Published online Apr 28, 2016. doi: 10.4329/wjr.v8.i4.390
Peer-review started: November 26, 2015
First decision: January 6, 2016
Revised: January 22, 2016
Accepted: February 16, 2016
Article in press: February 17, 2016
Published online: April 28, 2016
Processing time: 145 Days and 13.3 Hours
AIM: To evaluate whether intra-procedural cone-beam computed tomography (CBCT) performed during modified balloon-occluded retrograde transvenous obliteration (mBRTO) can accurately determine technical success of complete variceal obliteration.
METHODS: From June 2012 to December 2014, 15 patients who received CBCT during mBRTO for treatment of portal hypertensive gastric variceal bleeding were retrospectively evaluated. Three-dimensional (3D) CBCT images were performed and evaluated prior to the end of the procedure, and these were further analyzed and compared to the pre-procedure contrast-enhanced computed tomography to determine the technical success of mBRTO including: Complete occlusion/obliteration of: (1) gastrorenal shunt (GRS); (2) gastric varices; and (3) afferent feeding veins. Post-mBRTO contrast-enhanced CT was used to confirm the accuracy and diagnostic value of CBCT within 2-3 d.
RESULTS: Intra-procedural 3D-CBCT images were 100% accurate in determining the technical success of mBRTO in all 15 cases. CBCT demonstrated complete occlusion/obliteration of GRS, gastric varices, collaterals and afferent feeding veins during mBRTO, which was confirmed with post-mBRTO CT. Two patients showed incomplete obliteration of gastric varices and feeding veins on CBCT, which therefore required additional gelfoam injections to complete the procedure. No patient required additional procedures or other interventions during their follow-up period (684 ± 279 d).
CONCLUSION: CBCT during mBRTO appears to accurately and immediately determine the technical success of mBRTO. This may improve the technical and clinical success/outcome of mBRTO and reduce additional procedure time in the future.
Core tip: This is a retrospective study to evaluate the feasibility, usefulness and efficacy of cone-beam computed tomography (CBCT) in modified balloon-occluded retrograde transvenous obliteration (mBRTO) procedures including coil-assisted retrograde transvenous obliteration and plug-assisted retrograde transvenous oblitearation. With an intra-procedural three-dimensional CBCT, the technical success of mBRTO was determined prior to the completion of the procedure in 100% of cases. With CBCT, a complete anatomy of gastric varices including gastrorenal shunt, gastric varices, collaterals, afferent and efferent vessels were identified easily. The CBCT may improve the technical and clinical success of mBRTO procedures and potentially reduce additional procedure time and cost.
- Citation: Lee EW, So N, Chapman R, McWilliams JP, Loh CT, Busuttil RW, Kee ST. Usefulness of intra-procedural cone-beam computed tomography in modified balloon-occluded retrograde transvenous obliteration of gastric varices. World J Radiol 2016; 8(4): 390-396
- URL: https://www.wjgnet.com/1949-8470/full/v8/i4/390.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i4.390
Three-dimensional (3D) cone-beam computed tomography (CBCT) angiography has been used in the past on a variety of interventional procedures including renal biopsies, transcatheter chemoembolization for hepatocellular carcinomas, implantation of intra-arterial port systems in liver metastases, and partial splenic embolization[1-3]. The utilization of CBCT in traditional balloon-occluded retrograde transvenous obliteration (BRTO) in a small number of patients has been also described[4,5]. CBCT is potentially advantageous over conventional CT for interventional procedures as it incorporates 3D CBCT data, fluoroscopy and guidance software[1].
BRTO and modified-BRTO (mBRTO using coil or vascular plug instead of balloon) are receiving increased attention for the management of bleeding gastric varices[6-8]. BRTO has a high efficacy in stopping acute gastric variceal bleeding and has shown to have a significantly lower re-bleeding rate of gastric varices compared to TIPS or endoscopic treatment[9-14]. Recently, our group has shown the effectiveness of mBRTO using coils or vascular plugs in place of balloons[15-17], which is comparable to conventional BRTO[8-12,18,19].
During the BRTO or mBRTO procedure, visualization of the gastric varices, feeding vessels, and its collaterals, is currently guided by 2D angiogram or digital subtraction angiogram. However, a new means of imaging can be used that may provide better visualization. The CBCT is an advanced imaging device that uses C-arm flat-panel fluoroscopy systems to obtain and display 3D images, of which can be obtained during the procedure itself[20]. Therefore, CBCT provides multiple viewing planes compared to the 2D angiogram, which only provides a single plane for images[20].
Currently, there are no angiographic protocols of evaluating the technical success of BRTO or mBRTO during or immediately after the procedure. Traditionally, the obliterated vessels are evaluated with post-procedural CT; however, the intra-procedural CBCT thus allows for immediate assessment during and immediately after the procedure to demonstrate and confirm the complete obliteration/occlusion of varices.
In this study, we demonstrated the effectiveness of intra-procedural CBCT during mBRTO to confirm the technical success of gastric variceal embolization.
This retrospective study was approved by our institutional review board (Medical IRB 2). The patient records were de-identified prior to the analysis and the waiver of consent for retrospective study was granted. We evaluated 15 patients who received CBCT during the mBRTO between June 2012 and December 2014. All 15 patients had pre- and post-procedural contrast-enhanced CT for comparative analysis. Demographic, clinical, and laboratory data were collected and reviewed. All 15 patients underwent mBRTO for treatment of gastric variceal bleeding.
All 15 mBRTO procedures were performed with moderate sedation. Prior to mBRTO procedure, a triple or dual phase contrast-enhanced CT of the abdomen was obtained and reviewed. After pre-procedural planning with CT images, the right common femoral venous access was achieved and an 8 or 14 Fr vascular sheath (Cook Inc. Bloomington, IN, United States) was placed in the inferior vena cava or renal vein. Using a 0.035 glidewire and 4 or 5 Fr glide or C2 catheter, the gastrorenal shunt (GRS) was accessed. The catheter was exchanged with an occlusion balloon to perform a balloon-occluded retrograde venogram to assess and confirm the varices and the size of the shunt.
For coil-assisted retrograde transvenous obliteration (CARTO), our published protocol was performed[16]. Briefly, a double microcatheter system with a combination of two microcatheters (Renegade STC and Hi-Flo microcatheter, Boston Scientific Co., Natick, MA, United States) was used. Through a more proximally placed microcatheter within the GRS, correctly sized detachable coils (average 10.7 ± 3.8, range 4-23 coils, diameters 5-15 mm) were deployed to achieve a complete occlusion of the shunt confirmed with a venogram. Then, through the distally placed microcatheter, embolization was performed using gelfoam slurry (average 5.6 ± 3.0, range 3-15 packs; each pack = 2 cm × 6 cm × 7 mm) mixed with contrast agent, which was injected until the entire GRS, varices, collaterals and afferent feeding veins were in complete stasis.
For plug-assisted retrograde transvenous oblitearation (PARTO), the protocol following Gwon et al[19] was performed using Amplatzer vascular plugs (diameters 18 mm). In brief, instead of a double microcatheter system, a 7 or 8 Fr vascular sheath was advanced over the wire into the efferent GRS. Prior to the vascular plug deployment, a 4 Fr glidecatheter or a microcatheter was advanced into the distal GRS or into the gastric varices. After vascular plug deployment caused a complete stasis within the GRS, gelfoam slurry (average 9 ± 4.5, range 5-15 packs) with contrast agent was injected through the distally placed catheter until the entire GRS, varices, collaterals and afferent feeding veins were in complete stasis.
At this point, C-arm CBCT of the upper abdomen was performed according to the protocol described below. Once the complete occlusion of the efferent shunt, gastric varices, and afferent feeding vessels was confirmed, microcatheters and sheath were removed. During the procedure, the patient’s blood pressure, pulse, electrocardiogram, and arterial oxygen saturation were monitored.
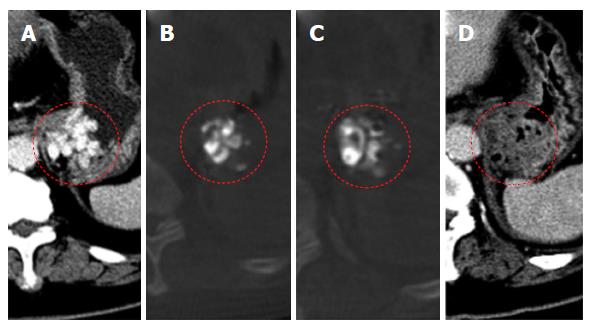
All 15 patients had a triple phase contrast-enhanced CT of abdomen 2-3 d post procedure, to assess the accuracy of CBCT in immediate assessment of obliteration of: (1) efferent GRS, (2) gastric varices, and (3) afferent feeding veins.
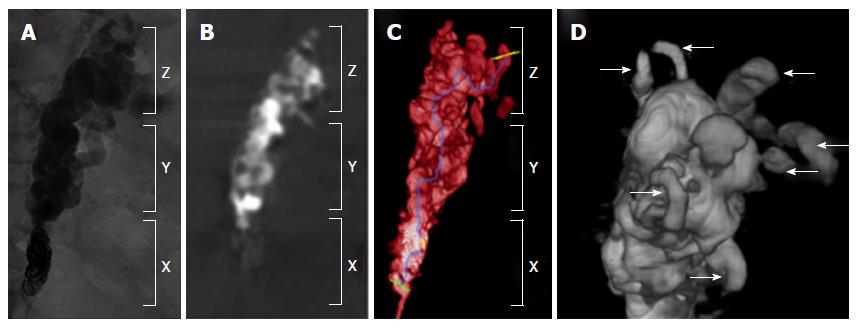
All 15 patients underwent non-contrast C-arm CBCT at the conclusion of mBRTO. Imaging was performed using commercially available flat-panel detectors (Philips Healthcare, Best, the Netherlands). The 2D and 3D images were acquired using XperCT technology and volumetric image reconstruction (Feldkamp back projection) was performed in a dedicated workstation. For each CBCT scan, 312 projection images (30 frames per second) were acquired covering a 200° clockwise arc at a rotation speed of 20° per second. As the images were being acquired, the projections were transferred to the reconstruction workstation. The two-dimensional (2D) projection images were reconstructed by using Feldkamp back projection into 3D volumetric images, with isotropic resolution of 0.98 mm for a 250 mm × 250 mm × 194 mm field of view (matrix size, 256 mm × 256 mm × 256 mm) (Figure 1).
Using 64-multidetector CT scanner (Sensation, Siemens Healthcare, Germany), contrast-enhanced triple phase CT (unenhanced, arterial and portal venous phase) was obtained from all 15 patients 2-3 d after the procedure. A bolus tracking was utilized with a trigger threshold at the upper abdominal aorta of 150 HU. The arterial phase was obtained at a 10-s delay time; and the portal venous phase was obtained at a 40-s delay time. A volume of 100 to 150 mL of iohexol 350 contrast material was used based on patient weight. The following scanning parameters were used: 120 kVp, 160-180 mAs (unenhanced) and 200-240 mAs (arterial and portal venous phase), 0.5 s per gantry rotation, pitch of 1-1.5 and 0.6 mm collimation.
Both CBCT and pre-BRTO contrast-enhanced CT images were evaluated separately by two IR MDs to evaluate the GRS, gastric varices and feeding veins. The degree of post-mBRTO venous thrombosis/obliteration was scored independently (Scale of 1 = minimal thrombosis to 5 = complete thrombosis) and success of mBRTO was determined prior to the end of the procedure. The CBCT images were also independently reviewed and compared to post-mBRTO contrast-enhanced CT images for its accuracy and diagnostic quality in assessing the GRS, gastric varices and feeding veins. The same scoring system was utilized to assess post-mBRTO CT images.
Paired-sample t-test was used to compare scores between CBCT images and post-mBRTO CT images. Statistical analysis was performed using SPSS software (version 15.0. SPSS, Chicago, IL, United States), with P values less than 0.05 considered to be statistically significant.
There were 7 men and 8 women with a mean age of 59 years (range, 46-86 years). All 15 patients presented with gastric variceal bleeding within one month. Three PARTO and twelve CARTO procedures were performed. Table 1 summarizes patient demographics.
| Patient demographics | |
| Male:female | 7:8 |
| Age (yr) | 59 (46-86) |
| Underlying liver disease n (%) | |
| Hepatitis C cirrhosis | 5 (33.3) |
| Alcoholic cirrhosis | 3 (20.0) |
| Non-alcoholic steatohepatitis | 3 (20.0) |
| Primary biliary cirrhosis | 2 (13.3) |
| Hepatitis B cirrhosis | 1 (6.7) |
| Cryotogenic cirrhosis | 1 (6.7) |
| Concomitant malignancy n (%) | |
| Hepatocellular carcinoma | 1 (6.7) |
| Metastatic neuroendocrine tumor | 1 (6.7) |
The CBCT images received 4.95/5.00 diagnostic scores. In all 15 patients, the necessary anatomy including the GRS, gastric varices and feeding vessels and the degree of gelfoam thrombosis within these three structures were accurately assessed. All CBCT images accurately determined the incomplete (n = 2) or complete (n = 13) obliteration of gastric varices to determine whether to continue or stop injecting gelfoam slurry. Two patients required additional gelfoam injection and repeat CBCT to confirm its completeness in obliterating the gastric varices.
No statistical difference (P = 0.164) was noted between the diagnostic score of CBCT images and post-procedure CT images in determining technical success of mBRTO evaluating complete thrombosis/obliteration of GRS and gastric varices. 100% correlation was noted between the contrast (gelfoam)-filled GRS and gastric varices seen in the CBCT images during the procedure and lack of contrast enhancement within the GRS and gastric varices seen in the post-mBRTO CT images. Both sets of images demonstrates complete filling of gelfoam slurry within the vessels which evolved into completely thrombosed vessels (Figure 2).
Successful coil or plug occlusion of efferent shunt with complete gelfoam embolization of the shunt and gastric varices was achieved in all 15 patients. A technical and clinical summary of mBRTO including the size of vascular plug, the number of coils and gelfoam packs used is shown in the Table 2.
| Technical summary of mBRTO | |
| Technical Success rate | 100% (15/15) |
| Clinical success rate | 100% (15/15) |
| Follow-up period | 684 ± 279 d |
| Major complication rate | 0% (0/15) |
| CARTO | |
| Number of coils used | 10.7 ± 3.8 |
| Diameters of coils used | 5-15 mm |
| Number of gelfoam Pack used | 5.6 ± 3.0 |
| PARTO | |
| Size of plugs used | 18 mm (3/3) |
| Number of gelfoam pack used | 9.0 ± 4.5 |
Clinical success rate was 100%. Complete thrombosis of the GRS and varices were seen in all patients as demonstrated by the intra-procedural CBCT and post-procedural follow-up CT within 2 d. All 15 patients had immediate cessation of upper GI bleeding and/or no recurrent bleeding during the follow up period (mean = 684 ± 279 d). No patients had clinical symptoms of variceal bleeding such as; hemodynamic instability, decreasing hemoglobin, hematemesis, anemia or melena.
The average follow up period was 684 ± 279 d (range 243–1134 d). Three patients had new or worsened ascites after mBRTO. No evidence of portal or splenic vein thrombosis, renal vein or caval thrombosis, renal failure or pulmonary embolization was observed. No patients showed signs of hepatic encephalopathy.
The benefits of using CBCT during various interventional procedures including transarterial chemoembolization, renal biopsy, splenic embolization and vertebroplasty have been demonstrated in several studies[1,2,21-24]. In addition, usefulness of CBCT in conventional BRTO using in-dwelling balloon and sclerosing agents has been described in several studies[5,25]. In these studies, authors concluded that CBCT can help assess the immediate progress of the procedure and potentially predict the outcome of the procedure. CBCT can provide enough information to either terminate or continue the procedure. Some of these studies have evaluated the diagnostic quality of CBCT and concluded that the CBCT images provided clinically acceptable quality images with additional information compared to 2D images including digital subtraction angiography (DSA). The additional information can help with assessing the progress of the procedure[24,26,27]. With the complexities of gastric varices and its collateral vessels seen during BRTO, it is extremely challenging to assess the complete obliteration/thrombosis of the gastric varices and its feeding vessels to determine the success of BRTO using just conventional 2D angiography or DSA.
In our study, we investigated that an intra-procedural CBCT, which provided immediate assessment of the mBRTO using plug or coils as occlusive device and gelfoam as thrombogenic agent for treatment of gastric varices. One of the main concerns for performing mBRTO is the effectiveness of gelfoam causing complete obliteration of gastric varices which can be very difficult to assess during the procedure using 2D angiography. Therefore, using CBCT can confirm the efficacy and completeness of modified BRTO following the procedure by immediately viewing completely thrombosed gastric varices, GRS and feeding vessels. By immediately assessing the mBRTO to confirm the obliteration of the varices, the procedure can be completed in one single procedure rather than proceeding into subsequent procedures if the mBRTO is not successful. By examining the efficacy of the mBRTO during the procedure while the patient is still in the angio room, the mBRTO can be confirmed as a success or be modified with more gelfoam injections or catheter adjustments, preventing the patient’s prolonged stay in the hospital if an unsuccessful mBRTO is detected later on post-procedure during follow ups.
The reported technical success rate of BRTO ranges from 78.7% to 100%[8]. We believe this technical success can be further improved using intra-procedural CBCT. In our study, intra-procedural determination of technical success of mBRTO has shown to correlate with clinical success of mBRTO, resulting in immediate cessation of gastric variceal bleeding or no recurrent bleeding in the future during follow-up. In two patients, intra-procedural CBCT showed incomplete thrombosis of gastric varices compared to the pre-procedural contrast-enhanced CT. Further gelfoam slurry injection was performed in both patients and repeat CBCT confirmed complete thrombosis of gastric varices. In all 15 patients, intra-procedural CBCT demonstrated the technical success of mBRTO. Subsequently, these 15 patients had clinical success of complete and immediate cessation of gastric variceal bleeding. All 15 patients had no recurrent bleeding during the follow up period of 421 ± 159 d.
Intra-procedural CBCT has diagnostic quality that correlates with clinical outcomes in procedures like: mBRTO, TACE and vertebroplasty. In our study, diagnostic score of intra-procedural CBCT was statistically not different compared to both pre- and post-procedural CT scores. Undoubtedly, this compatible selective diagnostic quality can make intra-procedural CBCT useful in determining the technical success and hence, clinical success. With this level of diagnostic quality, additional information can be obtained using intra-procedural CBCT such as evaluation of procedure-related complications, including portal vein thrombosis, splenic vein thrombosis and renal vein thrombosis. Once the complications are detected early, it is easier to intervene and treat them more effectively. This should be further investigated in the future studies.
Set-up time and protocol for intra-procedural CBCT is known to be time-consuming and burdensome. The intra-procedural image acquisition takes approximately 5 to 10 min; this frame includes the time required to position the patient, examination table, and C-arm in order to obtain the area of interest and to prepare the contrast media. The set-up time is often what hinders clinical use of the intra-procedural CBCT, especially when multiple (> 2) images are obtained[20]. The time for C-arm to rotate around a patient can range from 8 to 20 s depending on the particular apparatus used. Despite time constraints, intra-procedural CBCT’s 3D data set is easy to maneuver and has the ability to show the 2D oblique sections through any part of the object being imaged[20]. Given its ability to manipulate into 3D plane, C-arm CBCT has been recently used to examine tumor-feeding vessels, particularly in transcatheter arterial chemoembolization procedures, showing the potential of CBCT to recognize possible vessels that cannot be viewed on a conventional CT scan[24].
Our study had several limitations. Firstly, our study has a small sample size with potential selection bias as we included only 15 of 55 patients who received mBRTO at our institution. Secondly, as mentioned above, the intra-procedural CBCT in our study only imaged the upper abdomen, focused in GRS, gastric varices and feeding vessels. Therefore, it has no assessment of other parts of the abdomen and no assessment of the procedure-related complications. However, the post-procedural contrast-enhanced computed tomography was utilized to assess the complications, which were none. Lastly, the CBCT images were reviewed by the interventional radiologists with limited experience in assessing the CT images that may have affected the diagnostic scores and may have caused biased evaluation.
In conclusion, the intra-procedural CBCT provided immediate assessment in evaluating the technical success of mBRTO by providing a multi-planar image. This assessment seems effective in correlating and determining the clinical success of mBRTO. With our study and results from other studies, we can positively conclude that the intra-procedural CBCT may have the potential in aiding various abdominal procedures and improving both technical and clinical outcomes.
Currently, there are no angiographic protocols of evaluating the technical success of balloon-occluded retrograde transvenous obliteration (BRTO) or modified BRTO (mBRTO) during or immediately after the procedure. Traditionally, the obliterated vessels are evaluated with post-procedural computed tomography (CT); however, the intra-procedural cone-beam CT (CBCT) thus allows for immediate assessment during and immediately after the procedure to demonstrate and confirm the complete obliteration/occlusion of varices. In this study, the authors demonstrated the effectiveness of intra-procedural CBCT during mBRTO to confirm the technical success of gastric variceal embolization.
Utilization of CBCT in assessing the technical success of BRTO or mBRTO has not been fully studied and this study demonstrates the effectiveness and feasibility of using CBCT in mBRTO to improve the procedural outcomes.
Using intra-procedural CBCT in mBRTO (coil-assisted retrograde transvenous obliteration and plug-assisted retrograde transvenous oblitearation).
This study suggests that using CBCT during BRTO or mBRTO can effectively assess the success of the procedure. Therefore, this method can potentially reduce the procedure time and cost of BRTO/mBRTO.
The authors reported their own experiences in combining CBCT with BRTO in the treatment of bleeding GV. Although the sample size is small (15 patients), the content of this study is interesting, and it was well-written.
P- Reviewer: Changela K, Kim HC, Siramolpiwat S S- Editor: Gong ZM L- Editor: A E- Editor: Jiao XK
| 1. | Braak SJ, van Melick HH, Onaca MG, van Heesewijk JP, van Strijen MJ. 3D cone-beam CT guidance, a novel technique in renal biopsy--results in 41 patients with suspected renal masses. Eur Radiol. 2012;22:2547-2552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Deschamps F, Solomon SB, Thornton RH, Rao P, Hakime A, Kuoch V, de Baere T. Computed analysis of three-dimensional cone-beam computed tomography angiography for determination of tumor-feeding vessels during chemoembolization of liver tumor: a pilot study. Cardiovasc Intervent Radiol. 2010;33:1235-1242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Hirota S, Nakao N, Yamamoto S, Kobayashi K, Maeda H, Ishikura R, Miura K, Sakamoto K, Ueda K, Baba R. Cone-beam CT with flat-panel-detector digital angiography system: early experience in abdominal interventional procedures. Cardiovasc Intervent Radiol. 2006;29:1034-1038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Koizumi J, Hashimoto T, Myojin K, Fukushima T, Ichikawa T, Kagawa T, Kojima S, Watanabe N, Mine T, Nishibe T. C-arm CT-guided foam sclerotherapy for the treatment of gastric varices. J Vasc Interv Radiol. 2010;21:1583-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yamagami T, Yoshimatsu R, Miura H, Tanaka O, Yasui K, Yagi N, Yamada K. Usefulness of cone-beam computed tomography during balloon-occluded retrograde transvenous obliteration. Minim Invasive Ther Allied Technol. 2013;22:359-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Saad WE, Nicholson D, Lippert A, Wagner CC, Turba CU, Sabri SS, Davies MG, Matsumoto AH, Angle JF. Balloon-occlusion catheter rupture during balloon-occluded retrograde transvenous obliteration of gastric varices utilizing sodium tetradecyl sulfate: incidence and consequences. Vasc Endovascular Surg. 2012;46:664-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Garcia-Pagán JC, Barrufet M, Cardenas A, Escorsell A. Management of gastric varices. Clin Gastroenterol Hepatol. 2014;12:919-928.e1; quiz e51-e52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Park JK, Saab S, Kee ST, Busuttil RW, Kim HJ, Durazo F, Cho SK, Lee EW. Balloon-Occluded Retrograde Transvenous Obliteration (BRTO) for Treatment of Gastric Varices: Review and Meta-Analysis. Dig Dis Sci. 2015;60:1543-1553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 104] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 9. | Akahoshi T, Hashizume M, Tomikawa M, Kawanaka H, Yamaguchi S, Konishi K, Kinjo N, Maehara Y. Long-term results of balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding and risky gastric varices: a 10-year experience. J Gastroenterol Hepatol. 2008;23:1702-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 10. | Arai H, Abe T, Shimoda R, Takagi H, Yamada T, Mori M. Emergency balloon-occluded retrograde transvenous obliteration for gastric varices. J Gastroenterol. 2005;40:964-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Kim MY, Um SH, Baik SK, Seo YS, Park SY, Lee JI, Lee JW, Cheon GJ, Sohn JH, Kim TY. Clinical features and outcomes of gastric variceal bleeding: retrospective Korean multicenter data. Clin Mol Hepatol. 2013;19:36-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Sabri SS, Swee W, Turba UC, Saad WE, Park AW, Al-Osaimi AM, Caldwell SH, Matsumoto AH, Angle JF. Bleeding gastric varices obliteration with balloon-occluded retrograde transvenous obliteration using sodium tetradecyl sulfate foam. J Vasc Interv Radiol. 2011;22:309-316; quiz 316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Akahoshi T, Tomikawa M, Kamori M, Tsutsumi N, Nagao Y, Hashizume M, Maehara Y. Impact of balloon-occluded retrograde transvenous obliteration on management of isolated fundal gastric variceal bleeding. Hepatol Res. 2012;42:385-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Ninoi T, Nishida N, Kaminou T, Sakai Y, Kitayama T, Hamuro M, Yamada R, Nakamura K, Arakawa T, Inoue Y. Balloon-occluded retrograde transvenous obliteration of gastric varices with gastrorenal shunt: long-term follow-up in 78 patients. AJR Am J Roentgenol. 2005;184:1340-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 191] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 15. | Lee EW, Kee ST, McWilliams J, Gomes AS, Durazo F, Saab S, Goldstein L, Busuttil RW. Modified-BRTO (balloon-occluded retrograde transvenous obliteration) for the treatment of portal hypertensive variceal bleeding. J Vasc Interv Radiol. 2014;25:S8-S9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Lee EW, Saab S, Gomes AS, Busuttil R, McWilliams J, Durazo F, Han SH, Goldstein L, Tafti BA, Moriarty J. Coil-Assisted Retrograde Transvenous Obliteration (CARTO) for the Treatment of Portal Hypertensive Variceal Bleeding: Preliminary Results. Clin Transl Gastroenterol. 2014;5:e61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 17. | Park JK, Cho SK, Kee S, Lee EW. Vascular plug-assisted retrograde transvenous obliteration of portosystemic shunts for refractory hepatic encephalopathy: a case report. Case Rep Radiol. 2014;2014:391420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Cho SK, Shin SW, Lee IH, Do YS, Choo SW, Park KB, Yoo BC. Balloon-occluded retrograde transvenous obliteration of gastric varices: outcomes and complications in 49 patients. AJR Am J Roentgenol. 2007;189:W365-W372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Gwon DI, Ko GY, Yoon HK, Sung KB, Kim JH, Shin JH, Ko HK, Song HY. Gastric varices and hepatic encephalopathy: treatment with vascular plug and gelatin sponge-assisted retrograde transvenous obliteration--a primary report. Radiology. 2013;268:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Wallace MJ, Kuo MD, Glaiberman C, Binkert CA, Orth RC, Soulez G. Three-dimensional C-arm cone-beam CT: applications in the interventional suite. J Vasc Interv Radiol. 2008;19:799-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 128] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 21. | Braak SJ, Zuurmond K, Aerts HC, van Leersum M, Overtoom TT, van Heesewijk JP, van Strijen MJ. Feasibility study of needle placement in percutaneous vertebroplasty: cone-beam computed tomography guidance versus conventional fluoroscopy. Cardiovasc Intervent Radiol. 2013;36:1120-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Kapoor BS, Esparaz A, Levitin A, McLennan G, Moon E, Sands M. Nonvascular and portal vein applications of cone-beam computed tomography: current status. Tech Vasc Interv Radiol. 2013;16:150-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Kos S, Burrill J, Weir G, Salat P, Ho SG, Liu DM. Endovascular management of complex splenic aneurysm with the “amplatzer” embolic platform: application of cone-beam computed tomography. Can Assoc Radiol J. 2010;61:230-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Loffroy R, Lin M, Yenokyan G, Rao PP, Bhagat N, Noordhoek N, Radaelli A, Blijd J, Liapi E, Geschwind JF. Intraprocedural C-arm dual-phase cone-beam CT: can it be used to predict short-term response to TACE with drug-eluting beads in patients with hepatocellular carcinoma? Radiology. 2013;266:636-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 25. | Koizumi J, Hashimoto T, Myojin K, Itou C, Kagawa T, Nishibe T, Janne d’Othée B. Balloon-occluded retrograde transvenous obliteration of gastric varices: use of CT-guided foam sclerotherapy to optimize technique. AJR Am J Roentgenol. 2012;199:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Kakeda S, Korogi Y, Hatakeyama Y, Ohnari N, Oda N, Nishino K, Miyamoto W. The usefulness of three-dimensional angiography with a flat panel detector of direct conversion type in a transcatheter arterial chemoembolization procedure for hepatocellular carcinoma: initial experience. Cardiovasc Intervent Radiol. 2008;31:281-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Miyayama S, Yamashiro M, Hashimoto M, Hashimoto N, Ikuno M, Okumura K, Yoshida M, Matsui O. Comparison of local control in transcatheter arterial chemoembolization of hepatocellular carcinoma ≤ 6 cm with or without intraprocedural monitoring of the embolized area using cone-beam computed tomography. Cardiovasc Intervent Radiol. 2014;37:388-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |