Published online Dec 18, 2019. doi: 10.5312/wjo.v10.i12.416
Peer-review started: July 16, 2019
First decision: July 30, 2019
Revised: September 8, 2019
Accepted: September 22, 2019
Article in press: September 22, 2019
Published online: December 18, 2019
Processing time: 151 Days and 17 Hours
Many orthopedic surgeons require that their patients obtain dental clearance before elective total joint arthroplasty (TJA). However, there is no consensus substantiating the practice. To this end, a systematic review on the prevalence of dental pathology in TJA patients, risk factors for failing dental screening, and impact of dental evaluations was performed. Literature was sourced from PubMed and Scopus databases. Six papers were sourced from the initial search, one study was extracted from the references of the original six manuscripts, and one new publication was retrieved from a second search conducted after the first. The prevalence of dental pathology ranged from 8.8% to 29.4% across studies. Two of four papers reported lower than average or improvements in post-operative infection with pre-operative dental evaluations while two found no such association. There is insufficient evidence to support universal dental clearance before TJA.
Core tip: There is insufficient evidence to support universal dental clearance before total knee arthroplasty or total hip arthroplasty procedures for reducing periprosthetic joint infection, even for higher risk patients.
- Citation: Frey C, Navarro SM, Blackwell T, Lidner C, Del Schutte Jr H. Impact of dental clearance on total joint arthroplasty: A systematic review. World J Orthop 2019; 10(12): 416-423
- URL: https://www.wjgnet.com/2218-5836/full/v10/i12/416.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i12.416
While there have been improvements in total joint arthroplasty (TJA) throughout the years, it is compromised by the risk of periprosthetic joint infection (PJI), the most common cause of total knee arthroplasty (TKA) and total hip arthroplasty (THA) failure[1,2]. It is a devastating complication which results in significant patient morbidity. Infected revisions can easily exceed the cost of performing the primary arthroplasty and are projected to total $ 1.62 billion by 2020[3]. Key risk factors have been determined, and include poor nutritional status, smoking, inadequate blood sugar control, and poor dental health[4,5,6]. Ideally, knowledge of these factors can be used to develop risk mitigation strategies. One potential application is discerning the impact of dental procedures and pathologies on adverse outcomes in TJA.
There exists no absolute criteria or single test to diagnose PJI. Instead, diagnosis is based upon a mixture of lab results, cultures, and clinical findings[7]. The implication of a dental source is often based upon both the identification of a pathogen considered to be a constituent of the patient’s oral flora at the infection site and the timing of the infection with a seeding procedure[8]. This premise is based upon the finding that many events such as dental scaling and brushing one’s teeth can cause transient bacteremia when dental pathology is present[9,10]. Such reports have been cited when implementing dental prophylaxis in arthroplasty patients prior to dental procedures. Conversely, some orthopedic surgeons recommend that patients receive preoperative prophylactic antibiotics and/or dental clearance before TJA.
Given the lack of overarching guidelines on the role of dental clearance and its association with TJA outcomes, a systematic review was performed using data from primary studies to summarize the prevalence of dental pathology in patients scheduled for TKA and THA and the impact of dental evaluation and necessary interventions on outcomes.
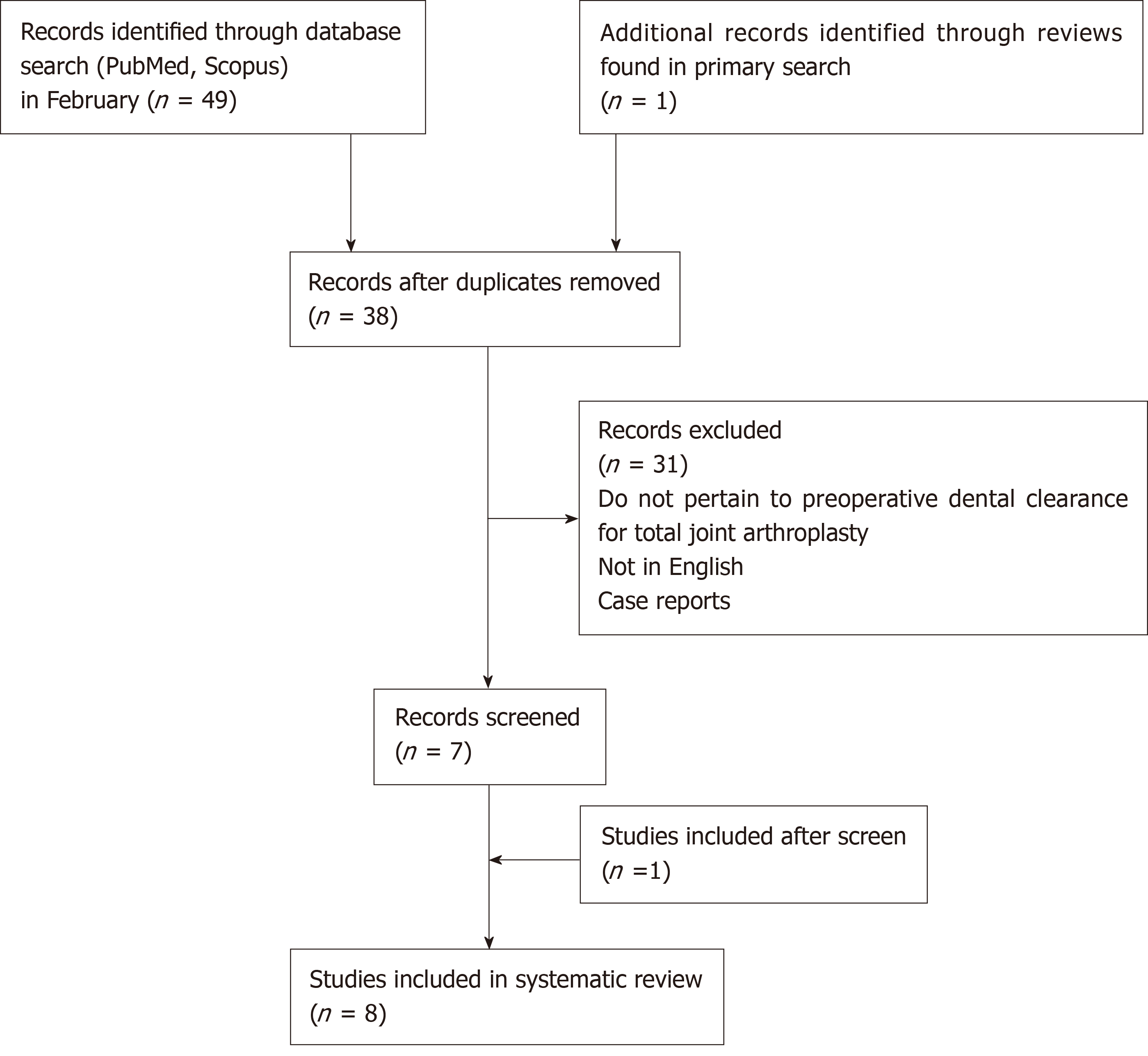
The literature search consisted of PubMed and Scopus database inquiries in February 2019 for the impact of dental clearance and the epidemiology of significant dental pathology in potential TJA patients (Figure 1). This was conducted by one author. Search terms consisted of “Arthroplasty AND Dental AND Clearance” and “Arthroplasty AND Dental AND Hygiene” for both databases. This yielded 6 papers that met all of the criteria (Table 1). One additional paper was selected from a review article that resulted from the initial search. Another paper was individually retrieved after the initial screen as it was accepted and published in May.
| Search | Hits |
| PubMed search results | |
| Arthroplasty and dental and clearance | 5 |
| Arthroplasty and dental and hygiene | 21 |
| Sourced from citations | 0 |
| Scopus search results | |
| Arthroplasty and dental and clearance | 5 |
| Arthroplasty and dental and hygiene | 18 |
| Sourced from citations | 1 |
Literature assessing the association between dental clearance and TJA outcomes were included. Manuscripts examining prevalence of and risk factors for failing dental clearance were included as well. Considering the scarcity of evidence, various summary measures were accepted, with a preference for risk ratios. Only human studies within the last 25 years were included to ensure that the results are applicable. Interventional, case-control, and cross-sectional studies were included. In total, eight studies met criteria. All studies were evaluated for quality and bias using a modified 27 item Downs and Black checklist[11]. For the power analysis (item 27), we substituted a simple score of 0 or 1 score. Papers received one point if they included power calculations. We decided to utilize this instrument to evaluate methodological quality because it is validated for both randomized and non-randomized studies. We did not use a formal metric to estimate risk of bias across studies.
After the studies were included, data concerning impact of dental clearance, model used, sample size, methods, results with statistical analysis, and conclusions were extracted by one author and transcribed in a table. This was reviewed by another author for verification. Next, inputs for the methodological quality analysis with the Downs and Black checklist were extracted.
Eight studies were included[12-19]. Of the 8, 7 (86%) included a dental evaluation performed by a dental professional[12-14,16-19] and five utilized questionnaires or interviews (71%)[13-17]. One paper used a questionnaire alone[15]. Although papers were selected from peer reviewed publications, 2 were not listed on PubMed[15,19]. The articles scored between 15 and 23 using our modified DandB checklist (Table 2). The papers were limited by several factors. For instance, none of the selected manuscripts were randomized or blinded, increasing risk of bias. Additionally, many of the papers had small sample sizes, and none demonstrated calculation of power. Lastly, it should be noted that the paper by Barrington and Barrington was designed to capture the primary outcome of dental pathology incidence, not for detecting PJI[16].
| Adamkiewicz et al[12] | Tokarski et al[13] | Vuorinen et al[14] | Wood et al[15] | Barrington et al[16] | Lampley et al[17] | Tai et al[18] | Sonn et al[19] | |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q2 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| Q3 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| Q4 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q5 | 1 | 2 | 2 | 2 | 1 | 1 | 2 | 1 |
| Q6 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q7 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 |
| Q8 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| Q9 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q10 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 |
| Q11 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q12 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 |
| Q13 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q16 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q17 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q18 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 |
| Q19 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q20 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q22 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q23 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q24 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Q25 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| Q26 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Q27 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 21 | 22 | 22 | 19 | 15 | 20 | 23 | 22 |
Four studies focused on the prevalence of dental pathology and/or dental hygiene practices in patients to undergo TJA (Table 3)[12-15]. Adamkiewicz et al[12] had dental evaluations performed on patients admitted for TJA preoperative workup in Poland. They found that 28.5% had clinically significant periodontal disease. This compares with 23% in previously published national data[20]. There were no significant differences in inflammatory markers or cell counts between the periodontal disease and healthy groups.
| Author | Model | n | Methods | Results | Conclusion |
| Adamkiewicz et al[12] | Patients at a tertiary University Hospital in Poland | 228 | Patients admitted for elective TJA received dental evaluation along with standard preoperative workup | Clinically significant periodontal disease was detected in 28.5% of patients | Periodontal disease is prevalent in patients undergoing TJA |
| Tokarski et al[13] | Patients at a tertiary care center in the United States | 300 | Patients answered a dental hygiene questionnaire then received dental evaluations and necessary interventions | 12% failed dental clearance. Patients with one or more of: Narcotic use, tobacco use, or last dentist visit over one year ago, had a 22% risk of failure compared to 6% for patients with no risk factors | It may be reasonable to only screen high risk patients for dental pathology |
| Vuorinen et al[14] | Patients at a public, tertiary care hospital in Finland | 731 | Patients filled out a prospective dental health questionnaire and underwent a dental examination and necessary interventions | 29.4% of patients failed dental clearance. 5.1% of patients had severe periodontitis. Tobacco use and root canal were risk factors. Regular dental examination was a preventive factor | The inspection and treatment of dental pathology is important prior to elective TJA |
| Wood et al[15] | Patients at a large academic center in Canada | 453 | Patients answered a dental hygiene survey at their 6 wk post-operative appointment | 76% of patients had a cleaning within 12 mo. 5% did not visit a dentist. 49% were informed of the impact of dental hygiene in reducing PJI | Patients generally have good oral hygiene, but patient education is inconsistent |
Tokarski et al[13] employed a dental hygiene questionnaire along with a dental evaluation. They found that 12% failed dental clearance, which, in this case, was defined as requiring a tooth extraction or root canal. The number increases to 19% when patients requiring fillings are included. Additionally, they identified that patients with one of three key risk factors (narcotic use, tobacco use, and last dentist visit over one year ago) had a 22% chance of failing the dental evaluation, compared with 6% if they did not have any.
Vuorinen et al[14] also used both questionnaires and dental evaluation in an attempt to determine which patients ought to receive dental clearance based on risk factors. Twenty-nine point four percent of patients failed clearance, 34% were found to have moderate gingivitis, and 5.1% of patients had severe periodontitis. This compares with national reports that 27% of Finnish patients had periodontal disease[21]. It was found that the only significant risk factors for failing dental clearance were history of root canal, dental visit for symptoms within the last 3 mo, infrequent dental checkups, and tobacco use. Patients with regular examination and no history of root canal were 50% less likely to fail clearance.
Lastly Wood et al[15] used a post-operative dental hygiene survey without professional dental evaluation. They found that patients in general report adequate oral hygiene and 76% having had a dental cleaning within the last year. Only 5% admitted to not having a dentist.
Four studies measured the impact of preoperative dental clearance on TJA outcomes (Table 4)[16-19]. Barrington and Barrington required patients to receive dental evaluation and the appropriate interventions before elective TJA[16]. Twenty-three percent were found to have active tooth decay requiring treatment. There were no significant differences between primary and revision groups. Although it was not the primary outcome, there were no infections related to the operation detected within the first 90 d post-operatively in any of the 100 patients.
| Author | Model | n | Methods | Results | Impact of clearance |
| Barrington et al[16] | Patients at a metropolitan, tertiary arthroplasty practice in the United States | 100 | Patients obtained dental clearance, cleaning, and dental interventions. On POD 1 or POD 2, patients were interviewed | 23% were not cleared due to dental decay and were treated. There were no periprosthetic infections within 90 d. One in four patients had dental pathology | It is difficult to draw a definitive conclusion |
| Lampley et al[17] | Elective TJA and hip fracture patients in a tertiary arthroplasty practice in the United States | 519 | Patients obtained dental clearance, cleaning, and interventions. On POD 1 or POD 2, patients were interviewed | Early postoperative infection rate was significantly lower in the clearance group. Only one infection had a possible dental source | Dental clearance and interventions did not reduce early postoperative infection |
| Tai et al[18] | Patients s/p resection arthroplasty and uninfected TKA controls from the Taiwanese NHIRD | 6295 | Patients with removal of infected TKA were matched with TKA patients without infections from the NHIRD and retrospectively analyzed | Compared to patients who did not receive scaling, those who received scaling once and 5-6 times in the previous three years had 20% and 31% less risk of TKA infection, respectively | Dental scaling was associated with lower risk of infection |
| Sonn et al[19] | Elective TJA patients at an unspecified location | 2457 | The data for a consecutive TJA patients was retrospectively analyzed | There were no significant associations between complication and dental evaluation or extraction | Dental evaluation +/- extraction did not improve complication rates |
Lampley and colleagues compared postoperative infections between elective TJA patients who had received dental clearance and hip fracture patients who received THA or hemiarthroplasties who did not receive pre-operative dental clearance[17]. Out of the patients who received dental clearance, 8.8% required treatment for periodontal disease. There was no significant difference in postoperative infection (less than 6 mo post-op) requiring reoperation. Of the 6 (1.7%) patients with infections in the elective group, only one failed the dental screen. A pathogen was detected in 5 out of the 6 cases. Four (2.5%) patients in the hip fracture group required reoperation for infection concern. Only one patient had an identifiable pathogen. None of the pathogens except, possibly, Peptostreptococcus magnus in the dental clearance group were of likely dental origin.
Tai et al[18] utilized a retrospective data from the National Health Insurance Research Database (NHIRD) to compare TKA patients who required “removal of hardware” plus 7 d of antibiotics within five years of the operation to those who did not. They found that dental checkups and scaling were associated with significantly lower post-operative infection rates. Only 7.1% of the infection group had regular checkup and scaling (5-6 times over last three years) compared to 9.9% in the healthy group. Moreover, 73.1% had no visits in the infection group compared to 67.8% in the healthy group. The adjusted OR of PJI when receiving regular checkup and scaling was 0.69 (0.54-0.89) and 0.84 (0.71-0.99) when less frequent.
Sonn et al[19] performed a retrospective review of 2457 patients who underwent primary TJA. Seventy-nine point one percent of these patients received dental evaluation before the operation, however, it appears this was decided on an individualized basis and not based on a predetermined, randomized approach. Complication-free rates at 36 mo were similar between those who did and did not receive dental evaluation. Although not significant, both the dental evaluation and extraction groups appeared more hazardous than the groups that did not have a dental workup [Hazard ratio (HR) = 1.95, P = 0.07 and HR = 1.24, P = 0.57]. The rate of PJI was measured to be 1.51%, however this was not compared between groups.
In this systematic review, we attempted to capture the prevalence of dental pathology and risk factors in populations in consideration for TJA as well as the impact of dental clearance and interventions on the outcomes of TJA procedures. In order to advocate for the institution of these rules, the benefits of pre-operative dental evaluation must outweigh the not-insignificant costs imposed on patients and the healthcare system at a whole. Overall, there is not enough concrete evidence to support dental evaluation for all patients.
We included four studies that paint a picture of dental health of TJA patients. Failure of dental clearance ranged from 8.8%[17] to 29.4%[14]. However, the standards for evaluation varied. The criteria used by Tokarski et al[13] measured failure as requiring tooth extraction or root canal. In fact, when carious lesions are included, failure rates increased from 12% to 19%[13]. Similarly, Lampley et al[17] measured failure as dental pathology necessitating intervention prior to surgery and only found a failure rate of 8.8%. Wood and colleagues detected good overall dental hygiene at a tertiary care center in Canada with 76% having had a dental checkup within the previous 12 mo and only 5% admitting to not seeing a dentist[15]. When compared by region, TJA patients in American tertiary care centers had failure rates from 8.8% to 23%[13,16]. This is moderately higher than failure rates in Poland (28.5%)[12] and Finland (29.4%)[14]. However, it is difficult to pool data do to differences in baseline patient population oral health status and variation in dental evaluation practice.
Two of the studies evaluated risk factors for failing dental clearance. Tokarski et al[13] found that of several risk factors, patients who had one or more of: Narcotic use, tobacco use, and no dental visit within the last 12 mo had a 22% risk of failure compared to 6% for patients with no risk factors. The authors concluded that it is feasible to exclusively screen those with high risk profiles. However, Vuorinen et al[14] found that tobacco use, history of root canal, dental visit for symptoms, and infrequent dental visits were significant risk factors. Patients with no root canal and regular checkups were less likely to fail, but grouping, as performed in the previous study, did not yield a significantly different risk profile. The authors concluded that they were unable to identify a group of patients who could avoid dental clearance.
We identified four papers that detail the impact of dental clearance and/or necessary interventions on the outcomes of TJA, with one of the four finding a significant positive impact of dental clearance and/or evaluation[16,18]. Firstly, Barrington and Barrington detected pathology requiring treatment in 23% of patients[16]. No periprosthetic joint infections were detected within 90 d of surgery. However, the study was small (n = 100) and not designed to capture the effect of dental evaluations so the results are difficult to interpret. Tai et al[18] found that patients with frequent dental scaling in the previous three years had 31% lower risk of PJI after TKA than those who did not receive scaling. Although these results reflect well upon frequent dental examination and scaling, it does not directly assess the impact of pre-operative dental clearance. In contrast, neither Lampley et al[17] nor Sonn et al[19] found evidence to support dental evaluations. Although the hip fracture group in the former study had an insignificantly higher reoperation rate (2.5% vs 1.7%), hardware was not removed in any of the four cases as no bacterial infection was identified. It should be noted that there were no true controls, follow up was poor in the hip fracture group (18% were deceased), and the threshold for failing clearance was high. Sonn et al[19] actually found higher complication rates in the dental evaluation and extraction groups, although this was not significant. This may be attributed to other confounding health risks not captured by the study.
The results of our systematic analysis are somewhat in line with current recommendations. In the proceedings of international consensus on orthopedic infections, 92% of voters agreed that patients with oral disease should receive appropriate interventions before elective TJA to reduce risk of infection despite limited evidence[8]. It was proposed that dental screening may be required for high risk patients. 76% of voters agreed that dental clearance should not be required for all patients to undergo TJA. Much like how prophylactic antibiotics for common dental procedures in all patients with joint prostheses is falling out of favor, we expect dental clearance protocol to change as new data emerges[22-25]. At the moment, we would not recommend for universal dental screening before TJA.
We performed this study to preferred reporting items for systematic reviews and meta-analyses guideline standards, however, there were still several limitations. First and foremost, literature regarding dental clearance for TJA is scarce. Our methods only disinterred four papers capturing the impact of dental evaluation and/or treatment on infections after TJA. Considering the relatively low incidence of periprosthetic infection, few of the studies were adequately powered to detect significance and none were designed as randomized controlled trials. Additionally, there is no common standard for preoperative dental evaluation. Criteria for failing dental clearance ranged from diagnosing dental caries to requiring tooth extraction or root canals. Amongst studies assessing prevalence of dental pathology, differences in location and clinical setting hinder synthesis of data. Lastly, some studies relied on self-reporting of questionnaires and surveys, which incur several inherent biases[26].
With an aging population, the number of total joint arthroplasties is likely to continue growing. Periprosthetic infection remains a great concern and quality improvement problem despite improvements in sterile and prophylactic techniques. There is little evidence to support universal dental clearance before TJA, even for higher risk patients. There remains a need for future research to elucidate the mechanism of periprosthetic infections and more robust analysis of patients with high risk dental pathologies to help guide interventions.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fenichel I, Pavone P, Peng BG S-Editor: Tang JZ L-Editor: A E-Editor: Liu MY
| 1. | Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 841] [Cited by in RCA: 913] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 2. | Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J. Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res. 2010;468:2046-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 180] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 3. | Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61-5.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1101] [Cited by in RCA: 1224] [Article Influence: 94.2] [Reference Citation Analysis (0)] |
| 4. | Romero J, Jones R, Brown T. Modifiable risk factors and preoperative optimization of the primary total arthroplasty patient. Curr Orthop Pract. 2017;28:272-275. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Alamanda VK, Springer BD. Perioperative and Modifiable Risk Factors for Periprosthetic Joint Infections (PJI) and Recommended Guidelines. Curr Rev Musculoskelet Med. 2018;11:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017;99-B:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 7. | Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty. 2018;33:1309-1314.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 885] [Cited by in RCA: 1407] [Article Influence: 201.0] [Reference Citation Analysis (0)] |
| 8. | Ares O, Arnold WV, Atilla B, Kumar Bari A, Battenberg A, Belzino M, Bhoite S, Clauss M, Egoavil M, Ferrand ML, Greenky M, Sarango J, Komnos G, Koo KH, Lee YK, Leibnitz M, Luis E, Naneti G, Ottolenghi J, Poojary A, Shen H, Sousa R, Thomas P, Volodymyr F, Wang Q. General Assembly, Prevention, Host Related Local: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019;34:S3-S12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Maharaj B, Coovadia Y, Vayej AC. An investigation of the frequency of bacteraemia following dental extraction, tooth brushing and chewing. Cardiovasc J Afr. 2012;23:340-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Forner L, Larsen T, Kilian M, Holmstrup P. Incidence of bacteremia after chewing, tooth brushing and scaling in individuals with periodontal inflammation. J Clin Periodontol. 2006;33:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 469] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 11. | Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5177] [Cited by in RCA: 5933] [Article Influence: 219.7] [Reference Citation Analysis (0)] |
| 12. | Adamkiewicz K, Płatek AE, Łęgosz P, Czerniuk MR, Małdyk P, Szymański FM. Evaluation of the prevalence of periodontal disease as a non-classical risk factor in the group of patients undergoing hip and/or knee arthroplasty. Kardiol Pol. 2018;76:633-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Tokarski AT, Patel RG, Parvizi J, Deirmengian GK. Dental clearance prior to elective arthroplasty may not be needed for everyone. J Arthroplasty. 2014;29:1729-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Vuorinen M, Mäkinen T, Rantasalo M, Leskinen J, Välimaa H, Huotari K. Incidence and Risk Factors for Dental Pathology in Patients Planned for Elective Total Hip or Knee Arthroplasty. Scand J Surg. 2018;1457496918816911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Wood TJ, Petruccelli D, Piccirillo L, Staibano P, Winemaker M, de Beer J. Dental hygiene in maintaining a healthy joint replacement: a survey of Canadian total joint replacement patients. Curr Orthop Pract. 2016;27:515-519. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Barrington JW, Barrington TA. What is the true incidence of dental pathology in the total joint arthroplasty population? J Arthroplasty. 2011;26:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Lampley A, Huang RC, Arnold WV, Parvizi J. Total joint arthroplasty: should patients have preoperative dental clearance? J Arthroplasty. 2014;29:1087-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Tai TW, Lin TC, Ho CJ, Kao Yang YH, Yang CY. Frequent Dental Scaling Is Associated with a Reduced Risk of Periprosthetic Infection following Total Knee Arthroplasty: A Nationwide Population-Based Nested Case-Control Study. PLoS One. 2016;11:e0158096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Sonn KA, Larsen CG, Adams W, Brown NM, McAsey CJ. Effect of Preoperative Dental Extraction on Postoperative Complications After Total Joint Arthroplasty. J Arthroplasty. 2019;34:2080-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Konopka T, Dembowska E, Pietruska M, Dymalski P, Górska R. Periodontal status and selected parameters of oral condition of Poles aged 65 to 74 years. Przegl Epidemiol. 2015;69:537-542, 643-647. [PubMed] |
| 21. | Suominen-Taipale L, Nordblad A, Vehkalahti M, Aromaa A. Oral health in the Finnish adult population: Health 2000 survey. Publications of the National Public Health Institute. Helsinki: Kansanterveyslaitos; 2008; . |
| 22. | Young H, Hirsh J, Hammerberg EM, Price CS. Dental disease and periprosthetic joint infection. J Bone Joint Surg Am. 2014;96:162-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Watters W, Rethman MP, Hanson NB, Abt E, Anderson PA, Carroll KC, Futrell HC, Garvin K, Glenn SO, Hellstein J, Hewlett A, Kolessar D, Moucha C, O'Donnell RJ, O'Toole JE, Osmon DR, Evans RP, Rinella A, Steinberg MJ, Goldberg M, Ristic H, Boyer K, Sluka P, Martin WR, Cummins DS, Song S, Woznica A, Gross L; American Academy of Orthopedic Surgeons; American Dental Association. Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures. J Am Acad Orthop Surg. 2013;21:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 24. | Sollecito TP, Abt E, Lockhart PB, Truelove E, Paumier TM, Tracy SL, Tampi M, Beltrán-Aguilar ED, Frantsve-Hawley J. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners--a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146:11-16.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 25. | DeFroda SF, Lamin E, Gil JA, Sindhu K, Ritterman S. Antibiotic Prophylaxis for Patients with a History of Total Joint Replacement. J Am Board Fam Med. 2016;29:500-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Choi BC, Pak AW. A catalog of biases in questionnaires. Prev Chronic Dis. 2005;2:A13. [PubMed] |