Published online Oct 28, 2015. doi: 10.4329/wjr.v7.i10.350
Peer-review started: May 20, 2015
First decision: July 10, 2015
Revised: July 31, 2015
Accepted: August 20, 2015
Article in press: August 21, 2015
Published online: October 28, 2015
Processing time: 162 Days and 10.7 Hours
AIM: To investigate the prevalence of relevant incidental findings (RIFs) detected during routine abdominal contrast-enhanced computed tomography (CeCT).
METHODS: We retrospectively evaluated the reports of a consecutive series of abdominal CeCT studies performed between January and May 2013. For each report, patients’ age and sex, admission as inpatient or outpatient, clinical suspicion as indicated by the requesting physician, availability of a previous abdominal examination, and name of the reporting radiologist were recorded. Based on the clinical suspicion, the presence and features of any RIFs (if needing additional workup) was noted.
RESULTS: One thousand forty abdominal CeCT were performed in 949 patients (528 males, mean age 66 ± 14 years). No significant difference was found between inpatients and outpatients age and sex distribution (P > 0.472). RIFs were found in 195/1040 (18.8%) CeCT [inpatients = 108/470 (23.0%); outpatients = 87/570 (15.2%); P = 0.002]. RIFs were found in 30/440 (6.8%) CeCT with a previous exam and in 165/600 (27.5%) without a previous exam (P < 0.001). Radiologists’ distribution between inpatients or outpatients was significantly different (P < 0.001). RIFs prevalence increased with aging, except for a peak in 40-49 year group. Most involved organs were kidneys, gallbladder, and lungs.
CONCLUSION: A RIF is detected in 1/5 patients undergoing abdominal CeCT. Risk of overdiagnosis should be taken into account.
Core tip: A relevant incidental finding (IF) is detected in one out of five patients undergoing abdominal contrast-enhanced computed tomography. Thus, in clinical practice, we daily perform unconscious collateral screening for a number of abdominal diseases. Notably, a problem still exists about how to deal with these findings, as their detection can be stressful and potentially harmful for patients, also contribute to increase in health care costs. On the one hand we have the risk of overdiagnosis, on the other hand there is a risk of legal issues for not having reported and suggested further work-up for these IFs.
- Citation: Sconfienza LM, Mauri G, Muzzupappa C, Poloni A, Bandirali M, Esseridou A, Tritella S, Secchi F, Di Leo G, Sardanelli F. Relevant incidental findings at abdominal multi-detector contrast-enhanced computed tomography: A collateral screening? World J Radiol 2015; 7(10): 350-356
- URL: https://www.wjgnet.com/1949-8470/full/v7/i10/350.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i10.350
Contrast-enhanced computed tomography (CeCT) has gained a crucial role in medical practice[1]. With the increase of number and quality of CeCT examinations, a concurrent increase of unexpected (incidental) findings unrelated to clinical suspicion has occurred[2]. Most of these incidental findings (IFs) are immediately recognized as benign or as anatomical variants and have no clinical relevance, but in a number of IFs additional workup is needed to reach a final diagnosis. This in turn generates anxiety for patients and additional costs for the healthcare systems[3].
The discovery of an IF has been cited among the causes of increased use of cross-sectional imaging and ionizing radiation exposure for medical reasons, being theoretically even detrimental for the patient[1]. Balancing the benefit of an early detection of a disease with the risk of overdiagnosis is crucial from a societal viewpoint when a screening program is planned[4]. Although some attempts to standardise the management of IFs have been made, in the clinical practice their management still vary widely between physicians and countries[5].
Several studies have been devoted to assess the prevalence of IFs and their relevance[6-12]. They have generally been performed to evaluate collateral findings detected during an imaging study dedicated to a single anatomical structure (e.g., IFs detected during CT colonography or cardiac CT/MRI, breast MRI, etc.)[6-11] or performed in a specific clinical setting (e.g., IFs discovered during emergency abdominal CT)[12]. Conversely, no data are available about relevant IFs that are occasionally detected in a series of consecutive patients undergoing abdominal CeCT.
The purpose of our work was to investigate the prevalence of relevant IFs detected during abdominal CeCT in the daily routine at our institution.
Institutional Review Board approval of IRCCS Ospedale San Raffaele, Milano, Italy was obtained and patients’ informed consent was waived. Our report is concerned with a retrospective evaluation of the reports of a consecutive series of abdominal CeCT performed at our institution between January and May 2014, including inpatients, outpatients, and patients coming from the emergency department. The last ones were considered as outpatients. CeCT examinations were performed using either a 16- or 64-slice CT systems (SOMATOM Emotion and Sensation, respectively; Siemens Medical, Erlangen, Germany) with oral administration of variable amount of diluted water-soluble iodinated contrast agent (Gastrografin, Bayer-Schering, Germany) and intravenous injection of iodinated contrast agent (Iomeron 350, Bracco, Milano, Italy) using different acquisition protocol according to the clinical suspicion. Electronic reports were retrieved from our radiology information system (RIS) (PolaRIS, El.Co., Cairo Montenotte, Savona, Italy) and were reviewed in consensus by two radiology residents (CM and MB) with three years’ experience in CeCT. For each report, they recorded patients’ age and sex, his/her admission as inpatient or outpatient, the clinical suspicion as indicated by the requesting physician, and the name of the radiologist who signed the report. Based on the clinical suspicion, the report was searched to detect the presence of relevant IFs. IF was defined as “an incidentally discovered mass or lesion detected by abdominal CeCT performed for an unrelated reason”[5]. IFs were considered as relevant if additional workup (other imaging tests, clinical evaluation, or follow-up) was suggested by the reporting radiologist. If no specific note was included in the report, the two reviewers assessed in consensus the needing of additional workup. In case of disagreement, a staff radiologist with 10 years of experience in CeCT (LMS) addressed the issue.
For all patients, reviewers noted the presence of previous cross-sectional imaging exams (ultrasound, CT, or magnetic resonance imaging) performed within one year. If this information was already included in the report, patients were classified as provided with a previous examination. Thus, reviewers rated any newly reported IF as not already known. If the report did not include any information, previous exams were searched for in our RIS. Finally, if none of the two abovementioned criteria were applicable, patients were considered to be lacking of previous exams. For patients who underwent more than one abdominal CeCT in the considered period, the first exam was treated according to the abovementioned criteria, while the second and/or the third following exam was considered to have an available previous exam.
Relevant IFs were also stratified according to 10-year age groups and classified according to the organ involved.
Statistical analysis was performed by one of the authors (GDL) who has advanced statistical expertise. Data regarding the present paper may be shared upon request prior further Institutional Review Board Approval.
Age distribution between inpatients and outpatients subgroups was compared using the U Mann-Whitney test. Sex distribution between inpatients and outpatients, as well as relevant IFs distribution in our series was compared within different subgroups (inpatients, outpatients, patients with or without a previous exam) using the Chi-square test. Odds ratios were also calculated. All calculations were performed using SPSS Statistics v. 19 (SPSS, Chicago, IL, United States) and Excel (Microsoft Excel® 2010, Redmond, WA, United States). A P-value less than 0.05 was considered as significant.
In the considered period, 1040 abdominal CeCT were performed in 949 patients (528 males, 421 females, mean age ± standard deviation 66 ± 14 years); 75 patients underwent two CeCT examinations and eight patients underwent three CeCT examinations.
Four hundred seventy out of 1040 (45.2%) CeCT examinations were performed in 401 inpatients (228 males, 173 females; mean age 67 ± 15 years) and 570/1040 (54.8%) in 548 outpatients (300 males, 248 females; mean age 65 ± 12 years). Age and sex distribution was not significantly different between inpatients and outpatients (P = 0.472 and P = 0.717, respectively).
Overall, relevant IFs were found in 195/1040 (18.8%) CeCT, one IF per exam: 108/470 (23.0%) in inpatients and 87/570 (15.2%) in outpatients, the difference being statistically significant (P = 0.002).
A previous exam was available for 440/1040 (42.3%) CeCT examinations while it was not available for the remaining 600/1040 (57.7%). Relevant IFs were found in 30/440 (6.8%) CeCT with a previous exam and in 165/600 (27.5%) with no previous exam (P < 0.001). Subgroup analyses between inpatients and outpatients, with or without a previous exam are reported in Tables 1 and 2. No statistical difference was found regarding the number of patients with or without previous exams subdivided into inpatients and outpatients.
| Previous exam | P | Odds ratio | ||
| Yes | No | (no/yes) | ||
| Inpatients | 14/187 (7.5) | 94/283 (33.2) | < 0.001 | 4.7 |
| Outpatients | 16/253 (6.3) | 71/217 (22.4) | < 0.001 | 3.7 |
| p | 0.632 | 0.003 | ||
| Previous exam | Yes/no | ||
| Yes | No | ||
| Inpatients | 187/1040 (18.0) | 283/1040 (27.2) | 0.66 |
| Outpatients | 253/1040 (24.3) | 317/1040 (30.5) | 0.80 |
| Inpatients/outpatients | 0.74 | 0.89 | P = 0.152 |
Exams were reported by nine different radiologists with three to 20 years experience in abdominal CeCT. The distribution of radiologists who reported CeCT exams of inpatients or outpatients was significantly different (P < 0.001). Full data are reported in Table 3.
| Radiologist | Overall | Inpatients | Outpatients | |||
| Reports | Relevant IFs | Reports | Relevant IFs | Reports | Relevant IFs | |
| A | 69/1040 (6.6) | 11/69 (16.0) | 43/470 (9.1) | 8/43 (18.6) | 26/570 (4.6) | 3/26 (11.5) |
| B | 59/1040 (5.7) | 11/59 (18.6) | 21/470 (4.4) | 3/21 (14.3) | 38/570 (6.6) | 8/38 (21.1) |
| C | 164/1040 (15.8) | 23/164 (14.0) | 75/470 (16.0) | 12/75 (16.0) | 89/570 (15.6) | 11/89 (12.4) |
| D | 353/1040 (33.9) | 81/353 (22.9) | 145/470 (30.9) | 41/145 (28.2) | 208/570 (36.4) | 40/208 (19.2) |
| E | 160/1040 (15.4) | 21/160 (13.1) | 48/470 (10.2) | 9/48 (18.7) | 112/570 (19.6) | 12/112 (10.7) |
| F | 102/1040 (9.8) | 12/102 (11.8) | 70/470 (14.9) | 10/70 (14.3) | 32/570 (5.6) | 2/32 (6.2) |
| G | 8/1040 (0.8) | 3/8 (37.5) | 5/470 (1.1) | 2/5 (40.0) | 3/570 (0.5) | 1/3 (33.3) |
| H | 28/1040 (2.7) | 8/28 (28.6) | 11/470 (2.3) | 4/11 (36.4) | 17/570 (3.0) | 4/17 (23.5) |
| I | 97/1040 (9.3) | 25/97 (25.8) | 52/470 (11.1) | 19/52 (36.5) | 45/570 (7.9) | 6/45 (13.3) |
| Total | 1040/1040 (100.0) | 195/1040 (18.8) | 470/470 (100.0) | 108/470 (23.0) | 570/570 (100.0) | 87/570 (15.3) |
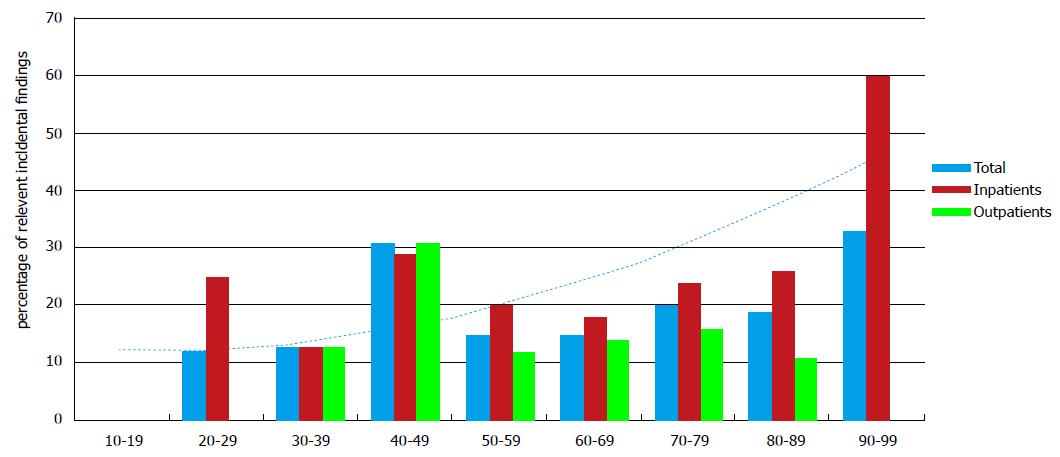
Distribution of relevant IFs stratified according to 10-year age groups (total, inpatients, and outpatients) is shown in Table 4 and graphically represented in Figure 1.
| Age | Overall | Inpatients | Outpatients | |||
| CeCT | Relevant IFs | CeCT | Relevant IFs | CeCT | Relevant IFs | |
| 10-19 | 6/1040 (0.6) | 0/6 (0.0) | 3/470 (0.6) | 0/3 (0.0) | 3/570 (0.5) | 0/3 (0.0) |
| 20-29 | 17/1040 (1.7) | 2/17 (11.8) | 8/470 (1.7) | 2/8 (25.0) | 9/570 (1.6) | 0/9 (0.0) |
| 30-39 | 40/1040 (3.8) | 5/40 (12.5) | 8/470 (1.7) | 1/8 (12.5) | 32/570 (5.6) | 4/32 (12.5) |
| 40-49 | 88/1040 (8.5) | 27/88 (30.6) | 34/470 (7.2) | 10/34 (29.4) | 54/570 (9.4) | 17/54 (31.5) |
| 50-59 | 130/1040 (12.5) | 20/130 (15.4) | 55/470 (11.7) | 11/55 (20.0) | 75/570 (13.6) | 9/75 (12.0) |
| 60-69 | 260/1040 (25.0) | 40/260 (15.4) | 112/470 (23.8) | 20/112 (17.8) | 148/570 (26.0) | 20/148 (13.5) |
| 70-79 | 361/1040 (34.7) | 73/361 (20.2) | 173/470 (36.8) | 42/173 (24.2) | 188/570 (33.0) | 31/188 (16.5) |
| 80-89 | 129/1040 (12.4) | 25/129 (19.4) | 72/470 (15.3) | 19/72 (26.4) | 57/570 (10.0) | 6/57 (10.5) |
| 90-99 | 9/1040 (0.8) | 3/9 (33.3) | 5/470 (1.1) | 3/5 (60.0) | 4/570 (0.7) | 0/4 (0.0) |
| Tot | 1040/1040 (100) | 195/1040 (18.8) | 470/470 (100) | 108/470 (23.0) | 570/570 (100) | 87/570 (15.2) |
Distribution of relevant IFs among involved organs is shown in Table 5. A list of the relevant Ifs is reported in Table 6.
| Anatomical site | Relevant IFs |
| Kidney | 28/195 (14.4) |
| Gallbladder | 27/195 (13.85) |
| Lung | 24/195 (12.3) |
| Uterus | 20/195 (10.3) |
| Adrenal gland | 19/195 (9.7) |
| Vessels | 19/195 (9.7) |
| Musculoskeletal | 12/195 (6.2) |
| Ovary | 12/195 (6.2) |
| Liver | 7/195 (3.6) |
| Spleen | 6/195 (3.1) |
| Prostate | 6/195 (3.1) |
| Bowel | 5/195 (2.6) |
| Bladder | 4/195 (2.1) |
| Pancreas | 3/195 (1.5) |
| Testicles | 3/195 (1.5) |
| IF | n % |
| Cholelithiasis | 27 (2.6%) |
| Uterine lesion | 20 (1.9%) |
| Adrenal mass | 19 (1.8%) |
| Non-simple renal cyst | 15 (1.4%) |
| Lung nodule | 13 (1.3%) |
| Adnexal mass | 12 (1.2%) |
| Kidney stones | 10 (1.0%) |
| Pleuric effusion | 8 (0.8%) |
| Focal liver lesion | 6 (0.6%) |
| Enlarged prostate | 6 (0.6%) |
| Focal splenic lesion | 5 (0.5%) |
| Abdominal aortic aneurysm | 4 (0.4%) |
| Bladder wall thickening | 4 (0.4%) |
| Aortic ectasia | 4 (0.4%) |
| Inguinal hernia | 4 (0.4%) |
| Focal pancreatic lesion | 3 (0.3%) |
| Focal renal lesion | 3 (0.3%) |
| Atheromasic aorta | 3 (0.3%) |
| Iliac aneurysm | 3 (0.3%) |
| Focal lesion of bones | 3 (0.3%) |
| Lung consolidation | 2 (0.2%) |
| Focal muscolar lesion | 2 (0.2%) |
| Appendicular enlargement | 2 (0.2%) |
| Hydrocele testis | 2 (0.2%) |
| Splenic artery aneurysm | 1 (0.1%) |
| Mesenteric artery aneurysm | 1 (0.1%) |
| Vertebral fracture | 1 (0.1%) |
| Diverticulitis | 1 (0.1%) |
| Ectasic portal vein | 1 (0.1%) |
| Endoleak | 1 (0.1%) |
| Emphysema | 1 (0.1%) |
| Spinal disc herniation | 1 (0.1%) |
| Colonic cancer | 1 (0.1%) |
| Stasis liver | 1 (0.1%) |
| Incisional hernia | 1 (0.1%) |
| Femoral artery occlusion | 1 (0.1%) |
| Splenomegaly | 1 (0.1%) |
| Subocclusion | 1 (0.1%) |
| Varicocele | 1 (0.1%) |
| Total | 195 (18.7%) |
This study was performed to evaluate the prevalence of relevant IFs in a consecutive series of patients who underwent abdominal CeCT at our institution. Our study shows that relevant IFs are commonly encountered, being detected in about one fifth of patients undergoing abdominal CeCT.
Prevalence of IFs has been reported in literature to vary from 3% to 58%[6-12], depending on the study population, the organ or system involved, and on criteria used to classify IFs. Several papers are focused on the rate of IFs detected during CT exams aimed to the evaluation of a single organ. For example, extracolonic IFs are reported to be detected in up to 23% of patients undergoing CT colonography[6,8] and this is nowadays considered one of the major issues regarding colon cancer screening with this technique. Dewey et al[13] reported a 5% prevalence of relevant extra-cardiac IFs and a 10% prevalence of non-relevant IFs during coronary CT angiography in a cohort of 108 patients. However, Gil et al[14] reported extra-cardiac IFs in 56% of their series, regardless to their severity. In the study of Law et al[15], 56 out of 295 patients (19%) had extra-coronary IFs requiring clinical or radiological follow up. Other studies deal with IFs prevalence in a single organ. Rinaldi et al[9] re-assessed the images of a series of abdominal CT exams to evaluate prevalence, reporting rates, and clinical implications of incidentally-discovered pulmonary nodules. In this retrospective case review, 39.1% of patients had lung nodules but only 8.4% of them were mentioned in the report. O’Connor et al[10] reported a 14% IFs prevalence in kidneys, while IFs prevalence in adrenal glands was reported to range between 3% and 7%[16]. Some authors investigated IFs prevalence in a specific setting, such as patients who underwent abdominal CT in emergency. In this particular context, IFs prevalence has been reported between 15% and 35%[12]. A recent literature review on 44 original studies on all imaging diagnostic modalities published between 1986 and 2007 reported a IFs mean prevalence of 23.6%[2]. To our knowledge, no previous report investigated the overall prevalence of relevant IFs in a consecutive series of routine abdominal CeCT.
In our series, we found a significantly higher amount of relevant IFs in inpatients compared to outpatients. This result could be explained by the fact that CT exams performed in inpatients are generally requested with a focused clinical question (e.g., staging in a patient with colon cancer). As findings are considered as incidental solely when not related to the clinical suspicion, the narrower the clinical suspicion the higher the possibility to detect an unrelated finding[2]. Conversely, clinical suspicion reported in outpatients’ requests is usually more generic (e.g., abdominal pain), allowing for an easier correlation to a wide range of IFs, although this is not necessarily the rule. In our study, patients from emergency department were included in the outpatients group because they are often sent with a generic clinical suspicion, based on ill-defined clinical data and symptoms.
In our series, the only independent predictor of a relevant IF was the availability of a previous exam. In patients who had not performed a previous exam, the odds ratio calculation demonstrated a probability of detecting a relevant IF about five times greater than in those who had a previous exam available. This was expected, as IFs that had been already detected in previous exam have been currently considered as already known and thus excluded from our analysis.
We found significant difference in the distribution of radiologists who reported CeCT exams performed in inpatients or in outpatients. This data is partially due to statistical analysis of a large number of radiologists and a relatively small number of exams per each reader. However, this could somewhat represent an additional explanation of the difference of relevant IFs prevalence between inpatients and outpatients.
Considering age group stratification (see Table 4), we found that relevant IFs increase with aging, as expected[17]. An exception is represented by the 40-to-49 year group, in which relevant IFs prevalence was about one third. Patients included in such a group were lacking of a previous exam in 70% of cases, compared to the overall value of 57.7%. As the absence of a previous exam increase the possibility of relevant IFs detection, this data can somewhat explain the unusual prevalence peak in that age group.
Regarding the classification of relevant IFs according to the anatomical site, we note that the most involved organs were kidneys, gallbladder, and lungs. For renal lesions, there is no validated criteria - apart from follow-up - to differentiate solid benign from malignant lesions[18]. This could partially explain the high incidence of relevant IFs, as for these lesions additional workup is frequently recommended. Regarding gallbladder, 10%-15% of occidental subjects will develop gallstones in their life. People with asymptomatic gallstones are likely to develop related problems in 1%-4% of cases, younger people being more at risk than elderly[19]. Although prophylactic cholecistectomy is usually unnecessary, this procedure can be justified in young subjects that are more prone to develop acute pancreatitis related to small stones[20]. This partially explains the high number of relevant IFs reported in our series, as additional workup (ultrasound follow-up or surgical evaluation) is usually suggested in these cases. In our series, we found 2.5% IFs related to lungs, considered as relevant in respect to previously published criteria[21]. In a previous paper, Rinaldi et al[9] reported an overall incidence of 39.1% of lung nodules visible on abdominal CeCT images, only 8.4% of them being described in radiologists’ report. However, our values are not directly comparable to theirs, as we included only reported incidentally discovered lung nodules deserving additional workup.
Early diagnosis and detection of asymptomatic diseases have well known advantages, being also at the basis of screening programs. However, additional workup of relevant IFs can be responsible of tests and procedure that are often expensive - both for patients and healthcare systems - stressful, and sometimes potentially harmful for patients (e.g., invasive procedures or ionizing radiations exposure). Also, it can happen that IFs are so slow-progressing that will never cause symptoms or death. When this happens, the diagnosis might have been correct but is clinically irrelevant. This important concept is also known as overdiagnosis and it is a risk that should be always taken into account when dealing with screening tools and early diagnosis in general[4].
Our study has some limitations. First, it was conducted at a single institution, so results may be not directly transferable to general population. Then, the retrospective nature of the study that was aimed solely to review radiological reports. Thus, our action was limited to analyze findings that were included in those reports. Also, our results may be somewhat underestimated. Moreover, being able to access previous exams only when provided by patients themselves or when performed at our institution have surely affected the data of patients considered as lacking of a previous exam. Finally, we do not know whether additional work-up was really performed. Thus we could not evaluate the real impact of IFs on the healthcare system.
Summarizing, a relevant IF is detected in one out of five patients undergoing abdominal CeCT. Thus, in clinical practice, we daily perform unconscious collateral screening for a number of abdominal diseases. Notably, a problem still exists about how to deal with these findings, as their detection can be stressful and potentially harmful for patients, also contributing to raise health care costs. On the one hand we have the risk of overdiagnosis, on the other hand the risk of legal issues for not having reported and suggested further work-up for these IFs[22].
Incidental findings (IFs) during contrast-enhanced computed tomography (CeCT) are increasingly being detected. This generates anxiety for patients and additional costs for the healthcare systems.
The study is concerned with the evaluation of IFs during CeCT of the abdomen.
A relevant IF is detected in one out of five patients undergoing abdominal CeCT. Thus, in clinical practice, the authors daily perform unconscious collateral screening for a number of abdominal diseases.
A problem still exists about how to deal with these findings, as their detection can be stressful and potentially harmful for patients, also contribute to increase in health care costs. On the one hand we have the risk of overdiagnosis, on the other hand there is a risk of legal issues for not having reported and suggested further work-up for these IFs.
Abdominal CE-CT: CeCT of the abdomen, a panoramic examination of the abdomen used to evaluate a wide range of pathologic conditions. IF: An incidentally discovered mass or lesion detected by abdominal CeCT performed for an unrelated reason.
The manuscript is well written.
P- Reviewer: Chu JP, Kumar J S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [PubMed] |
| 2. | Lumbreras B, Donat L, Hernández-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010;83:276-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 284] [Cited by in RCA: 265] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 3. | Berland LL. Incidental extracolonic findings on CT colonography: the impending deluge and its implications. J Am Coll Radiol. 2009;6:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Sardanelli F. Evidence-based radiology and its relationship with quality. In Bruno MA, Abujudeh HH, eds. Quality and safety in Radiology. New York: Oxford University Press 2009; 256-290. |
| 5. | Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 624] [Cited by in RCA: 606] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 6. | Yee J, Kumar NN, Godara S, Casamina JA, Hom R, Galdino G, Dell P, Liu D. Extracolonic abnormalities discovered incidentally at CT colonography in a male population. Radiology. 2005;236:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Veronesi G, Bellomi M, Spaggiari L. The rate of incidental findings in lung cancer screening trials is not negligible. Eur Radiol. 2008;18:529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Secchi F, Lanza E, Cannaò PM, Petrini M, Sconfienza LM, Sardanelli F. Noncardiac findings in clinical cardiac magnetic resonance: prevalence in 300 examinations after blind reassessment. J Comput Assist Tomogr. 2013;37:382-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Rinaldi MF, Bartalena T, Giannelli G, Rinaldi G, Sverzellati N, Canini R, Gavelli G. Incidental lung nodules on CT examinations of the abdomen: prevalence and reporting rates in the PACS era. Eur J Radiol. 2010;74:e84-e88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | O’Connor SD, Pickhardt PJ, Kim DH, Oliva MR, Silverman SG. Incidental finding of renal masses at unenhanced CT: prevalence and analysis of features for guiding management. AJR Am J Roentgenol. 2011;197:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Lazoura O, Vassiou K, Kanavou T, Vlychou M, Arvanitis DL, Fezoulidis IV. Incidental non-cardiac findings of a coronary angiography with a 128-slice multi-detector CT scanner: should we only concentrate on the heart? Korean J Radiol. 2010;11:60-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Ekeh AP, Walusimbi M, Brigham E, Woods RJ, McCarthy MC. The prevalence of incidental findings on abdominal computed tomography scans of trauma patients. J Emerg Med. 2010;38:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Dewey M, Schnapauff D, Teige F, Hamm B. Non-cardiac findings on coronary computed tomography and magnetic resonance imaging. Eur Radiol. 2007;17:2038-2043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Gil BN, Ran K, Tamar G, Shmuell F, Eli A. Prevalence of significant noncardiac findings on coronary multidetector computed tomography angiography in asymptomatic patients. J Comput Assist Tomogr. 2007;31:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Law YM, Huang J, Chen K, Cheah FK, Chua T. Prevalence of significant extracoronary findings on multislice CT coronary angiography examinations and coronary artery calcium scoring examinations. J Med Imaging Radiat Oncol. 2008;52:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | National Institute of Health. NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens State Sci Statements. 2002;19:1-25. [PubMed] |
| 17. | Goldstein S. The biology of aging. N Engl J Med. 1971;285:1120-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 88] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Lee SI, Krishnaraj A, Chatterji M, Dreyer KJ, Thrall JH, Hahn PF. When does a radiologist’s recommendation for follow-up result in high-cost imaging? Radiology. 2012;262:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Sanders G, Kingsnorth AN. Gallstones. BMJ. 2007;335:295-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 87] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Venneman NG, Buskens E, Besselink MG, Stads S, Go PM, Bosscha K, van Berge-Henegouwen GP, van Erpecum KJ. Small gallstones are associated with increased risk of acute pancreatitis: potential benefits of prophylactic cholecystectomy? Am J Gastroenterol. 2005;100:2540-2550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Swensen SJ. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1178] [Cited by in RCA: 1129] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 22. | Berlin L. Professionalism and disclosing errors. AJR Am J Roentgenol. 2012;198:W315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |