Published online Feb 18, 2019. doi: 10.5312/wjo.v10.i2.101
Peer-review started: September 12, 2018
First decision: October 5, 2018
Revised: November 3, 2018
Accepted: January 10, 2019
Article in press: January 10, 2019
Published online: February 18, 2019
Processing time: 159 Days and 7.9 Hours
Scaphoid fracture is the most commonly fractured carpal bone in the athletic patient, accounting for over 85% of all sport-related carpal bone fractures, and is particularly common in sports involving high impact injuries to the wrist. The management of such injuries comprises both conservative and surgical techniques, as guided by fracture location and type. Athletes demonstrate a unique challenge with regards to the management of scaphoid fractures due to their requirement to return to sport, as soon as able.
To review systemically all studies recording return to sport following scaphoid fractures, to collate information on return rates to sport (RRS) and mean return times (RTS) to sport and to determine differences in sporting outcome for the various treatment methods.
A systematic search of MEDLINE, EMBASE, CINAHAL, Cochrane, Google Scholar, Physiotherapy Evidence Database, SPORTDiscus, Web of Science and Scopus was performed in August 2018 using the keywords “scaphoid”, “fracture”, “acute”, “carpal”, “athletes”, “sports”, “non-operative”, “conservative”, “operative” and “return to sport”. All studies that recorded RRS and RTS following scaphoid fractures were included. RTS was recorded as the length of time from commencement of either primary conservative management or primary surgical procedure to return to sport.
Eleven studies were included: Two randomised controlled trials, six retrospective cohort studies and three case series. Seven studies reported on conservative management (n = 77), and eight studies reported on surgical management (n = 83). For conservative management, RRS was 90% (69/77), and the mean RTS was 9.6 wk. Three studies allowed to return to sport in cast [RRS 89% (25/28); RTS 1.9 wk], and four studies required completion of cast treatment prior to returning to sport [RRS 90% (44/49); RTS 13.9 wk]. Four studies recorded fracture union data: Union rate 85% (47/55); mean time to union 14.0 wk. For surgical management, RRS was 98% (81/83), and RTS was 7.3 wk. Three studies reported on Percutaneous Screw Fixation [RRS 97% (32/33); RTS 6.5 wk], and five studies reported on Open Reduction Internal Fixation [RRS 98% (49/50); RTS 7.9 wk]. Six studies recorded fracture union data: Union rate 97% (69/71); mean time to union 9.8 wk. On meta-analysis, RRS (RR = 1.09; 95% confidence interval (CI): 1.00-1.18; P < 0.045), RTS (MD 2.3 wk; 95%CI: 0.79-3.87; P < 0.002), union rates (RR = 1.14; 95%CI: 1.01-1.28; P < 0.030) and mean times to union (MD 4.2 wk; 95%CI: 3.94-4.36; P < 0.001) were all significantly better for the surgical cohort compared to the conservative cohort.
Surgical management of scaphoid fractures can provide significantly improved RRS and RTS to sport compared to conservative management. Both treatments, however, remain acceptable options, and athletes should be fully informed of the benefits and risks of both prior to deciding treatment plans. Immediate return to sport in a cast should be avoided due to the significant risk of non-union.
Core tip: We recorded returned rates (RRS) and return times (RTS) to sport following acute scaphoid fractures. Eleven studies were included. Seven studies reported on conservative treatment (n = 77); eight studies reported on surgical treatment (n = 83). For conservative management, RRS was 90% (69/77), and RTS was 9.6 wk. For surgical management, RRS was 98% (81/83), and RTS was 7.3 wk. On meta-analysis, RRS (P < 0.045) and RTS (P < 0.002) were significantly better for surgical management compared to conservative management. Surgical management of acute scaphoid fractures can provide significantly improved RRS and RTS compared to conservative management.
- Citation: Goffin JS, Liao Q, Robertson GA. Return to sport following scaphoid fractures: A systematic review and meta-analysis. World J Orthop 2019; 10(2): 101-114
- URL: https://www.wjgnet.com/2218-5836/full/v10/i2/101.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i2.101
The scaphoid is the most commonly fractured carpal bone in the athletic patient, occurring a rate of 0.06 per 1000 population and accounting for over 85% of all sport-related carpal bone fractures[1]. These fractures usually arise from a fall onto a hyperextended wrist, resulting in longitudinal loading of the scaphoid and a subsequent failure of the dorsal cortex on compression[2]. The scaphoid is at particular risk from sports involving high impact injuries to the wrist, such as football, rugby and basketball[1].
Clinicians should have a high index of suspicion in athletes presenting with post-traumatic pain on the radial aspect of the wrist or in the anatomical snuffbox region[3]. Sensitive examination findings include tenderness in the anatomical snuffbox, scaphoid tubercle and pain on longitudinal compression of the thumb[4]. Clinically, this fracture can be difficult to diagnose and may not become visible until repeated scaphoid view radiographs are obtained[3]. When negative, the second line imaging is either magnetic resonance imaging or computed tomography scan: This is particularly valuable when considering return to sport in affected athletes[5,6].
These fractures can be divided according to their location (proximal third; waist or middle third; distal third), fracture displacement (undisplaced or minimally displaced; displaced) and fracture stability[3]. The Herbert Classification is the most common classification, which groups scaphoid fractures into stable (A) and unstable fractures (B)[7]. Stable fracture patterns include those of the scaphoid tubercle (A1) and incomplete fractures through the scaphoid waist (A2). Unstable fracture patterns include distal oblique fractures (B1), complete waist fractures (B2), proximal pole fractures (B3), transscaphoid perilunate dislocation (B4) and comminuted fractures (B5)[7].
Management of these injuries is based on the location and nature of the fracture[3]. Undisplaced stable fractures (A1 and A2) are routinely treated conservatively with a scaphoid or forearm cast for 8 wk to 12 wk, until the fracture unites[3,8]. Due to the risk of non-union and avascular necrosis, displaced fractures are treated surgically with open reduction and internal fixation[3]. Occasionally, displaced distal fractures of the scaphoid tubercle, which are symptomatic, can be treated with surgical excision[3]. The treatment of undisplaced unstable fractures remains controversial: Some clinicians advise conservative management with a scaphoid or forearm cast for 8 to 12 wk; while others recommend surgical management with internal screw fixation (often feasible through a percutaneous approach)[3,9]. Previous studies have demonstrated an earlier return to sport when comparing surgical to conservative management for undisplaced unstable fractures of the scaphoid waist: However, treatment practises of these injuries still remain varied among clinicians[9-11]. Athletes demonstrate a unique challenge with regards to the management of such fractures due to their requirement to return to sport as quickly as possible[12].
The aim of this review was to assess systemically all studies recording return to sport following scaphoid fractures, allowing collation of information on return rates to sport (RRS) and mean return times to sport (RTS), and determining differences in sporting outcome for the various treatment methods.
The authors performed a systematic literature review in August 2018 using the listed databases: CINAHAL, Cochrane Collaboration Database, EMBASE, Google Scholar, Medline (PubMed), Physiotherapy Evidence Database, Scopus and Web of Science and SPORTDiscus. The search was limited to peer-reviewed articles in the English language that reported on rates and times of return to sports following acute scaphoid fractures. The key terms used for the search in each database included “scaphoid”, “fracture”, “acute”, “carpal”, “sports”, “athletes”, “non-operative”, “conservative”, “operative” and “return to sport”. All available studies were included for review with no restrictions on publication year.
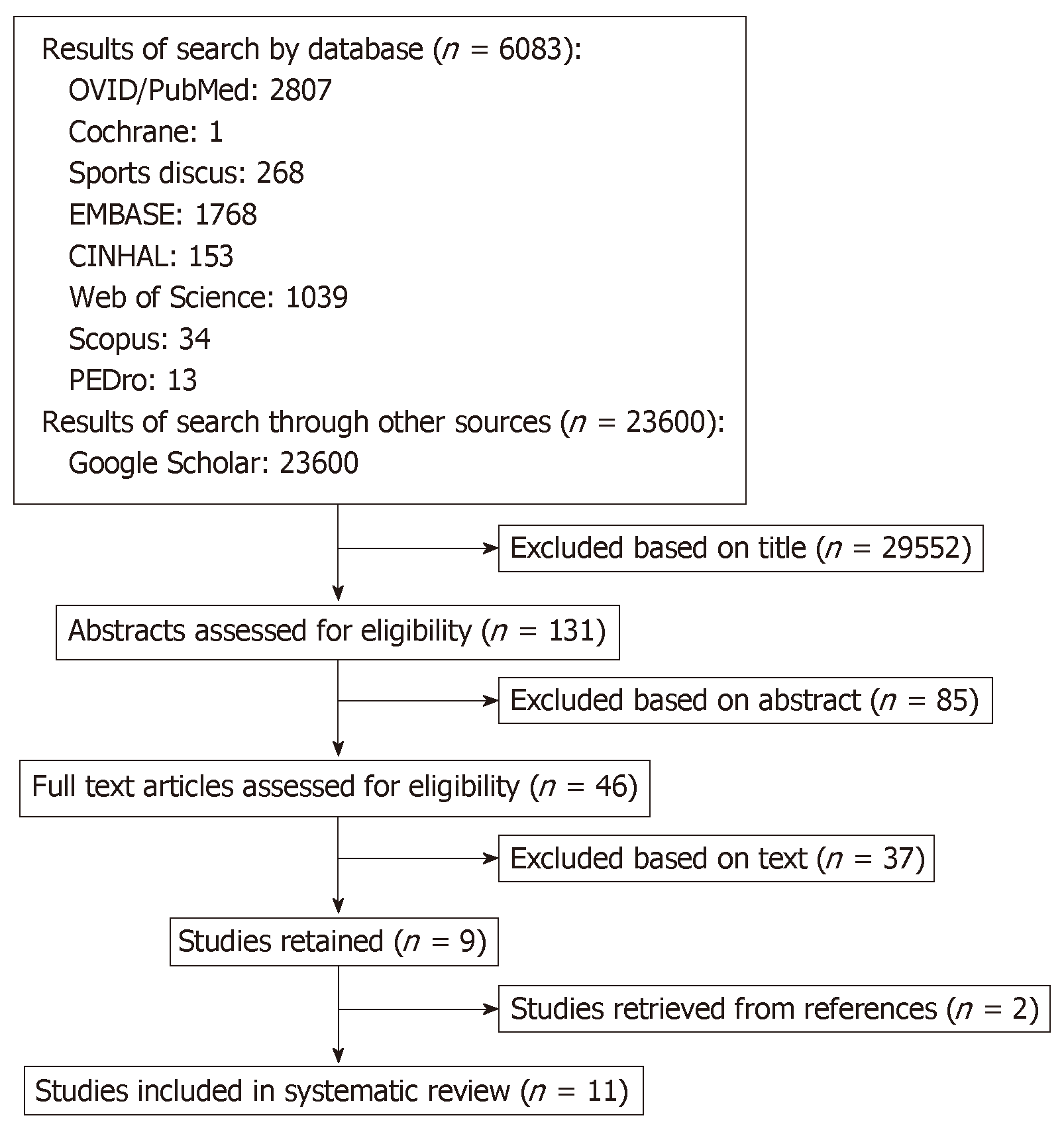
All three authors performed an independent review of the retrieved titles and the subsequently selected abstracts, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines[13]. Table 1 records the inclusion and exclusion criteria as per the PRISMA guidelines. Abstracts, anecdotal articles, case reports, review articles, animal, cadaver and in vitro studies were all excluded from the review unless they contained relevant clinical information. The full-text article was downloaded when exclusion could not be established from review of the abstract alone. The reference lists of the retrieved articles were also assessed to identify further studies for inclusion. Disagreements in study selection for inclusion in this review were to be resolved through consensus discussion between the three authors: There were, however, no major disagreements. Figure 1 summarises the selection process for the review, as per the PRISMA guidelines.
| Inclusion criteria | Exclusion criteria |
| Acute scaphoid fractures | Scaphoid Fracture Delayed Union or Non-Union |
| Elite or recreational athletes | No sporting outcome data reported |
| Return rates to sporting activity reported | Paediatric fractures (age under 15) |
| Time to return to sporting activity reported | Concomitant upper or lower limb fractures |
| Two or more fractures reported | Reviews, case reports, abstracts or anecdotal articles |
| Peer-reviewed journals | Animal, cadaver or in vitro studies |
| English language |
The following data were extracted from the included studies: general patient demographics; mechanism of injury; fracture location; conservative and surgical management methods; return rates and return times to sport; return rate to pre-injury level of sport; rate of fracture union; time to fracture union and complications. The primary outcome measures were RRS and RTS. Secondary outcome measures included rates of return to pre-injury level of sport, fracture union rate, time to fracture union and complications following treatment. Return to pre-injury level of sport was defined as the ability of the athlete to return to their previous level of play (i.e., to the same competitive standard as pre-injury).
For conservatively-managed patients, RTS was recorded as the time length from commencement of conservative management to return to sport. For surgically managed patients, RTS was recorded as the time length from the primary surgical procedure to return to sport.
When a patient was unable to return to sport from the primary treatment technique, requiring conversion to a secondary treatment, this was recorded as a non-return to sport.
The modified Coleman methodology score (CMS) was employed to determine the quality of the included studies[14]: This has been used in a number of similar reviews[15-20]. The studies were scored by all three authors: the inter-observer reliability of the scoring process was 0.92 (95% confidence interval (CI): 0.90–0.94).
Meta-analysis comparisons were performed on cohorts for the following variables: RRS, RTS, rate of fracture union and time to fracture union. These were processed using RevMan Version 5.3 (The Cochrane Group). To assess comparisons between dichotomous data, risk ratios (RRs) with a random effects model were utilised. To assess comparisons between continuous data, mean differences (MDs) with a random effects model were utilised. The I2 statistic was used to analyse the heterogeneity of the included studies: This was significant when I2 was greater than 50%. The significance level was identified as P < 0.05.
The process of study selection is reported in Figure 1. In total, 46 unique abstracts and 11 unique articles were assessed. The search strategy yielded 11 relevant publications, published from 1979 to 2014, with data available on clinical and functional outcomes of patients who returned to sports activity after sustaining an acute scaphoid fracture[9,10,21-29]. There were two randomised controlled trials[9,10], six retrospective cohort studies[21-26] and three case series[27-29].
Table 2 summarises the characteristics of the articles included in this review. The table contains information on study location, patient demographics including gender and age, fracture type/location, management methods, sporting activities reported and level of sport.
| Ref. | Study location | n | Fracture type/ location | Gender (count) | Mean age | Study design | Treatment | Sport activity | Level of sport |
| Adolfsson et al[10] (2001) | Linkoping & Lund, Sweden | 5 | Waist (5) | N/A | 31 (15-75) | RCT | PSF (3); Conservative (2) | Soccer (3); Swimming (1); Squash (1) | National level |
| Bedi et al[25] (2007) | Ann Arbor, Michigan, United States | 6 | B2 (6) | N/A | 25 (16-62) | RCS | ORIF (6) | Sport (6) | Collegiate/ Professional |
| Ellsasser and Stein[27] (1979) | St. Louis, Missouri, United States | 2 | - | M: 2 | N/A | CS | Conservative (2); Returned immediately | American football (2) | Professional |
| Huene[28] (1979) | Fresno, California, United States | 4 | - | N/A | N/A | CS | ORIF (4) | Sport (4) | N/A |
| McQueen et al[9] (2008) | Edinburgh, United Kingdom | 55 | B1 (1); B2 (54) | M: 50 F: 10 | 29.4 (17-65) | RCT | PSF (28); Conservative (27) | N/A | N/A |
| Muramatsu et al[24] (2002) | Yamaguchi, Japan | 10 | A2 (3); B2 (6); B3 (1) | M: 10 | 17.3 (13-22) | RCS | ORIF (10) | Badminton (1); Baseball (2); Basketball (2); Boxing (2); Handball (1); Judo (2); Rugby (1); Soccer (16); Tennis (1); Track (2) | N/A |
| Rettig et al[22] (1994) | Indianapolis, Indiana, United States | 30 | MT (30) | M: 25 F: 5 | 18.3 | RCS | ORIF (18); Conservative (12); Returned immediately | Sport (30) | N/A |
| Rettig and Kollias[23] (1996) | Indianapolis, Indiana, United States | 12 | MT (10) PT (2) | M: 11 F: 1 | 21 (17-31) | RCS | ORIF (12) | Baseball (2); Basketball (8); Archery (2) | N/A |
| Riester et al[21] (1985) | Syracuse, New York, United States | 14 | MT (11) PT (3) | M: 13 F: 1 | N/A | RCS | Conservative (14); Returned immediately | American Football (12); Basketball (1); Soccer (1) | Intercollegiate/ High school |
| Robertson et al[26] (2012) | Edinburgh, United Kingdom | 20 | MT (11); PT (4); DT (5) | M: 20 | 26.1 | RCS | PSF (2); Conservative (18) | Soccer (20) | N/A |
| Robertson et al[29] (2014) | Edinburgh, United Kingdom | 2 | MT (1); DT (1) | M: 2 | 21 | CS | Conservative (2) | Rugby (2) | N/A |
Of the 170 fractures, 131 (77%) occurred in male patients, 13 (8%) in female patients and 26 (15%) failed to specify gender. Of the 170 fractures recorded, follow-up data were achieved for 160 (94.1%). The mean age at the time of injury ranged from 17.3 years[24] to 31.0 years[10]. The most common recorded sports were American football, soccer, baseball and basketball (Table 2).
Four studies described fracture configuration using a formal fracture classification[9,10,24,25]: all four used the Herbert Classification[9,10,21-25]. Three studies recorded fracture location without using a formal classification[21-23]. Four studies failed to report on fracture location[26-29].
The reported fracture types comprised waist/middle third (n = 68), proximal third (n = 9), distal third (n = 6), Herbert A2 (n = 3), Herbert B1 (n = 1), Herbert B2 (n = 66) and Herbert B3 (n = 1). There was no avulsion fracture recorded in the studies.
The CMS for all the studies was 59.5 (range 42-82) (Table 3)[9,10,21-29]. The CMS was 58.6 for the studies reporting on conservative management (range 42-82) (Table 3)[9,10,21,22,26,27,29]. The CMS was 62.9 for the studies reporting on surgical management (range 44-82) (Table 3)[9,10,22-26,28].
| Ref. | n | Mean follow-up | Coleman score | Return Rate | Return rate by treatment modality | Return rate to same level of sport | Return time (range) | Return time (range) by treatment modality | Rate of union | Time to union (range) | Complications by treatment modality |
| Adolfsson et al[10] (2001) | 5 | - | 70 | 5/5 | C: 2/2; S: 3/3 | C: 2/2; S: 3/3 | 8.2 (6-12) wk | C: 11.5 (11-12) wk; S: 6 wk | C: 2/2; S: 3/3 | C: N/A; S: N/A | C: Persistent radial border wrist pain (1); S: Nil |
| Bedi et al[25] (2007) | 6 | 98 (12-272) wk | 64 | 5/6 | S: 5/6 | S: 5/6 | N/A | S: N/A | S: N/A | S: N/A | S: Non-union (6%) ; Scar sensitivity (6%) |
| Ellsasser & Stein[27] (1979) | 2 | - | 42 | 2/2 | C: 2/2 | C: 2/2 | 0 wk | C: 0 wk | S: N/A | S: N/A | C: Nil |
| Huene[28] (1979) | 4 | - | 48 | 4/4 | S: 4/4 | S: 4/4 | 7 (6-8) wk | S: 7 (6-8) wk | S: N/A | S: N/A | S: SRNN (40%) |
| McQueen et al[9] (2008) | 55 | 1 yr | 82 | 53/55 | C: 26/27; S: 27/28 | C: 26/27; S: 27/28 | 10.9 (2-26) wk | C: 15.5 (6-26) wk; S: 6.4 (2-20) wk | C: 23/27; S: 27/28 | C: 13.9 (8-36) wk; S: 9.2 (8-18) wk | C: Non-union (4); Malunion (3); AVN (2); CRPS (1); Radioscaphoid OA(1); S: Peri-operative breakage of the cannulated screwdriver (2) Symptomatic metalwork (1); Non-union (1) |
| Muramatsu et al[24] (2002) | 10 | - | 66 | 10/10 | S: 10/10 | n/a | 10.7 (6-13) wk | S: 10.7 (6-13) wk | S: 10/10 | S: 9.2 (6–16) wk | S: nil |
| Rettig et al[22] (1994) | 30 | C: 48.7 (9-136) wk; S: 49.3 (5-164) wk | 63 | 29/30 (96.7%) | C: 11/12; S: 18/18 | n/a | 6.6 (0-21) wk | C: 4.3 (0-10) wk; S: 8 (3-21) wk | C: 11/12; S: 18/18 | C: 14.2 (8-26) wk; S: 11.2 (4-24) wk | C: Non-union (1); S: nil |
| Rettig & Kollias[23] (1996) | 12 | 2.9 yr | 66 | 12/12 (100%) | S: 12/12 | S: 12/12 | 5.8 (1-10) wk | S: 5.8 (1-10) wk | S: 11/12 | S: 9.8 (6-18) wk | S: Non-union (1) |
| Riester et al[21] (1985) | 14 | 47 mo (3.9 yr) | 65 | 12/14 | C: 12/14 (85.7%) | C: 12/14 | 0 wk | C: 0 (0-0) wk | C: 11/14 | C: N/A | C: Non-union (3) (of which 2 patients required surgical intervention) |
| Robertson et al[26] (2012) | 20 | 30 (24-36) mo | 44 | 16/20 | C: 14/181; S: 2/2 | C: 13/181; S: 2/2 | 12.2 (6-24) wk | C: 12.7 (6-24) wk; S: 8.5 (8-9) wk | C: N/A; S: N/A | C: N/A; S: N/A | C: Non-union (3) (all 3 patient required delayed conversion to surgical fixation); S: Nil |
| Robertson et al[29] (2014) | 2 | 40 (34-46) mo | 44 | 2/2 | C: 2/2 | C 2/2 | 4 (4-4) wk | C: 4 (4-4) wk | C: N/A | C: N/A | C: Nil |
Of 160 fractures available for follow up, 77 were managed conservatively, and 83 were managed surgically. Of those managed conservatively, 28 were allowed to return to sport in cast, while 49 were only allowed to return to sport following cast treatment. Of those managed surgically, 50 were treated with open reduction and internal fixation (ORIF), and 33 were treated with percutaneous surgical fixation (PSF).
Seventy-seven of the scaphoid fractures were managed conservatively[9,10,21,22,26,27,29], of which 28 were allowed to return to sport in cast[21,22,27], and 49 were only allowed to return to sport following cast treatment[9,10,26,29].
The recorded forms of cast immobilisation included short arm thumb spica cast with the wrist in a neutral position[21], colles casts without thumb immobilisation[9] and below elbow plaster casts[10]. Two of the studies provided the patient with a specific silastic[21] or orthoplast[22] “playing” cast, which was used during sporting activities[22].
For the studies that allowed return in cast, the mean duration of immobilisation ranged from 3 mo to 6 mo[21,22,27]. For the studies that did not allow return in cast, the mean duration of immobilisation was 10 wk maximum[9,10,26,29].
Eighty-three of the scaphoid fractures were managed surgically[9,10,22-26,28]; the reported surgical techniques included ORIF (n = 50)[22-25,28] and PSF (n = 33)[9,10,26].
PSF was performed in three studies[9,10,26], of which two reported on surgical technique and post-operative rehabilitation[9,10]. Both studies performed the technique through a minimal incision over the distal pole of the scaphoid and used a cannulated scaphoid screw for fixation[9,10]. Post-operatively, Adolfsson et al[10] immobilised patients for 3 wk full time in a below elbow plaster splint, then 3 wk part time with a removable plastic splint during sports or vigorous activities; McQueen et al[9] used no immobilisation post-operatively, encouraging patient to mobilise as able. McQueen et al[9] advocated referral to physiotherapy post-operatively if clinically indicated.
ORIF was performed in five studies[22-25,28], of which four reported on surgical technique and post-operative rehabilitation[22-25]. Three studies used a volar (Russe-Type) approach to the scaphoid[22-24]; one used a dorsal approach[25]. All studies performed fixation with a scaphoid screw[22-25]. Post-operative immobilisation regimes comprised: a below elbow spica splint for 7 d to 10 d followed by a resting splint as needed[22,23]; below elbow cast immobilisation for 1 wk to 7 wk (mean 4 wk) with duration of cast immobilisation based on the intra-operative findings and the clinical judgement of the responsible surgeon[24]; a below-elbow plaster splint for 2 wk, followed by a removable forearm splint for 2 wk to 4 wk[25]. Formal physiotherapy programmes were described in three studies[22,23,25].
Three studies used formal validated scoring systems to assess functional outcomes post intervention[9,24,25]. Two studies reported on scaphoid fractures treated with ORIF[24,25]; the other study was a randomised controlled trial comparing conservative vs surgical management[9]. The functional scores used included the Disabilities of the Arm, Shoulder and Hand Score[25], the Mayo wrist score[24], the modified Green/O’Brien score[9] and a Visual Analogue Score for Pain[25].
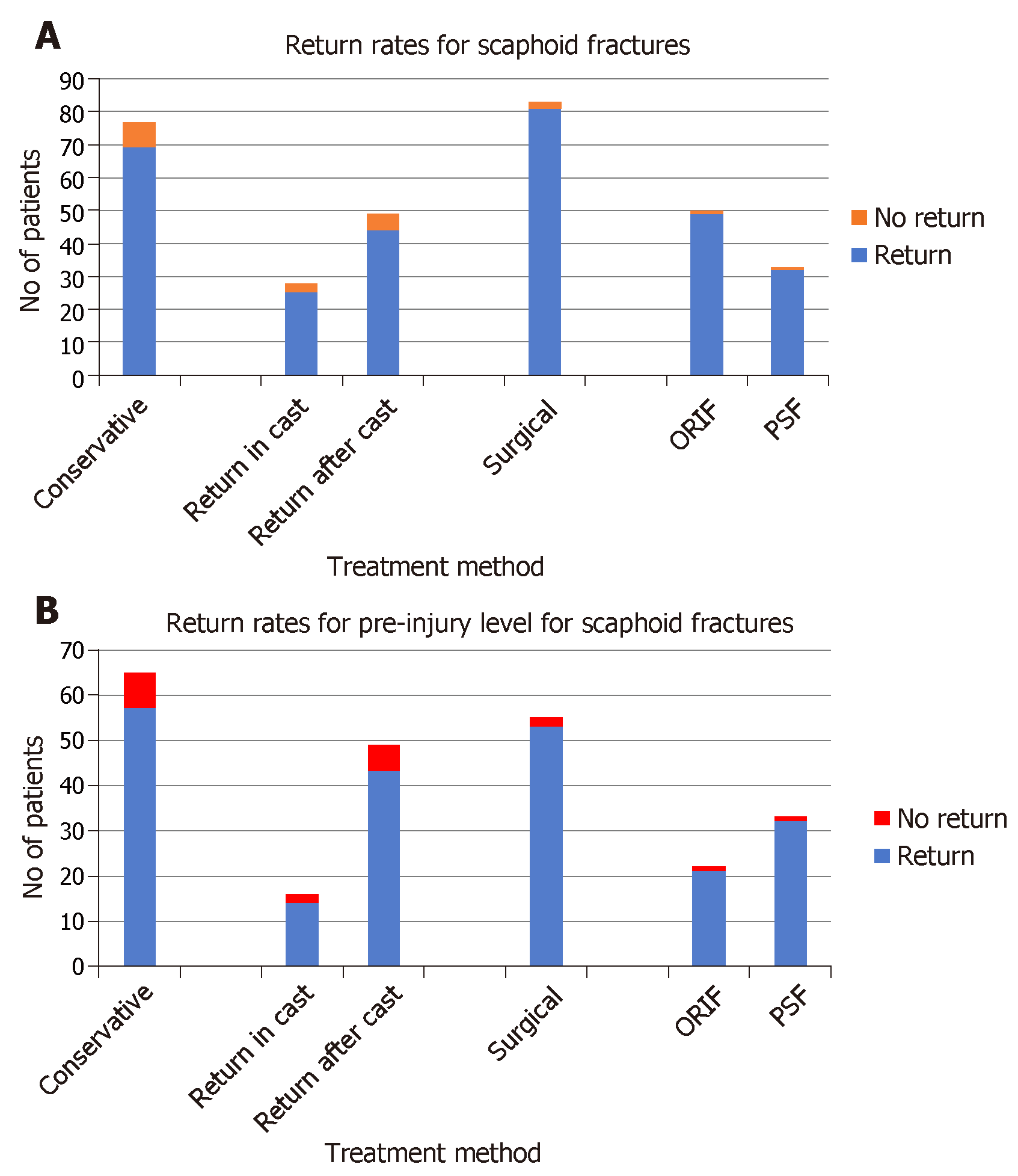
Conservative management: The RRS for conservatively-managed scaphoid fractures are provided in Table 4 and Figure 2A. RRS to pre-injury level of sport for each conservative management method are provided in Table 4 and Figure 2B.
| Mode of treatment | n | Return rates to sport | Mean return times to sport | Return rate to pre-injury level of sport | Union rate | Mean time to union |
| All[9,10,21-29] | 160 | 150/160 (94%)[9,10,21-29] | 8.4 wk[9,10,21-24,26-29] | 110/120 (92%)[9,10,21,23,25-29] | 116/126 (92%)[9,10,21-24] | 11.3 wk[9,22-24] |
| Conservative[9,10,21,22,26,27,29] | 77 | 69/77 (90%)[9,10,21,22,26,27,29] | 9.6 wk[9,10,21,22,26,27,29] | 57/65 (88%)[9,10,26,29] | 47/55 (85%)[9,10,21,22] | 14.0 wk[9,22] |
| Conservative - return in cast[21,22,27] | 28 | 25/28 (89%)[21,22,27] | 1.9 wk[21,22,27] | 14/16 (88%)[21,27] | 22/26 (85%)[21,22] | 14.2 wk[22] |
| Conservative - return after cast[9,10,26,29] | 49 | 44/49 (90%)[9,10,26,29] | 13.9 wk[9,10,26,29] | 43/49 (88%)[9,10,26,29] | 25/29 (86%)[9,10] | 13.9 wk[9] |
| Surgical[9,10,22-26,28] | 83 | 81/83 (98%)[9,10,22-26,28] | 7.3 wk[9,10,22-24,26,28] | 53/55 (96%)[9,10,23,25,26,28] | 69/71 (97%)[9,10,22-24] | 9.8 wk[9,22-24] |
| ORIF[22-25,28] | 50 | 49/50 (98%)[22-25,28] | 7.9 wk[22-24,28] | 21/22 (95%)[23,25,28] | 39/40 (98%)[22-24] | 10.3 wk[22-24] |
| PSF[9,10,26] | 33 | 32/33 (97%)[9,10,26] | 6.5 wk[9,10,26] | 32/33 (97%)[9,10,26] | 30/31 (97%)[9,10] | 9.2 wk[9] |
For the “conservative” synthesis cohort, the RRS was 90% (69/77). For patients who returned to sport in a cast, the RRS was 89% (25/28). For patients who returned to sports after cast removal, the RRS was 90% (44/49).
Surgical management: The RRS for scaphoid fractures managed surgically are provided in Table 4 and Figure 2A. Return rates to pre-injury level of sport for each surgical management method are provided in Table 4 and Figure 2B.
For the “surgical” synthesis cohort, the RRS was 98% (81/83). For patients treated with ORIF, the RRS was 98% (49/50). For patients treated with PSF, the RRS was 97% (32/33).
On meta-analysis, when comparing the “conservative” synthesis cohort to the “surgical” synthesis cohort, the difference in RRS was significant (RR = 1.09; 95%CI: 1.00-1.18; P < 0.045: I2 = 0%, P = 0.78).
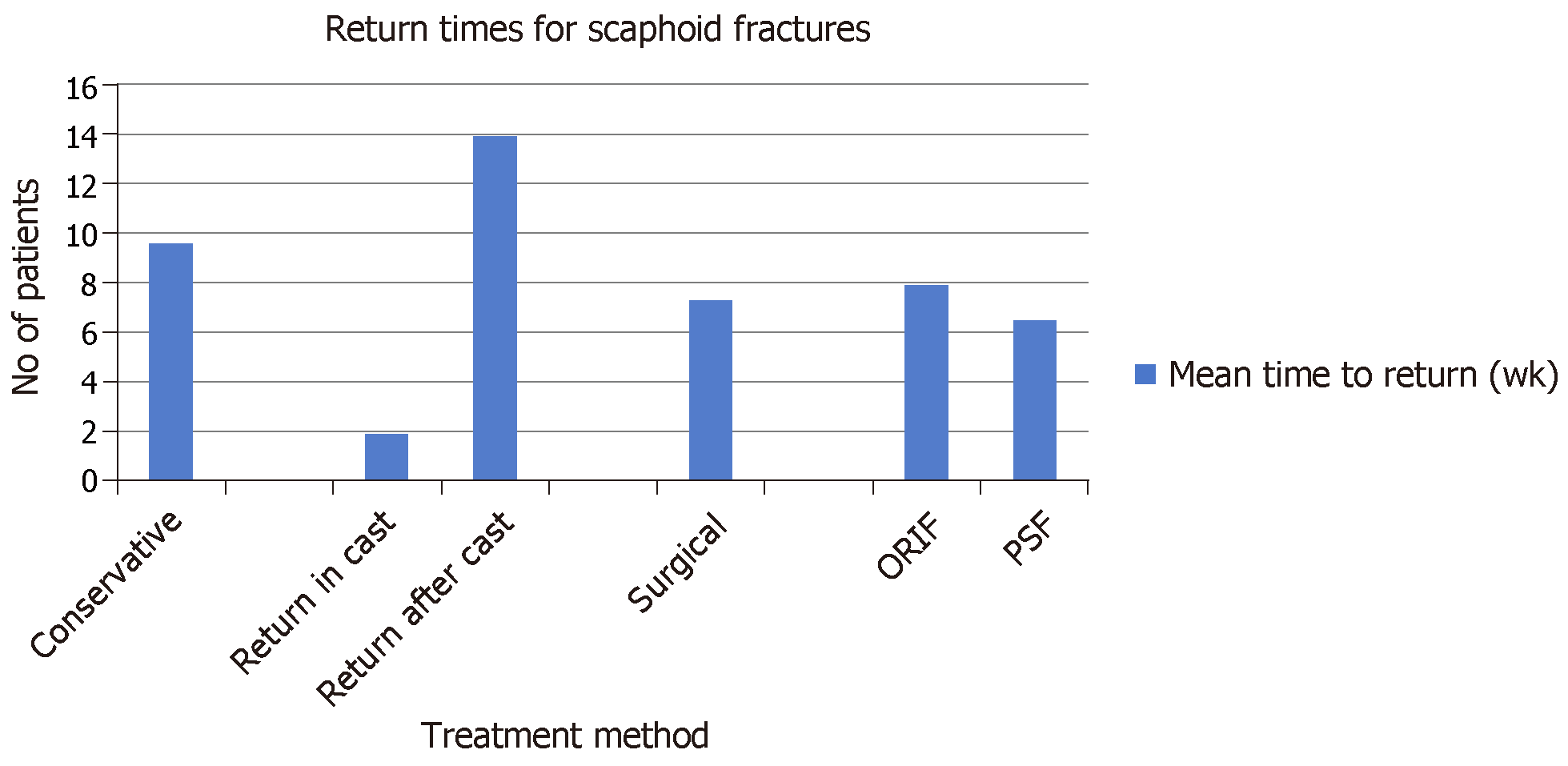
Conservative management: The RTS for the conservatively-managed scaphoid fractures are provided in Table 4 and Figure 3. For the “conservative” synthesis cohort, the mean RTS was 9.6 (0-16) wk. For patients who returned to sport in a cast, the mean RTS was 1.9 (0-4) wk. For patients who returned to sports after cast removal, the mean RTS was 13.9 (4-16) wk.
Surgical management: The RTS for surgically managed scaphoid fractures are provided in Table 4 and Figure 3. For the “surgical” synthesis cohort, the mean RTS was 7.3 (6-11) wk. For patients treated with ORIF, the mean RTS was 7.9 (6-11) wk. For patient treated with PSF, the mean RTS was 6.5 (6-9) wk.
On meta-analysis, comparing the “conservative” synthesis cohort to the “surgical” synthesis cohort, the difference in the mean RTS was significant (MD 2.3 wk; 95%CI: 0.79-3.87; P < 0.002).
Conservative management: Four studies reporting on conservatively managed fractures recorded data on fracture union[9,10,21,22]. The union rate for this cohort was 85% (47/55), and the mean time to union was 14.0 (14-14) wk. For patients who returned to sport in a cast, the union rate was 85% (22/26), and the mean time to union was 14.2 wk[21,22]. For patients who returned to sports after cast removal, the union rate was 86% (25/29), and the mean time to union was 13.9 wk[9,10].
Surgical management: Five studies reporting on surgically managed fractures recorded data on fracture union[9,10,22-24]. The union rate for this cohort was 97% (69/71), and the mean time to union was 9.8 (9-11) wk. For patients treated with ORIF, the union rate was 98% (39/40), and the mean time to union was 10.3 (9-11) wk[22-24]. For patients treated with PSF, the union rate was 97% (30/31), and the mean time to union was 9.2 (9-9) wk[9,10].
On meta-analysis, comparing the “conservative” cohort to the “surgical” cohort, the difference in union rates (RR = 1.14; 95%CI 1.01-1.28; P < 0.030: I2 = 0%, P = 0.99) and mean union times (MD 4.2 wk; 95%CI 3.94-4.36; P < 0.001) were both significantly better for the ‘surgical’ cohort (Table 4).
Conservative management: Two of the three studies, which comprised conservatively-managed patients who returned to sport immediately in cast, reported complications[21,22]. These comprised non-union (8%-21%)[21,22] and delayed surgical intervention for non-union (14%)[21] (Table 3).
Three of the four studies, which comprised conservatively-managed patients who returned to sport after cast treatment, reported complications[9,10,26]. These comprised non-union (15%-17%)[9,26], delayed surgical intervention for non-union (17%)[26], avascular necrosis (7%)[9], complex regional pain syndrome (4%)[9], malunion (11%)[9], radioscaphoid osteoarthritis (4%)[9] and persistent radial border wrist pain (50%)[10] (Table 3).
Surgical management: One of the three studies, reporting on patients treated with PSF, reported complications[9]. These comprised peri-operative breakage of the cannulated screwdriver (7%)[9], symptomatic metalwork (4%)[9] and non-union (4%)[9] (Table 3).
Three of the five studies, reporting on patients treated with ORIF, reported complications[23,25,28]. These comprised non-union (8%)[23]; scar sensitivity(6%)[25] and superficial radial nerve neuropraxia (40%)[28].
The management of scaphoid fractures remains a challenge in the athletic population. The findings from our review demonstrate that surgical management offers the best outcome regarding RRS and RTS post treatment. Not only does conservative management result in significantly lower RRS and RTS, it also demonstrates a substantial rate of fracture non-union, which can further impair athletes in their recovery from this injury.
In this review, the methodological quality of studies was lower than that of previous similar systematic reviews looking at return to sports following various fracture types, with a mean CMS of 59.5[16-20]. Thus, despite the inclusion of two randomised controlled trials in this study[9,10], this demonstrates a need for further high-quality research in this area including level one studies.
The management of scaphoid fractures is dependent on the location and the nature of the fracture. Of the recorded fracture types in the review, scaphoid waist fractures (waist, middle third, Herbert B2, Herbert A2) comprised the significant majority, representing 89% of these. All fractures types recorded in the review were, however, amenable to either surgical or conservative treatment as acute management: and these were therefore considered suitable for synthesis into the sub-cohorts accordingly.
From this review, the authors found that conservative management offered an RRS of 90% (88% return rate to pre-injury level of sport) with a mean RTS of 9.6 wk. While this can be considered satisfactory, as compared to figures reported from other fracture types, the return rates and return times were significantly lower compared to those reported from surgical management. With this, the rate of non-union from the conservatively-managed cohort was 15%, which again was significantly higher than that for the surgically managed cohort (3%)
To note, with the conservatively-managed cohort, there were three studies that advocated immediate return to sport following the injury, using cast or splint immobilisation[21,22,27]. This group demonstrated a non-union rate of 15%, which is likely the result of excessive movement at the fracture site secondary to early return to sporting activities. All three studies were published over 30 years ago[21,22,27], and such practice is currently not recommended for this reason[3]. Given that this provided return times of 0 wk for their patients, this considerably skews the “return time” data for the conservatively-managed patients. When the return times for the “conservative” cohort are analysed in consideration of this, the mean RTS for the patients who returned to sport following cast treatment was 13.9 wk. This is considerably longer than that recorded by the “surgical” cohort (7.3 wk) and so provides further recommendation towards surgical management of these injuries.
Thus, while conservative management can provide acceptable results in terms of RRS and RTS, athletes should be appropriately informed of the likely increased return time, decreased return rate and increased non-union rate associated with this treatment, in comparison to surgical management. Given the comparably high non-union rate associated with return to sport in cast, it is currently not recommended to allow patients to return to sports during cast immobilisation.
On analysis of the data from the “surgical” cohort, the authors found that this treatment provided an RRS of 98% (96% return rate to pre-injury level of sport) and a mean RTS of 7.3 wk: both these figures were significantly less than those from the “conservative” cohort. The union rate was also significantly higher for the “surgical” cohort (97%) compared to the “conservative” cohort (85%). ORIF and PSF provided similar RRS (98% and 97% respectively): however, PSF provided a marginally improved mean RTS (6.5 wk vs 7.9 wk). This is likely accounted for by the reduced tissue dissection, reduced duration of post-operative immobilisation and the simpler fracture patterns amenable to PSF when compared to ORIF[9,10,22-26,28]. However, despite this, both treatment methods offered similar union rates (98% vs 97%), providing evidence of the substantial benefit that surgical stabilisation and compression can provide to bone healing with this injury[9,10,22-26,28]. Our findings correlate with a similar systematic review, comparing conservative to surgical management of scaphoid waist fractures, which demonstrated earlier return to work and faster time to union with surgical management[30].
Given the substantial benefits in RRS, RTS and union rates for surgical management as compared to conservative management, surgical management should be the recommended option for treatment of these injuries in the athlete[31]. However, given that conservative management remains a reasonable option, any treatment recommendation must include a full discussion regarding the benefits and risk of both surgical and conservative management, particularly detailing the risk of surgical complications (surgical site infection, metalwork-related symptoms, neuro-vascular injury and wound problems) when describing surgical management[32,33].
To note, there were a number of different immobilisation techniques and regimes used in the included studies [9,10,21,25]. A clear benefit of surgical stabilisation is that it reduces the requirement for post-operative immobilisation, facilitating an accelerated return to sporting activities[9,10,22-26,28]. However, on comparing studies within the conservative and surgical cohorts, significant variations were noted within each treatment group. Within the surgical cohort, post-operative immobilisation post ORIF ranged from 1 wk to 7 wk, with a variety of below elbow spica splints, casts and plaster splints employed[22-25,28]. Of the studies that employed PSF, one did not require post-operative immobilisation[9], while another required splinting up 6 wk post-operatively[10]. Within the conservative cohort, the methods of immobilisation included a short arm thumb spica cast with the wrist in a neutral position[21], colles’ cast without thumb immobilisation[9] and below elbow plaster casts[10], while the mean duration of immobilisation ranged from 10 wk to 6 mo[9,10,26,29]. Interestingly, the studies that allowed return to sport in a cast had considerably longer immobilisation durations (3 mo to 6 mo)[21,22,27] than the other studies[9,10,26,29]. Given the substantial variety present, it was not possible to analyse the effect of immobilisation methods and duration on sporting outcome. However, such variation clearly demonstrates an area of future research, whereby the optimal methods and duration of immobilisation can be determined for these fractures to improve further RRS and RTS.
The use of formal functional outcomes scores was lower when compared to similar reviews assessing other fracture types[15-20]. Only three of the 11 studies used formal functional assessments to assess patient outcome[9,24,25]. Future prospective studies should aim to utilise validated functional assessment scoring systems in order to assess further the effect of immobilisation and rehabilitation following fractures of the scaphoid in athletes.
The first of these relates to the fact that a number of the earlier studies included in the review had very limited information on patient demographics as well as post-operative care. Although they provided the relevant information regarding RRS and RTS, the lack of additional information limited our ability to perform more detailed analyses, assessing for associated predictive factors of sporting outcome.
Further to this, most of the included studies did not provide detailed information regarding sporting outcomes, often failing to provide information on return to pre-injury level of sport. To accommodate for this, the authors designated three main categories for sporting outcome (return to sport, RTS, return to pre-injury level of sport), allowing clear definitive outcome data to be extracted from each study, thus facilitating direct comparisons to be made on the effect of different treatments from the various studies included.
A further limitation of the review lies in the inclusion of studies from several years previous, which report on treatment methods that are no longer recommended[21,22,27]. Three of the earlier studies allowed patients to return to sports immediately in cast, which positively skewed the RTS for the conservative cohort[21,22,27]: such practice is actively discouraged in current practice given the substantial risk of fracture displacement and non-union[3]. However, the results were appropriately divided into sub-cohorts, demonstrating the effects of such practices on the synthesis data.
The final limitation comprises the variety of fracture locations present within the review. While the significant majority of the recorded fractures were within the scaphoid waist region, a number of studies reported on fractures both within the proximal and distal third regions of the scaphoid. However, all recorded fracture types were suitable for either conservative or surgical management, and so it was considered appropriate to synthesise these accordingly for outcome analyses.
Over 90% of athletes who sustain a scaphoid fracture can expect to return to sport. While conservative management can provide acceptable results regarding RRS and RTS, surgical management can provide athletes with a significantly greater chance of returning to sport and allow them to return to sport significantly quicker. It can also provide them with a significantly higher rate of fracture union. However, given that both treatments remain considerable options, all patients should be comprehensively informed of the benefits and risk of both treatment methods prior to deciding management. In particular, patients should be made aware of the risk of surgical complications, which include surgical site infection, neurovascular injury, metalwork-related symptoms and wound problems. Return to sport during cast immobilisation should be actively discouraged due to the high risk of non-union. Further prospective randomised controlled trials should aim to define better the benefit over surgical over conservative management for treatment of these injuries in athletic patients.
Scaphoid fractures account for over 85% of all sport-related carpal bone fractures and are particularly common in sports involving high impact injuries to the wrist. The management of such injuries comprises both conservative and surgical techniques, as guided by fracture location and type. Athletes demonstrate a unique challenge with regards to the management of scaphoid fractures due to their requirement to return to sport as soon as able.
Scaphoid fractures significantly impact an athlete’s ability to return to sport. This topic should therefore be addressed to understand further the outcome of various treatment options and to optimise the management of these injuries.
To identify the available literature reporting on the sporting outcomes of both conservative and surgical management of scaphoid fractures in the athletic population.
A systematic review of the available literature was performed, identifying all articles reporting on return rates to sport (RRS) and return times to sport (RTS) following acute scaphoid fractures. A total of 160 acute scaphoid fractures were included for analysis.
The RRS for conservative management and for surgical management were 90% and 98%, respectively. The mean RTS was lower in the surgical cohort at 7.3 wk, compared to 9.6 wk in the conservative cohort. Union rate was higher in the surgical cohort at 97% compared to 85% in the conservative cohort. On meta-analysis, surgical management of scaphoid fractures provided significantly better RRS, RTS, union rates and mean times to union as compared to conservative management.
Most athletes can expect to return to sports following scaphoid fractures, with either conservative or surgical management. Surgical management did however offer improved RRS, RTS and union rates. Both treatment options remain appropriate in the management of scaphoid fractures, and patients should be counselled accordingly prior to treatment decisions. Return to sport in a cast should be discouraged due to the risk of non-union.
The management of scaphoid fractures remains a challenge in the athletic population. Further well-designed studies should aim to address this topic in order to provide a better understanding of the RRS and RTS following the various treatment methods for acute scaphoid fractures in the athlete.
Biostatistics statement: The statistical methods of this study were reviewed by Greg Robertson from the Edinburgh Orthopaedic Trauma Unit. He has had a degree level statistical method training from the University of Edinburgh. He can be contacted at greg_robertson@live.co.uk. The statistical methods employed in this study have been used previously by the authors in several similar systematic reviews: all of these have been published in peer-reviewed journals.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lee PN S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39:1377-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Weber ER, Chao EY. An experimental approach to the mechanism of scaphoid waist fractures. J Hand Surg Am. 1978;3:142-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 96] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Coutr-Brown C, McQueen M, Tornetta P. Trauma. 1st ed. Philadelphia: Lippincott Williams Wilkins 2006; . |
| 4. | Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up. J Hand Surg Br. 1998;23:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 85] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Ring D, Lozano-Calderón S. Imaging for suspected scaphoid fracture. J Hand Surg Am. 2008;33:954-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Winston MJ, Weiland AJ. Scaphoid fractures in the athlete. Curr Rev Musculoskelet Med. 2017;10:38-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66:114-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 8. | Geoghegan JM, Woodruff MJ, Bhatia R, Dawson JS, Kerslake RW, Downing ND, Oni JA, Davis TR. Undisplaced scaphoid waist fractures: is 4 weeks' immobilisation in a below-elbow cast sufficient if a week 4 CT scan suggests fracture union? J Hand Surg Eur Vol. 2009;34:631-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | McQueen MM, Gelbke MK, Wakefield A, Will EM, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90:66-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 150] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg Br. 2001;26:192-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 126] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Dy CJ, Khmelnitskaya E, Hearns KA, Carlson MG. Opinions regarding the management of hand and wrist injuries in elite athletes. Orthopedics. 2013;36:815-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Rizzo M, Shin AY. Treatment of acute scaphoid fractures in the athlete. Curr Sports Med Rep. 2006;5:242-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47103] [Article Influence: 2943.9] [Reference Citation Analysis (0)] |
| 14. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 765] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 15. | Del Buono A, Smith R, Coco M, Woolley L, Denaro V, Maffulli N. Return to sports after ankle fractures: a systematic review. Br Med Bull. 2013;106:179-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Robertson GA, Wood AM. Return to sports after stress fractures of the tibial diaphysis: a systematic review. Br Med Bull. 2015;114:95-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Robertson GA, Wood AM. Return to Sport After Tibial Shaft Fractures: A Systematic Review. Sports Health. 2016;8:324-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Robertson GA, Wood AM. Return to sport following clavicle fractures: a systematic review. Br Med Bull. 2016;119:111-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Robertson GAJ, Goffin JS, Wood AM. Return to sport following stress fractures of the great toe sesamoids: a systematic review. Br Med Bull. 2017;122:135-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Robertson GAJ, Wong SJ, Wood AM. Return to sport following tibial plateau fractures: A systematic review. World J Orthop. 2017;8:574-587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Riester JN, Baker BE, Mosher JF, Lowe D. A review of scaphoid fracture healing in competitive athletes. Am J Sports Med. 1985;13:159-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 48] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Rettig AC, Weidenbener EJ, Gloyeske R. Alternative management of midthird scaphoid fractures in the athlete. Am J Sports Med. 1994;22:711-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Rettig AC, Kollias SC. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med. 1996;24:182-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 75] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Muramatsu K, Doi K, Kuwata N, Kawakami F, Ihara K, Kawai S. Scaphoid fracture in the young athlete--therapeutic outcome of internal fixation using the Herbert screw. Arch Orthop Trauma Surg. 2002;122:510-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Bedi A, Jebson PJ, Hayden RJ, Jacobson JA, Martus JE. Internal fixation of acute, nondisplaced scaphoid waist fractures via a limited dorsal approach: an assessment of radiographic and functional outcomes. J Hand Surg Am. 2007;32:326-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 26. | Robertson GA, Wood AM, Bakker-Dyos J, Aitken SA, Keenan AC, Court-Brown CM. The epidemiology, morbidity, and outcome of soccer-related fractures in a standard population. Am J Sports Med. 2012;40:1851-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 27. | Ellsasser JC, Stein AH. Management of hand injuries in a professional football team. Review of 15 years of experience with one team. Am J Sports Med. 1979;7:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Huene DR. Primary internal fixation of carpal navicular fractures in the athlete. Am J Sports Med. 1979;7:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Robertson GA, Wood AM, Heil K, Aitken SA, Court-Brown CM. The epidemiology, morbidity and outcome of fractures in rugby union from a standard population. Injury. 2014;45:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | Modi CS, Nancoo T, Powers D, Ho K, Boer R, Turner SM. Operative versus nonoperative treatment of acute undisplaced and minimally displaced scaphoid waist fractures--a systematic review. Injury. 2009;40:268-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Belsky MR, Leibman MI, Ruchelsman DE. Scaphoid fracture in the elite athlete. Hand Clin. 2012;28:269-278, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Moatshe G, Godin JA, Chahla J, Cinque ME, Kennedy NI, Sanchez G, Beaulieu-Jones BR, LaPrade RF, Provencher MT. Clinical and Radiologic Outcomes After Scaphoid Fracture: Injury and Treatment Patterns in National Football League Combine Athletes Between 2009 and 2014. Arthroscopy. 2017;33:2154-2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | de Boer BNP, Doornberg JN, Mallee WH, Buijze GA. Surgical Versus Conservative Treatment for Nondisplaced Scaphoid Waist Fractures. Buijze GA, Jupiter JB, editors. Scaphoid Fractures: Evidence-Based Management. Elsevier 2018; 99-106. |