Peer-review started: June 19, 2014
First decision: July 10, 2014
Revised: February 17, 2015
Accepted: March 16, 2015
Article in press: March 18, 2015
Published online: April 28, 2015
Processing time: 307 Days and 23 Hours
AIM: To compare diagnostic sensitivity, specificity and accuracy of magnetic resonance cholangiopancreatography (MRCP) without contrast medium and endoscopic ultrasound (EUS)/endoscopic retrograde cholangiopancreatography (ERCP) for biliary calculi.
METHODS: From January 2012 to December 2013, two-hundred-sixty-three patients underwent MRCP at our institution, all MRCP procedure were performed with the same machinery. In two-hundred MRCP was done for pure hepatobiliary symptoms and these patients are the subjects of this study. Among these two-hundred patients, one-hundred-eleven (55.5%) underwent ERCP after MRCP. The retrospective study design consisted in the systematic revision of all images from MRCP and EUS/ERCP performed by two radiologist with a long experience in biliary imaging, an experienced endoscopist and a senior consultant in Hepatobiliopancreatic surgery. A false positive was defined an MRCP showing calculi with no findings at EUS/ERCP; a true positive was defined as a concordance between MRCP and EUS/ERCP findings; a false negative was defined as the absence of images suggesting calculi at MRCP with calculi localization/extraction at EUS/ERCP and a true negative was defined as a patient with no calculi at MRCP ad at least 6 mo of asymptomatic follow-up. Biliary tree dilatation was defined as a common bile duct diameter larger than 6 mm in a patient who had an in situ gallbladder. A third blinded radiologist who examined the MRCP and ERCP data reviewed misdiagnosed cases. Once obtained overall data on sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) we divided patients in two groups composed of those having concordant MRCP and EUS/ERCP (Group A, 72 patients) and those having discordant MRCP and EUS/ERCP (Group B, 20 patients). Dataset comparisons had been made by the Student’s t-test and χ2 when appropriate.
RESULTS: Two-hundred patients (91 men, 109 women, mean age 67.6 years, and range 25-98 years) underwent MRCP. All patients attended regular follow-up for at least 6 mo. Morbidity and mortality related to MRCP were null. MRCP was the only exam performed in 89 patients because it did show only calculi into the gallbladder with no signs of the presence of calculi into the bile duct and symptoms resolved within a few days or after colecistectomy. The patients remained asymptomatic for at least 6 mo, and we assumed they were true negatives. One hundred eleven (53 men, 58 women, mean age 69 years, range 25-98 years) underwent ERCP following MRCP. We did not find any difference between the two groups in terms of race, age, and sex. The overall median interval between MRCP and ERCP was 9 d. In detecting biliary stones MRCP Sensitivity was 77.4%, Specificity 100% and Accuracy 80.5% with a PPV of 100% and NPV of 85%; EUS showed 95% sensitivity, 100% specificity, 95.5% accuracy with 100% PPV and 57.1% NPV. The association of EUS with ERCP performed at 100% in all the evaluated parameters. When comparing the two groups, we did not find any statistically significant difference regarding age, sex, and race. Similarly, we did not find any differences regarding the number of extracted stones: 116 stones in Group A (median 2, range 1 to 9) and 27 in Group B (median 2, range 1 to 4). When we compared the size of the extracted stones we found that the patients in Group B had significantly smaller stones: 14.16 ± 8.11 mm in Group A and 5.15 ± 2.09 mm in Group B; 95% confidence interval = 5.89-12.13, standard error = 1.577; P < 0.05. We also found that in Group B there was a significantly higher incidence of stones smaller than 5 mm: 36 in Group A and 18 in Group B, P < 0.05.
CONCLUSION: Major finding of the present study is that choledocholithiasis is still under-diagnosed in MRCP. Smaller stones (< 5 mm diameter) are hardly visualized on MRCP.
Core tip: The present paper is the report on a series of patients evaluated for biliary disease. Particularly the study is focused on performance of magnetic resonance cholangiopancreatography performance as the upfront examination tool for this group of diseases as compared to endoscopic ultrasounds and endoscopic retrograde cholangiopancreatography. Furthermore we did an extensive revision of the worldwide literature on the issue and discuss results of the review comparing them to our own.
- Citation: Polistina FA, Frego M, Bisello M, Manzi E, Vardanega A, Perin B. Accuracy of magnetic resonance cholangiography compared to operative endoscopy in detecting biliary stones, a single center experience and review of literature. World J Radiol 2015; 7(4): 70-78
- URL: https://www.wjgnet.com/1949-8470/full/v7/i4/70.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i4.70
Despite continuing technological progress and the increasing availability of imaging tests, such as endoscopic ultrasound (EUS), computed tomography (CT), and magnetic resonance imaging (MRI), accurately detecting hepatobiliary and pancreatic diseases remains a challenge for clinicians and radiologists.
Magnetic resonance cholangiopancreatography (MRCP) is the most accurate, noninvasive imaging study for the hepatobiliary system[1-3]. However, endoscopic retrograde cholangiopancreatography (ERCP) combined with EUS is the gold standard for evaluating hepatobiliary and pancreatic ducts morphology, moreover it allows many therapeutic interventions that carry a greater morbidity and mortality[4-7].
The advantages of MRCP include the lack of invasiveness, ionizing radiation, and/or contrast media in the biliary and pancreatic ducts and general feasibility with no need for anesthesia. Furthermore, MRCP helps detect clinical relevant extrabiliary ductal diseases, which may also be responsible for a patient’s symptoms[3].
Several studies have compared MRCP and ERCP, and most suggested patients should be examined with ERCP without prior MRCP when laboratory values or other imaging studies strongly suggest an abnormal hepatobiliary process such as a stone, stricture, or obstruction[8,9]. However, for patients who complain of right upper quadrant abdominal pain, without laboratory values or imaging studies that suggest an obstructive hepatobiliary or pancreatic process, many studies suggest using MRCP to determine whether ERCP is necessary in order to avoid useless morbidity[1-11].
We retrospectively reviewed the medical records of patients evaluated for cholestasis and/or right upper quadrant abdominal pain without imaging studies that suggested overt biliary obstruction. We assumed ERCP was the gold standard (100% sensitivity and specificity in the hands of an experienced provider). We studied MRCP for sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) in diagnosing choledocholithiasis and stricture of the hepatobiliary system.
The aim of the study was to obtain data for MRCP and EUS/ERCP related to outcome in patients evaluated for cholestasis and/or right upper quadrant abdominal pain without images indicating biliary obstruction.
From January 2012 to December 2013, two-hundred-sixty-three patients underwent MRCP at our institution. In two-hundred MRCP was done for pure hepatobiliary symptoms and these patients are the subjects of this study. Among these two-hundred patients, one-hundred-eleven (55.5%) underwent ERCP after MRCP. All MRCP images were retrospectively reviewed from three experienced radiologists in the field of hepatobiliary diseases. EUS/ERCP procedures were all conducted by experienced endoscopist. Data from both MRCP and EUS/ERCP were finally reviewed and compared by the radiologists, the endoscopist and an experienced hepatobiliary surgeon. We retrospectively reviewed all clinical records and images of these latter patients. Bile duct dilatation was defined as choledocus larger than 6 mm in a patient whose gallbladder was in situ. Gamma glutamyl transpeptidase was considered changed at a twofold normal value (0-31 mg/dL).
Patient consent for processing of personal data was acquired according to our institution’s protocol.
All scans were performed on a 1.5 Tesla Magnetic Resonance (Intera 1.5 T Pulsar; Philips, Amsterdam, the Nederlands) according to our institutional standardized MRCP protocol. All patients were examined in the supine position. A channel-phased array body coil was used. Before the scan, pineapple juice, a negative oral contrast agent, was taken orally by all patients[12]. The scans were performed as follows: The first scan was T2/TSE/HR: TR 3024, TE 115 Flip Angle 90° slices thickness 7 mm. The second scan was T1/Proset GR FFE: TR 230, TE4.6 Flip Angle 85° slices thickness 7 mm. The third scan was MRCP/3D/HR triggered: TR1800, TE650 Flip Angle 90° slices thickness 1 mm. The fourth scan was MRCP/MS breath hold: TR8000, TE800, Flip Angle 90° slice thickness 40 mm with MIP retro-reconstruction. No drug administration or contrast medium was required.
The indications for ERCP were persistent cholestasis and right upper quadrant abdominal pain, with a positive MRCP for stones or stricture, independent of bile duct dilatation. Written informed consent was obtained from all patients before the procedures were performed. Combined EUS and ERCP were performed under sedation using intravenous Propofol and Ramifentanyl. EUS was performed with a radial echoendoscope (GF-UE 160; Olympus Medical Systems Co., Tokyo, Japan). Subsequent ERCP-related procedures were performed following EUS during the same session using a duodenoscope (JF-Q-180W; Olympus Medical Systems Co.). Papillotomies were performed with either a Cook-DASH-1 or a Cook DASH-21 Papillotome (Cook Medical, Limerick, Ireland). Biliary cannulation was done using a guide wire (Cook MET-35-480 coupled to the Dash-1Ppapillotome and Cook MET II21-480 coupled to the DASH-21 Papillotome; Cook Medical). Calculi were extracted with either a Dormia Basket (Memory Soft Wire Basket: MSB 1.5 × 3.5 G22136; MSB 2.5 × 5 G22019; MSB 2 × 4 G21525; MSB 3 × 6 - 6 G 21913 (six wires); MSB 2 × 4 - 6 G21544 (six wires); Cook Medical) or an extraction balloon (Cook TXR-8.5-12-15-A; Cook Medical).
All MRCP and ERCP images were retrospectively reviewed by two radiologists who had experience in hepatobiliary diseases. Previous reports were re-examined paying attention to choledocholithiasis, strictures, extra luminal compressions, and dilatation. Hepatobiliary and pancreatic tree obstruction was defined as any obstruction in the system secondary to a mass, stone, or stricture. Biliary tree dilatation was defined as a common bile duct diameter larger than 6 mm in a patient who had an in situ gallbladder. A third blinded radiologist who examined the MRCP and ERCP data reviewed misdiagnosed cases.
Dataset comparisons had been made by the Student’s t-test and χ2 when appropriate. An independent biostatistician reviewed the whole dataset and approved it.
All the data were blinded reviewed by an indepen dent biostatician.
From January 2012 to December 2013, we evaluated 263 patients with confirmed colelithiasis and symptoms suggesting the presence of stones in the biliary tract. Table 1 shows the criteria we used for first evaluation of patient to be addressed towards further examination. Patients showing a low risk were addressed to MRCP, patients showing high risk were addressed to upfront EUS/ERCP. Moreover, patients showing signs of cancer at ultrasound (US) and/or CT scan were excluded from the study. Two-hundred patients (91 men, 109 women, mean age 67.6 years, and range 25-98 years) underwent MRCP. All patients attended regular follow-up for at least 6 mo. Morbidity and mortality related to MRCP were null. MRCP was the only exam performed in 89 patients because it did show only calculi into the gallbladder with no signs of the presence of calculi into the bile duct and symptoms resolved within a few days or after colecistectomy. The patients remained asymptomatic for at least 6 mo, and we assumed they were true negatives.
| Age > 55 yr |
| Evidence/suspicion of calculi at US |
| Choledocus larger than 6 mm at US (in patients having gallbladder) |
| Conjugated bilirubin higher than 51 micromoles/L |
| Persistence of cholestasis 72 h after the acute episode |
| All criteria present: Biliary tree lithiasis probability > 90% |
| All but one criteria: Biliary tree lithiasis probability about 20% |
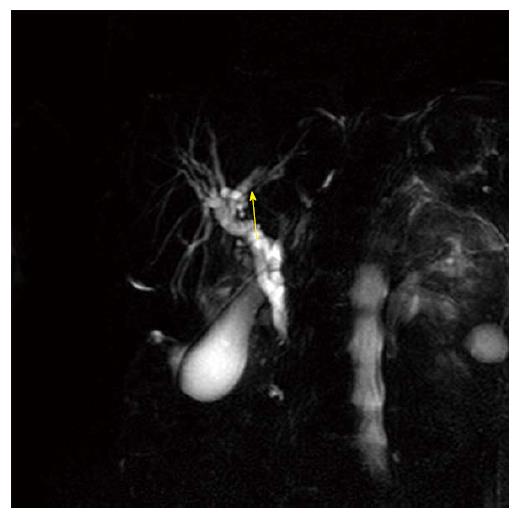
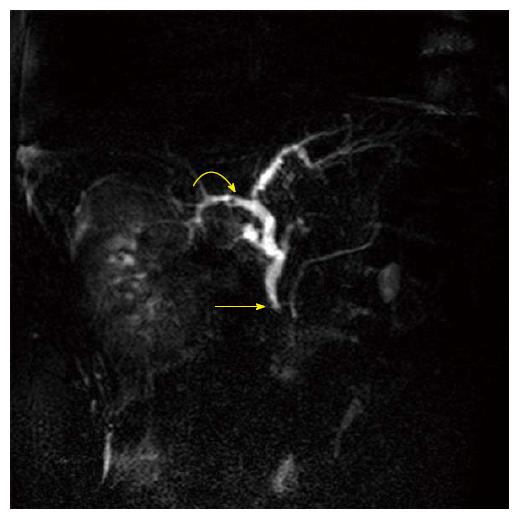
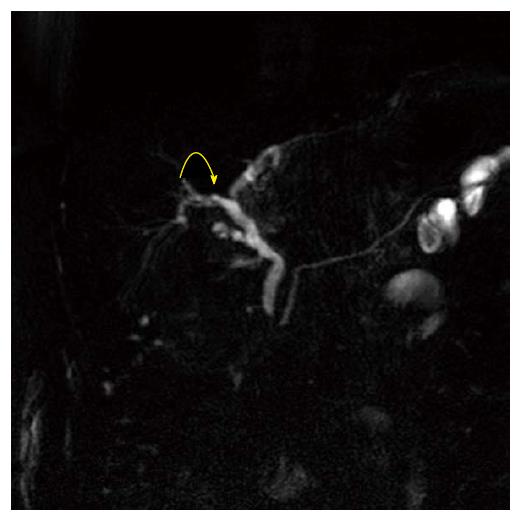
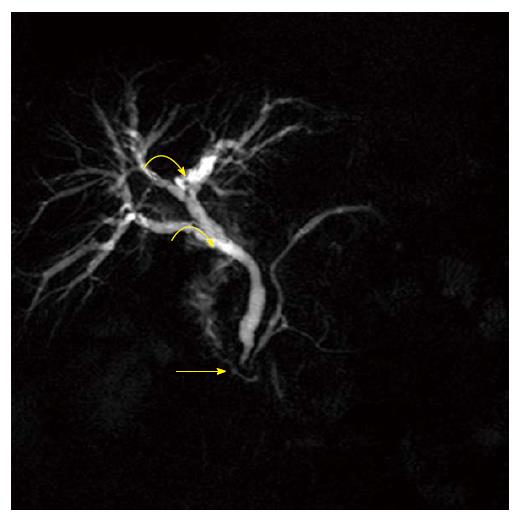
Seventy-two patients with calculi into the biliary tree diagnosed at MRCP (Figures 1-3) were scheduled to receive EUS/ERCP within no more than 1 wk as well as patients who showed persistence or recurrence of symptoms even with a negative MRCP scan. Furthermore, patients who showed recurrence of symptoms at some point during follow-up were also provided EUS/MRC even if they had an MRCP scan reported as non-diagnostic exam. One hundred eleven (53 men, 58 women, mean age 69 years, range 25-98 years) underwent ERCP following MRCP. We did not find any difference between the two groups in terms of race, age, and sex. The overall median interval between MRCP and ERCP was 9 d.
One hundred eight patients (97.3%) underwent a therapeutic intervention during ERCP such as stone/sludge extraction, stricture dilatation, or papillotomy. The median number of extracted stones was 2.6 (mean 2.4, range 1-12). The extracted stones had a median diameter of 7.8 mm (mean 8.1, range 2-36). ERCP-related complications included 3 acute cases of pancreatitis, in 1 case severe requiring surgical debridement; 1 duodenal microperforation resolved conservatively within 1 wk, and 4 patients bled from the papillotomy that in 2 cases required endoscopic hemostasis. Perioperative mortality was 0.9% (1 patient died of myocardial infarction during the procedure).
MRCP diagnosis of biliary stone was correct in 72 patients confirmed and removed with EUS/ERCP with 100% concordance between the two methods, no false positives were reported at MRCP.
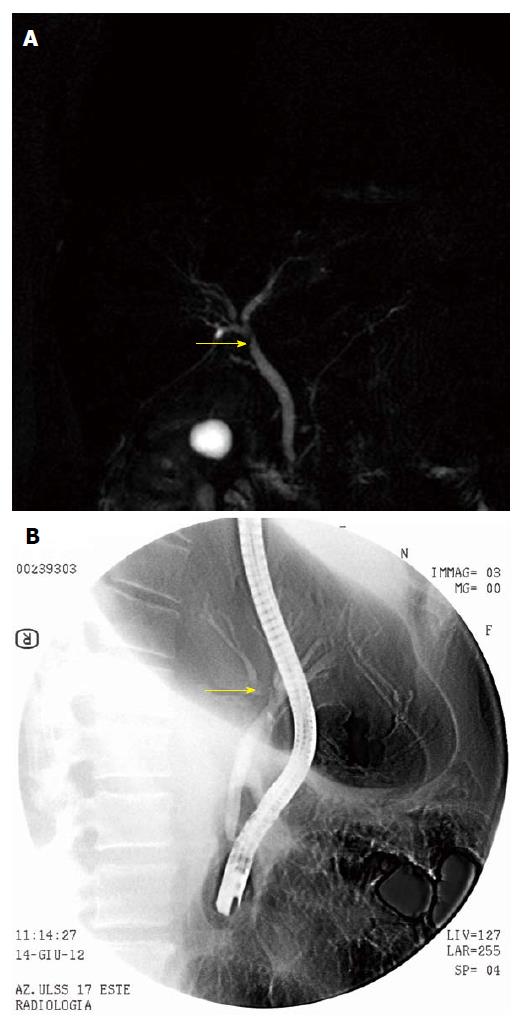
In 21 cases, MRCP did not show the presence of calculi. In 9 of these cases, radiologic diagnosis was biliary stricture (Figure 4), in 2 cases MRCP was negative, and in 10 cases only microlithiasis of the gallbladder was diagnosed. All 21 patients underwent EUS/ERCP, in 9 cases due to the MRCP diagnosis of biliary stricture (Figure 5), in 3 cases for persistent cholestasis, and in the latter 9 for recurrence of symptoms during follow-up. Among these cases, 16 were found at EUS to have biliary microstones or sludge that was removed by ERCP during the same procedure, in 6 cases EUS did not show stones but after papillotomy and choledocus exploration microcalculi or sludge were extracted. In 1 case, even EUS and ERCP did not show any significant biliary disease, and the patient was diagnosed with sclerosing cholangitis. In 2 cases, the ERCP confirmed the associated presence of a choledocal stenosis. At this point, we divided patients into two groups. The first group (Group A) consisted of 72 patients who had concordant MRCP and EUS/ERCP (44 women and 28 men, median age 67 years, range 29-81); the second group consisted of 20 patients who had discordant MRCP and EUS/ERCP (14 women and 7 men, median age 59 years, range 25-98).
When we compared the two groups, we did not find any statistically significant difference regarding age, sex, and race. Similarly, we did not find any differences regarding the number of extracted stones: 116 stones in Group A (median 2, range 1 to 9) and 27 in Group B (median 2, range 1 to 4). When we compared the size of the extracted stones we found that the patients in Group B had significantly smaller stones: 14.16 ± 8.11 mm in Group A and 5.15 ± 2.09 mm in Group B; 95% confidence interval = 5.89-12.13, standard error = 1.577; P < 0.05. We also found that in Group B there was a significantly higher incidence of stones smaller than 5 mm: 36 in Group A and 18 in Group B, P < 0.05. MRCP also diagnosed 35 biliary strictures, 9 of which on EUS/ERCP were revealed to be microstones; therefore, we correctly diagnosed 26 biliary strictures on MRCP, and conversely, all the ERCP confirmed biliary stenoses were previously correctly defined by MRCP. In detecting biliary stones MRCP sensitivity was 77.4%, Specificity 100% and accuracy 80.5% with a PPV of 100% and NPV of 85%; EUS showed 95% sensitivity, 100% specificity, 95.5% accuracy with 100% PPV and 57.1% NPV. The association of EUS with ERCP performed at 100% in all the evaluated parameters.
Table 2 shows the general data on MRCP per formance, and Table 3 gives details on MRCP features for biliary strictures and stones. On the subsequent blinded review performed on the false-negative patients, in only 3 of the 9 cases with previous diagnosis of stenosis, reviewers suspected the presence of microcalculi but without unanimity in each case.
| ERCP+ | ERCP- | ||
| MRCP+ | 102 | 0 | PPV 100% |
| MRCP- | 8 | 90 | NPV 91.8% |
| Sensitivity 92.7% | Specificity 100% | Accuracy 96% |
| Diagnosis | Sensitivity | Specificity | Accuracy | PPV | NPV |
| Choledocholithiasis | 77.40% | 100% | 80.50% | 100% | 85% |
| Hepatobiliary/pancreatic stricture | 100% | 95% | 57.50% | 79% | 100% |
Various types of lesions can cause biliary obstruction; the most frequent are calculi. MRCP is an abdominal MR imaging method that allows noninvasive visualization of the intra- and extrahepatic tree and requires no contrast administration. Recent studies reported that administration of gadoxetic disodium acid or gadobenate dimeglumine improves the sensitivity and specificity of the tool[13,14]. A more recent paper from Choi and Colleagues showed no difference in performance of MRCP with or without contrast medium in detecting biliary stones[15]. Gadoxetic disodium acid (Primovist, Schering Co., Berlin, Germany) and gadobenate dimeglumine (MultiHance, Bracco, Milan, Italy) are both hepatocyte-selective T1-weighted MR agents that are administered intravenously and excreted primarily through the biliary system thus allowing the direct visualization of the biliary tree. Visualization starts after 20 to 100 min following injection, depending on the agent, and lasts for 1-2 h. Use of these contrast agents should provide anatomic information and functional data and should have detected the misdiagnosed stones in our series. We investigated patients with T2-weighted TSE scans that assessed the main sign of biliary tree obstruction: dilatation of extrahepatic or intrahepatic bile ducts. We found that the thin slices provided by this TSE technique may display ductal filling defects as areas of signal void surrounded by bright bile; they provide an optimal contrast between the hyperintense signal of the bile and the hypointense signal of the pathology. The secondary imaging signs of suspected obstruction include hypointense signal defects caused by gallstones or irregularly shaped defects of contours or border in the biliary tree[16]. In our series, stone size was the primary factor that determined efficacy of MRI scans. The hugest limitation of this MRCP technique in detecting lithiasis is that the slices are thicker than 5 mm and this requires partial volume averaging in T2 and T1 series. This can lead to false-negative results when stones are smaller than 5 mm in diameter. The best stone detection was due to the 3D series, in most reviewed cases.
Our data do not differ significantly from those reported in literature[17-24] (Table 4). In detail, we found MRCP had slightly higher sensitivity and PPV than other reported series and slightly lower accuracy in diagnosing biliary calculi when the calculi were smaller than 5 mm (Figure 6). We believe that this may at least partially depend upon the decision not to use a biliary specific contrast. All but one of the missed calculi were smaller than 5 mm, and the high incidence of microstones or sludge is a well-recognized factor that negatively influences the overall MRCP performance independently from the use of contrast medium[11-16,23-25]. The 10 patients diagnosed with microlithiasis of the gallbladder were scheduled for elective surgery; all underwent EUS/ERCP for recurrence of cholestasis or pain. Because some EUS/ERCP was performed with a median interval of 12 d after MRCP, theoretically we cannot exclude that some were true negative at magnetic resonance and developed symptoms of deferred migration of microcalculi. These patients had initially normal blood tests; therefore, the decision not to perform an EUS/ERCP was correct according to reports from Sakai et al[24].
| Ref. | Sensitivity (%) | Specificity (%) | Accuracy (%) | PPV (%) | NPV (%) | Cohort numerosity |
| De Waele et al[17] | 82.6 | 97.5 | 94.2 | 90.5 | 95.2 | 104 pts |
| Shanmugam et al[18] | 97.98 | 84.4 | 374 pts | |||
| Moon et al[19] | 80 | 32 pts | ||||
| Kondo et al[20] | 88 | 28 pts | ||||
| Norero et al[21] | 97 | 74 | 90 | 89 | 90 | 125 pts |
| Scaffidi et al[22] | 88 | 72 | 83 | 87 | 72 | 140 pts |
| Li et al[23] | 84.5 | 87.4 | 165 pts | |||
| Li et al[24] | 64.09 | 80 | 66.27 | 95.27 | 26.17 | 255 pts |
| 80.411 | 79.411 | 69.231 | 94.441 | 48.211 | ||
| Bilgin et al[13] | 82.3 | 96 | 91.7 | 108 pts | ||
| Present study | 100 | 95 | 57.5 | 100 | 85 | 200 pts |
The high incidence of microcalculi is responsible for the high incidence of false negatives in our stone disease group. Even in the 10 cases in which we found microcalculi in the gallbladder but not in the choledocus, we can only hypothesize, based on the clinical evolution of the patients, that they could have migrated in the delay time. However, even when these patients showed symptoms, either cholestasis or pain, 4 remained negative on the EUS/ERCP, and choledocholithiasis was diagnosed only at sphincterotomy and balloon extraction. These data have been reported by other series[25,26].
Our study confirmed that choledocholithiasis continues to be underdiagnosed on MRCP mostly for patients with stones smaller than 5 mm. Nonetheless, MRCP remains the most reliable exam for discriminating which patients to address for more invasive tests (EUS/ERCP) with high sensitivity and specificity. Even if the use of biliary specific contrast is reported to enhance sensitivity, specificity, and NPV[2,23,27,28], this agent may carry additional morbidity related to the administration of contrast that, in our opinion, is not completely balanced by the increase in performance. Our data show that MRCP without contrast medium is a highly sensitive tool for biliary disease; it even has slightly lower specificity. In our series, most stone misdiagnoses were related to calculi smaller than 5 mm or strictures due to concurrent edema in subclinical cholangitis.
MRCP without intravenous contrast is a highly sensitive tool for diagnosing common bile duct stones larger than 5 mm and biliary strictures. This imaging carries a null morbidity. For stones smaller than 5 mm, sensitivity may decrease, but in our opinion, this potential weakness may be corrected with careful clinical follow-up and avoid many useless ERCPs and related morbidity.
The present paper presents a single centre experience comparing accuracy, efficacy and safety of magnetic resonance cholangiopancreatography with endoscopic ultrasounds and/or endoscopic retrograde cholangiopancreatography (ERCP). Data on findings are presented with regards to the presence/absence of biliary tree dilation and size of extracted stones.
Biliary obstruction diagnosis and treatment.
This paper focuses on the small stone disease outlining that even a close follow up may rule diagnosis thus avoiding an excessive use of ERCP.
May be of some help in clinical decision making.
MRCP: Magnetic resonance cholangiopancreatography; EUS: Endoscopic ultrasonography; ERCP: Endoscopic retrograde cholangiopancreatography.
Nicely written article.
P- Reviewer: Gatselis NK, Losanoff JE, Maroni L S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Rahman R, Ju J, Shamma’s J, Goebel S, Sundaram U. Correlation between MRCP and ERCP findings at a tertiary care hospital. W V Med J. 2010;106:14-19. [PubMed] |
| 2. | Chang JH, Lee IS, Lim YS, Jung SH, Paik CN, Kim HK, Kim TH, Kim CW, Han SW, Choi MG. Role of magnetic resonance cholangiopancreatography for choledocholithiasis: analysis of patients with negative MRCP. Scand J Gastroenterol. 2012;47:217-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Sohns JM, Staab W, Dabir D, Spiro JE, Bergau L, Schwarz A, Sohns C. Current role and future potential of magnetic resonance cholangiopancreatography with an emphasis on incidental findings. Clin Imaging. 2014;38:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Salminen P, Laine S, Gullichsen R. Severe and fatal complications after ERCP: analysis of 2555 procedures in a single experienced center. Surg Endosc. 2008;22:1965-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Zuber-Jerger I, Endlicher E, Kullmann F, Gelbmann CM. A new grading system to evaluate the risk of endoscopic retrograde cholangiopancreatography. J Gastroenterol. 2009;44:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Navaneethan U, Konjeti R, Venkatesh PG, Sanaka MR, Parsi MA. Early precut sphincterotomy and the risk of endoscopic retrograde cholangiopancreatography related complications: An updated meta-analysis. World J Gastrointest Endosc. 2014;6:200-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, Søreide JA. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Wilcox CM, Kim H, Trevino J, Ramesh J, Monkemuller K, Varadarajulu S. Prevalence of normal liver tests in patients with choledocholithiasis undergoing endoscopic retrograde cholangiopancreatography. Digestion. 2014;89:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Hu KC, Wang HY, Chang WH, Chu CH, Lin SC, Liu CJ, Wu MS, Shih SC. Clinical presentations of patients from different age cohorts with biliary tract stone diseases. J Gastroenterol Hepatol. 2014;29:1614-1619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Richard F, Boustany M, Britt LD. Accuracy of magnetic resonance cholangiopancreatography for diagnosing stones in the common bile duct in patients with abnormal intraoperative cholangiograms. Am J Surg. 2013;205:371-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Maccioni F, Martinelli M, Al Ansari N, Kagarmanova A, De Marco V, Zippi M, Marini M. Magnetic resonance cholangiography: past, present and future: a review. Eur Rev Med Pharmacol Sci. 2010;14:721-725. [PubMed] |
| 12. | Coppens E, Metens T, Winant C, Matos C. Pineapple juice labeled with gadolinium: a convenient oral contrast for magnetic resonance cholangiopancreatography. Eur Radiol. 2005;15:2122-2129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Bilgin M, Toprak H, Burgazli M, Bilgin SS, Chasan R, Erdogan A, Balcı C. Diagnostic value of dynamic contrast-enhanced magnetic resonance imaging in the evaluation of the biliary obstruction. ScientificWorldJournal. 2012;2012:731089. [PubMed] |
| 14. | Reiner CS, Merkle EM, Bashir MR, Walle NL, Nazeer HK, Gupta RT. MRI assessment of biliary ductal obstruction: is there added value of T1-weighted gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced MR cholangiography? AJR Am J Roentgenol. 2013;201:W49-W56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Choi IY, Yeom SK, Cha SH, Lee SH, Chung HH, Hyun JJ, Kim BH. Diagnosis of biliary stone disease: T1-weighted magnetic resonance cholangiography with Gd-EOB-DTPA versus T2-weighted magnetic resonance cholangiography. Clin Imaging. 2014;38:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Parnaby CN, Jenkins JT, Ferguson JC, Williamson BW. Prospective validation study of an algorithm for triage to MRCP or ERCP for investigation of suspected pancreatico-biliary disease. Surg Endosc. 2008;22:1165-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | De Waele E, Op de Beeck B, De Waele B, Delvaux G. Magnetic resonance cholangiopancreatography in the preoperative assessment of patients with biliary pancreatitis. Pancreatology. 2007;7:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Shanmugam V, Beattie GC, Yule SR, Reid W, Loudon MA. Is magnetic resonance cholangiopancreatography the new gold standard in biliary imaging? Br J Radiol. 2005;78:888-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 54] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Moon JH, Cho YD, Cha SW, Cheon YK, Ahn HC, Kim YS, Kim YS, Lee JS, Lee MS, Lee HK. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005;100:1051-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 108] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, Yamamoto N, Hirano K, Komatsu Y, Tada M. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 139] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 21. | Norero E, Norero B, Huete A, Pimentel F, Cruz F, Ibáñez L, Martínez J, Jarufe N. [Accuracy of magnetic resonance cholangiopancreatography for the diagnosis of common bile duct stones]. Rev Med Chil. 2008;136:600-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Scaffidi MG, Luigiano C, Consolo P, Pellicano R, Giacobbe G, Gaeta M, Blandino A, Familiari L. Magnetic resonance cholangio-pancreatography versus endoscopic retrograde cholangio-pancreatography in the diagnosis of common bile duct stones: a prospective comparative study. Minerva Med. 2009;100:341-348. [PubMed] |
| 23. | Li P, Zhang Z, Li J, Jin L, Han W, Zhang J. Diagnostic value of magnetic resonance cholangiopancreatography for secondary common bile duct stones compared with laparoscopic trans-cystic common bile duct exploration. Med Sci Monit. 2014;20:920-926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Sakai Y, Tsuyuguchi T, Yukisawa S, Tsuchiya S, Sugiyama H, Miyakawa K, Ohara T, Ebara M, Miyazaki M, Yokosuka O. Diagnostic value of magnetic resonance cholangiopancreatography for clinically suspicious spontaneous passage of bile duct stones. J Gastroenterol Hepatol. 2008;23:736-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Tofigh AM, Razmjoie F, Khabbaz A, Ayazi K, Farahmand S, Honar BN, Nikshoar MR. Comparing the efficacy of preoperative magnetic resonance cholangiopancreatography with intra-operative cholangiography in patients suspicious to biliary stones. Gastroenterol Hepatol Bed Bench. 2013;6:80-85. [PubMed] |
| 26. | Kawakubo K, Kawakami H, Kuwatani M, Haba S, Kudo T, Abe Y, Kawahata S, Onodera M, Ehira N, Yamato H. Safety and utility of single-session endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography for the evaluation of pancreatobiliary diseases. Gut Liver. 2014;8:329-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Fernández-Esparrach G, Ginès A, Sánchez M, Pagés M, Pellisé M, Fernández-Cruz L, López-Boado MA, Quintó L, Navarro S, Sendino O. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. Am J Gastroenterol. 2007;102:1632-1639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Hossary SH, Zytoon AA, Eid M, Hamed A, Sharaan M, Ebrahim AA. MR cholangiopancreatography of the pancreas and biliary system: a review of the current applications. Curr Probl Diagn Radiol. 2014;43:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |