Published online Jul 28, 2013. doi: 10.4329/wjr.v5.i7.264
Revised: June 5, 2013
Accepted: July 4, 2013
Published online: July 28, 2013
Processing time: 108 Days and 1.9 Hours
We report a case of a 42-year-old male with symptomatic choledochocele and incidental pancreas divisum diagnosed with magnetic resonance cholangiopan- creatography (MRCP). Small choledochocele is rare congenital malformation associated with non-specific symptoms and a delay in diagnosis. The coexistence of choledochocele and pancreas divisum is extremely rare with only two case reports published in literature. In both cases MRCP failed to diagnose any biliary or pancreatic abnormality. This case suggests that the patients with recurrent abdominal pain and pancreas divisum should not be presumed to be suffering from pancreatitis. Careful evaluated for additional anomalies in the biliary tree should be sought for refractory symptoms. MRCP is a useful one-stop-shop for diagnosing pancreatic and biliary ductal anomalies.
Core tip: Small choledochocele is a rare congenital malformation associated with non-specific symptoms and a delay in diagnosis. The coexistence of choledochocele and pancreas divisum is extremely rare with only two cases reported in literature. In both cases magnetic resonance cholangiopancreatography (MRCP) failed to diagnose any biliary or pancreatic abnormality. We report a case of a 42-year-old male with symptomatic choledochocele and incidental pancreas divisum diagnosed with MRCP.
- Citation: Patidar Y, Agarwal N, Gupta S, Arora A, Mukund A, Rajesh S. Choledochocele with pancreas divisum: A rare co-occurrence diagnosed on magnetic resonance cholangiopancreatography. World J Radiol 2013; 5(7): 264-266
- URL: https://www.wjgnet.com/1949-8470/full/v5/i7/264.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i7.264
Choledochocele is a rare congenital malformation associated with non-specific symptoms which may result in a delay in diagnosis. The coexistence of choledochocele and pancreas divisum is extremely rare with only two cases reported in literature. In both cases magnetic resonance cholangiopancreatography (MRCP) failed to diagnose any biliary or pancreatic abnormality. We report a case of a 42-year-old male with symptomatic choledochocele and incidental pancreas divisum diagnosed with MRCP.
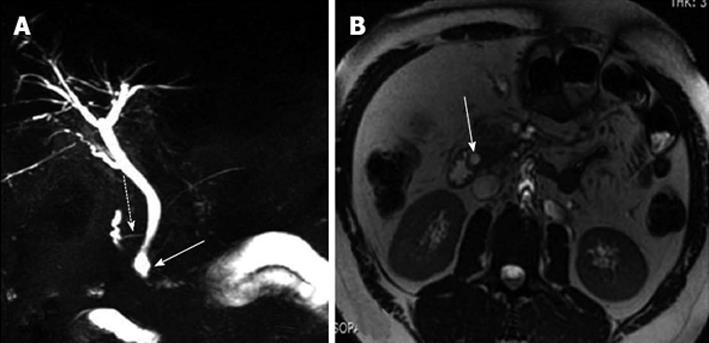
A 42-year-old male presented with recurrent upper abdominal pain following an uneventful cholecystectomy one year ago. Epigastric pain typically developed after a meal and gradually abated within a few hours. The blood count was within normal limits. The liver function tests revealed slight elevation of gamma-glutamyl transferase. The serum amylase and lipase levels were not elevated and upper gastrointestinal tract endoscopy was normal. A MRCP study revealed cystic dilatation of the terminal portion of the distal common bile duct. In addition, the pancreas was seen to drain predominantly through the duct of Santorini into the minor papilla (Figure 1). A diagnosis of choledochocele (type IIIb) with pancreas divisum was made. In our case, pancreas divisum was an incidental finding and not the cause of abdominal pain, as the patient had no documented laboratory or radiological evidence of pancreatitis during any of the previous episodes or the present hospital stay. The patient was advised intervention but he refused and was lost to follow-up.
Although the co-existence of choledochal cysts and pancreas divisum has been described in a few case reports[1,2], association of choledochocele with pancreas divisum is extremely rare with only two published case report[3,4]. Pancreas divisum occurs due to failure of the ventral and dorsal pancreatic ducts to fuse during embryogenesis[5]. The exocrine secretions are preferentially drained into the minor papilla through the dorsal duct and duct of Santorini. Impedance to the flow of pancreatic secretions through a relatively narrow minor papilla results in increased intraductal pressure which is hypothesised to cause recurrent pancreatitis[5]. On the other hand, one of the causes of choledochal cysts is suggested to be the reflux of pancreatic enzymes into the proximal biliary system because of the anomalous arrangement of the pancreaticobiliary ductal system[6]. Although the fusion of pancreatic buds and development of the pancreaticobiliary system occurs during the same period of embryological development, a choledochocele is usually not associated with anomalies of the pancreaticobiliary system[7]. A choledochocele is believed to represent a simple diverticulum occurring between the ampullary and common duct components of the sphincter or a congenital duodenal duplication that arises in that region[7]. Also, the pathology of choledochocele is different from other forms of choledochal cyst, and its lining is most commonly the duodenal mucosa which suggests that choledochoceles not only have features of the pancreaticobiliarysystem, but also those of the duodenum[3].
A choledochocele have been classified as a subtype (type III) of choledochal cysts by Todani et al[6]. They are characterized by cystic ectasia of the intraduodenal portion of the common bile duct. Choledochoceles are further classified as type IIIA (cystic dilatation of the common channel), type IIIB (cystic dilatation of the intramural bile duct with a common pancreaticobiliary channel) and type IIIC (cystic dilatation of the intramural bile duct opening into the duodenum separately from the pancreatic duct[8].
Intermittent episodes of upper abdominal pain represent the most common clinical presentation of choledochocele[6]. Acute pancreatitis with hyperamylasemia is occasionally present, as is obstructive jaundice. The diagnosis is easily missed unless a high index of suspicion of the entity exists and full investigation is carried out.
Unlike the present case, all previously reported cases had clinical and laboratory evidence of pancreatitis. Although endoscopic retrograde cholangiopancreatography (ERCP) has long been regarded as the gold standard for diagnosing choledochal cysts and evaluating anomalous pancreatobiliary junction, over the past ten years multiple studies have shown MRCP to be just as sensitive, if not more, than conventional cholangiography[9].
Complications include secondary biliary cirrhosis, spontaneous rupture of the cyst and cholangiocarcinoma[10,11]. Choledochoceles may be drained or resected endoscopically. Surveillance for dysplasia should be considered for lesions that are not resected.
In conclusion, patients with recurrent abdominal pain and pancreas divisum should not be presumed to be suffering from pancreatitis. Careful evaluation for additional anomalies in the biliary tree should be sought for refractory symptoms. MRCP is a useful one-stop-shop for diagnosing pancreatic and biliary ductal anomalies as demonstrated in this case report.
P- Reviewers Bradley EL, Kamisawa T, Kozarek R, Souza JLS, Sperti C S- Editor Gou SX L- Editor A
E- Editor Lu YJ
| 1. | Dalvi AN, Pramesh CS, Prasanna GS, Rege SA, Khare R, Ravikiran CS. Incomplete pancreas divisum with anomalous choledochopancreatic duct junction with choledochal cyst. Arch Surg. 1999;134:1150-1152. [PubMed] |
| 2. | Tuggle DW, Smith EI. Pancreas divisum, pancreatic pseudocyst, and choledochal cyst in an 8-year-old child. J Pediatr Surg. 1989;24:52-53. [PubMed] |
| 3. | Sonoda M, Sato M, Miyauchi Y, Yazumi S, Nakamura M. A rare case of choledochocele associated with pancreas divisum. Pediatr Surg Int. 2009;25:991-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Garrido A, León R, López J, Márquez JL. [An exceptional case of choledochocele and pancreas divisum in an elderly man]. Gastroenterol Hepatol. 2012;35:8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Agha FP, Williams KD. Pancreas divisum: incidence, detection, and clinical significance. Am J Gastroenterol. 1987;82:315-320. [PubMed] |
| 6. | Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269. [PubMed] |
| 7. | O’Neill JA, Choledochal cyst. In: Grosfeld JL, editor. Pediatric surgery, 6th edn. Mosby: Philadelphia 2006; 1620–1634. |
| 8. | Kamisawa T, Yoshiike M, Egawa N, Tsuruta K, Okamoto A, Matsukawa M. Classification of choledochocele. Hepatogastroenterology. 2005;52:29-32. [PubMed] |
| 9. | Irie H, Honda H, Jimi M, Yokohata K, Chijiiwa K, Kuroiwa T, Hanada K, Yoshimitsu K, Tajima T, Matsuo S. Value of MR cholangiopancreatography in evaluating choledochal cysts. AJR Am J Roentgenol. 1998;171:1381-1385. [PubMed] |
| 10. | Kagawa Y, Kashihara S, Kuramoto S, Maetani S. Carcinoma arising in a congenitally dilated biliary tract. Report of a case and review of the literature. Gastroenterology. 1978;74:1286-1294. [PubMed] |
| 11. | Arulprakash S, Balamurali R, Pugazhendhi T, Kumar SJ. Pancreas divisum and choledochal cyst. Indian J Med Sci. 2009;63:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |