Published online Dec 18, 2019. doi: 10.5312/wjo.v10.i12.446
Peer-review started: January 14, 2019
First decision: March 15, 2019
Revised: April 4, 2019
Accepted: September 22, 2019
Article in press: September 22, 2019
Published online: December 18, 2019
Processing time: 331 Days and 17.9 Hours
Anterior cruciate ligament reconstruction (ACLR) has a high incidence of re-tear in younger patients. Despite comparable functional outcomes, the incidence of re-tear using single and double bundle ACLR methods has not been well reported.
To hypothesize that double bundle hamstring ACLR has a lower graft rupture rate compared with single bundle hamstring ACLR grafts in young patients.
One hundred and twelve patients < 30 years of age at the time of primary double bundle ACLR were eligible for study participation. 91 (81.3%) could be contacted, with a mean age of 20.4 years (range 13-29) and mean post-operative follow-up time of 59 mo (range 25-107). Telephone questionnaires evaluated the incidence (and timing) of subsequent re-tear and contralateral ACL tear, further surgeries, incidence and time to return to sport, and patient satisfaction.
Of the 91 patients, there were 6 (6.6%, 95%CI: 1.4-11.7) ACL graft re-ruptures, with a mean time to re-rupture of 28 mo (range 12-84). Fourteen patients (15.4%) experienced a contralateral ACL rupture and 14 patients (15.4%) required further surgery to their ipsilateral knee. fifty patients (54.9%) returned to pre-injury level of sport. Of those < 20 years (n = 45), 4 patients (8.9%, 95%CI: 0.4-17.3) experienced a re-rupture, with mean time to re-injury 15 mo (range 12-24). Comparative analysis with existing literature and revealed a non-significant Chi-squared statistic of 2.348 (P = 0.125).
A trend existed toward lower graft rupture rates in young patients undergoing double bundle ACLR utilizing a hamstring autograft, compared with rates reported after single bundle ACLR.
Core tip: Double bundle anterior cruciate ligament (ACL) reconstruction has a low re-rupture rate (6.6%) in the young, active population. In addition, re-rupture rates are shown to be at least comparable with Single Bundle ACL reconstructions techniques.
- Citation: Lim CR, Henson T, Ebert J, Annear P. Anterior cruciate ligament reconstruction using a double bundle hamstring autograft configuration in patients under 30 years. World J Orthop 2019; 10(12): 446-453
- URL: https://www.wjgnet.com/2218-5836/full/v10/i12/446.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i12.446
Anterior cruciate ligament (ACL) tears are prevalent, and surgical ACL reconstruction (ACLR) is considered the current standard of clinical treatment[1]. Unfortunately, a high incidence of re-rupture (20%-30%) has been reported, particularly in younger patients[2,3]. While the gold standard in ACLR has traditionally been bone-patellar tendon-bone graft, hamstrings autografts have become more popular with a recent systematic review and meta-analysis suggesting comparable outcomes between the two and less post-operative complications using hamstrings[4,5].
The two distinct bundles of the ACL (anterior-medial bundle and posterior-lateral) are responsible for anterior-posterior stability and rotational stability retrospectively[6,7]. Despite this, traditional single bundle hamstring ACLR has become more favorable in recent years, which requires the harvest of hamstring tendon to create a single graft that is passed through a single tibial and femoral tunnel[5]. Double bundle hamstring ACLR involves the creation of two grafts and two additional tunnels. Studies have compared single and double bundle ACLR graft constructs[8-14]. A Cochrane review in 2012 by Tiamklang et al[8] concluded that a double bundle configuration may provide better knee stability and return to sport capacity; however, double bundle ACLR provided similar rates of re-rupture in adults and there was a higher incidence of subsequent notchplasty required due to notch impingement.
To the best of our knowledge, previous research has not sought to compare the outcomes of single and double bundle ACLR configurations using a hamstring autograft in the younger population, where the incidence of re-tear is considerably higher. This study aimed to investigate the rate of ACL re-rupture in young patients undergoing double bundle ACLR, and compared this to the available literature largely focused around single bundle ACLR graft constructs.
The arthroscopically-assisted double bundle ACLR operative technique involved autologous harvesting of semitendinosus and gracilis tendons to form two distinct grafts. Tibial tunnels were drilled based on the tibial ACL footprint with anterior-lateral and posterior-medial tunnels. Femoral tunnels were drilled in a similar fashion based on the anatomical footprint of the native ACL. Each graft was then passed through their respective tunnel and tensioned at maximal manual tension after ten cycles of the knee (0-90°). Post-operatively, patients were braced in an extension splint for 2-3 wk to reduce knee swelling and protect the construct, with crutch ambulation as required. Early range of motion exercises were encouraged, with a focus on regaining full active knee extension. Stationary cycling, swimming, and closed chain conditioning were allowed at 6-8 wk. Jogging and open chain strength exercises were commenced at 16 wk with a return to sport between 9 and 12 mo.
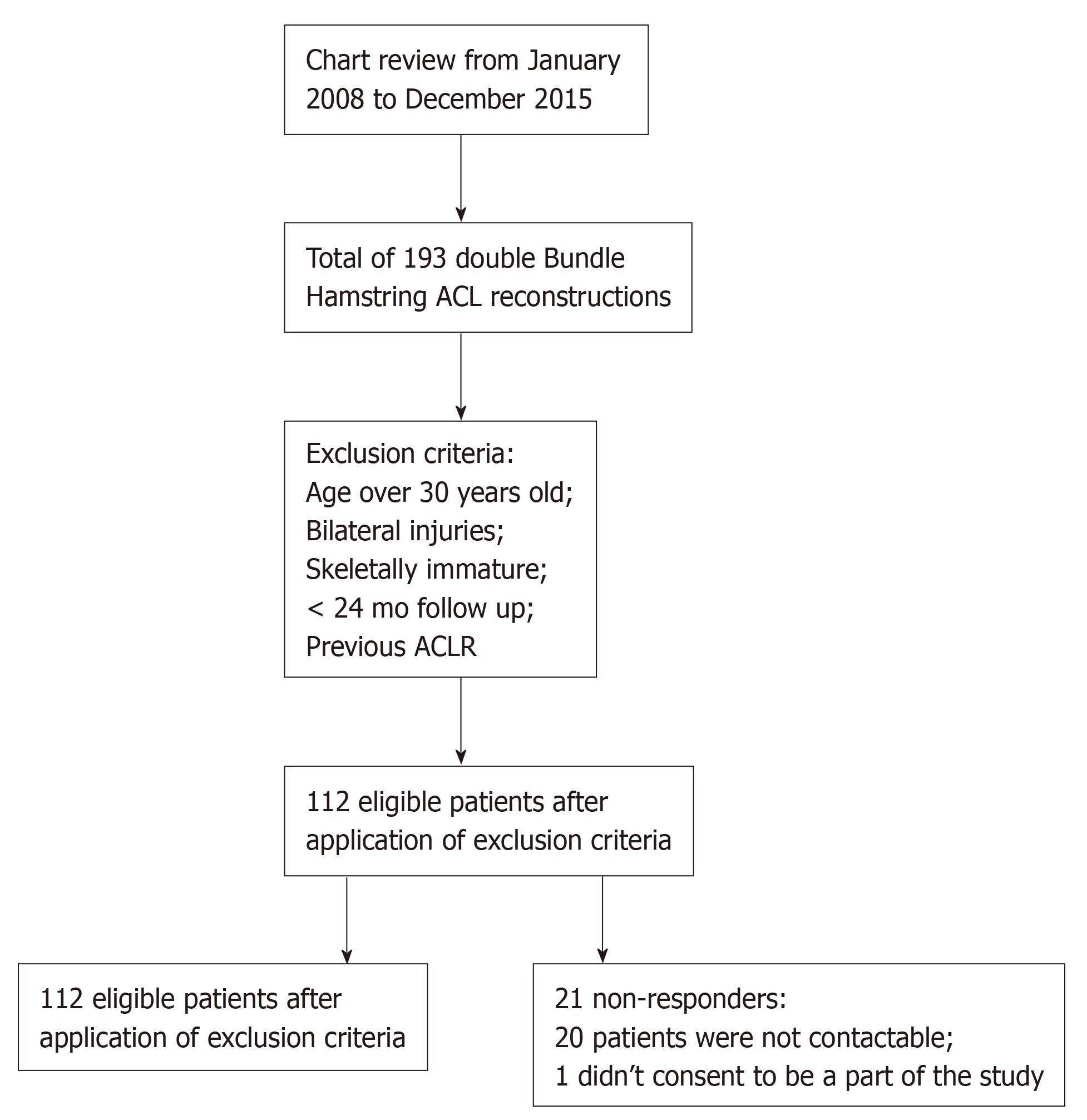
All patients who underwent primary double bundle ACLR utilizing a hamstrings autograft under a single orthopedic surgeon (PA), between January 2008 and December 2015, were reviewed for eligibility for the study (n = 193) (Figure 1). Initially, the medical records (clinical notes, operation records, radiology reports) of all patients that underwent surgery through the nominated period were manually reviewed to determine eligibility. Patients were included in the current study if they were skeletally mature at the time of ACLR surgery and required a primary ACLR, consenting to the double bundle ACLR technique which was the preferred method of the principal investigator at the time, with or without concomitant meniscal surgery. Patients were excluded upon initial chart review if they were ≥ 30 years of age at the time of surgery, had bilateral injuries, had undergone prior ACLR on the ipsilateral or contralateral knee, and/or those that had < 24 mo of clinical follow-up. Of the 113 eligible patients, 1 had a femoral condyle impaction fracture with their ACL injury and was excluded from the study leaving 112 for data collection. Ethics was granted from the relevant hospital ethics committee.
Basic demographical and injury characteristics, together with details of pre- and post-operative clinical management were collected from chart review. All patients included as per the inclusion/exclusion criteria for this study were then contacted via phone, to ascertain the following outcomes: (1) The incidence (and timing) of subsequent ACL re-tear and/or contralateral ACL tear; (2) The incidence (and timing) of other ipsilateral and/or contralateral knee injuries/surgeries (whether they be related to the graft such as ACL re-tear, or not); and (3) Whether the patient had undergone any other second orthopedic opinions and/or surgeries relating to their operated (or contralateral) knee. Patient satisfaction with their surgical outcome was also evaluated, via a 5-point categorical scale: (1) Completely unsatisfied; (2) Mostly unsatisfied; (3) Uncertain; (4) Mostly satisfied; and (5) Completely satisfied. Finally, the timing and ability of the patient to return to their pre-injury level of sport were evaluated.
All information collected from the chart review and standardized phone interview was logged in an excel spreadsheet to ensure consistent collection and documentation. This study sought to determine the incidence of ACL re-injury, contralateral injury, and combined ACL (ipsilateral re-tear and contralateral rupture) injury in patients < 30 years, though also more specifically in younger patients < 20 years of age as previously undertaken and reported by Webster et al[2] χ2 test were used to compare categorical outcomes between the current study (double bundle ACLR employing a hamstrings autograft) and that of Webster et al[2] (single bundle ACLR employing a hamstrings autograft). Statistical analysis was conducted using SPSS software (SPSS, Version 23.0, SPSS Inc., United States), while statistical significance was determined at P < 0.05.
Of the 112 patients eligible for the study based on inclusion criteria, 91 (81.3%) responded and consented to participation (Table 1). Of the non-responders (n = 21), 20 patients could not be contacted, and one patient did not consent.
| Variable | Measure | Total Cohort (< 30 yr) | Patients (20-29 yr) | Patients (< 20 yr) | |
| Dataset (2018) | Dataset (2018) | Dataset (2018) | Webster et al[2], 2016 | ||
| Patients | n | 91 | 46 | 45 | 316 |
| Age (yr) | mean (SD), range | 20.4 (4.7), 13-29 | 24.0 (2.5), 20-29 | 16.2 (1.8), 13-19 | 17.2 (NR), 11-19 |
| Clinical follow-up (mo) | mean (SD), range | 59 (26), 25-107 | 63 (27), 29-107 | 55 (25), 25-102 | 60 (NR), 36-120 |
| Males | n (%) | 51 (56.0) | 29 (63.0) | 22 (48.9) | 200 (63.6) |
| Right knee | n (%) | 40 (44.0) | 25 (54.3) | 22 (48.9) | NR |
| Concurrent meniscal surgery | n (%) | 44 (48.4) | 18 (39.1.9) | 26 (57.8) | NR |
| ACL re-ruptures | n (%) | 6 (6.6) | 2 (4.3) | 4 (8.9) | 57 (18) |
| ACL re-ruptures | 95%CI | 95%CI: 1.4%-11.7% | 95%CI: 1.6%-10.3% | 95%CI: 0.4%-17.3% | 95%CI: 17%-29% |
| Mean time to re-rupture (mo) | mean (SD), range | 28 (28), 12-84 | 55.0 (41.7), 25-84 | 15 (6), 12-24 | 21.6 (NR), NR |
| Repair of re-rupture | n (%) | 5 (83.3) | 1 (50) | 3 (75) | NR |
| Subsequent surgery to ipsilateral knee | n (%) | 14 (15.4) | 7 (15.2) | 7 (15.6) | NR |
| Contralateral ACL injury | n (%) | 14 (15.4) | 9 (19.6) | 5 (11.1) | 56 (17.7) |
| Combined ACL injuries | n (%) | 20 (22.0) | 11 (23.9) | 9 (20.0) | 113 (35.8) |
Of the 91 patients < 30 years of age at the time of surgery, the mean age was 20.4 years (range 13-29) (Table 1). Six patients (6.6%, 95%CI: 1.4-11.7) patients had a re-rupture of their primary double bundle hamstring ACLR, with a mean time to re-injury of 28 mo (range 12-84) (Table 1). Of those < 20 years of age (n = 45), 4 patients (8.9%, 95%CI: 0.4-17.3) experienced a re-rupture, with a mean time to re-injury of 15 mo (range 12-24) (Table 1). Of the 6 patients that had experienced re-injury at the time of analysis, 5 patients (83.3%) had undergone revision ACLR and the remaining patient was on the wait list for revision.
A total of 14 patients (15.4%) experienced a contralateral ACL rupture at the time of study review (Table 1), with all of these having undergone contralateral ACLR without further injury at the time of review. There was a total of 20 (22.0%) ACL injuries to either the ipsilateral or contralateral knee (Table 1). Of all the patients who suffered an ACL graft re-rupture, none had a contralateral ACL rupture. In those < 20 years of age, 5 patients (11.1%) had experienced a contralateral ACL tear.
A total of 14 patients (15.4%) required further surgery (including revision ACLR) to their ipsilateral knee, with 7 patients (15.6%) < 20 years of age requiring subsequent surgery (Table 1). The most common reason for re-operation was revision ACLR (5 patients), notchplasty (4 patients) or removal of the tibial screw (2 patients).
Overall, 50 patients (54.9%) returned to their pre-injury level of sport, with the mean time to return to sport at 13.4 mo (range 6-36). A total of 13 patients (14.3%) did not return to any level of sport. A total of 20 (22%) professional athletes were included in the study, of which 6 (30%) managed to return to a professional level of sport. Australian Rules Football (AFL) was the most common sporting reason for injury, occurring in 31 (34.1%) patients. This was followed by netball (n = 18, 19.8%), soccer (n = 7, 7.7%) and basketball (n = 6, 6.6%), with motor vehicle accidents accounting for 2.2% (n = 2). All 6 re-ruptures occurred in the 78 (6.4%) patients that returned to sport post-operatively. However, at the time of contact 1 of these re-ruptures had given up playing all sports. Mean satisfaction levels were 4.27 with 81 (89.1%) of patients being either mostly satisfied or completely satisfied with their knee outcome. Only 1 patient was completely unsatisfied, and he was awaiting revision ACLR for re-rupture of his graft.
The data from this population was then compared to a paper written by Webster et al[2] in 2016. As per Webster et al[2]’s classification of “young” ACLR patients (< 20 years of age), sub-group comparative analysis in ACL re-tears revealed a non-significant χ2 statistic of 2.3 (P = 0.125), when comparing those < 20 years of age in the current study (Table 1).
ACL re-tears are common, particularly in the young active cohort, and a more robust graft construct may be required in these patients to reduce the incidence of a subsequent re-injury. The primary findings from this study are that double bundle ACLR construct in younger patients (< 30 years) resulted in: (1) A low rate of graft re-rupture (6.6%) and (2) A low rate of contralateral ACL insult (15.4%). A Cochrane review by Tiamklang et al[8] in 2012 comparing double bundle and single bundle ACLR combined six studies reporting a re-rupture rate of 1/169 (0.5%) vs 4/185 (2.2%), respectively. Since then, Suomalainen et al[9] conducted a randomized controlled trial and reported 11 graft failures in 90 (12.2%) patients undergoing primary ACLR at the time of five years follow up (mean age 33 years). Of the 30 patients undergoing a double bundle ACLR, only 1 (3.3%) graft rupture was reported, which was significantly lower when compared to single bundle ACLR[10]. More recently, Mohtadi et al[11], in 2014, conducted a randomized controlled trial of 109 double bundle and 111 single bundle ACLRs, with a mean age of 29 years, and compared graft failure rates. Results showed high failure rates, 19 graft failures (17.4%) in the double bundle population vs 29 (26.1%) in those undergoing single bundle ACLR (P = 0.043), with a mean time to failure of 16 mo[11]. The study also reported 6 (5%) contralateral ACL tears in their double bundle ACLR cohort[11]. These studies suggest that re-rupture rates in double bundle ACLR could indeed be lower.
This study reported an ACL re-tear incidence of 8.9% in patients < 20 years, with a further 11.1% experiencing a contralateral tear, at a minimum of 2 years post-surgery (mean 59 mo). It should also be noted that while there were only 4 re-ruptures in this young cohort, one of these patients returned to sport prior to complete their rehab at their own discretion. This potentially presents a higher re-tear rate than could have been observed should the minimum time to return to sport have been followed. Webster et al[2] presented outcomes on re-rupture incidence, time to re-rupture, re-operations and contralateral ACL tear in 316 patients < 20 years undergoing primary single bundle ACLR. They followed patients to a similar post-operative timeline (mean 60 mo, range 36-120) as the current study, and reported an 18% re-rupture rate, with almost 18% of patients further experiencing a contralateral ACL injury, with a mean time to re-rupture of 21.6 mo. Unfortunately, sample sizes within the two cohorts were not large enough to permit an adequately powered statistical comparison. There are known limitations with comparing samples across different studies, such as differences in post-operative rehabilitation regimes and differences in activity/sport status. However, these were both Australian patient cohorts and at the very least the encouraging outcomes in the double bundle ACLR cohort in the current study suggests a platform for further research.
ACLR does not guarantee the patient to return to sport, and as reported by Ardern et al[15] only 63% of patients may resume pre-injury level of activity participation and only 44% return to competition. Therefore, the patients ability to return to sport is often a measure of both surgical and rehabilitation success, as well as a measure of patient satisfaction[16]. The current study demonstrated that 54.9% of patients undergoing double bundle ACLR were able to return to their pre-operative level of competitive sport, and these statistics are in keeping with previous studies that have quoted a return to sport percentage of 50%-70% for double bundle ACLR[17,18].
Despite 55% of patients in the current study returning to their pre-operative level of competitive sport, almost 89% were satisfied with their outcome at the time of follow up with a mean score of 4.27/5. This highlights the varied factors that contribute to a satisfied patient. Satisfaction rates in the current study are comparable to that reported by Günay et al[19] who investigated post-operative satisfaction at minimum two years follow up of 29 transphyseal ACLR patients, revealing a mean satisfaction level of 9/10, with 41% of patients returning to their pre-morbid level of sport[19]. In addition, Toritsuka et al[20] investigated 78 patients undergoing double bundle ACLR and reported 94% had a near normal, to normal feeling knee. While patient-reported outcomes remain a critical outcome measure in the success of an operation, there are limitations with retrospective measures of patient satisfaction. Satisfaction draws on the patient’s ability to recall their pre-operative state, the surgical procedure, and the early, mid, and later post-operative phases.
While the double bundle ACLR configuration may provide a more robust graft construct, apprehension throughout the orthopedic community does exist. Firstly, it is a more technically demanding surgical procedure which may also contribute to longer operating times. Secondly, a Cochrane review by Tiamklang et al[8] in 2012, demonstrated no statistical differences between single and double bundle ACLR methods in patient-reported outcomes scores (Lysholm score, International Knee Documentation Committee score and Tegner score), adverse events and both short and long-term complications[8]. However, even with the limited data available, the double bundle configuration favored a better return to pre-injury level sport, anterior (KT-1000) and rotational (pivot shift) knee stability measures, and the development of newly occurring meniscal injuries[8]. While these benefits may be of higher relevance in the young active cohort, this review did not sub-categorize participants into different age groups to better evaluate the high-risk younger population.
A recent study by Sonnery-Cottet et al[21] in 2017 looked at anterior lateral ligament (ALL) reconstruction in conjunction with ACLR. The study concluded that graft failure was 2.5 times less likely in those with ALL and ACL reconstruction when compared with ACL reconstruction alone. The use of extra-articular ligamentous restraint may be the future direction of ACLR; however, longer term follow-up is needed. Unfortunately, young athletes with ACL ruptures are often still considered to have a career ending sporting injury. Future research should include randomized controlled trials comparing single bundle, double bundle, and ALL ACLR techniques in younger patients to better ascertain the optimal surgical technique in this high-risk population.
There are several limitations to acknowledge in the current study. Firstly, the retrospective nature of the study precludes data being collected from early post-operative time points. Secondly, while comparisons have been made to the existing literature by Webster et al[2] looking at young Australians undergoing single bundle ACLR using autologous hamstrings, there are limitations with cross evaluating two separate studies. This may include differences in pre-operative and post-operative demographics, management, and rehabilitation regimes, provided to patients. For example, there were discrepancies between the distribution of males and females in those < 20 years of age, with a 64% male population in the Webster et al[2] paper and only 49% in this sample population. Therefore, a gender bias may present in comparing those two cohorts. In addition, the current study had a patient response rate of 81%. Webster et al[2] reported a response rate of 89% in their young cohort, while others have reported a response rate of 79% at 2 years follow-up[2,22]. While patients over this post-operative time frame will be lost to attrition, there are always issues with missing data in the non-responder population and studies have suggested they may have worse outcomes[22]. Finally, the value in the current study presented the incidence (and timing) of ACL re-tear and contralateral ACL injury in this young cohort undergoing double bundle ACLR using autologous hamstrings. However, it was clearly underpowered to show statistical significance that a double bundle ACLR hamstring configuration would provide a reduced failure rate than single bundle configurations, in these young patients. The active nature and high failure rates in a younger population make this cohort useful in detecting differences in durability between these varied graft constructs.
In conclusion, this study presents a low ACL graft re-injury rate in young patients undergoing double bundle ACLR with a hamstring autograft, 6.6% in < 30-year old’s and 9.1% in < 20-year-olds. The incidence of contralateral ACL injury was 11.1%. While underpowered to detect statistically significant differences in patients < 20-years old, these rates appear better than that reported in a similarly aged cohort undergoing single bundle ACLR[2]. Further research is required to ascertain if double bundle ACLR produces better outcomes for these high-risk patients, particularly with respect to graft longevity and longer-term knee health.
Anterior cruciate ligament reconstruction (ACLR) is a common procedure in the young active population. Current re-rupture rates in single bundle techniques have been quoted as high as 20%-30%. While studies have shown that there are similar functional outcomes between single and double bundle ACL reconstruction techniques the re-rupture rates have not been well reported.
This body of research aims to investigate if double bundle ACL reconstruction techniques have lower re-rupture rates in comparison to single bundle ACL reconstruction.
The main objective of this research was to compare re-rupture rates of single bundle and double bundle ACL reconstruction in the young, active population. If re-rupture rates are suggestive of being lower, more research, such as a randomized control trial between the two techniques could be done to further assess the viability of double bundle ACL reconstruction, specifically in these patients.
All patients under the age of 30 years old who underwent a double bundle ACL reconstruction at a single orthopedic clinic were assessed for eligibility for the study. Of the 112 patients, 91 (81.3%) could be contacted to complete an over the phone questionnaire. Outcomes assessed included the incidence (and timing) of subsequent re-tear and contralateral ACL tear, further surgeries, incidence and time to return to sport, and patient satisfaction. Chi-Squared tests (P < 0.05) were then used to compare the population in this study and a recent study by Webster et al[2], looking at re-rupture rates in single bundle ACL reconstructions from a similar population.
Six of the 91 patients enrolled in the study suffered from re-rupture (6.6%, 95%CI, 1.4–11.7). The mean time to re-rupture was 28 mo (range 18-24) with an additional 14 patients (15.4%) suffering from a contralateral ACL tear in the follow-up period. 14 patients (15.4%) required further surgery to their ipsilateral knee. 50 patients (54.9%) managed to return to their pre-injury level of sport, unfortunately, none of the professional level athletes returned o profession level sport. 1 patient who played amateur level netball did go on to play at a professional level with their double bundle ACL reconstruction. Comparative analysis of re-rupture rates with the Webster et al[2] paper, that investigated single bundle ACL reconstructions revealed a non-significant chi-squared statistic of 2.348 (P = 0.125).
Double bundle re-rupture rates are low (6.6%). However, while there was a trend towards lower re-rupture rates in the double bundle ACL reconstruction population, there was no statistical significance in comparative testing when compared with a single bundle ACL reconstruction cohort. Double Bundle ACL reconstruction may have lower re-rupture rates that single bundle techniques but further research needs to be done to investigate these theories. The risk of re-rupture with double bundle ACL reconstruction is low in the young, active population. When compared with single bundle ACL reconstruction techniques, double bundle reconstructions have at least comparable re-rupture rates. Further research is needed to fully investigate the re-rupture rate differences between these two techniques. There is a significant paucity of knowledge regarding double bundle ACL reconstruction outcomes, with few studies investigating re-rupture rates in the young, active population. Double bundle ACL reconstruction has lower re-rupture rates than single bundle ACL reconstruction in the young, active population. Double bundle ACL reconstruction could be considered as a technique to adopt in high risk, young, active patients. Double bundle reconstructions have low re-rupture rates in the young, active, population. These rates are at least comparable with current single bundle ACL reconstruction re-rupture rates. The hypothesis that double bundle ACL reconstructions would have lower re-rupture rates in the young, active population when compared with single bundle techniques was not proven in this study. However statistical analysis reported no significant difference between the two techniques with regard to re-rupture rate. Double bundle ACL reconstruction could be considered as a technique for young, active patients with ACL tears looking for repair.
Double bundle ACL reconstruction could be considered as technique in young, active patients with ACL tears looking for repair. Further research is required to investigate more deeply the differences in outcomes (in particular re-rupture rates) between these two techniques in the young, active population. A randomized control trial looking at the two techniques, double bundle vs single bundle ACL reconstruction, would provide the highest level of evidence.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Abulezz TA, Anand A S-Editor: Gong ZM L-Editor: A E-Editor: Ma YJ
| 1. | Shea KG, Carey JL, Richmond J, Sandmeier R, Pitts RT, Polousky JD, Chu C, Shultz SJ, Ellen M, Smith A, LaBella CR, Anderson AF, Musahl V, Myer GD, Jevsevar D, Bozic KJ, Shaffer W, Cummins D, Murray JN, Patel N, Shores P, Woznica A, Martinez Y, Gross L, Sevarino K; American Academy of Orthopaedic Surgeons. The American Academy of Orthopaedic Surgeons evidence-based guideline on management of anterior cruciate ligament injuries. J Bone Joint Surg Am. 2015;97:672-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Webster KE, Feller JA. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44:2827-2832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 367] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 3. | Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 374] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 4. | Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8:229-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Chee MY, Chen Y, Pearce CJ, Murphy DP, Krishna L, Hui JH, Wang WE, Tai BC, Salunke AA, Chen X, Chua ZK, Satkunanantham K. Outcome of Patellar Tendon Versus 4-Strand Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Prospective Randomized Trials. Arthroscopy. 2017;33:450-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;216-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1147] [Cited by in RCA: 948] [Article Influence: 19.0] [Reference Citation Analysis (1)] |
| 7. | Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Suomalainen P, Järvelä T, Paakkala A, Kannus P, Järvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40:1511-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 10. | Kondo E, Yasuda K, Azuma H, Tanabe Y, Yagi T. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med. 2008;36:1675-1687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 224] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 11. | Mohtadi N, Chan D, Barber R, Paolucci EO. Reruptures, Reinjuries, and Revisions at a Minimum 2-Year Follow-up: A Randomized Clinical Trial Comparing 3 Graft Types for ACL Reconstruction. Clin J Sport Med. 2016;26:96-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Branch TP, Siebold R, Freedberg HI, Jacobs CA. Double-bundle ACL reconstruction demonstrated superior clinical stability to single-bundle ACL reconstruction: a matched-pairs analysis of instrumented tests of tibial anterior translation and internal rotation laxity. Knee Surg Sports Traumatol Arthrosc. 2011;19:432-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Lee YS, Nam SW, Sim JA, Lee BK. Comparison of anatomic ACL reconstruction between selective bundle reconstruction and double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:2803-2810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N. Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med. 2010;38:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 159] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 15. | Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1016] [Cited by in RCA: 842] [Article Influence: 60.1] [Reference Citation Analysis (0)] |
| 16. | Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23:3623-3631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 17. | Brophy RH, Schmitz L, Wright RW, Dunn WR, Parker RD, Andrish JT, McCarty EC, Spindler KP. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40:2517-2522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 275] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 18. | McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD; MOON Group, Reinke EK. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40:2523-2529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 229] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 19. | Günay S, Karaduman A, Oztürk BB. Effects of Aircast brace and elastic bandage on physical performance of athletes after ankle injuries. Acta Orthop Traumatol Turc. 2014;48:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Toritsuka Y, Amano H, Kuwano M, Iwai T, Mae T, Ohzono K, Shino K. Outcome of double-bundle ACL reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2009;17:456-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, Helito CP, Thaunat M. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am J Sports Med. 2017;45:1547-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 363] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 22. | Imam MA, Barke S, Stafford GH, Parkin D, Field RE. Loss to follow-up after total hip replacement: a source of bias in patient reported outcome measures and registry datasets? Hip Int. 2014;24:465-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |