INTRODUCTION
Approximately 20%-40% of patients with abdominal aortic aneurysms (AAA) can have unilateral or bilateral iliac artery aneurysms and/or ectasia[1,2]. This influences and compromises the distal sealing zone during endovascular aneurysm repair (EVAR). There are a few endovascular techniques that can be used to treat these types of aneurysms, such as intentional occlusion/over-stenting of the internal iliac artery on one or both sides to create a distal landing zone in the external iliac artery, as well as the “bell-bottom” technique. There is a paucity of data and evidence for the “snorkel and sandwich” technique, which can be useful in a few clinical scenarios[3]. The most recent endovascular technique features treatment with an iliac branch stent graft. This review discusses the currently available endovascular techniques, and it outlines the pros and cons of each method, while paying particular attention to the branch iliac stent graft.
Occlusion of the internal iliac artery
The occlusion of one or both internal iliac arteries, usually with coils and/or an Amplatz plug to create an optimal distal landing zone during EVAR, represents the longest established technique. While there is good long-term follow-up evidence regarding endoleak and the technique’s high technical success[4], this procedure can have significant negative effects on a patient’s quality of life. The major problem associated with unilateral and/or bilateral internal iliac artery occlusion is buttock claudication, which can disappear with time, but is unpredictable[5]. The available literature describes buttock claudication in 16%-55% of cases, followed by impotence in 10%-17% of cases after embolization of the internal iliac arteries[6,7]. Additionally, rare serious complications, such as spinal and bowel ischemia, may occur in up to 1%-3% of bilateral internal iliac artery occlusion cases, and gluteus necrosis may also occur[8]. There is no general consensus regarding the use of either sequential or staged embolization of both internal iliac arteries, but in a majority of centres where both internal iliac arteries should be embolized, the staged strategy is most common[9]. Proximal embolization of the internal iliac artery is strongly advised to allow for collateral circulation[10]. Generally, the intention should be to maintain the patency of at least one internal iliac artery, and factors such as the patient’s age, activity level, cardiac status, and possible future thoracic abdominal aortic interventions should be analysed throughout the treatment decision-making process.
“Bell-bottom” technique
The other endovascular technique used to treat a “hostile” distal landing zone is the bell-bottom technique. This technique is relatively simple (Figure 1) but it can be used in an iliac artery of up to 24 mm in diameter given that the largest diameter of the stent graft is 28 mm. Attention should be paid to the quality of the distal landing zone, as well as the assessment of calcification, thrombus, and the length of the distal landing zone. During long-term follow-up, the “bell-bottom” technique has shown increased frequency of the need for a secondary intervention, mainly due to the progression of artery dilatation, and also based on migration of the stent graft[11].
Figure 1 A 73-year-old patient with abdominal aortic aneurysm and bilateral common iliac artery aneurysm treated with flared limb (“Bell-Bottom” technique).
“Snorkel/chimney and sandwich/parallel” technique
The use of a parallel stent graft to maintain an open internal iliac artery was first described by Lobato. He suggests that creating an overlap between the internal iliac artery stent and external iliac artery stent of at least 5 cm can minimize possible endoleak within the gutters of both stent grafts[12]. This technique offers the potential to treat more patients when compared with other endovascular techniques. Lobato described achieving a good result with this technique; however, there is sparse literature available on this method. Transbrachial and/or axillary (unilateral or bilateral) access are necessary for placement of the stent graft. The other problems associated with the sandwich parallel stent graft include the fact that the two grafts can compress each other, increasing the risk for thrombosis, further manipulation in the aortic arch during placement of the stent graft, increasing the risk for cerebral embolization; and the stent graft is generally longer when compared with branch stent graft technology.
The snorkel or chimney technique has been primarily used to treat pararenal AAA and thoracoabdominal aneurysms in acute settings with promising initial results[13,14]. This procedure can also be used as a bailout intervention following unintentional covering of important side branch, or in the treatment of, endoleak type 1 after EVAR in selected cases[15]. The first published report of the snorkel technique was described by Greenberg et al[16] in 2003. There are various articles that describe high technical success, good mid-term follow-up, and patency of the snorkel/chimney stent graft in the treatment of thoracoabdominal aneurysms in selected patients[17]. However, problems associated with endoleak and missing long-term follow-up are still limiting factors. Furthermore, the periscope technique was developed as a modification of the snorkel technique; for this procedure, the stent graft is placed transfemorally, is distally orientated, and is used to facilitate retrograde flow through the artery. It is important to note that the majority of patients treated with the snorkel and/or periscope technique are thoracoabdominal aneurysm cases, not aortoiliac aneurysm cases, with internal iliac artery preservation.
Finally, the iliac artery’s tortuosity and problems associated with placement and force on the placed stent graft are the main constraints of this technique in the treatment of aortoiliac aneurysms. There are some other innovative treatment options, such as the crossover chimney technique, that can preserve the internal iliac artery as well[18].
BRANCH ILIAC STENT GRAFT
The newest branch stent graft technology expands upon the endovascular treatment of aortoiliac aneurysms, while maintaining and preserving the anterograde flow of important side branches. There are a few devices currently on the market (Zenith Cook, Bloomington, IN, United States; JOTEC E-iliac stent graft, JOTEC GmbH, Hechingen, Germany; and Gore Excluder iliac branch stent graft, GORE and Associates, Newark, DE, United States). The majority of the available literature features the Cook Zenith iliac branch device (IBD). There are three different IBD devices: The straight-side IBD (S-IBD) (Figure 2), the helical-side IBD (H-IBD), and the bifurcated-bifurcated IBD (BB-IBD). The difference between the S-IBD and H-IBD lies in the overlapping zone; in the first option, a balloon-expandable stent graft is used, and in H-IBD, a self-expandable stent is used given its longer overlapping zone. Furthermore, H-IBD performs better in cases of a tortuous internal iliac artery. Both stent grafts feature a 20 French (Fr) delivery system with a preloaded catheter. The preloaded catheter allows for guide wire placement, which is snared from the contralateral side and/or via brachial access, and it provides a path through which to place the bridge stent graft. The S-IBD, which is the device that is most frequently reported in the literature, is a second-generation, modular, two-branch vessel device that consists of a main iliac limb and features an additional reinforced stump for the internal iliac artery side branch. The proximal segment of the IBD has a diameter of 12 mm, and the distal segment can be 10 mm or 12 mm in diameter. The common iliac segment can be 45 mm or 61 mm in length, while the external iliac artery segment is either 41 mm or 58 mm in length. Briefly bilateral femoral artery exposure or percutaneous access is used during the intervention. The S-IBD is orientated and partially deployed above the internal iliac artery with the help of four markers. The 12 Fr sheath is placed in the contralateral femoral artery after the long guide wire is snared. Once the S-IBD is in the desired position, the side arm is exposed, and the sheath is withdrawn. The 12 Fr sheath advances from the contralateral side over the aortic bifurcation into the side branch. The 5 Fr sheath and/or diagnostic catheter are placed following puncture of the valve of the 12 Fr sheath, and selective catheterisation of the internal iliac artery is performed. Once selective catheterisation of the internal iliac artery guide wire is complete, the wire is usually exchanged for a stiffer stainless steel guide wire; when this is achieved, the stent graft is deployed in a standard manner. The main bifurcated stent graft is usually placed via the opposite site to the S-IBD. The most recent development in this treatment modality is the BB-IBD device, which represents a combination of H-IBD and the bifurcated distal component of a fenestrated device[20].
Figure 2 Zenith branch iliac stent grafts.
Straight-side iliac branch device.
Indications and anatomical constraints for using the iliac branch stent graft
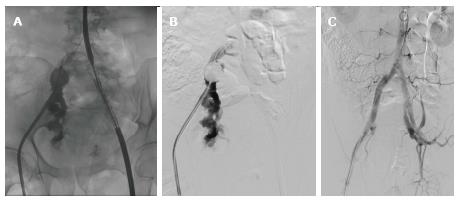
Generally, the indication for AAA treatment is a large aneurysm (> 5.5 cm in men and > 5 cm in women), and an aneurysm of the iliac artery > 3-3.5 cm (Figure 3).
Figure 3 A 68-year-old male with an abdominal aortic aneurysm and an iliac artery aneurysm.
A: Preoperative angiography; B: Control angiography after the placement of an Advanta stent graft in the left internal iliac artery without endoleak; C: Control angiography after the deployment of IBD and a bifurcated stent graft; D: Computed tomography angiography and three dimensional reconstruction at 3 mo. IBD: Iliac branch device.
To ensure that the intervention is successful, proper patient selection is very important. However, no standardised morphological criteria have been established for the use of IBD, although the following anatomical criteria must be present: (1) A length from the aortic bifurcation to the iliac bifurcation of > 50 mm (for S-IBD and H-IBD); (2) An inner iliac bifurcation diameter of at least 16 mm; (3) An internal iliac artery featuring a landing zone of at least 10 mm in the healthy segment; (4) An internal iliac artery diameter of 5-11 mm; (5) An assessment of the aortic bifurcation, iliac artery tortuosity, and stenosis, as well as calcification and thrombus in the iliac artery; and (6) A sufficient external iliac artery with a landing zone > 2 cm.
Some of the potential problems associated with these methods can be overcome with transbrachial access during deployment of the stent grafts in the internal iliac arteries.
Precise placement of a bridge stent graft is another technical issue. There are several peripheral stent grafts, such as the Advanta stent graft (Atrium Medical, Hudson, NH, United States), Fluency and Life stent grafts (Bard Peripheral Vascular Inc., Murray Hill, NJ, United States), Viabahn stent graft (Karlsruhe, Germany), and Be stent graft (Bentley InnoMed GmbH, Hechingen, Germany).
In the event that an internal iliac artery aneurysm presents itself, a stent graft may eventually be placed in one of the two side branches of the internal iliac artery; however, there could be an increased risk of endoleak[21].
Technical success and complications
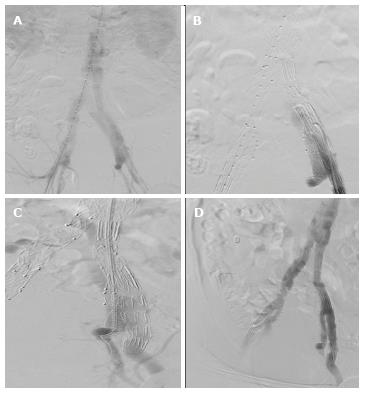
Technical success is defined as the uneventful placement of a stent graft with accompanying branch patency, and without type 1 or type 3 endoleak by the end of the intervention. As with other new techniques, a learning curve and the mastering of patient selection improve the results and technical success of this procedure, which ranges from 85%-96.3%[22-24]. In some small series, technical success is 100%[25]. The placement of a branched device is achieved through an intervention, and it is not associated with major complications; however, complications can occur - one such example includes rupture of the external iliac artery during manipulation (Figure 4). Until now, there have been no reports on the mortality rates associated with branch device implantation. Endoleak type 1 is rare and can occur in about 0.5% of patients, while endoleak type 3 occurs in 1%[26]; transbrachial access and placement of an additional stent graft usually solves this problem (Figure 5). Moreover, buttock claudication was reported in up to 4% of patients with ZBIS at 5-year follow-up[27]. Verzini et al[28] compared IBD and occlusion of the internal iliac artery, where the rate of buttock claudication in the IBD group was 4%, as compared with 22% in the iliac artery embolization group. The same research group reported endoleak type 2 in 4% of patients in the IBD group and in 19% of patients in the embolization group[29].
Figure 4 Rupture of the right external iliac artery during manipulation.
A, B: Partially deployed IBD on the left side. An occlusive balloon placed in the right common iliac artery. Angiography revealed the rupture site at the proximal part of the external iliac artery; C: Control angiography following placement of the two fluency stent grafts on the right side, and completion of the procedure with the placement of an IBD device on the left side. IBD: Iliac branch device.
Figure 5 Bilaterally placed branch stent graft.
A, B: Control angiography with endoleak type 3 on the left side; C: Transbrachial access and placement of an additional stent graft; D: Final control angiography featuring a good result and without endoleak.
Follow-up and secondary interventions
Encouraging mid- and short-term follow-up results featuring branch patency of up to 88% in a 5-6-year period were reported[27,29]. An absence of long-term results still limits the wide use of a branch stent graft, and the costs of the device play a role as well. Branch graft occlusion is a potential complication of this procedure, and it has reportedly occurred in 1.2%-11% of cases[23,27,30]; moreover, graft limb occlusion in the external iliac artery has also been reported. Branch graft occlusion is usually asymptomatic, while external iliac limb occlusion can be treated with crossover bypass and/or thrombectomy, or with the use of thrombolytic treatment.
CONCLUSION
Iliac branch stent graft placement represents a further development in endovascular medicine, and it has been associated with a high technical success rate without serious complications in the hands of an experienced professional. Very good results were obtained during short- and mid-term follow-up. Occlusion of the internal iliac artery is a rare cause of serious complications, but it can heavily impact quality of life, especially in asymptomatic patients where incidentally discovered AAA and iliac artery aneurysms require treatment. Although the costs of the stent graft can impact treatment decisions, an iliac branch stent graft should be used in selected patients as a means of maintaining patency of at least one internal iliac artery or, in some cases, bilaterally, especially in younger patients.