Published online May 28, 2014. doi: 10.4329/wjr.v6.i5.210
Revised: April 17, 2014
Accepted: May 8, 2014
Published online: May 28, 2014
Processing time: 201 Days and 13.2 Hours
AIM: To investigate effect of body dimensions obtained from localizer radiograph and transverse abdominal computed tomography (CT) images on Size Specific Dose Estimate.
METHODS: This study was approved by Institutional Review Board and was compliant with Health Insurance Portability and Accountability Act. Fifty patients with abdominal CT examinations (58 ± 13 years, Male:Female 28:22) were included in this study. Anterior-posterior (AP) and lateral (Lat) diameters were measured at 5 cm intervals from the CT exam localizer radiograph (simple X-ray image acquired for planning the CT exam before starting the scan) and transverse CT images. Average of measured AP and Lat diameters, as well as maximum, minimum and mid location AP and Lat were measured on both image sets. In addition, off centering of patients from the gantry iso-center was calculated from the localizers. Conversion factors from American Association of Physicists in Medicine (AAPM) report 204 were obtained for AP, Lat, AP + Lat, and effective diameter (√ AP * Lat) to determine size specific dose estimate (SSDE) from the CT dose index volume (CTDIvol) recorded from the dose reports. Data were analyzed using SPSS v19.
RESULTS: Total number of 5376 measurements was done. In some patients entire body circumference was not covered on either projection radiograph or transverse CT images; hence accurate measurement of AP and Lat diameters was not possible in 11% (278/2488) of locations. Forty one patients were off-centered with mean of 1.9 ± 1.8 cm (range: 0.4-7 cm). Conversion factors for attained diameters were not listed on AAPM look-up tables in 3% (80/2488) of measurements. SSDE values were significantly different compared to CTDIvol, ranging from 32% lower to 74% greater than CTDIvol.
CONCLUSION: There is underestimation and overestimation of dose comparing SSDE values to CTDIvol. Localizer radiographs are associated with overestimation of patient size and therefore underestimation of SSDE.
Core tip: American Association of Physicists in Medicine (AAPM) report 204 has proposed a new method, “Size specific dose estimate” (SSDE) to represent more accurate estimations of patient doses. In this study we evaluated the feasibility of SSDE in clinical setting and figured out the shortcomings of the technique. We measured diameters in 50 patients at every 5 cm interval in addition to the maximum, minimum and mid-location on both localizer radiograph and transverse computed tomography (CT) images. SSDE values were calculated based on AAPM report look-up tables. Obtained SSDE values at each level were compared to each other as well as to CT dose index volume.
- Citation: Pourjabbar S, Singh S, Padole A, Saini A, Blake MA, Kalra MK. Size-specific dose estimates: Localizer or transverse abdominal computed tomography images? World J Radiol 2014; 6(5): 210-217
- URL: https://www.wjgnet.com/1949-8470/full/v6/i5/210.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i5.210
Traditionally surface or skin dose has been used for plain radiography[1]. For computed tomography (CT), since the X-rays are incident from 360° views, surface dose is not indicative of the highest absorbed dose[2,3]. Therefore, we rely on metrics for dose estimation such as CT dose index volume [CT dose index volume (CTDIvol), measured in mGy] and dose length product (DLP, mGy.cm). In order to monitor radiation doses, the International Electrochemical Commission[4] requires all scan manufacturers to display radiation output with descriptors such as CTDIvol and DLP before and after examination in the form of dose page or image[5-7].
One of the major limitations of CTDIvol is that it does not represent actual patient absorbed doses, as it does not take into account the heterogeneous attenuation and size of individual patients[8-10]. Recently, the American Association of Physicists in Medicine (AAPM) report 204[11], has proposed a new method, “size specific dose estimate” (SSDE) to represent more accurate estimations of patient doses. SSDE takes into account patient size in order to enable users to optimize CTDIvol based on patient’s physical dimensions[12-17]. Look-up tables of this report provide conversion factors that can be applied on CTDIvol to calculate SSDE for appropriate phantom sizes (16 and 32 cm). Conversion factors are based on 4 different measurements, anterior-posterior (AP), lateral (Lat), AP + Lat and effective diameter which can be measured from either localizer radiograph or transverse CT images. We hypothesize that there may be significant dose differences between CTDIvol and calculated SSDE and that the latter calculation may be significantly affected by the method of obtaining the patient dimensions. The purposes of this study were thus to compare CTDIvol and calculated SSDE and assess the effect of variations in adult patient dimensions obtained from localizer radiographs and transverse abdominal CT images on the calculation of SSDE for abdominal CT examinations.
None of the authors have any financial disclosures pertinent to this study. All the authors had complete unrestricted access to study data during the study.
Fifty patients undergoing “routine” abdominal CT examinations performed between 12/7/2011 and 12/9/2011 (age 58 ± 13 years female:male 22:28) were included in the study. Institutional Review Board waived the written consent for this retrospective study. In order to evaluate variability in physical dimensions, particularly for those heavy patients who may touch the display field of view, 25 consecutive patients were placed in weight groups of less than 90 kg (n = 25, female:male 15:10) and 90 kg or above (n = 25, female:male 7:18). These 50 abdominal CT examinations were scanned on 9 different scanners in our institution (GE LightSpeed 8, n = 10, LightSpeed VCT, n = 14, Discovery CT750 HD, n = 3, LightSpeed 16, n = 23). Patient demographic data (age, gender, weight) as well as scan parameters (tube current, noise index, tube voltage, pitch, gantry rotation time, slice thickness, increment, table speed and scan length) were tabulated for each patient. CTDIvol, DLP and phantom size was also recorded from the scanner dose report page.
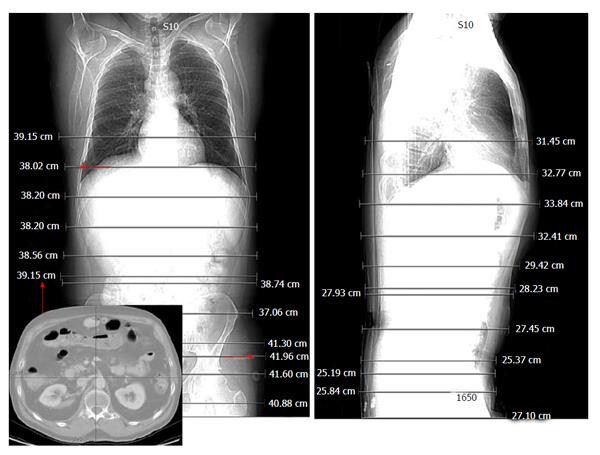
Digital Imaging and Communication in Medicine-format images were extracted from the hospital’s Picture Archiving and Communicating System (AGFA HealthCare) and available digital measurement calipers were used to obtain patient dimensions. As per the AAPM report 204 recommendations, AP and Lat diameters were measured on transverse CT images. AP was also measured from the lateral localizer radiograph at every 5 cm interval (along the z axis) from the start to the end of the scan length. Lat diameter was measured from the frontal localizer radiograph at every 5 cm interval. In addition, the maximum, minimum AP and Lat from the localizer radiographs as well as the mid-scan range location were measured (Figure 1). All of these measurements (that is, at 5 cm interval, maximum, minimum and mid location AP and Lat) were also measured on the transverse CT images. One of the study co-investigators (SP) measured all the diameters. Average of interval measurements was also calculated as an indicator of interval measurements. AP + Lat and effective diameter (√ AP * Lat) were calculated as stated by AAPM report 204[11].
We recorded the number of CT examinations without skin to skin coverage in the reconstructed field of view and performed similar measurements in the available field of view. In addition, vertical off centering of patients from the gantry iso-center was calculated from the lateral localizers. In centered patients gantry iso-center matches patient’s center. Gantry iso-center was determined as the midpoint of the field of view while patient’s center was determined as midpoint of maximum AP diameter. The distance between these two points was recorded as the off-centering estimation[18-21].
In order to estimate SSDE, conversion factors from look up tables of AAPM report No. 204 for 32 cm phantom size (same as recorded phantom size on our cases’ dose page report) were multiplied by CTDIvol. Since tables do not include diameters with decimals, all diameters with decimals were rounded to the nearest whole number. SSDE conversion factors for patient diameters not defined in the AAPM report number 204 were reported as missing (AP > 45 cm, Lat > 45 cm, AP + Lat > 90 cm, Effective diameter > 45 cm). In addition, SSDE values larger than 5 mGy were reported as rounded off integer number and for SSDE values less than 5 mGy only one decimal number was reported[11]. Furthermore, for comparison of manual measurements of physical dimensions and calculation of SSDE values, we also obtained SSDE values derived from automated radiation dose tracking software installed at our institute[22].
Four different study groups used different methods to develop a way to convert scanner CTDIvol to SSDE[11]. Two of them used physical measurements while the other two used Monte Carlo (MC) measurements. In MC measurement the probability of electron distribution and its behavior is evaluated mathematically[22-25]. The 1st group scanned 11 anthropomorphic phantoms, from newborn to adult size, on two scanners (GE Healthcare and Siemens Healthcare) and measured the radiation dose with ion chamber according to AAPM report 111[26]. The second group scanned standard cylindrical polymethylmethacrylate (PMMA) phantoms on 4 different scanners (GE HealthCare, Siemens HealthCare, Toshiba Medical and Philips HealthCare). They measured CTDIvol at different kV levels from 80 to 140 in 16-slice and 64-slice scanners. The third group stimulated abdominal CT scans on eight voxelized patient models with different sizes from newborn to large adult, and calculated organ specific doses via MC stimulation. Measured values were normalized according to CTDIvol and correlated to patients’ peripheral diameters at the central slice. The fourth group used the “Simple Investigative Environment for Radiological Research Applications” MC measurements to measure dose on cylinders with different components (water, PMMA, polyethylene) at various diameters and increments. Results from this multicenter study led to the introduction of look-up tables of conversion factors according to patients’ diameters. They recommended measuring the physical diameter of the patient at the scanner or post-scanning on transverse CT images or on the localizer radiograph and finding the suitable conversion factor out of the tables.
Data were analyzed with SPSS Statistical software (version 19, IBM, United States) and Microsoft EXCEL 2010 (Microsoft Inc., Redmond, Washington, United States). Student’s paired sample t-test was used to compare patient’s diameters derived from transverse CT and localizer radiographs as well as displayed CTDIvol and SSDE. Average diameter, AP + Lat and effective diameters, variations between patient diameters and SSDE values were calculated.
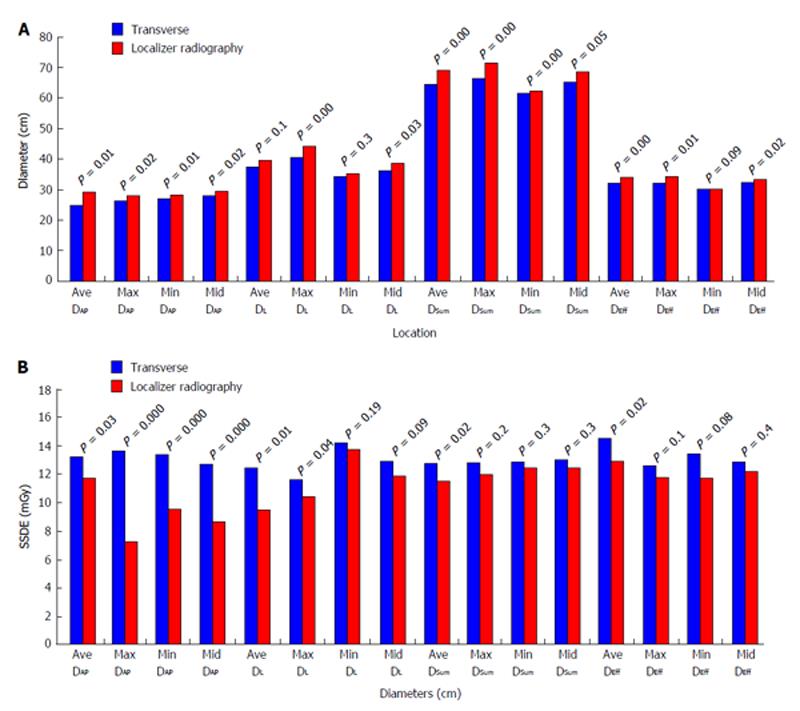
Number of 5 cm interval measurements was different among patients based on the scan length. A total of 5376 measurements were obtained, including interval measurements, maximum, minimum, mid-scan location and average of interval measurements on axial images and localizer radiograph. Details of this number of measurements are tabulated in Table 1 (Table 1 detailed legends: Number of interval measurements at each 5 cm was different among patients based on scan length. Total number of SSDE value is demonstrated on this table). Difference between measurements on localizer and transverse CT images for all values, including averages of interval measurements, maximum, minimum, and mid-scan location are illustrated in Figure 2A. Comparing localizer radiographs and transverse CT images, there was 5% difference between average of intervals of AP diameters (29.1 ± 4.7 cm vs 27.5 ± 3.8 cm, P = 0.01) and 5% difference at corresponding Lat diameters (localizer radiograph: 39.6 ± 5.5 cm and transverse: 37.4 ± 4.2 cm, P = 0.01).
| Number of patients | Number of intervals based on scan length + average of intervals, max, min, mid-scan length | Number of diameters (AP, Lat, AP + Lat, √ AP * Lat) on transverse images and localizer | Number of SSDE | Number of calculated SSDE in all patients |
| 4 | 8 + 4 | 96 | 96 | 384 |
| 24 | 9 + 4 | 104 | 104 | 2496 |
| 18 | 10 + 4 | 112 | 112 | 2016 |
| 4 | 11 + 4 | 120 | 120 | 480 |
| Total = 50 | Total = 5376 |
Differences in diameters in male and female as well as at different weight groups were tabulated in Table 2 (Table 2 detailed legends: Diameters were different between female and male as well as in patients less than 90 kg and higher than 90 kg. Average of intervals for each group is tabulated in the table.).
| AP (transverse images) | Lat (transverse images) | AP (localizer) | Lat (localizer) | |
| Female | 25.5 ± 3.6 (18.1-31.3) | 37.0 ± 4.5 (29.4-46.9) | 27.4 ± 4.6 (19.9-36.1) | 39.1 ± 5.6 (27.8-48.0) |
| Male | 28.2 ± 4.0 (23.0-40.9) | 37.7 ± 3.9 (30.1-46.2) | 30.4 ± 4.9 (22.7-46.2) | 40.0 ± 5.4 (29.2-49.8) |
| P value | < 0.0100 | 0.2000 | < 0.0100 | 0.2000 |
| < 90 kg | 24.4 ± 2.4 (18.1-29.9) | 34.4 ± 2.8 (28.8-40.7) | 26.0 ± 3.0 (18.1-32.9) | 36.0 ± 4.2 (27.8-46.6) |
| ≥ 90 kg | 29.7 ± 3.4 (26.0-40.8) | 39.6 ± 2.7 (35.7-44.9) | 32.3 ± 4.2 (27.0-48.7) | 42.4 ± 3.3 (35.5-46.2) |
| P value | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 |
In total, 11% (278/2488) of measured diameters were out of field of view. In 64% (32/50, female:male 18:14) of patients, skin-to-skin diameter were not visualized at some levels; Lat diameter on transverse CT and Lat diameter on the localizer radiograph had the highest number of incomplete skin to skin visualization. However, AP diameters of transverse CT images were visible skin-to-skin in all of the cases. Of the 32 patients with incomplete skin-skin diameters, 46% (15/32) were less than 90 kg (102/278 diameters) and 64% (17/32, 176/278 diameters) were more than 90 kg. In 10% of patients (5/50, female:male 2:3), Lat diameter of transverse CT was out of the field of view in the whole stack; four of these five patients weighted more than 90 kg. Also, in 4% (2/50) of patients, Lat diameter on localizer radiograph was not measurable as it was out of the field of view in the whole stack.
Forty one patients were off-centered from the gantry isocenter, with mean off-centering of 1.9 ± 1.8 cm (range: 0.4-7 cm). The average of intervals for AP and Lat diameters of localizer radiograph in patients with less than 2 cm off-centering and 2 or more than 2 cm off-centering was AP: 27.9 ± 3.8 and 30.5 ± 8.9 (P = 0.03) and Lat: 39.2 ± 4 and 40.6 ± 7.8 (P = 0.21), respectively.
Displayed CTDIvol for routine abdominal CT examinations was 12.0 ± 5.6 mGy. Females were scanned at lower CTDIvol of 10.8 ± 4 mGy than males at 13 ± 6.5 mGy (P < 0.001).
SSDE values were not calculated in 3% (80/2488) of measurements since conversion factors for the attained values were not listed on the look-up tables (AP > 45 cm, Lat > 45 cm, AP + Lat > 90 cm, Effective diameter > 45 cm). Regardless of the patient’s weight (less than 90 kg or more than 90 kg groups), SSDE measurements were different from displayed CTDIvol (P < 0.001).
Variations of SSDE values for each pair of measured diameters on transverse CT and localizer radiograph are illustrated in details in Figure 2A. There was no significant difference between SSDE values of AP + Lat and Effective diameters (min, max and mid scan length) taken out from transverse CT or localizer.
We evaluated the ratio of SSDE to displayed CTDIvol at some locations (average of intervals, maximum, minimum and mid-scan length) on both transverse images and localizer radiograph. This ratio was within 20% range except for minimum Lat diameter which the average was 26% ± 23% (Table 3) (Table 3 detailed legends: Extent of SSDE variations to displayed CTDIvol at maximum, minimum, average and mid location of localizer radiograph is shown in this table. Smallest mean variation noted at effective diameter which is from 0% to 12%. Largest mean variation is seen with antero-posterior diameter which is 21% less to 6% more. Table 3 detailed legends: Extent of SSDE variations to displayed CTDIvol at maximum, minimum average and mid location of transverse images is shown in this table. Smallest mean variation noted at effective diameter which is from 10% to 16%. Largest mean variation is seen with lateral diameter which is 8% to 31% more). SSDE values pertaining to AP + Lat and effective diameters of localizer radiograph had the least variation on average, maximum and minimum locations. However, SSDE derived from the localizer radiograph had the least fluctuations comparing to SSDE derived from transverse images. SSDE to CTDIvol ratio was 20% ± 21% (-30%, 68%) as calculated by the automated radiation dose software.
| DAP | DL | DSum | DEff | |||||
| Range | Mean | Range | Mean | Range | Mean | Range | Mean | |
| Localizer radiograph | ||||||||
| Average | 0.20, 0.46 | 0.06 ± 0.14 | -0.17, 0.55 | 0.12 ± 0.18 | -0.26, 0.50 | 0.04 ± 0.17 | -0.25, 0.47 | 0.04 ± 0.16 |
| Maximum | -0.32, 0.01 | -0.21 ± 0.08 | -0.13, 0.50 | 0.08 ± 0.17 | -0.28, 0.27 | 0.01 ± 0.16 | -0.30, 0.43 | 0.00 ± 0.16 |
| Minimum | -0.26, 0.11 | -0.11 ± 0.09 | -0.17, 0.65 | 0.26 ± 0.23 | -0.27, 0.26 | 0.03 ± 0.19 | -0.27, 0.59 | 0.04 ± 0.19 |
| Mid location | -0.30, 0.08 | -0.15 ± 0.10 | -0.17, 0.69 | 0.13 ± 0.23 | -0.22, 0.56 | 0.16 ± 0.23 | -0.20, 0.64 | 0.12 ± 0.17 |
| Transverse computed tomography images | ||||||||
| Average | -0.23, 0.59 | 0.13 ± 0.14 | -0.13, 0.50 | 0.15 ± 0.16 | -0.27, 0.50 | 0.11 ± 0.15 | -0.26, 0.53 | 0.11 ± 0.15 |
| Maximum | -0.25, 0.67 | 0.18 ± 0.19 | -0.13, 0.50 | 0.08 ± 0.16 | -0.17, 0.59 | 0.08 ± 0.15 | -0.29, 0.53 | 0.10 ± 0.17 |
| Minimum | -0.16, 0.66 | 0.13 ± 0.16 | -0.06, 0.70 | 0.31 ± 0.19 | -0.20, 0.61 | 0.11 ± 0.17 | -0.14, 0.59 | 0.16 ± 0.15 |
| Mid location | -0.25, 0.74 | -0.10 ± 0.17 | -0.17, 0.55 | 0.19 ± 0.20 | -0.12, 0.56 | 0.16 ± 0.14 | -0.19, 0.64 | 0.10 ± 0.23 |
A correlation between patient’s weight and average of intervals for AP and Lat diameter was found. The correlation was stronger with transverse CT diameters: Lat diameter (r2 = 0.89, P < 0.001) and AP diameter (r2 = 0.92, P < 0.001) in comparison to localizer radiograph: Lat diameter (r2 = 0.36, P < 0.01) and AP diameter (r2 = 0.93, P < 0.01).
We also found a correlation between patient’s weight and CTDIvol (r2 = 0.74, P < 0.01) as well as SSDE. SSDE values pertaining to AP, AP + Lat and effective diameters of transverse images showed (r2 = 0.6, P < 0.01) better correlation with patients’ weight.
Our study highlights a number of previously unreported aspects of adjusting or converting currently displayed scanner output radiation dose (CTDIvol) to patient SSDE with the use of patient’s measured diameter from CT images. For example, measurement of patient dimensions from localizer radiographs and transverse CT images provide substantially different values, with overestimation of both AP and Lat diameter on localizer radiographs compared to the transverse CT images. Both anterior-posterior and lateral localizer radiographs are associated with similar extent of overestimation of AP and Lat diameter. This overestimation of patient diameters on localizer radiograph is seen in all patients regardless of their size and gender or location of measurement of these diameters along the scan length. We believe that this overestimation of patient size on localizer radiograph likely stems from image magnification with the two dimensional projection based localizer radiographs similar to magnification noted in conventional radiography as well. Since the extent of image magnification with localizer radiograph depends on the patient size, direction of the projection radiograph and patient centering in the gantry iso-center, a constant conversion factor to adjust for this magnification is unlikely to work in all circumstances.
Due to this overestimation of AP and Lat diameter obtained from localizer radiograph, there is significant underestimation of SSDE when localizer radiograph based measurements of patient size are used compared to the transverse CT images. Thus, AP and Lat diameter should be measured from transverse CT images in order to avoid underestimation of SSDE.
However, there are also some concerns with the use of transverse CT images over localizer radiographs. As noted in our study, in almost 10% of CT examinations, transverse CT images did not include skin to skin coverage of the body region in the reconstructed field of view, which precludes precise measurement of patient diameter. Indeed, lack of skin to skin coverage in the field of view of transverse CT images is not uncommon in routine clinical practice. Contrary to underestimation of SSDE noted with localizer radiographs, measurement of AP and Lat diameter from cropped transverse CT images will lead to underestimation of these measurements and overestimation of SSDE from the look up tables.
There are several implications of our study. Firstly, transverse CT images should be preferred over the localizer radiographs for measurement of patient size since the latter are associated with overestimation of patient size and therefore underestimation of SSDE.
Secondly, since there is similar fluctuation in SSDE with the use of average, mid-location or minimum and maximum diameters measurement of patient size from mid slice location is perhaps the most convenient and least subjective location. Thirdly, when transverse CT images do not include skin to skin coverage, there is inadequate measurement of patient size which leads to overestimation of SSDE.
To address this issue, technologists or radiologists should reconstruct at least one transverse CT image, preferably at the mid slice location with skin to skin coverage of the patient. This however, may not be possible in a very large patient, for example with a greater than 50 cm diameter (as this is the limit of the reconstructed scan field of view in many scanners) as well as in patients who are not or cannot be centered properly in the gantry iso-center.
Fourthly, our study points to a strong and statistically significant positive correlation between both AP and Lat diameters measured from the transverse CT images and patients’ weights (r2 = 0.89-0.92, P < 0.001). This suggests the possibility of using patient weight in addition to or in lieu of patient diameters to estimate SSDE when dimensions are either not available or not feasible (for example, not included in the reconstructed field of view). Although not proven or specifically addressed in our study, we postulate that the use of patient weight in lieu of patient diameter may actually provide a more accurate SSDE compared to patient diameter in patients with complex deformities or an asymmetric chest or abdomen (as in severe or complex chest wall or spinal deformities). Fifthly, despite concerns regarding measurement of patient diameters from both localizer radiographs and transverse CT images, our study points to considerable potential underestimation (32%) and overestimation (74%) of dose from CTDIvol, which is corrected for by estimation of SSDE and which far exceeds up to 5% fluctuations in estimation of patient diameters. Therefore, we strongly recommend the use of SSDE for normalizing CTDIvol according to patient size.
There are limitations in our study. Our sample size was small. Only adult subjects were evaluated and pediatric patients were not included. Therefore, results of our study may not apply to smaller pediatric patients. This study was performed in one CT center and may not reflect the practice of acquisition of transverse CT images in other centers. We did not assess the effect of complex patient morphology (severe or complex chest wall or spinal deformities) on the feasibility of measuring patient diameters, when non-lateral and non-anterior-posterior diameters might be a more accurate representation of patient’s maximum and minimum diameters. Our study did not assess inter-observer or intra-observer variations in measurement of patient diameters and their effects on estimation of SSDE. However, software based estimation of patient diameter is commercially available which should address any non systematic human errors in measurements of these diameters[22].
In conclusion, the use of SSDE helps convert CTDIvol into more patient size specific radiation dose. Transverse CT images should be used to estimate patient size since localizer radiographs generally overestimate patient size due to magnification. Measurement of patient size can be obtained from the mid-slice location on the transverse CT image series.
Size specific dose estimate is recently introduced by American Association of Physicists in Medicine in order to better estimate the patients’ radiation exposure from computed tomography (CT) exams. Measured diameters of patients are used to adjust the scanner displayed CT dose index volume (CTDIvol) to size specific dose estimate (SSDE).
There is no accurate means of measuring radiation exposure to patients from CT exams. Hence it is essential to work on and refine current methods.
In this study the authors aimed to assess the feasibility of the newly suggested method in daily clinical practice and on human bodies.
Result of this study explains that it is not always possible to get the accurate diameter from CT images. So it is prudent to have a standardize measure that has the least fluctuation in values.
SSDE in mGy unit is the adjusted CTDIvol according to patients’ diameters.
This is a well-designed and-written manuscript. The results of the manuscript are important for current radiology literature and will be an inspirational tool for future researches on this topic.
P- Reviewers: Battal B, Bernardin L, Ciledag N S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | George J, Eatough JP, Mountford PJ, Koller CJ, Oxtoby J, Frain G. Patient dose optimization in plain radiography based on standard exposure factors. Br J Radiol. 2004;77:858-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Pooley RA, McKinney JM, Miller DA. The AAPM/RSNA physics tutorial for residents: digital fluoroscopy. Radiographics. 2001;21:521-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Report of AAPM Task Group 23: CT Dosimetry. The Measurement, Reporting and Management of Radiation Dose in CT. Accessed on 25th March 2014. Available from: http: //www.aapm.org/pubs/reports/rpt_96.pdf. |
| 4. | Evaluation and routine testing in medical imaging departments Part 26: Constancy tests imaging performance of computed tomography X-ray equipment. IEC 61223-2-6 ed2.0. . |
| 5. | Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, Saini S. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-628. [PubMed] |
| 6. | Duan X, McCollough C. Risks, benefits, and risk reduction strategies in thoracic CT imaging. Semin Respir Crit Care Med. 2014;35:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | McCollough CH, Primak AN, Braun N, Kofler J, Yu L, Christner J. Strategies for reducing radiation dose in CT. Radiol Clin North Am. 2009;47:27-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 656] [Cited by in RCA: 540] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 8. | Huda W, Scalzetti EM, Roskopf M. Effective doses to patients undergoing thoracic computed tomography examinations. Med Phys. 2000;27:838-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 104] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | McCollough CH, Leng S, Yu L, Cody DD, Boone JM, McNitt-Gray MF. CT dose index and patient dose: they are not the same thing. Radiology. 2011;259:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 309] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 10. | Li X, Samei E, Williams CH, Segars WP, Tward DJ, Miller MI, Ratnanather JT, Paulson EK, Frush DP. Effects of protocol and obesity on dose conversion factors in adult body CT. Med Phys. 2012;39:6550-6571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Report of AAPM Task Group 204. Size-Specific Dose Estimates (SSDE) in Pediatric and Adult Body CT Examinations. Accessed on 14th February 2013. Available from: http: //www.aapm.org/pubs/reports/. |
| 12. | Westra SJ, Li X, Gulati K, Singh S, Liu B, Kalra MK, Abbara S. Entrance skin dosimetry and size-specific dose estimate from pediatric chest CTA. J Cardiovasc Comput Tomogr. 2014;8:97-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Khatonabadi M, Kim HJ, Lu P, McMillan KL, Cagnon CH, DeMarco JJ, McNitt-Gray MF. The feasibility of a regional CTDIvol to estimate organ dose from tube current modulated CT exams. Med Phys. 2013;40:051903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Wang J, Christner JA, Duan X, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size specific dose estimation in CT. Part II. Implementation on abdomen and thorax phantoms using cross sectional CT images and scanned projection radiograph images. Med Phys. 2012;39:6772-6778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Wang J, Duan X, Christner JA, Leng S, Yu L, McCollough CH. Attenuation-based estimation of patient size for the purpose of size specific dose estimation in CT. Part I. Development and validation of methods using the CT image. Med Phys. 2012;39:6764-6771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Brady SL, Kaufman RA. Investigation of American Association of Physicists in Medicine Report 204 size-specific dose estimates for pediatric CT implementation. Radiology. 2012;265:832-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 17. | Christner JA, Braun NN, Jacobsen MC, Carter RE, Kofler JM, McCollough CH. Size-specific dose estimates for adult patients at CT of the torso. Radiology. 2012;265:841-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 150] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 18. | Kim MS, Singh S, Halpern E, Saini S, Kalra MK. Ablation margin assessment of liver tumors with intravenous contrast-enhanced C-arm computed tomography. World J Radiol. 2012;4:102-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Li J, Udayasankar UK, Toth TL, Seamans J, Small WC, Kalra MK. Automatic patient centering for MDCT: effect on radiation dose. AJR Am J Roentgenol. 2007;188:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 142] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Matsubara K, Koshida K, Ichikawa K, Suzuki M, Takata T, Yamamoto T, Matsui O. Misoperation of CT automatic tube current modulation systems with inappropriate patient centering: phantom studies. AJR Am J Roentgenol. 2009;192:862-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Gudjonsdottir J, Svensson JR, Campling S, Brennan PC, Jonsdottir B. Efficient use of automatic exposure control systems in computed tomography requires correct patient positioning. Acta Radiol. 2009;50:1035-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Gudjonsdottir J; eXposure™. Accessed on 15th February 2013. Available from: http: //www.radimetrics.com/default/?page_id=1325. |
| 23. | Turner AC, Zhang D, Khatonabadi M, Zankl M, DeMarco JJ, Cagnon CH, Cody DD, Stevens DM, McCollough CH, McNitt-Gray MF. The feasibility of patient size-corrected, scanner-independent organ dose estimates for abdominal CT exams. Med Phys. 2011;38:820-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 24. | Turner AC, Zankl M, DeMarco JJ, Cagnon CH, Zhang D, Angel E, Cody DD, Stevens DM, McCollough CH, McNitt-Gray MF. The feasibility of a scanner-independent technique to estimate organ dose from MDCT scans: using CTDIvol to account for differences between scanners. Med Phys. 2010;37:1816-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | DeMarco JJ, Cagnon CH, Cody DD, Stevens DM, McCollough CH, O’Daniel J, McNitt-Gray MF. A Monte Carlo based method to estimate radiation dose from multidetector CT (MDCT): cylindrical and anthropomorphic phantoms. Phys Med Biol. 2005;50:3989-4004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 116] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 26. | Report of AAPM Task Group 111: The Future of CT Dosimetry. Comprehensive Methodology for the Evaluation of Radiation Dose in X-Ray Computed Tomography. Accessed on 14th February 2013. Available from: http: //www.aapm.org/pubs/reports/. |