Published online Feb 28, 2016. doi: 10.4329/wjr.v8.i2.142
Peer-review started: August 31, 2015
First decision: September 8, 2015
Revised: October 16, 2015
Accepted: December 16, 2015
Article in press: December 18, 2015
Published online: February 28, 2016
Processing time: 182 Days and 0.1 Hours
The increased use of ionization radiation for diagnostic and therapeutic purposes, the rapid advances in computed tomography as well as the high radiation doses delivered by interventional procedures have raised serious safety and health concerns for both patients and medical staff and have necessitated the establishment of a radiation protection culture (RPC) in every Radiology Department. RPC is a newly introduced concept. The term culture describes the combination of attitudes, beliefs, practices and rules among the professionals, staff and patients regarding to radiation protection. Most of the time, the challenge is to improve rather than to build a RPC. The establishment of a RPC requires continuing education of the staff and professional, effective communication among stakeholders of all levels and implementation of quality assurance programs. The RPC creation is being driven from the highest level. Leadership, professionals and associate societies are recognized to play a vital role in the embedding and promotion of RPC in a Medical Unit. The establishment of a RPC enables the reduction of the radiation dose, enhances radiation risk awareness, minimizes unsafe practices, and improves the quality of a radiation protection program. The purpose of this review paper is to describe the role and highlight the importance of establishing a strong RPC in Radiology Departments with an emphasis on promoting RPC in the Interventional Radiology environment.
Core tip: Radiation protection culture (RPC) is a combination of knowledge, beliefs and practices related to radiation safety. The establishment of a RPC in a Radiology Department demands substantial knowledge of radiation risks, safety rules and active participation of all stakeholders. Professionals have the key role in the creation of a RPC. A strong RPC provides more effective diagnosis and treatment, improves patient and staff safety and reduces radiation exposure. The objective of our study is to highlight the role of RPC in a Radiology Department with an emphasis on promoting RPC in the Interventional Radiology environment.
- Citation: Ploussi A, Efstathopoulos EP. Importance of establishing radiation protection culture in Radiology Department. World J Radiol 2016; 8(2): 142-147
- URL: https://www.wjgnet.com/1949-8470/full/v8/i2/142.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i2.142
Culture is one of the most complicated and obscure concepts. Among the many definitions one may find in the literature, the most attractive one for the purpose of this text is that culture is “…the total range of activities and ideas of a group of people with shared traditions, which are transmitted and reinforced by members of the group…”[1]. The term culture is not only associated with a high level of art, civilization and religion but also strongly affects business, communication, marketing and safety.
During the recent years the concept of safety culture has been gaining ground in organizations mainly due to the rapid advancement of technology and the concern about employees’ health and safety. Safety culture reflects attitudes, values, norms and practices that professional and employees share concerning risk and safety. Safety culture is often used in conjunction with terms like “nuclear safety culture”, “patient safety culture”, “health safety culture”, “occupational safety culture”, “organization safety culture” and “environment safety culture”.
Regarding the safe use of ionizing radiation in the medical field and nuclear industry, International Radiation Protection Association (IRPA) first established the concept of radiation protection culture (RPC) in 2008 following the proposal of the French Society for Radiation Protection. The proposal was favourably greeted by the participating Associate Societies, the World Health Organisation (WHO) and the European ALARA Network. At the first Workshop of IRPA on RPC in 2009, professionals proposed a number of definitions for RPC and prepared the action plan for the development of a strong RPC. Two years later, after a series of meetings, the Association published the final draft on Guiding Principles for Establishing a RPC and very recently, in June 2014, the draft was issued in its final form and published in the website of IRPA[2].
Hence, the RPC is a newly introduced concept for professionals, staff and patients. The goal of this paper is to provide the role of RPC with an emphasis on promoting RPC in the Interventional Radiology environment.
A thorough understanding of the term RPC is the first step towards developing a strong RPC in a Radiology Department. According to IRPA, RPC is defined as “The combination of knowledge, values, behaviours and experience of radiation protection in all its aspects for patients, workers, population and environment, and in all exposure situations, combining scientific and social dimensions”[2]. In other words, RPC is the assembly of attitudes, strategies and practices among staff and leaders that should be emphasized in radiation protection safety. As it is obvious, RPC is a part of safety culture oriented on the effects and risks of ionization radiation.
Each Radiology Department has guidelines and practical rules for the safe use of ionizing radiation even if not all members of the department are aware of that. Does this actual mean that every Radiology Department has a RPC program? On this question, opinions diverge. Some support that RPC exists in every Radiology Department; however this culture can be positive or negative, strong or weak. Others recognize that culture is a combination of attitudes and regulations and claim that RPC is either present or absent within a Radiology Department. In authors’ opinion, RPC exists in most Radiology Departments. The challenge is to improve rather than to build a RPC. Most often, it proves to be more difficult to improve an existing culture rather than to create a new one as workers and all stakeholders must unlearn the old behaviors and practices before they adopt the new ones.
The objectives of RPC are to provide a safe working environment, promote knowledge of radiation risks, minimize unsafe practices, control radiation risks, share responsibility among workers and improve the quality of an already existing radiation protection program. All the aforementioned objectives are achieved through the active participation and interaction of all the workers inside the department.
The increasing use of ionization radiation for diagnostic and therapeutic purposes especially in higher dose procedures such as computed tomography (CT) and interventional radiology have raised serious safety and health concerns for both patients and medical staff.
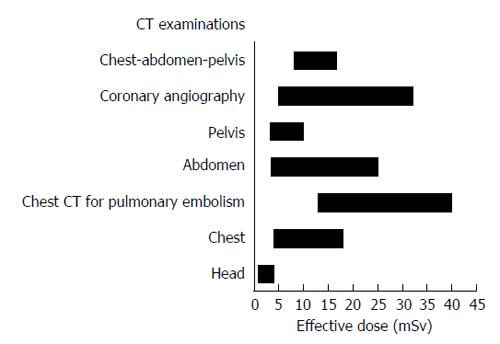
During the last 15-year period the number of CT examinations has almost tripled and now contribute to more than 60% of the total collective dose from X-ray examinations[3,4]. A typical head CT scan, which is the most frequent CT examination in adults and children, delivers an effective dose of about 4 mSv whereas the effective doses for abdomen and coronary angiography CT examinations can reach 25 and 32 mSv, respectively (Figure 1)[5,6].
The concern for the increased use of CT exams is more pronounced for pediatric patients. A recent survey revealed that the frequency of CT examinations has doubled in children under 5 years old while it has tripled in older children the last 20 years[7]. Pediatric patients are more sensitive to radiation-induced risks compared to adults due to their longer post-exposure life expectancy and their rapidly dividing cells. Two recent epidemiological studies on large pediatric populations demonstrated positive association between radiation exposures received from CT scans and cancer incidence[8,9]. It is worth mentioning that even today there is lack of optimized, size-based protocols for pediatric procedures in clinical routine and therefore children may be over-exposed to radiation.
Concerning the field of interventional radiology (IR), the new advances in fluoroscopy imaging equipment as well as the development of new interventional tools and devices (balloon, catheters, stents) led to a significant increase of 78% in interventional (non-CT) procedures the period between 1998-2008[3].
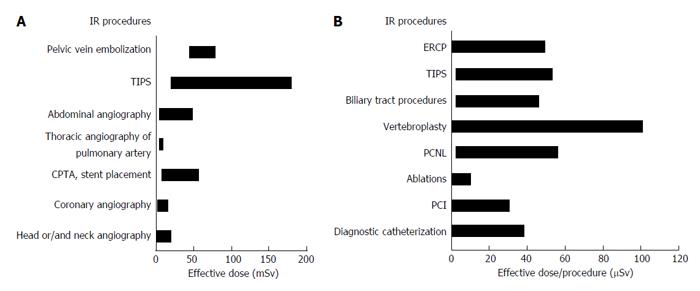
Radiation protection and safety is an extremely important issue for IR medical staff. IR procedures are usually complex, demands high fluoroscopy times, high dose rates and a large number of cine acquisitions. Therefore, they deliver high radiation doses both to patients and medical staff. Figure 2 presents the effective dose from various IR examinations for patients and medical staff[5,10,11]. IR procedures deliver effective dose to the patients ranging from 5 to 160 mSv[5] and contribute about 8% to collective dose[3] even though they consist of a small percentage in the total number of X-ray examinations performed in a given population. Variations in the value of occupational doses for the same type of procedure are largely due variations in the X-ray equipment, the technique, the training of health professionals on radiation protection issues, the optimization of protocols as well as to the availability and use of protection tools.
There are several reports in the literature concerning radiation-induced deterministic effects on both patients and medical staff during IR procedures[12,13]. The most common deterministic effects in patients are erythema, skin necrosis, hair loss and permanent epilation as well as cataract formation in occupational settings. Most of the time, the deterministic injuries arise from the poor knowledge on radiation protection rules, the lack of quality assurance programs, the performance of wrong practices and the improper or no use of radiation protection tools.
The key role for the implementation of RPC in a Radiology Department is initially the development of a strategic plan where every decision and process takes into account radiation safety of staff and patients. Then this strategic plan must be turned into an action plan in order to create the conditions for the incorporation of radiation safety in the routine work of the department. But how we can achieve the establishment of a RPC program in Radiology Departments and how easy is it to apply a “culture” on a daily basis?
The most important factor contributing to the creation of a RPC is the continuous education and training of the staff and professionals with the attendance of courses, workshops, seminars and electronic-learning programs in a normal periodical basis. Theoretical education and practical training in radiation protection aim to ensure that healthcare professionals will obtain a strong foundation in radiation protection and a basic knowledge of the technology of each modality. Education is an essential aspect for the optimization of clinical protocols and the reduction of radiation exposure. Physicians, radiographers, nurses and other medical staff need to have a substantial knowledge of radiation protection regulations and a comprehensive understanding of the factors that affect patient and occupational dose in order to minimize the harmful effects of ionizing radiation. Medical staff should be adequately trained in order to keep the dose as low as reasonably achievable (ALARA principle), be familiar with radiation quantity units, pay special attention to radiation protection of pregnant and pediatric patients and proper use of the radiation protection equipment.
Literature review revealed that there is poor education in radiation protection of medical staff. A study from Salerno et al[14] on the evaluation of radiation risks knowledge in pediatric fellows and resident demonstrated that only 35% of medical staff have sufficient knowledge for radiation risk from common radiological examinations. Furthermore, it is impressive to be noted that a multicenter study conducted by Vano et al[15] in pediatric interventional cardiology departments in Latin America revealed that only 64% of the physicians used their personnel dosimeter and only 36% were aware of the doses received. European Commission[16] and more recently the International Commission of Radiation Protection[17] published guidelines highlighting the need for education and training of medical staff on radiation protection. It is important to understand that education does not only offer new knowledge but also facilitates the development of new skills and attitudes.
The active stakeholder engagement of all levels including health authorities, researchers, medical staff and patients is the second milestone for the establishment of a RPC. In a Radiology Department, multi-disciplinary collaboration is needed. Radiologists, medical physicists, radiographers, nurses and other specialists must collaborate closely one to each other, in order to ensure patient safety and best clinical outcome. RPC is strongly dependent on the behavior of all stakeholders. The effective communication among workers leads to the creation of a supportive and motivating work environment where everyone has a clear role. A positive workplace is characterized by trust and respect among stakeholders and allows the exchange of experience and knowledge. A strong leadership increases the radiation risk awareness and allows the performance of safer practices, which prompts minimizing errors.
Quality assurance (QA) program is another essential step in the implementation of RPC. According to WHO, the QA program in diagnostic radiology is defined as “an organized effort by the staff operating a facility to ensure that the diagnostic images produced are of sufficiently high quality so that they consistently provide adequate diagnostic information at the lowest possible cost and with the least possible exposure of the patient to radiation’’[18]. The objectives of a QA program is to improve patient care and comfort, ensure accurate diagnosis and proper function of the equipment, produce high quality images following the ALARA principle, ensure patient and staff safety and minimize cost. A QA program should include the following major elements[19,20]: (1) Responsibility: There should be an assignment of the responsibility with specific duties for the performance of QA procedures. Both managers and employee are responsible for the implementation and improvement of QA programs in clinical routine; (2) Equipment specifications: Accurate specifications must be provided for each modality according to the facilities needs; (3) Standards for image quality: Standards, criteria and limits for diagnostic acceptable images should be documented and accessible; (4) Monitoring and maintenance: Monitoring, testing and maintenance of radiology equipment should be established and performed on a regular basis; (5) Evaluation: There must be regularly recurring evaluation of the adequacy and effectiveness of the X-ray equipment performance and the QA program itself; (6) Records: Every department should keep records about the equipment, quality control tests, dosimetry data, maintenance and repair of the modalities. The records must be easily accessible to the staff; (7) Manual: The manual must include list of duties and responsibilities of the staff as well as a list of the tests to be performed; (8) Education: QA specialists shall have continuing education and training in order to be qualified and up-to-date; (9) Committee: Each department should establish a committee composed of radiologists, medical physicists and radiographers with the top priority being the QA and the radiation safety; and (10) Review: Ongoing review of the QA program is important in order to assess the effectiveness of the QA procedures.
The implementation of a RPC should be driven from the highest level. Managers, medical professionals and workers should be directly involved and have a key role in the execution of RPC in every department. Radiation protection experts enhance safety culture, provide leadership, develop relationships with the administration and the employees and are responsible for the staff training and the creation of guidelines and recommendations under the guidance of radiation protection associates (e.g., IRPA). Managers should be able to change unsafe practices and behavioral hazards, recognize safe practices and report accidents in order to prevent recurrence. Furthermore, the healthcare staff should implement the guidelines and the recommendations, ensure the proper practice of examinations, improve patient health care and build trust between patients and staff.
The direct impact of the implementation of RPC is the substantial reduction of radiation dose on both patients and staff. Fetterly et al[21] showed a significant reduction of about 40% on cumulative skin dose of patients in an invasive cardiovascular laboratory after the establishment of a safety culture. The ways in which the safety culture was achieved included a number of practical and technical changes such as reporting of high air-kerma procedures, training for fellows on radiation exposure safety issues, maximum distance between the X-ray source and patient, increased use of X-ray beam spectral filters and reduced fluoroscopy frame rates. A strong RPC enables more efficient diagnosis and treatment and helps minimize harmful effects. The foundation of a RPC program has an important effect on the operation of the Radiology Department: It improves the efficiency and service quality, reduces cost and incorrect practices and promotes a good reputation.
RPC is a combination of attitudes, priorities, policies and practices concerning radiation safety. The foundation of a RPC program is a dynamic process that needs continuous evaluation and systematic improvement with the use of quantitative and qualitative tools in order to examine how well the RPC is being implemented and to check whether the program is achieving the desired goals. RPC should be an integral part of clinical routine and demands deep knowledge of radiation risks, safety rules and active participation of all stakeholders. Insufficient knowledge and lack of collaboration are the most significant barriers in the implementation of RPC. For the successful establishment of a strong RPC program, authorities, professionals, employee and patients must fully comprehend the role and the impact of RPC in a Radiology Department and fill the gap between theory and practice.
P- Reviewer: Chow J, Faasse T, Landrigan-Ossar M S- Editor: Kong JX L- Editor: A E- Editor: Liu SQ
| 1. | Hanks P. Collins Dictionary of the England Language. 1st ed. Glasgow: William Collins Sons and Co 2004; 407. |
| 2. | Available from: http://www.irpa.net/members/IRPA-Guiding%20Principles%20on%20RP%20Culture%20-2014%20.pdf. |
| 3. | Hart D, Wall , BF , Hillier MC, Shrimpton PC. Frequency and collective dose for medical and dental X-ray examinations in the UK, 2008. Chilton: Health Protection Agency 2010; HPA-CRCE-012. |
| 4. | Smith-Bindman R, Miglioretti DL, Johnson E, Lee C, Feigelson HS, Flynn M, Greenlee RT, Kruger RL, Hornbrook MC, Roblin D. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA. 2012;307:2400-2409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 599] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 5. | Mettler FA, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1427] [Cited by in RCA: 1364] [Article Influence: 80.2] [Reference Citation Analysis (0)] |
| 6. | Dougeni E, Faulkner K, Panayiotakis G. A review of patient dose and optimisation methods in adult and paediatric CT scanning. Eur J Radiol. 2012;81:e665-e683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 116] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 7. | Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167:700-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1033] [Cited by in RCA: 1029] [Article Influence: 85.8] [Reference Citation Analysis (0)] |
| 8. | Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2528] [Cited by in RCA: 2636] [Article Influence: 202.8] [Reference Citation Analysis (1)] |
| 9. | Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, Giles GG, Wallace AB, Anderson PR, Guiver TA. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1349] [Cited by in RCA: 1393] [Article Influence: 116.1] [Reference Citation Analysis (0)] |
| 10. | Kim KP, Miller DL, Balter S, Kleinerman RA, Linet MS, Kwon D, Simon SL. Occupational radiation doses to operators performing cardiac catheterization procedures. Health Phys. 2008;94:211-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 204] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 11. | Kim KP, Miller DL, Berrington de Gonzalez A, Balter S, Kleinerman RA, Ostroumova E, Simon SL, Linet MS. Occupational radiation doses to operators performing fluoroscopically-guided procedures. Health Phys. 2012;103:80-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 12. | Balter S, Hopewell JW, Miller DL, Wagner LK, Zelefsky MJ. Fluoroscopically guided interventional procedures: a review of radiation effects on patients’ skin and hair. Radiology. 2010;254:326-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 407] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 13. | Sun Z, AbAziz A, Yusof AK. Radiation-induced noncancer risks in interventional cardiology: optimisation of procedures and staff and patient dose reduction. Biomed Res Int. 2013;2013:976962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Salerno S, Marchese P, Magistrelli A, Tomà P, Matranga D, Midiri M, Ugazio AG, Corsello G. Radiation risks knowledge in resident and fellow in paediatrics: a questionnaire survey. Ital J Pediatr. 2015;41:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Vano E, Ubeda C, Miranda P, Leyton F, Durán A, Nader A. Radiation protection in pediatric interventional cardiology: An IAEA PILOT program in Latin America. Health Phys. 2011;101:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | European Commission. Guidelines on Radiation Protection Education and Training of Medical Professionals in the European Union (RP 175). Luxembourg: Publications Office of the European Union 2014; . |
| 17. | Vañó E, Rosenstein M, Liniecki J, Rehani MM, Martin CJ, Vetter RJ. ICRP Publication 113. Education and training in radiological protection for diagnostic and interventional procedures. Ann ICRP. 2009;39:7-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | World Health Organization. Quality Assurance in Diagnostic Radiology. Geneva: Macmillan Procrom 1982; . |
| 19. | Inkoom S, Schandorf C, Emi-Reynolds G, Fletcher JJ. Quality Assurance and Quality Control of Equipment in Diagnostic Radiology Practice - The Ghanaian Experience. Available from: http://cdn.intechopen.com/pdfs-wm/23741.pdf. |
| 20. | Available from: http://www.ecfr.gov/cgi-bin/text-idx?SID=3ee286332416f26a91d9e6d786a604ab&mc=true&tpl=/ecfrbrowse/Title21/21tab_02.tpl. |
| 21. | Fetterly KA, Mathew V, Lennon R, Bell MR, Holmes DR, Rihal CS. Radiation dose reduction in the invasive cardiovascular laboratory: implementing a culture and philosophy of radiation safety. JACC Cardiovasc Interv. 2012;5:866-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |