Published online Jan 18, 2020. doi: 10.5312/wjo.v11.i1.68
Peer-review started: May 26, 2019
First decision: August 31, 2019
Revised: September 23, 2019
Accepted: October 27, 2019
Article in press: October 27, 2019
Published online: January 18, 2020
Processing time: 202 Days and 17.9 Hours
To discuss the rare event of spontaneous resolution of a lumbar ganglion cyst, a personal case report and 25 cases culled from the literature were described in detail. We focused on demographic, classification, clinical and radiological findings, treatment, outcome and radiological resolution.
A 51-year-old man presented to our observation with complaints of low back and right leg pain. Lumbar magnetic resonance imaging (MRI). showed a L4-L5 ganglion cyst. The patient was referred to medical therapy and bracing. After 4 wk, he showed a complete resolution of pain. The complete spontaneous resolution of the cyst was demonstrated by the followed-up MRI.
Spontaneous resolution of lumbar ganglion is very rare and only 26 cases, including ours, were reported in literature. Different degrees of biomechanical impairment seem to play a fundamental role in the pathogenesis. Related symptoms are essentially represented by low back and/or radicular pain, without significant neurological disorders. Anti-inflammatory drugs, light unloading exercises and brace could be recommended to administrated pain and decrease facet loads. Mean time for clinical improvement was 7 mo, while MRI disappearance occurred in an average time of 11 mo. Therefore, surgery should be applied when conservative treatment, prolonged at least 6 mo, fails.
Core tip: Our paper is an original study that analyzes in detail and for the first time, on the basis of a personal observation, the clinical and radiological scenario related to the rare spontaneous resolution of a lumbar ganglion cyst. The term “ganglion cyst” was used according to the recent our morphological classification. Discussing natural history and biomechanical features of this pathology, we propose some recommendations that could be adopted in cases with a propensity to spontaneous resolution.
- Citation: Chiarella V, Ramieri A, Giugliano M, Domenicucci M. Rapid spontaneous resolution of lumbar ganglion cysts: A case report. World J Orthop 2020; 11(1): 68-75
- URL: https://www.wjgnet.com/2218-5836/full/v11/i1/68.htm
- DOI: https://dx.doi.org/10.5312/wjo.v11.i1.68
Spinal articular cysts are more frequently found in the lumbar spine and often they are treated by surgical cystectomy, with or without spinal instrumentation. Recently, the term “ganglion” was proposed to identify the pathological entity, together with an original morphological classification to define possible localizations[1]. Remission of this type of cyst after conservative treatment was not so frequently reported in literature[2]. We report a case of clinical and radiological resolution of a symptomatic lumbar ganglion cyst (LGC) after conservative treatment, discussing mechanisms that could have led to its disappearance.
A 51-year-old man presented to our observation with complaints of low back and right leg pain with a L5 dermatomeric distribution.
His disorders persisted from 10 d.
Personal and family history were negative for medical or surgical diseases.
Lasègue test was highly positive, without neurological deficits. Tendon reflexes were normal. Laboratory tests were normal.
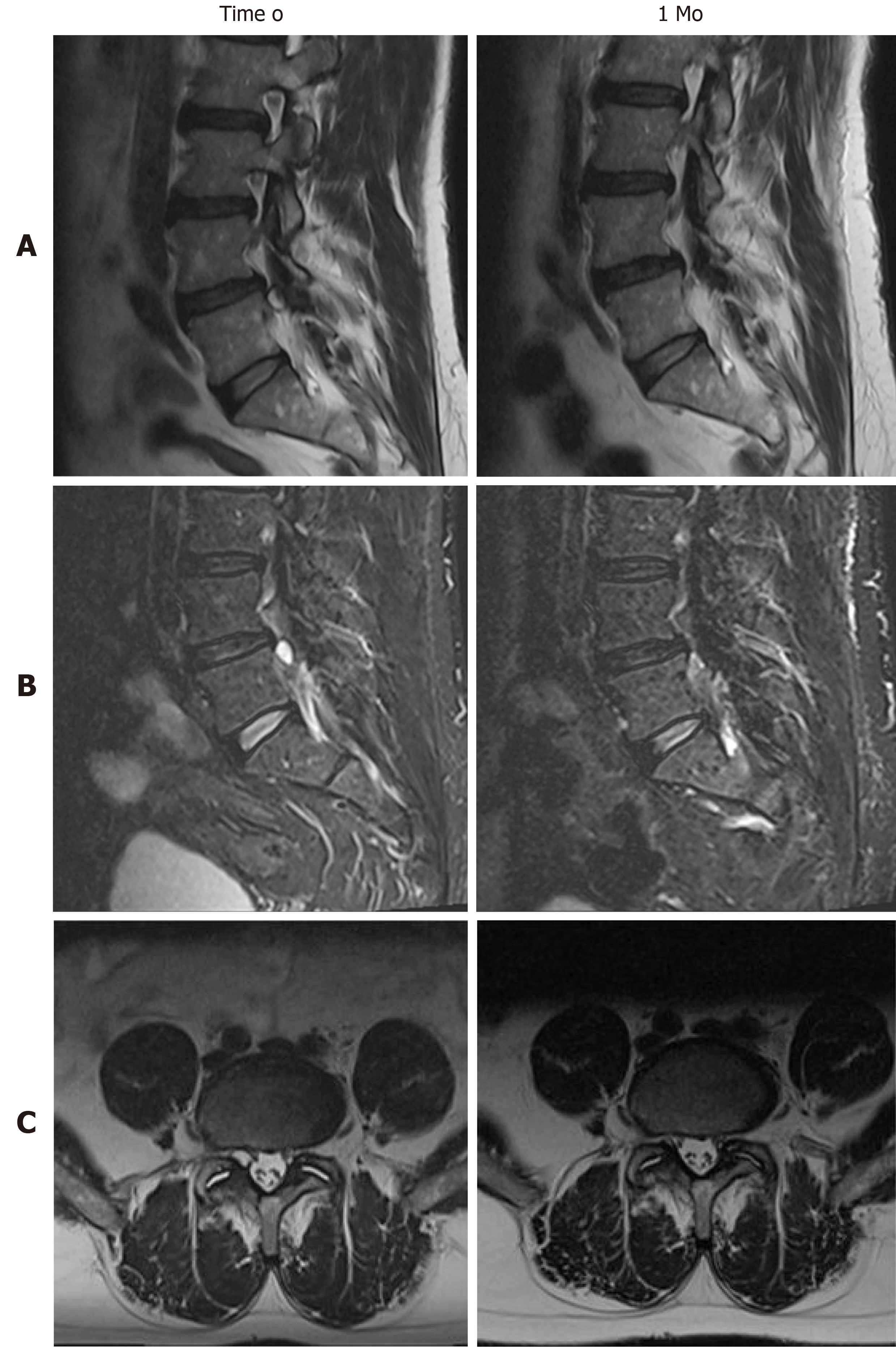
Lumbar MRI showed a cystic lesion in the L4-L5 spinal canal, medial and adjacent to the right internal facet joint, iso-hypointense in T1 and hyperintense in T2-weighted images, compatible with a ganglion cyst.
Final diagnosis was: A symptomatic right L4-L5 LGC.
After discussion on treatment options, the patient was referred to medical therapy, based on NSAID, SAID for 10 d and lumbar bracing. Clinical follow-up was instituted after 4 wk, advising the patient to call us in case of neurological worsening. Surprisingly, 4 wk later, the patient showed complete resolution of the symptoms. We scheduled a new lumbar MRI after 2 d, in order to evaluate the evolution of the lesion. T1 and T2 sequences demonstrated the complete resolution of the LGC as well as compression of the right L5 nerve root (Figure 1).
We conducted a PubMed research on literature published until October 2018. The search was undertaken using the keywords ‘‘lumbar cyst”, “ganglion cyst’’, ‘‘synovial cyst’’, “juxtafacet cyst”, “facet joint cyst”, and “resolution”. References from the retrieved reports were checked to identify other possible results. We enrolled cases with radiological documented remission of LGC and/or clinical improvement after conservative treatment based on rest, lumbar bracing, drugs and/or kinesiotherapy, excluding all those treated by surgery or deep percutaneous procedures (e.g. radiofrequency, epidural injection etc). For every case collected, we analyzed age, sex, symptoms, neurological deficits and treatment received. When radiological data were available, we classified the localization of the LGC following our previous original classification[1] and we searched for the presence of instability signs, even in the follow-up images. Outcome clinical data were classified in 4 categories: (1) Excellent; (2) Good; (3) Fair; or (4) Poor, according to Macnab[3] (Table 1).
| Grade | Criteria |
| Excellent | No pain; no restriction of activity |
| Good | Occasional back or leg pain of sufficient severity to interfere with the patient’s ability to do his normal work |
| Fair | Improved functional capacity, but handicapped by intermittent pain of sufficient severity to curtail or modify work or leisure activities |
| Poor | No improvement or insufficient improvement to enable increase in activities; further operative intervention required |
Demographic, clinical and radiological data were summarized in Table 2. The total number of cases, including ours, was 26. Male: Female ratio was 1.6 (16 males and 10 females) and the mean age was 56 (range 15-75). Most of localizations were in L4-L5 (17; 65%), followed by L5-S1 (6; 23%) and L3-L4 (3; 12%). In 1 case LGCs were bilateral. All classified LGCs (21; 81%) were in the spinal canal and medium: Medium-external in 9 cases (33%), medium-internal in 4 (15%), purely medium in 7 (26%); 1 case (4 %) was purely external (intra-foraminal); in 6 cases (22%) there were no data available to classify the LGC. In all papers the radiological diagnosis was made by MRI, except for 2 cases published before year 2000 in which diagnosis was made by CT scans. Associated spondylolisthesis was detected in 5 (19%) cases, while increased interfacet fluid in 9 (33%). Clinical presentation was constantly characterized by single or double radiculopathy due to irritation of exiting and/or traversing nerve roots. Low back pain accompanied radicular pain 11 times (42%), while pure low back pain was the only symptom in 2 cases (8%). Sensory radicular deficits were identified in 4 cases (15%). There were no cases of motor deficits. Before observation, the mean duration of symptoms was 6.8 mo (range 5 d - 36 mo). When reported (18 cases; 70%), among conservative treatments, a lumbar brace was used in 5 cases (28%), nonsteroidal anti-inflammatory drugs in 13 (72%), corticosteroids in 2 (11%) as well as gabapentin. Rest was recommended in 10 cases (55%), while kinesiotherapy (especially unloading exercises) in 8 (44%). Chiropractic manipulation was performed on 4 patients (22%). Radiological reduction or resolution of the lesion were evaluated by CT or MRI in 21 cases (81%), but in 4 cases images were not available in papers. The mean time for radiological resolution was 11 mo (range 2 d - 48 mo). Signs of instability remained unchanged, except in 2 cases (13%) for reduction of interfacet fluid amount. The mean time for clinical improvement was 7 mo (range 2 d - 24 mo). Final clinical condition was good or excellent in all cases.
| Author/Yr | Age | Sex | Level/ Side | Classification1 | Imaging | Instability | Symptoms | Duration | Deficit | Treat-ment | Imag-ing control/Time | Instability control | Control | Out-come2 | |
| 1 | Mercader et al[2], 1985 | 65 | F | L4-L5/ right | Med-Int | CT | SPL | Rad | 8 mo | \ | Rest-NSAID-KT-brace | CT reduction/3 mo | SPL | 3 mo | Good |
| 2 | Coulier et al[4], 1998 | 47 | F | L4-L5/bilat | Med/ Med | CT | NR | LBP | NR | \ | Brace | CT/20 mo: left resolution, right reduced | NR | 20 mo | Excel-lent |
| 3 | Maezawa et al[5], 2000 | 15 | M | L4-L5/left | Med | MRI | NR | LBP + Rad | 2 mo | \ | Brace | MRI resolution/3 mo | NR | 3 mo | Excel-lent |
| 4 | Houten et al[6], 2003 | 64 | M | L4-L5/ right | NA | MRI | NR | LBP + Rad | 7 mo | \ | Conservative (na) | MRI resolution/1 mo (na images) | NR | 1 mo | Good |
| 5 | 57 | F | L4-L5/left | NA | MRI | NR | Rad | 5 mo | \ | NSAID-gabap-entin | MRI resolution/8 mo (na images) | NR | 8 mo | Good | |
| 6 | 58 | F | L4-L5/left | Med-Ext | MRI | NR | LBP + Rad | 18 mo | \ | Conservative (na) | MRI resolution/4 mo | NR | 4 mo | Good | |
| 7 | Swartz et al[7], 2003 | 58 | F | L5-S1/ right | Med-Ext | MRI | SPL | Rad | 1 mo | \ | Rest-NSAID-KT-brace | MRI resolution/18 mo | SPL | 12 mo | Good |
| 8 | Cox[8], 2005 | 71 | M | L3-L4/ right | NA | MRI | NR | Rad | 6 mo | \ | Rest-NSAID- chiropractic | MRI reduction/9 mo | NR | 9 mo | Good |
| 9 | 59 | F | L4-L5/left | Med-Ext | MRI | IFFa | Rad | NR | \ | Rest-NSAID-chirop-ractic | Not performed | NR | 2 mo | Excellent | |
| 10 | Ewald et al[9], 2005 | 65 | F | L4-L5/ right | Med-Ext | MRI | SPL | Rad | 5 mo | \ | Rest-NSAID-KT | MRI reduction/3 mo | SPL | 3 mo | Good |
| 11 | Illerhaus et al[10], 2005 | 50 | M | L4-L5/ right | Med-Int | MRI | IFFa | LBP + Rad | 12 mo | \ | NSAID-KT | MRI resolution/7 mo | IFFa | 7 mo | Good |
| 12 | Beukelaar et al[11], 2010 | 59 | M | L4-L5/ right | Med | MRI | IFFa | LBP + Rad | 2 mo | L5 S | Conservative (na) | MRI reduction/3 mo | IFFb | 3 mo | Excellent |
| 13 | Bashir et al[12], 2012 | 47 | M | L4-L5/ right | NA | MRI | NR | Rad | 6 mo | \ | Rest-NSAID-KT | Not performed | NR | 24 mo | Excellent |
| 14 | 58 | M | L4-L5/left | Med | MRI | IFFa | Rad | 3 mo | \ | Rest-NSAID-KT | MRI resolution/2 mo (na images) | NR | 2 mo | Excellent | |
| 15 | 41 | M | L5-S1/ right | NA | MRI | NR | Rad | 12 mo | \ | Rest-NSAID-KT | Not performed | NR | 24 mo | Excellent | |
| 16 | Barazi et al[13], 2012 | 48 | F | L4-L5/ right | NA | MRI | NR | Rad | NR | \ | Conservative (na) | MRI resolution/8 mo (na images) | NR | 8 mo | Good |
| 17 | Cox et al[14], 2012 | 75 | M | L3-L4/left | Med-Int | MRI | NR | Rad | 36 mo | \ | Chiropractic | Not performed | NR | 2 mo | Good |
| 18 | Tepe et al[15], 2012 | 64 | M | L5-S1/left | Ext | MRI | SPL | Rad | 2 mo | L5 S | Conservative (na) | MRI reduction/1 yr, resolu-tion/4 yr | SPL | 12 mo | Good |
| 19 | Mattei et al[16], 2012 | 56 | M | L5-S1/ right | Med | MRI | IFFa | Rad | NR | S1 S | NSAID-KT | MRI resolution/13 mo | IFFa | 1 mo | Excellent |
| 20 | Pulhornet al[17], 2012 | 72 | M | L4-L5/ right | Med-Ext | MRI | IFFa | LBP | NR | \ | Conservative (na) | MRI resolution/18 mo | IFFa | 18 mo | Excellent |
| 21 | Ngo et al[18], 2013 | 58 | F | L4-L5/ right | Med-Ext | MRI | NR | LBP + Rad | 5 d | \ | SAID-chiropractic | Not performed | NR | 3 mo | Excellent |
| 22 | Kim et al[19], 2015 | 58 | M | L3-L4/left | Med-Ext | MRI | SPL | LBP + Rad | 4 mo | \ | Conservative (na) | MRI resolution/4 yr | SPL | 1 mo | Excellent |
| 23 | Delen et al[20], 2015 | 63 | M | L5-S1/left | Med | MRI | IFFa | LBP + Rad | 1 mo | S1 S | NSAID-gabapentin | MRI resolution/1 mo | ↑IFF | 1 mo | Excellent |
| 24 | Sinha et al[21], 2016 | 66 | M | L5-S1/left | Med-Int | MRI | NR | LBP + Rad | 12 mo | \ | Conservative (na) | MRI resolution/12 mo | NR | 12 mo | Good |
| 25 | Ucler et al[22], 2017 | 36 | F | L4-L5/ right | Med-Ext | MRI | IFFa | LBP + Rad | 10 d | \ | Rest | MRI resolution/2 d | IFFa | 2 d | Excellent |
| 26 | Our case | 51 | M | L4-L5/ right | Med-Ext | MRI | IFFa | LBP + Rad | 10 d | \ | Rest-NSAID-SAID-brace | MRI resolution/1 mo | IFFb | 1 mo | Excellent |
The number of reported synovial cysts of the lumbar spine have been increasing probably due to the availability of magnetic resonance imaging technique. Recently, the term “ganglion” and a new morphological classification were introduced to identify the pathological entity and its localization[1].
LGCs are usually associated with osteoarthritis of the adjacent facet joint, degenerative spondylosis and/or spondylolisthesis, particularly in middle aged or elderly patients. The majority of such cysts require surgical resection due to persistent radicular symptoms and/or occasional paresis[4], that could be associated to fusion if pre-operative instability is detected[1]. While ganglion cysts elsewhere (e.g. the wrist) spontaneously resolve in 40% of patients, the spontaneous resolution of root compression with radiological disappearance of LGC were rarely reported in literature.
We collected 24 cases from the literature[2,4,5] that affected the adult lumbar spine in adults and one more in the adolescent spine (Table 2)[6-22]. All ganglia, detected by CT or MRI and classified according to Domenicucci et al[1], were in the spinal canal and in medium position (95% of cases), except one reported by Tepe et al[15] that was purely external. Most were associated to indirect signs of segmental hypermobility (e.g. increase of synovial fluid) or proper instability. They were able to give, exiting and/or transiting nerve roots, irritation and compression, with prevalently single radiculopathy but without significant neurological deficits. Their resolution, demonstrated by radiological follow-up in 17 cases (68%), was always associated to substantial clinical improvement or full recovery. Indirect radiological signs of segmental instability remained unchanged after resolution, except in one case[10] in which occurred the reduction of interfacet synovial fluid amount, similar to our MRI follow-up findings.
Explaining the spontaneous resolution of LGC is complicated, in part because of the high prevalence of surgical removal. Some authors have supported the thesis that progressive degenerative changes of the facet joint lead to fixation of the previously hypermobile facets, so that intra-articular pressure decreases and the cyst shrinks[6]. The cyst may also undergo degenerative changes, losing connection with the facet joint and resolving because of a lack of supply[9]. Other possible causes for resolution include rupture, as seen in other different articular districts of the human body, with the extrusion of its contents, followed by reabsorption of the cystic wall[7]; or reduction of the local intra-articular forces that contributed to synovial herniation through the facet joint capsule. The last hypothesis could be supplied by the antigravitary lumbar bracing or unloading exercises usage in most cases described, including ours (11/19; 58%). Also chiropractic manipulations seemed clinically effective[14,18], though only one paper[8] showed the radiological resolution of the cyst. So, in our patient, who underwent treatment with NSAIDs, corticosteroids and lumbo-sacral bracing, LGC probably resolved because of the association between decreased inflammatory fluid production and microtraumatic loads.
An early clinical and radiological remission as ours is referred in only 2 cases[20,22]. Two fast clinical resolutions were previously reported, but without radiological confirmation of the cyst reabsorption[6,18]. Other two early clinical improvement were described, but radiological resolution was achieved after over one year[16,19]. Generally, clinical improvement and radiological remission occurred on average respectively in 7 and 11 mo.
The natural history of spinal ganglion cysts is unknown and there is scant literature involving their non-surgical therapy. In the lumbar spine, different degrees of biomechanical impairment seem to play a fundamental role in their pathogenesis, but LGCs should be considered as dynamic entities. In other words, formation and resolution appear strictly influenced by event and regression of inflammatory and mechanical phenomena.
Although rarely, the symptoms related to LGC, essentially represented by low back and/or radicular pain, could regress spontaneously, if cystic evolution (enlargement, hemorrhage, worsening of spondylolisthesis) with associated worsening of neurological status does not occur.
Our case is the twenty-sixth in literature. Based on our experience and reviewing data, we can suggest that in case of absence of neurological deficits and in selected compliant patients, percutaneous procedures or surgery should be considered when conservative treatment, consisting of rest, pharmacological therapy, kinesiotherapy and/or lumbar bracing, prolonged at least for 6 mo, fails to produce symptoms control. We recommend, anti-inflammatory drugs and light unloading exercises to control pain and reduce intra-cystic fluid, but also rest and lumbar bracing to achieve the decrease of loads on arthritic facets. We also recommend MRI confirmation of cyst resolution, which can be helpful to understand mechanisms responsible of resolution.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kahveci R, Li S, Peng BG S-Editor: Zhang L L-Editor: A E-Editor: Liu MY
| 1. | Domenicucci M, Ramieri A, Marruzzo D, Missori P, Miscusi M, Tarantino R, Delfini R. Lumbar ganglion cyst: Nosology, surgical management and proposal of a new classification based on 34 personal cases and literature review. World J Orthop. 2017;8:697-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Mercader J, Muñoz Gomez J, Cardenal C. Intraspinal synovial cyst: diagnosis by CT. Follow-up and spontaneous remission. Neuroradiology. 1985;27:346-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53:891-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 552] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 4. | Coulier B, Ghosez JP, Mailleux P. Computed tomography diagnosis of clinically well-tolerated bilateral lumbar vertebral synovial cysts. JBR-BTR. 1998;81:141-143. |
| 5. | Maezawa Y, Baba H, Uchida K, Furusawa N, Kubota C, Yoshizawa K. Spontaneous remission of a solitary intraspinal synovial cyst of the lumbar spine. Eur Spine J. 2000;9:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Houten JK, Sanderson SP, Cooper PR. Spontaneous regression of symptomatic lumbar synovial cysts. Report of three cases. J Neurosurg. 2003;99:235-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Swartz PG, Murtagh FR. Spontaneous resolution of an intraspinal synovial cyst. AJNR Am J Neuroradiol. 2003;24:1261-1263. [PubMed] |
| 8. | Cox JM, Cox JM 2nd. Chiropractic treatment of lumbar spine synovial cysts: a report of two cases. J Manipulative Physiol Ther. 2005;28:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ewald C, Kalff R. Resolution of a synovial cyst of the lumbar spine without surgical therapy -- a case report. Zentralbl Neurochir. 2005;66:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Illerhaus B, Scholz M, Pechlivanis I, Gries N, König M, Harders A. [MRT follow-up study of spontaneous regression of lumbar articular facet cyst]. Rofo. 2005;177:1717-1719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | de Beukelaar JW, Dallenga A, de Jong GJ, de Winter KJ, Bakker SL. [Juxta facet cyst of the lumbar spine: an uncommon cause of lumbar radiculopathy]. Ned Tijdschr Geneeskd. 2010;154:A1673. [PubMed] |
| 12. | Bashir el F, Ajani O. Management of lumbar spine juxtafacet cysts. World Neurosurg. 2012;77:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Barazi S, D’Urso P, Thomas N. Concomitant Spontaneous Resolution and Appearance of a New Contralateral Lumbar Synovial Cyst: Case Report. J Neurol Surg Part A Cent Eur Neurosurg. 2012;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Cox JM. Chiropractic management of a patient with lumbar spine pain due to synovial cyst: a case report. J Chiropr Med. 2012;11:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Tepe S, Kara M, Iplikcioglu AC. Spontaneous Disappearance of Lumbar Synovial Cyst. J Neurological Sciences. 2012;29:154-158. |
| 16. | Mattei TA, Goulart CR, McCall TD. Pathophysiology of regression of synovial cysts of the lumbar spine: the ‘anti-inflammatory hypothesis’. Med Hypotheses. 2012;79:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Pulhorn H, Murphy M. Spontaneous resolution of a symptomatic synovial cyst of the lumbar spine. Br J Neurosurg. 2012;26:123-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Ngo T, Decina P, Hsu W. Spontaneous resolution of symptoms associated with a facet synovial cyst in an adult female - a case report. J Can Chiropr Assoc. 2013;57:87-92. [PubMed] |
| 19. | Kim HS, Ju CI, Kim SW, Kim SH. Contralateral Juxtafacet Cyst Development after the Spontaneous Resolution of a Previous Facet Cyst. J Korean Neurosurg Soc. 2015;58:563-565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Delen E, Tütüncüler B, Akıncı AT, Kunduracılar M. Spontaneous Regression of a Symptomatic Lumbar Facet Synovial Cyst in One Month. Sch J Appl Med Sci. 2015;3:1587-1589. |
| 21. | Sinha P, Panbehchi S, Lee MT, Parekh T, Pal D. Spontaneous resolution of symptomatic lumbar synovial cyst. J Surg Case Rep. 2016;2016:rjw166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Ucler N, Ozturk S, Gulkesen A, Kaplan M. Rapid spontaneous regression of a lumbar juxta-facet cyst. Neurol India. 2017;65:417-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |