Published online Aug 28, 2013. doi: 10.4329/wjr.v5.i8.325
Revised: June 9, 2013
Accepted: July 18, 2013
Published online: August 28, 2013
Processing time: 138 Days and 11.3 Hours
We are the first to report a case that showed spontaneous resolution of epidural hematoma which was related to a steroid-induced osteoporotic compression fracture. The patient had a painful fracture with an intravertebral cleft at L1 accompanying an epidural hematoma posteriorly. Immediate pain relief was achieved after percutaneous vertebroplasty. Complete resolution of hematoma was noted three months after procedure. We theorized that intravertebral stability after treatment might have played a role in this patient.
Core tip: We are the first to report a case treated with PVP that showed spontaneous resolution of epidural hematoma related to a compression fracture with an intravertebral cleft, resulting in an amelioration of spinal canal compromise. We theorized that intravertebral stability after PVP might have played a role in this patient.
- Citation: Hirata H, Hiwatashi A, Yoshiura T, Togao O, Yamashita K, Kamano H, Kikuchi K, Honda H. Resolution of epidural hematoma related to osteoporotic fracture after percutaneous vertebroplasty. World J Radiol 2013; 5(8): 325-327
- URL: https://www.wjgnet.com/1949-8470/full/v5/i8/325.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i8.325
Percutaneous vertebroplasty (PVP) is a minimally invasive and widespread procedure that provides pain relief and stability for osteoporotic compression fractures refractory to conservative therapy[1]. Presence of spinal canal compromise is considered as a relative contraindication for PVP according to the American College of Radiology (ACR) Practice Guideline[1], because spinal cord compression after treatment has been reported[2]. However, there have been reports that PVP can be performed safely in patients with spinal canal compromise by using careful cement injection[3-5]. In these cases, epidural hematoma (EDH) as a cause of spinal canal compromise has been rarely reported. Although Singh et al[5] have reported a case with spinal canal compromise secondary to EDH from an osteoporotic compression fracture; they did not describe the changes in the EDH after the procedure, or the long-term follow-up results. Herein we report a case with complete spontaneous resolution of EDH related to a compression fracture with an intravertebral cleft after PVP.
A 73-year-old woman with a history of 17-year history of steroid use for multiple sclerosis presented at our institution with low back pain [visual analog scale (VAS) = 4]. Two months before presentation, she had been diagnosed with a compression fracture at L1 because of a fall. The pain had been refractory to conservative treatment with a corset and analgesics. The patient had a long history of weakness and hyperreflexia of the lower extremities and blurred vision associated with multiple sclerosis. The patient showed severe secondary osteoporosis on admission (T-score of -3.6 at the neck of the femur).
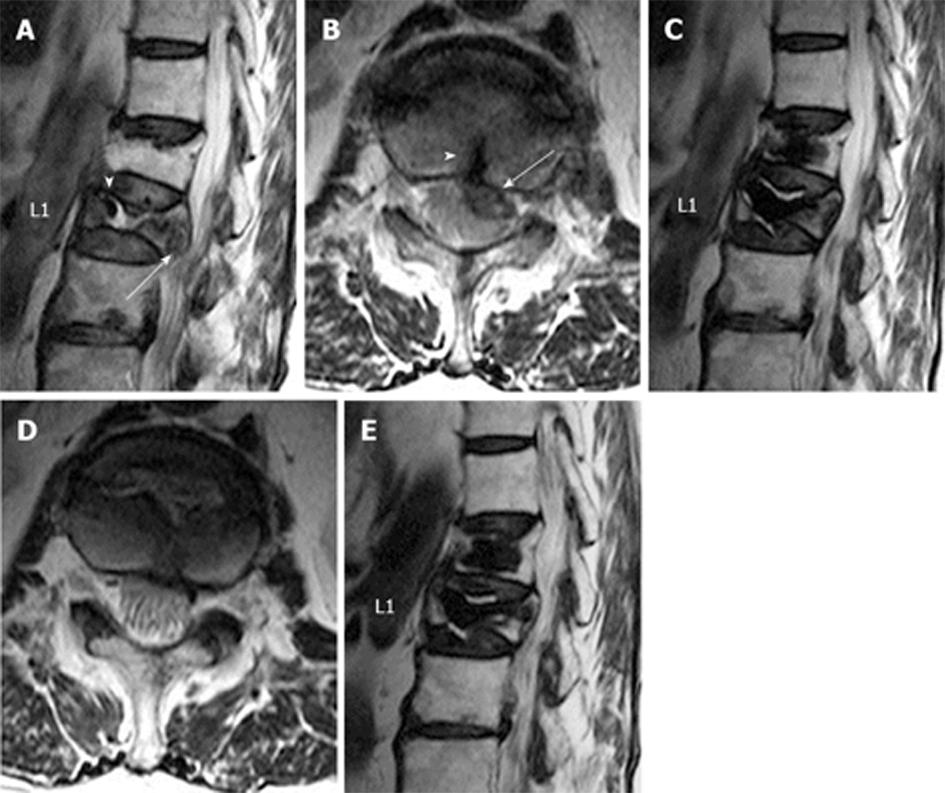
Preoperative magnetic resonance (MR) images showed an unhealed compression fracture at L1 with an intravertebral cleft. T2-weighted images showed a hypointense structure in the anterior aspect of the thecal sac at L1 (Figure 1A and B). This structure was hyperdense on computed tomography and slightly hyperintense on T1-weighted images (not shown). Postcontrast fat-suppressed T1-weighted images showed no enhancement in the epidural component, while there was contrast enhancement at L1 vertebral body (not shown). There is a fracture line connecting an intravertebral cleft and this structure, likely representing an EDH. There was also a chronic compression fracture at T12.
PVP at L1 was performed through a bipedicular approach with 11-gauge bone biopsy needles. Polymethylmethacrylate with barium sulfate was injected under biplane fluoroscopic guidance. Care was taken that extravasation into the epidural space did not occur. Prophylactic treatment at T12 was also performed in consideration of the risk of subsequent fracture in this patient[6-9]. The total amounts of cement injected were 6.0 mL at L1 and 4.0 mL at T12. There was no neurological deficit during or after the procedure. The patient reported immediate pain relief (VAS = 2). Postoperative MR images obtained immediately after the treatment showed that the intravertebral cleft at L1 was filled with cement without cement leakage into the spinal canal. There was no increase in size of the EDH or worsening of spinal stenosis. Follow-up MR images obtained 3 mo after the treatment revealed complete resolution of the EDH and amelioration of the spinal canal compromise (Figure 1C and D). At that time, the patient had no pain and did not require analgesics (VAS = 0). Postoperative images obtained three years after the treatment showed maintenance of the spinal canal without subsequent compression fracture (Figure 1E). She has been free of pain without any new neurological deficits for 3 years.
To the best of our knowledge, we are the first to report a case treated with PVP that showed spontaneous resolution of EDH related to a compression fracture with an intravertebral cleft, resulting in an amelioration of spinal canal compromise. Spinal canal compromise after PVP is a well-known complication. According to the ACR Practice Guideline[1], the presence of spinal canal compromise is a relative contraindication for PVP because of a risk of spinal cord compression after the procedure[2]. However, recent reports have suggested that PVP can be performed for fractures with spinal canal compromise caused by retropulsion of fractured bone fragments[3,4]. Hiwatashi et al[3] have evaluated the size of the spinal canal and the degree of retropulsion of fractured bone fragments in vertebrae with spinal canal compromise before and after treatment. They have reported that the size of the spinal canal was maintained a year after the procedure. Singh et al[5] have reported a case of PVP used to treat osteoporotic compression fracture with spinal canal compromise caused by stable EDH. However, the EDH in their case was located posterior to the thecal sac, which was a different location from our case. Furthermore, they did not describe the changes of the hematoma after the procedure.
Previous reports described spontaneous resolution of acute spinal EDH with conservative treatment[10]. In our case, there was an EDH related to an intravertebral cleft two months after the occurrence of fracture. Because of the presence of the fracture line between the intravertebral clef and the EDH, we theorized that the instability of the fracture was a cause of hematoma. This continuous instability might have prevented the spontaneous resolution of hematoma. Although there was no control, the stabilization after successful PVP may have contributed to the spontaneous resolution of hematoma.
The efficacy of prophylactic PVP is a matter of controversy. Based on the ACR Practice Guideline, prophylactic PVP is contraindicated except for research purposes[1]. However, Kobayashi et al have reported prophylactic PVP could prevent the subsequent fractures[6]. Previous studies have reported that steroid use[7], and the presence of an intravertebral cleft[8] are causes of subsequent fractures. In addition, Trout et al[9] have reported that subsequent fractures are often seen above the cemented vertebrae. Because the present patient developed no new fracture over the three-year follow-up, the prophylactic treatment in this particular patient with high risk of compression fracture was considered beneficial.
In conclusion, we are the first to report a case treated with PVP that showed spontaneous resolution of EDH related to a compression fracture with an intravertebral cleft. We theorized that intravertebral stability after PVP might have played a role in this patient.
P- Reviewer Epstein LJ S- Editor Zhai HH L- Editor A E- Editor Liu XM
| 1. | American College of Radiology. ACR–ASNR–ASSR–SIR–SNIS Practice guideline for the performance of vertebral augmentation. ACR Practice Guideline. 2012; Available from: http://www.acr.org/~/media/0AB72B20B91D4571A262BE946E889DC3.pdf . |
| 2. | Ratliff J, Nguyen T, Heiss J. Root and spinal cord compression from methylmethacrylate vertebroplasty. Spine (Phila Pa 1976). 2001;26:E300-E302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 129] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 3. | Hiwatashi A, Yoshiura T, Yamashita K, Kamano H, Dashjamts T, Honda H. Morphologic change in vertebral body after percutaneous vertebroplasty: follow-up with MDCT. AJR Am J Roentgenol. 2010;195:W207-W212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Li CH, Chang MC, Liu CL, Chen TS. Osteoporotic burst fracture with spinal canal compromise treated with percutaneous vertebroplasty. Clin Neurol Neurosurg. 2010;112:678-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Singh A, Wetherington CA, Gilula LA. Percutaneous vertebroplasty in osteoporotic compression fracture with epidural hematoma. AJR Am J Roentgenol. 2006;186:909-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Kobayashi N, Numaguchi Y, Fuwa S, Uemura A, Matsusako M, Okajima Y, Ishiyama M, Takahashi O. Prophylactic vertebroplasty: cement injection into non-fractured vertebral bodies during percutaneous vertebroplasty. Acad Radiol. 2009;16:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Hiwatashi A, Westesson PL. Patients with osteoporosis on steroid medication tend to sustain subsequent fractures. AJNR Am J Neuroradiol. 2007;28:1055-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Trout AT, Kallmes DF, Lane JI, Layton KF, Marx WF. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol. 2006;27:1586-1591. [PubMed] |
| 9. | Trout AT, Kallmes DF, Layton KF, Thielen KR, Hentz JG. Vertebral endplate fractures: an indicator of the abnormal forces generated in the spine after vertebroplasty. J Bone Miner Res. 2006;21:1797-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. AJNR Am J Neuroradiol. 1999;20:1365-1372. [PubMed] |