Copyright
©The Author(s) 2016.
World J Orthop. May 18, 2016; 7(5): 272-279
Published online May 18, 2016. doi: 10.5312/wjo.v7.i5.272
Published online May 18, 2016. doi: 10.5312/wjo.v7.i5.272
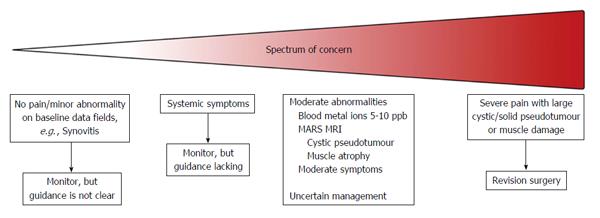
Figure 1 Diagram demonstrating the spectrum of concern for patients with metal-on-meta hip implants.
The decision on how to manage patients at the extremes of the spectrum is relatively straightforward. However the majority of patients fall into to the middle category, where the management is uncertain or difficult. MRI: Magnetic resonance imaging; MARS: Metal artefact reduction sequence.
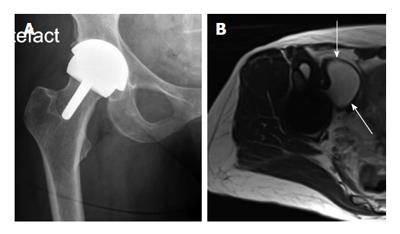
Figure 2 Middle of the spectrum - A typical patient with moderate problems.
This 58-year-old very active lady with a right hip resurfacing arthroplasty (A: X-ray AP hip) implanted 8 years ago. She has minimal symptoms and moderately raised blood metal ion levels (Cobalt 13 ppb, Chromium 7 ppb). A magnetic resonance imaging scan (B: Axial T2 weighted image) has revealed a 6 cm cystic pseudotumour anterior to the hip (arrows).
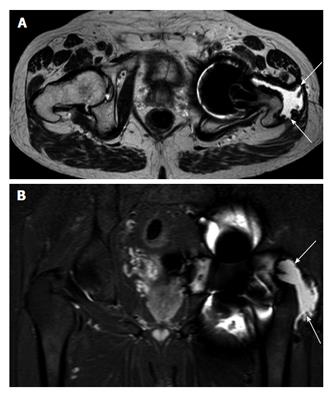
Figure 3 Axial (A) and coronal (B) magnetic resonance imaging.
Example of abductor stripping secondary to a pseudotumour (marked by arrows). The pseudotumour can be seen traversing the posterior hip around the greater tuberosity onto its lateral aspect, which is now void of abductor tendon insertion.
Figure 4 A 58-year-old patient with bilateral large diameter total hip replacement metal-on-meta implanted 9-years ago, moderate hip symptoms and raised metal ion levels (Cobalt 17 ppb, Chromium 13 ppb).
She presented to the general surgeons with abdominal pain and distension. Coronal magnetic resonance imaging scan (above) demonstrated a large cystic pseudotumour extending into the pelvis up to the level of the L2 vertebra and abutting the right kidney in the retroperitoneal space (arrows). The cystic pseudotumour was drained prior to surgical excision with both orthopaedic and vascular surgeons present.
- Citation: Berber R, Skinner JA, Hart AJ. Management of metal-on-metal hip implant patients: Who, when and how to revise? World J Orthop 2016; 7(5): 272-279
- URL: https://www.wjgnet.com/2218-5836/full/v7/i5/272.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i5.272