open Rev. 2019;4:351-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Jenny JY, Miehlke RK, Giurea A. Learning curve in navigated total knee replacement. Knee. 2008;15:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty. J Bone Joint Surg Am. 2007;89:1497-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Peltola M, Malmivaara A, Paavola M. Learning curve for new technology? J Bone Joint Surg Am. 2013;95:2097-2103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Anand R, Graves SE, de Steiger RN, Davidson DC, Ryan P, Miller LN, Cashman K. What is the benefit of introducing new hip and knee prostheses? J Bone Joint Surg Am. 2011;93 Suppl 3:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Peltola M, Malmivaara A, Paavola M. Introducing a knee endoprosthesis model increases risk of early revision surgery. Clin Orthop Relat Res. 2012;470:1711-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Nunley RM, Nam D, Berend KR, Lombardi AV, Dennis DA, Della Valle CJ, Barrack RL. New total knee arthroplasty designs: do young patients notice? Clin Orthop Relat Res. 2015;473:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Suter LG, Paltiel AD, Rome BN, Solomon DH, Thornhill TS, Abrams SK, Katz JN, Losina E. Placing a price on medical device innovation: the example of total knee arthroplasty. PLoS One. 2013;8:e62709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop Suppl. 2012;83:1-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 193] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 13. | Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop. 2014;85:480-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 182] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 14. | Weber M, Worlicek M, Voellner F, Woerner M, Benditz A, Weber D, Grifka J, Renkawitz T. Surgical training does not affect operative time and outcome in total knee arthroplasty. PLoS One. 2018;13:e0197850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Whittaker JP, Dwyer KA, Howard J, Huey V, Lesko J, Nunley RM, Verdonk P. Learning curve with a new primary total knee arthroplasty implant: a multicenter perspective with more than 2000 patients. Arthroplast Today. 2018;4:348-353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Robertsson O, Knutson K, Lewold S, Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001;83:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Cohen RG, Sherman NC, James SL. Early Clinical Outcomes of a New Cementless Total Knee Arthroplasty Design. Orthopedics. 2018;41:e765-e771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Aprato A, Risitano S, Sabatini L, Giachino M, Agati G, Massè A. Cementless total knee arthroplasty. Ann Transl Med. 2016;4:129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 19. | Zhou K, Yu H, Li J, Wang H, Zhou Z, Pei F. No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: A systematic review and meta-analysis. Int J Surg. 2018;53:312-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 20. | Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: an analysis of risk factors. Int Orthop. 2007;31:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 21. | de Steiger RN, Liu YL, Graves SE. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97:635-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 191] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 22. | Jones CW, Jerabek SA. Current Role of Computer Navigation in Total Knee Arthroplasty. J Arthroplasty. 2018;33:1989-1993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 121] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 23. | Gromov K, Kristensen BB, Jørgensen CC, Hansen TB, Kehlet H, Husted H. [Fast-track total knee arthroplasty]. Ugeskr Laeger. 2017;179. [PubMed] |
| 24. | Cram P, Cai X, Lu X, Vaughan-Sarrazin MS, Miller BJ. Total knee arthroplasty outcomes in top-ranked and non-top-ranked orthopedic hospitals: an analysis of Medicare administrative data. Mayo Clin Proc. 2012;87:341-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |