Published online Dec 28, 2014. doi: 10.4329/wjr.v6.i12.924
Revised: October 4, 2014
Accepted: November 7, 2014
Published online: December 28, 2014
Processing time: 163 Days and 11.5 Hours
Traumatic injuries of the carotid artery may result in severe morbidity and mortality. The most common location of carotid artery injury is the cavernous segment, which may result in fistulous connection to the cavernous sinus and ophthalmic veins, which in turn lead to pressure symptoms in the ipsilateral orbit. Unlike the commonly reported direct traumatic carotid-cavernous fistula, we describe an unusual case of a 38-year-old man presented with a traumatic brain injury led to a fistula connection between the cavernous carotid artery and the ipsilateral basal vein of Rosenthal, with eventual drainage to the straight and transverse sinuses. The basal vein of Rosenthal is usually formed from confluence of anterior and middle cerebral veins deep in the Sylvian fissure and drain the insular cortex and the cerebral peduncles to the vein of Galen. Immediate endovascular deployment of a covered stent in the cavernous carotid artery allowed sealing the laceration site. Three months follow up showed a non-focal neurological examination and healed carotid laceration over the covered stent.
Core tip: Most carotid-cavernous fistulae lead to pressure symptoms in the orbit. This case report suggests alternate routing to the basal vein of Rosenthal, which may convey different implications. Various treatment options used for conventional fistulae; though, in this report we highlight the utility of a covered stent system (Jostent Graftmaster) in the management of carotid-rosenthal fistula.
- Citation: Allam H, Callison RC, Scodary D, Alawi A, Hogan DW, Alshekhlee A. Traumatic carotid-rosenthal fistula treated with Jostent Graftmaster. World J Radiol 2014; 6(12): 924-927
- URL: https://www.wjgnet.com/1949-8470/full/v6/i12/924.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i12.924
Blunt craniocervical vascular injuries are uncommon with estimated incidence of 1.1%-2.7% in a screened blunt head trauma population[1]. The prevalence of carotid injury with skull base fracture is 2%, which appear more common in females[2]. Most commonly reported location of the fistulous connection is between the cavernous carotid artery (CCA) and the cavernous sinus resulting in direct and less commonly indirect carotid-cavernous fistulae[3]. The cavernous sinus drains anteriorly to the ophthalmic vein and thus, most of these fistulae result into pressure symptoms in the ipsilateral orbit. Though less frequently, injury to the CCA may lead to intracerebral and subarachnoid hemorrhages. Injury to the CCA with fistulous connection to deep cerebral vein is more complex and has not been reported. We present a case of traumatic laceration of the CCA with fistulous connection to the basal vein of Rosenthal following a traumatic brain injury with basilar skull fracture and traumatic subarachnoid hemorrhage. We discuss treatment options including a covered stent placement to seal the carotid laceration.
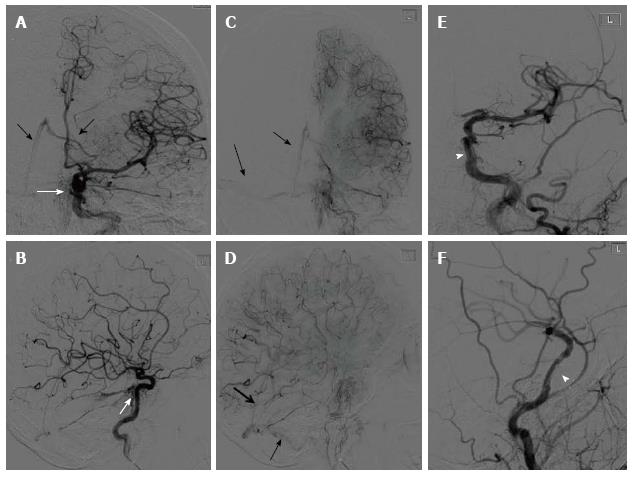
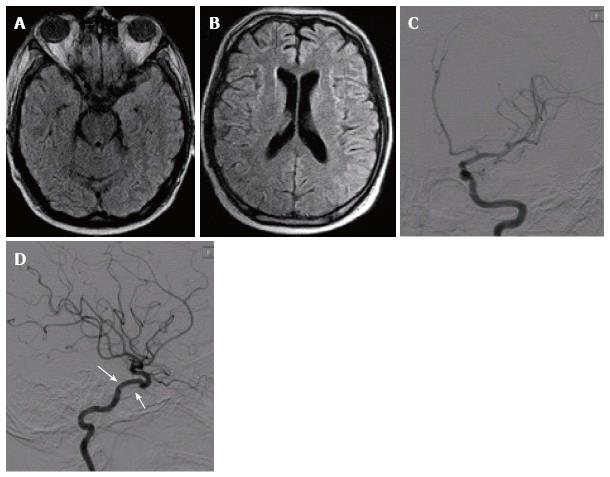
A 38-year-old man with a known history of epilepsy presented to the emergency department after falling off a motorized bicycle resulting in multiple facial and skull base fractures. On admission, he was awake and alert with initial Glasgow Coma Scale of 14 that rapidly decline to 4; he required sedation and emergent endotracheal intubation. Immediate cranial computed tomography showed multiple fractures in the face and skull base with Fisher grade IV subarachnoid hemorrhage and evidence of air at the skull base. Emergent 6-vessel cerebral angiogram revealed contrast extravasation at the cavernous segment of the left CCA (Figure 1A and B). The blood leakage pointed medially and posteriorly with evidence of early venous filling in basal vein of Rosenthal, straight and transverse dural sinuses (Figure 1B, C and D). Decision to sacrifice the left internal carotid artery was halted by the poor collateral supply with balloon test occlusion. Transvenous obliteration of the straight sinuses and deep cerebral veins carry a high risk of thalamic and peduncular infarction and death[4]. Therefore, a transarterial covered Jostent Graftmaster (Abbott Vascular) deployment across the lacerated cavernous segment of the ICA was performed. The operation performed through a 7 French 90 cm Cook shuttle sheath guiding system that was positioned in the distal left common carotid artery. A Transend EX microwire (300 cm) was advanced in the M2 segment of the left middle cerebral artery using an exchange method. A balloon mounted 3.5 mm × 16 mm Jostent Graftmaster was navigated over the Transend EX microwire into the left cavernous carotid segment. The stent was then deployed by balloon inflation to the recommended nominal pressure. Control angiography showed a decreased contrast extravasation from the lacerated segment (Figure 1E and F). The procedure was followed by immediate oral loading dose of Clopidogrel (300 mg) via a nasogastric tube. He was maintained on a daily aspirin (325 mg) and Clopidogrel (75 mg) throughout the hospital course and after discharge. He was closely monitored for vasospasms during the hospital stay with serial transcranial Doppler studies. He remained in coma for a few days with neurological examination showing response to pain in all extremities and reactive pupils. Mental state continued to improve and he made it to a full mental recovery after 14 d and he was then discharged to acute rehabilitation center. After 3 mo, his neurological examination was normal, follow-up angiography showed no contrast extravasation, in-stent thrombosis, or stent migration; and brain MRI failed to show any ischemic changes (Figure 2).
The major deep cerebral veins include the internal cerebral vein and basal vein of Rosenthal. Both of these veins are paired and large, and they drain towards the great cerebral vein of Galen. In addition, the vein of Galen receives tributaries from a pair of internal occipital veins and drain into the straight sinus. The basal vein of Rosenthal is formed from confluence of anterior and middle cerebral veins deep in the Sylvian fissure and drain the insular cortex and the cerebral peduncles. After receiving the tributaries, basal vein of Rosenthal courses posteriorly around the cerebral peduncles to the vein of Galen. The basal vein of Rosenthal is identified angiographically by a small deflection when it crosses the cerebral peduncles (Figure 1B). Unlike the anterior laceration in the CCA which usually leads to pressure symptoms in the orbit, posterior carotid laceration may lead to subarachnoid hemorrhage and death. To approach the CCA, craniotomy through the cavernous sinus to trap the fistula is technically difficult and usually reserved for cases when endovascular approach fails to seal the laceration[5,6]. Thus, we opted to pursue the deployment of a covered stent system to seal the laceration. The Jostent Graftmaster is approved for epicardial coronary artery pseudo-aneurysms and perforation[7]. They are used with variable success in the treatment of pseudo-aneurysms and post traumatic carotid cavernous fistulae[8-10]. The Jostent Graftmaster consists of a single expanded polytetrafluoroethylene layer sandwiched between two coaxial stainless steel slotted tubes that is balloon-expandable (Abbott Vascular). The rigid framework of these stents occasionally prohibits safe navigation within tortuous cerebrovascular anatomy. Therefore, covered stents are not always technically feasible, and if force used for navigation, it may lead to unintended complications such as dissection or spasm of small cerebral vessels. Moreover, covered stents are more thrombogenic compared to other stents; thus, dual antiplatelet therapy was administered in our patient despite the initial hemorrhagic presentation. Despite the risks, covered stent remains an option to treat CCA laceration with fistulous connection to deep cerebral veins.
A 38-year-old man presented with traumatic subarachnoid hemorrhage.
Rapid decline in Glasgow Coma Scale from 14 to 4 required sedation and emergent endotracheal intubation. Computed tomography (CT) imaging confirmed the diagnosis of subarachnoid hemorrhage with fracture at the skull base.
Ruptured cerebral aneurysm, traumatic dissection or laceration of a cerebral vessel.
All laboratory data including blood count, metabolic panel and liver function test were within normal limits.
CT imaging confirmed the presence of blood in the subarachnoid space along with fracture at the skull base. Cerebral angiography showed laceration and contrast extravasation in the posterior head region with evidence of fistulous connection to the basal vein of Rosenthal.
Traumatic carotid-rosenthal fistula.
Endovascular implantation of a covered stent (Jostent Graftmaster) across the lacerated segment of the cavernous carotid artery.
No previous report of a similar fistulous connection between the cavernous carotid artery and the basal vein of Rosenthal. However, a few case reports using the covered stent in the treatment of conventional carotid-cavernous fistulae.
Posterior laceration of cavernous carotid artery may lead to subarachnoid hemorrhage and possible connection to the basal venous drainage. This complication has different implication compared to anterior laceration of the cavernous carotid artery.
This case report highlights the importance of identifying the fistulous connection in the venous brain drainage. In addition, the case suggests that a covered Jostent Graftmaster is a treatment option to seal vessel laceration in life threatening hemorrhage.
Nice case report, well written and concise.
P- Reviewer: Cuellar H, Goktay AY, Latsios G, Rodriguez GJ, van Rooij WJ S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Sliker CW. Blunt cerebrovascular injuries: imaging with multidetector CT angiography. Radiographics. 2008;28:1689-1708; discussion 1709-1710. [PubMed] |
| 2. | Sun GH, Shoman NM, Samy RN, Pensak ML. Analysis of carotid artery injury in patients with basilar skull fractures. Otol Neurotol. 2011;32:882-886. [PubMed] |
| 3. | Ellis JA, Goldstein H, Connolly ES, Meyers PM. Carotid-cavernous fistulas. Neurosurg Focus. 2012;32:E9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 199] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 4. | Crawford SC, Digre KB, Palmer CA, Bell DA, Osborn AG. Thrombosis of the deep venous drainage of the brain in adults. Analysis of seven cases with review of the literature. Arch Neurol. 1995;52:1101-1108. [PubMed] |
| 5. | Gemmete JJ, Chaudhary N, Pandey A, Ansari S. Treatment of carotid cavernous fistulas. Curr Treat Options Neurol. 2010;12:43-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | van Loveren HR, Keller JT, el-Kalliny M, Scodary DJ, Tew JM. The Dolenc technique for cavernous sinus exploration (cadaveric prosection). Technical note. J Neurosurg. 1991;74:837-844. [PubMed] |
| 7. | Lansky AJ, Yang YM, Khan Y, Costa RA, Pietras C, Tsuchiya Y, Cristea E, Collins M, Mehran R, Dangas GD. Treatment of coronary artery perforations complicating percutaneous coronary intervention with a polytetrafluoroethylene-covered stent graft. Am J Cardiol. 2006;98:370-374. [PubMed] |
| 8. | Kalia JS, Niu T, Zaidat OO. The use of a covered stent graft for obliteration of high-flow carotid cavernous fistula presenting with life-threatening epistaxis. J Neurointerv Surg. 2009;1:142-145. [PubMed] |
| 9. | Wang C, Xie X, You C, Zhang C, Cheng M, He M, Sun H, Mao B. Placement of covered stents for the treatment of direct carotid cavernous fistulas. AJNR Am J Neuroradiol. 2009;30:1342-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Wang YL, Ma J, Li YD, Ding PX, Han XW, Wu G. Application of the Willis covered stent for the management of posttraumatic carotid-cavernous fistulas: an initial clinical study. Neurol India. 2012;60:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |