Published online Aug 28, 2014. doi: 10.4329/wjr.v6.i8.629
Revised: May 24, 2014
Accepted: June 18, 2014
Published online: August 28, 2014
Processing time: 142 Days and 15.5 Hours
Pancreatico-duodenal artery (PDA) pseudoaneurysms are rare vascular conditions with high mortality rates after rupture and they are frequently secondary to pancreatitis, surgery, trauma or infection. Due to the high risk of rupture and bleeding, it is mandatory to treat all pseudoaneurysms, regardless of their size or symptomatology. First option of treatment is open surgical repair, but it has high mortality rate, especially in hemodynamically unstable patients. In the recent years, percutaneous ultrasonography (US)- or computed tomography-guided thrombin injection was proposed as an alternative method for treating visceral aneurysms and pseudoaneurysms, but few reports described this therapy in case of peri-pancreatic pseudoaneurysms. We present a rare case of pseudoaneurysm of the PDA in a patient with no previous history of pancreatitis nor major surgery but with an occlusive lesion of the celiac axis. To the best of our knowledge this is the first reported case of PDA pseudoaneurysm successfully treated in emergency by single transabdominal US-guided injection of thrombin after failed attempts of percutaneous catheterization of the feeding vessel of the pseudoaneurysm.
Core tip: We present a rare case of pseudoaneurysm of the pancreatico-duodenal artery (PDA) in a patient with no risk factors but with an occlusive lesion of the celiac axis. To the best of our knowledge this is the first reported case of PDA pseudoaneurysm successfully treated in emergency by single transabdominal ultrasonography-guided injection of thrombin after failed attempts of percutaneous catheterization of the feeding vessel of the pseudoaneurysm.
- Citation: Barbiero G, Battistel M, Susac A, Miotto D. Percutaneous thrombin embolization of a pancreatico-duodenal artery pseudoaneurysm after failing of the endovascular treatment. World J Radiol 2014; 6(8): 629-635
- URL: https://www.wjgnet.com/1949-8470/full/v6/i8/629.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i8.629
Pancreatico-duodenal artery (PDA) pseudoaneurysms are potentially life-threatening but rare vascular conditions, accounting for 2% of splanchnic artery aneurysms and with mortality rates after rupture of 15%-50%[1-4].
They are mostly due to pancreatitis, surgery, trauma, infection, iatrogenic lesions, vasculitis and atherosclerosis[5], but also to the presence of a celiac axis or common haepatic artery stenosis/occlusion, known as Sutton-Kadir syndrome[6,7]. These lesions may be identified by means of different imaging techniques [ultrasonography (US), computed tomography (CT), magnetic resonance imaging (MRI) and digital subtraction angiography (DSA)].
Due to the high risk of rupture and bleeding and the absence of predictive factors, it is recommended to treat all pseudoaneurysms, regardless of their size or symptomatology[8]. Open surgical repair, consisting of resection, ligation, exclusion, bypass or endo/organ resection, has high-mortality rate and is applied in hemodynamically unstable patients or as secondary approach after failed transcatheter embolization[9].
In the recent years, with the development of materials and techniques in the field of interventional radiology, percutaneous endovascular management of such a pseudoaneurysm is becoming the first-line treatment, with low morbidity and mortality[10,11].
Percutaneous US- or CT-guided injection is an alternative method for treating visceral aneurysms and pseudoaneurysms[12-23], but few reports described this therapy in case of superior mesenteric artery (SMA) or PDA pseudoaneurysms[9,24-28].
To the best of our knowledge, this is the first reported case of a PDA pseudoaneurysm percutaneously treated by direct thrombin injection by US guidance after failing of endovascular treatment.
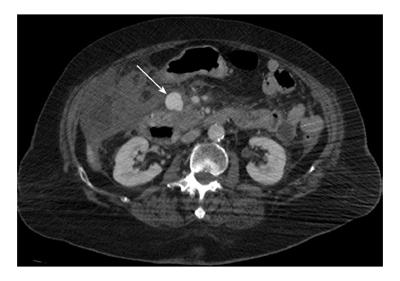
An 82-year-old woman was in a peripheral hospital two days before for cerebral haemorrhage and was admitted in emergency to our central hospital with the suspicion of acute bleeding. During the hospital stay routine laboratory investigation revealed severe anaemia with haemoglobin drop to 6.0 g/dL and contrast-enhanced thoraco-abdominal CT scan was performed on a 64-slice multi-detector Siemens scanner. It identified an oval, rounded mass within the pancreatic head with slow centrifugal contrast-enhancement, presumed to be a bleeding pseudoaneurysm with a haematoma and a small haemoperitoneum around the spleen (Figure 1). The feeding artery to the pseudoaneurysm was identified as a PDA, given the area of distribution and the origin from SMA. The patient’s surgical history was unremarkable and did not have history of chronic pancreatitis.
At the admission the patient underwent to endotracheal intubation but was hemodynamically stable. Due to her age and clinical co-morbidities, open surgery was not the best option and an attempt with endovascular procedure was decided.
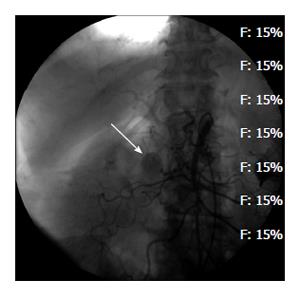
Angiography was performed using Siemens equipment (Axiom Artis U, Siemens AG, Forchheim, Germany). Under local anaesthesia (lidocaine 2%), using the Seldinger technique, a selective SMA catheterization (Cobra Glidecath, 5F, 65-cm-long, Terumo, Tokyo, Japan) with a hydrophilic guidewire (0.035”, 150-cm-long, Terumo) confirmed the pseudoaneurysm of 2-cm on diameter of the PDA area (Figure 2). Both the examination of the SMA made in different projections, including the lateral view and superselective catheterization (Progreat, 2.7F, 130-cm-long, Terumo, Tokyo, Japan) of at least 4 proximal branches did not show the pseudoaneurysm so that the feeding vessel could not be identified.
Selective catheterization (Radifocus guidewire, 0.035”, 150-cm-long, and Cobra Glidecath, 5F, 65-cm-long, Terumo) of the celiac artery (CA) was performed, but the gastroduodenal artery (GDA) was not depicted, because of a close stenosis of the take-off of CA from the abdominal aorta.
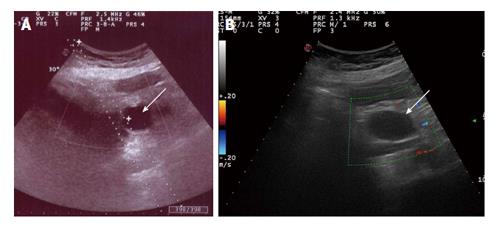
Since we were not able to identify and catheterize the feeding vessel, and considering the patient’s high-risk clinical condition, percutaneous embolization with thrombin injection was suggested. The procedure was performed after local anaesthesia (lidocaine 2%) and a Chiba needle (Ecojekt 18G, 20-cm-long, HS Hospital Service, Aprilia, Latina, Italy) was inserted into the pseudoaneurysmal sac through the anterior abdominal wall under US guidance (MyLab, Esaote, Genova, Italy) and 2 mL (1000 IU) of human thrombin (Tisseel, Baxter AG, Rome, Italy) were injected. During the injection, the anechoic area of pseudoaneurysm turned into hypoechoic area and the colour signals disappeared because of immediate thrombosis was achieved on the US control (Figure 3).
A final SMA selective control DSA performed at the end of the procedure confirmed complete exclusion of the pseudoaneurysm with no endoleak and preserved perfusion of the SMA.
Finally, haemostasis of the puncture site at the right common femoral artery (CFA) was obtained using a vascular closure device (Angioseal 6F, Saint Jude, MN, United States).
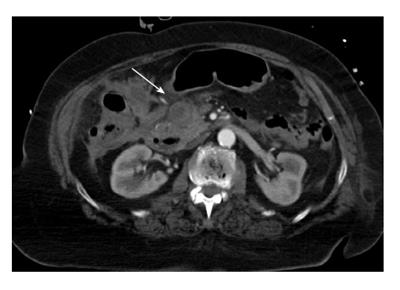
Thrombotic or immunologic complications of thrombin were not observed. A 1-wk follow-up abdominal CT scan showed a completely thrombosed PDA pseudoaneurysm with no endoleak or recurrence of bleeding, and preserved flow through the SMA branches (Figure 4). Patient’s condition was stable and the blood test normalized. Doppler ultrasound examinations at 2 wk and 3 mo confirmed thrombosis of the pseudoaneurysm, without any echographic signs of blood flow within.
Patient was discharged from the intensive care unit and she is now under careful clinic and imaging follow-up.
Natural history of the visceral false aneurysms is potentially the rupture and a lethal abdominal haemorrhage, with a rupture rate of 50% and a mortality rate up to 80%[29].
Causes of SMA aneurysm and pseudoaneurysm formation include chronic pancreatitis, atherosclerosis, trauma, surgery, biopsy, infection, collagen vascular disease, medial necrosis, arthritis and dissection.
Symptoms depend on the location and include abdominal pain, melena, body loss, internal haemorrhage and hypovolemic shock due to pseudoaneurysm rupture.
Our patient did not have history of chronic pancreatitis and was suspected to have an internal haemorrhage because of onset of severe anaemia and lacking a worsening of the brain haemorrhage.
Imaging techniques for the diagnosis of pseudoaneurysms include US, CT, MRI and DSA[4]; this shows precise location, morphology, size of the sac, feeding collateral vessels and efferent arteries if present, and enables immediate endovascular treatment.
PDA or SMA pseudoaneurysms require immediate treatment due to a high mortality, up to 90%, in the case of not treatment[18] and it includes open surgical repair and non surgical procedures.
Surgical treatment, traditionally a first-line therapy option[30], is invasive and is associated with high risk of infection, haemorrhage and long rehabilitation time. Deep retroperitoneal and retroduodenal position of the vessels involved in peri-pancreatic aneurysms is technically challenging for the surgeon and as much as 70% of the PDA aneurysms are not detected at surgery[3].
Non surgical management includes endovascular and percutaneous techniques[31]. At present endovascular treatment is considered the first choice for embolization of PDA and SMA pseudoaneurysm and the technical success ranges from 56% to 100%[10,31-33]. Coils, gelfoam, thrombin, glue (N-butyl-cyanoacrylate), stent-graft and Amplatzer vascular plug (AVP, ev3, Plymouth, Unites States), are different materials for endovascular management and the choice depends on the vascular anatomy of the target lesion and the patient’s clinical condition[34].
Recently, 2 new agents have been used for endovascular treatment of aneurysms and pseudoaneurysms: ethylene vinyl alcohol copolymer (Onyx, Micro Therapeutics, Irvine, CA, Unites States)[35] and a multilayer flow modulator stent (Cardiatis, Multilayer, Bruxels, Belgium)[32,36].
When antegrade superselective catheterization of the feeding vessel of the PDA pseudoaneurysm fails owing to vessel tortuosity, a retrograde catheterization of the PDA by way of collateral vessels from the GDA could potentially be advantageous.
Unfortunately, in our patient a close stenosis at the origin of the CA did not allowed retrograde catheterization of PDA. As Sutton et al[6] and Kadir et al[7] reported, proximal obstruction of the CA induces consequent compensatory hypertrophy of the PDA and causes hemodynamic alterations that favour the development of PDA aneurysms and pseudoaneurysms[34,37].
An alternative option to endovascular management of the pseudoaneurysms is the percutaneous embolization by thrombin injection under US or CT guidance.
At first, this method was used for the treatment of iatrogenic pseudoaneurysms of the CFA[38,39], but there are few reports of treating visceral artery aneurysms and pseudoaneurysms, usually as second procedure after failed transarterial embolization[9,12-28].
In our case we attempted to identify angiographically the feeding vessel of the pseudoaneurysm, also replacing shape and type of the catheter and changing obliquity of the X-rays beam projection, but superselective catheterization of the feeding branch of the pseudoaneurysm failed.
After exclusion of open surgery approach for high risk-surgery patient, a non-vascular procedure was proposed, by means of percutaneous thrombin injection directly into the pseudoaneurysmal sac.
Thrombin is a clotting factor formed in coagulating form from prothrombin, which hydrolyzes bonds of fibrinogen and allows polymerization of the fibrinogen to form a fibrin clot. The commercially used product is a solution of a sterile protein substance that includes human fibrinogen and artificial aprotinine, which must be mixed with a human thrombin solution in the presence of calcium. After the injection, it acts immediately: the clot is bio-absorbable, and the risk of infection, tissue necrosis or inflammation is minimized.
The first report on the use of thrombin for percutaneous embolization of aneurysms of both peripheral and visceral arteries was in 1986 from Cope et al[12].
Afterwards this technique was applied to treat several visceral aneurysms and pseudoaneurysms, and type II and type I endoleak following endovascular repair of abdominal and thoracic aortic aneurysms. Potential complications of thrombin use are distal thrombosis, visceral artery occlusion and immunologic reactions[18]. Given the risk of distal embolization, the use of embolic protection device was suggested[28]. It is advised to evaluate the free flowing component of the total volume of the pseudoaneurysm, and the quantity of thrombin to prevent the leakage of thrombin from the sac[20].
The Table 1 presents an overview of the literature where peri-pancreatic pseudoaneurysms were treated by transabdominal thrombin injection US- or CT-guided, along with volume and type of the used thrombin, results, complications and follow up.
| Ref. | Patient age (yr) | Patient sex | Artery | No | Size (mm) | Technique | Needle | Thrombin | Dose (IU) | Immediate result | Adverse effects | Rebleeding | Retreatment | Follow-up (method) |
| Sparrow et al[18] | 50 | F | GDA | 1 | 30 | US-guided | 22 G | Bovine | 1000 | Success | No | No | No | 8 wk (US) |
| Manazer et al[19] | 42 | M | GDA | 1 | 30 × 30 | CT-guided | Not specified | Not specified | 4000 | Success | No | None | No | 10 wk (CT) |
| Armstrong et al[23] | Not available | Not available | SMA | 1 | Not available | US-guided | Not specified | Human | 750 | Success | Not available | Yes (two times in 6 mo) | Thrombin injection | 6 mo (CT) |
| Geoghegan et al[17] | 24 | M | GDA | 1 | 40 × 35 | CT-guided | 22 G | Not specified | Not specified | Success | Mild abdominal pain | No | No | 1 wk (CT) |
| Szopiński et al[24] | 49 | F | SMA | 1 | 60 × 44 × 45 | US-guided (after failed TCE) | Spinal needle | Bovine | 1600 | Success | No | No | No | 6 mo (US) |
| Ghassemi et al[26] | 77 | M | SPDA | 1 | 51 × 46 | CT-guided (after failed TCE) | 22 G | Not specified | 1300 | Success | No | No | No | 4 mo (CT) |
| Williams et al[25] | 55 | M | IPDA | 1 | 30 × 15 | CT-guided | 22 G | Bovine | 1000 | Success | No | No | No | 9 mo (CT) |
| McErlean et al[9] | 46 | M | GDA/PDA | 1 | 25 × 20 | US-guided | Not specified | Human | Not specified | Success | No | No | No | 3 mo (CT) |
| De Rosa et al[13] | Not specified | Not specified | GDA/SMA | 2 | Not specified | CT-guided (after failed TCE) | Not specified | Bovine | 4500 | Success | Not specified | Yes (24 h) | Not known | 15 d (death for PE) |
| De Rosa et al[13] | Not specified | Not specified | GDA/SMA | 1 | Not specified | US-guided | Not specified | Human | 400 | Success | Not specified | No | No | Not specified |
| Nicholson et al[15] | Not specified | Not specified | GDA/SMA | 4 | Not specified | CT-guided | Not specified | Not specified | Not specified | Success | Not specified | Yes (multiple) | Thrombin injection | 6 mo (with CT) |
| Laganà et al[14] | 69 | M | GDA | 1 | 50 | US-guided + coils | 22 G | Bovine | 2000 | Success | No | Yes (1 mo) | Coils | 24 mo |
| Fankhauser et al[16] | Not specified | Not specified | PDA | 2 | Not specified | US + fluoro-guided | Not specified | Not specified | Not specified | Success | Not specified | No | No | Unknown (mean 524 d) |
| Present Case Report | 82 | F | PDA | 1 | 20 | US-guided | 18 G | Human | 1000 | Success | No | No | No | 3 mo (US) |
In the majority of cases 1000-1500 IU of thrombin were injected into the pseudoaneurysmal sac and the human thrombin is today preferred to bovine thrombin for a minor risk of anaphylactic reaction. In one case additional use of coils was suggested for the embolisation of the afferent artery, to prevent the possible reperfusion of the pseudoaneurysm[14].
CT usually provides appropriate guide to percutaneous procedure, but US-guide allows real-time evaluation of the amount of thrombin being injected and of the patency of the pseudoaneurysmal sac. Furthermore US-guided injection allows real-time visualization of the needle track, lowing the risk of accidental puncture of bowel, vascular or organs.
Thrombin injection resulted in complete thrombosis and exclusion of the majority of the treated pseudoaneurysmal sacs, even during the follow up imaging control with US or CT scan, although the longest follow-up period was of 24 mo. There were not major complications referred to transabdominal access because of use of small calibre needles, except for our study in which we used an 18 G needle because only an 18 G US-guide was available in emergency. Table 1 shows important risk of early rebleeding of the treated pseudoaneurysm that required at least one additional thrombin injection, reported by some Authors[13-15,23]. These results indicate the importance of a close post-embolization follow-up with US or CT, required to identify high-risk patients, who need further treatment.
In conclusion, transabdominal thrombin injection could be the first line treatment when the incannulation or identification of the feeding vessel of peri-pancreatic pseudoaneurysm failed, especially in patients not candidate for open surgical approach[40]. Moreover, in these patients, this treatment could be considered as “bridge-to-surgery” allowing the stabilisation of the ruptured vessel and the further surgical treatment.
An 82-year-old woman with cerebral haemorrhage was admitted in emergency with the suspicion of acute bleeding.
Severe anaemia (haemoglobin drop to 6.0 g/dL) but haemodynamically stable.
Increasing of the cerebral haemorrhage, thoraco-abdominal source of bleeding.
Haemoglobin = 6.0 g/dL; haemodynamically stable.
Contrast-enhanced thoraco-abdominal computed tomography scan showed an oval, rounded mass of 2-cm on diameter within the pancreatic head with slow centrifugal contrast-enhancement, presumed to be a bleeding pseudoaneurysm with a haematoma and a small haemoperitoneum around the spleen.
Selective angiography of the superior mesenteric artery confirmed a pancreatico-duodenal artery pseudoaneurysm.
The patient was treated with 2 mL (1000 IU) of human thrombin percutaneously injected into the pseudoaneurysmal sac under ultrasonography (US) guide.
Few reports described peri-pancreatic pseudoaneurysms treated by percutaneous US-guided thrombin injection after failing of the endovascular treatment.
Pancreatico-duodenal artery pseudoaneurysm, or false aneurysm, is a vessel diameter dilatation without all vessel wall layers and is the consequence of a vessel wall disruption limited only by the adventitia or by the surrounding tissues.
Pancreatico-duodenal artery pseudoaneurysm embolization by percutaneous US-guided thrombin injection is feasible after failing of the endovascular treatment, especially in patients not candidate for open surgical approach.
This report describes a successful percutaneous US-guided treatment of the rare pancreatico-duodenal artery pseudoaneurysm after a failed endovascular approach.
P- Reviewer: Lin GM, Yamasaki T S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Uher P, Nyman U, Ivancev K, Lindh M. Aneurysms of the pancreaticoduodenal artery associated with occlusion of the celiac artery. Abdom Imaging. 1995;20:470-473. [PubMed] |
| 2. | Iyomasa S, Matsuzaki Y, Hiei K, Sakaguchi H, Matsunaga H, Yamaguchi Y. Pancreaticoduodenal artery aneurysm: a case report and review of the literature. J Vasc Surg. 1995;22:161-166. [PubMed] |
| 3. | Moore E, Matthews MR, Minion DJ, Quick R, Schwarcz TH, Loh FK, Endean ED. Surgical management of peripancreatic arterial aneurysms. J Vasc Surg. 2004;40:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radio Graphics. 2013;33:E71-E96. [RCA] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Stanley JC, Wakefield TW, Graham LM, Whitehouse WM, Zelenock GB, Lindenauer SM. Clinical importance and management of splanchnic artery aneurysms. J Vasc Surg. 1986;3:836-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Sutton D, Lawton G. Coeliac stenosis or occlusion with aneurysm of the collateral supply. Clin Radiol. 1973;24:49-53. [PubMed] |
| 7. | Kadir S, Athanasoulis CA, Yune HY, Wilkov H. Aneurysms of the pancreaticoduodenal arteries in association with celiac axis occlusion. Cardiovasc Radiol. 1978;1:173-177. [PubMed] |
| 8. | Trastek VF, Pairolero PC, Bernatz PE. Splenic artery aneurysms. World J Surg. 1985;9:378-383. [PubMed] |
| 9. | McErlean A, Looby S, Lee MJ. Percutaneous ultrasound-guided thrombin injection as first-line treatment of pancreatic pseudoaneurysm. Cardiovasc Intervent Radiol. 2007;30:526-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Spiliopoulos S, Sabharwal T, Karnabatidis D, Brountzos E, Katsanos K, Krokidis M, Gkoutzios P, Siablis D, Adam A. Endovascular treatment of visceral aneurysms and pseudoaneurysms: long-term outcomes from a multicenter European study. Cardiovasc Intervent Radiol. 2012;35:1315-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Sachdev U, Baril DT, Ellozy SH, Lookstein RA, Silverberg D, Jacobs TS, Carroccio A, Teodorescu VJ, Marin ML. Management of aneurysms involving branches of the celiac and superior mesenteric arteries: a comparison of surgical and endovascular therapy. J Vasc Surg. 2006;44:718-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 157] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Cope C, Zeit R. Coagulation of aneurysms by direct percutaneous thrombin injection. AJR Am J Roentgenol. 1986;147:383-387. [PubMed] |
| 13. | De Rosa A, Gomez D, Pollock JG, Bungay P, De Nunzio M, Hall RI, Thurley P. The radiological management of pseudoaneurysms complicating pancreatitis. JOP. 2012;13:660-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 14. | Laganà D, Carrafiello G, Mangini M, Dionigi G, Caronno R, Castelli P, Fugazzola C. Multimodal approach to endovascular treatment of visceral artery aneurysms and pseudoaneurysms. Eur J Radiol. 2006;59:104-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 15. | Nicholson AA, Patel J, McPherson S, Shaw DR, Kessel D. Endovascular treatment of visceral aneurysms associated with pancreatitis and a suggested classification with therapeutic implications. J Vasc Interv Radiol. 2006;17:1279-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Fankhauser GT, Stone WM, Naidu SG, Oderich GS, Ricotta JJ, Bjarnason H, Money SR. The minimally invasive management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2011;53:966-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 129] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 17. | Geoghegan T, Tuite D, McAuley G, O’Keeffe S, Torreggiani WC. Percutaneous thrombin injection for the treatment of a post-pancreatitis pseudoaneurysm of the gastroduodenal artery. Eur Radiol. 2004;14:2144-2145. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Sparrow P, Asquith J, Chalmers N. Ultrasonic-guided percutaneous injection of pancreatic pseudoaneurysm with thrombin. Cardiovasc Intervent Radiol. 2003;26:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Manazer JR, Monzon JR, Dietz PA, Moglia R, Gold M. Treatment of pancreatic pseudoaneurysm with percutaneous transabdominal thrombin injection. J Vasc Surg. 2003;38:600-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Puri S, Nicholson AA, Breen DJ. Percutaneous thrombin injection for the treatment of a post-pancreatitis pseudoaneurysm. Eur Radiol. 2003;13 Suppl 4:L79-L82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Huang IH, Zuckerman DA, Matthews JB. Occlusion of a giant splenic artery pseudoaneurysm with percutaneous thrombin-collagen injection. J Vasc Surg. 2004;40:574-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Luchs SG, Antonacci VP, Reid SK, Pagan-Marin H. Vascular and interventional case of the day. Pancreatic head pseudoaneurysm treated with percutaneous thrombin injection. AJR Am J Roentgenol. 1999;173:830, 833-834. [PubMed] |
| 23. | Armstrong EM, Edwards A, Kingsnorth AN, Freeman S, Roobottom CA. Ultrasound guided thrombin injection to treat a pseudoaneurysm secondary to chronic pancreatitis. Eur J Vasc Endovasc Surg. 2003;26:448-449. [PubMed] |
| 24. | Szopiński P, Ciostek P, Pleban E, Iwanowski J, Serafin-Król M, Marianowska A, Noszczyk W. Percutaneous thrombin injection to complete SMA pseudoaneurysm exclusion after failing of endograft placement. Cardiovasc Intervent Radiol. 2005;28:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Williams M, Alderson D, Virjee J, Callaway M. CT-guided percutaneous thrombin injection for treatment of an inferior pancreaticoduodenal artery pseudoaneurysm. Cardiovasc Intervent Radiol. 2006;29:669-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Ghassemi A, Javit D, Dillon EH. Thrombin injection of a pancreaticoduodenal artery pseudoaneurysm after failed attempts at transcatheter embolization. J Vasc Surg. 2006;43:618-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Wallace MJ, Choi E, McRae S, Madoff DC, Ahrar K, Pisters P. Superior mesenteric artery pseudoaneurysm following pancreaticoduodenectomy: management by endovascular stent-graft placement and transluminal thrombin injection. Cardiovasc Intervent Radiol. 2007;30:518-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Juszkat R, Krasiński Z, Wykrętowicz M, Staniszewski R, Majewski W. Transarterial thrombin injection secured with an embolic protection device as a treatment for a superior mesenteric artery pseudoaneurysm. Cardiovasc Intervent Radiol. 2011;34:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Kaufman JA, Lee MJ. Vascular and Interventional Radiology: The Requisites, 2nd ed. Philadelphia: Elsevier 2013; 229-264. |
| 30. | Pulli R, Dorigo W, Troisi N, Pratesi G, Innocenti AA, Pratesi C. Surgical treatment of visceral artery aneurysms: A 25-year experience. J Vasc Surg. 2008;48:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 229] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 31. | Ikeda O, Tamura Y, Nakasone Y, Iryou Y, Yamashita Y. Nonoperative management of unruptured visceral artery aneurysms: treatment by transcatheter coil embolization. J Vasc Surg. 2008;47:1212-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Balderi A, Antonietti A, Ferro L, Peano E, Pedrazzini F, Fonio P, Grosso M. Endovascular treatment of visceral artery aneurysms and pseudoaneurysms: our experience. Radiol Med. 2012;117:815-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45:276-283; discussion 283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 425] [Article Influence: 23.6] [Reference Citation Analysis (1)] |
| 34. | Flood K, Nicholson AA. Inferior pancreaticoduodenal artery aneurysms associated with occlusive lesions of the celiac axis: diagnosis, treatment options, outcomes, and review of the literature. Cardiovasc Intervent Radiol. 2013;36:578-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Jiménez AB, Herraez JG, Membrives PP, Girelli JH, Haurie G, Gòmez DD, Berta JE. Transcatheter embolization of a pancreatic pseudoaneurysm using a new liquid embolic agent, ethylene vinyl alcohol copolymer (onyx). Pancreas. 2009;38:110-112. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Balderi A, Antonietti A, Pedrazzini F, Ferro L, Leotta L, Peano E, Grosso M. Treatment of a hepatic artery aneurysm by endovascular exclusion using the multilayer cardiatis stent. Cardiovasc Intervent Radiol. 2010;33:1282-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Kalva SP, Athanasoulis CA, Greenfield AJ, Fan CM, Curvelo M, Waltman AC, Wicky S. Inferior pancreaticoduodenal artery aneurysms in association with celiac axis stenosis or occlusion. Eur J Vasc Endovasc Surg. 2007;33:670-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 38. | Kang SS, Labropoulos N, Mansour MA, Michelini M, Filliung D, Baubly MP, Baker WH. Expanded indications for ultrasound-guided thrombin injection of pseudoaneurysms. J Vasc Surg. 2000;31:289-298. [PubMed] |
| 39. | Elford J, Burrell C, Freeman S, Roobottom C. Human thrombin injection for the percutaneous treatment of iatrogenic pseudoaneurysms. Cardiovasc Intervent Radiol. 2002;25:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Kemmeter P, Bonnell B, VanderKolk W, Griggs T, VanErp J. Percutaneous thrombin injection of splanchnic artery aneurysms: two case reports. J Vasc Interv Radiol. 2000;11:469-472. [PubMed] |