Published online Jul 28, 2012. doi: 10.4329/wjr.v4.i7.335
Revised: May 19, 2012
Accepted: May 26, 2012
Published online: July 28, 2012
Chondroblastoma is a rare benign cartilaginous neoplasm of bone. The recurrence rate is high and complications are frequent following open curettage with bone grafting which is the standard treatment forchondroblastomas. We performed radiofrequency ablation in three cases of tibialchondroblastoma using the bipolar system. One patient experienced residual pain for which repeat ablation was performed. No other complications were observed during follow-up. Radiofrequency ablation may offer an effective alternative for the treatment of selected cases of chondroblastoma. The lesion characteristics which are likely to influence treatment outcome and the advantages offered by the bipolar system are discussed.
- Citation: Rajalakshmi P, Srivastava DN, Rastogi S, Julka PK, Bhatnagar S, Gamanagatti S. Bipolar radiofrequency ablation of tibialchondroblastomas: A report of three cases. World J Radiol 2012; 4(7): 335-340
- URL: https://www.wjgnet.com/1949-8470/full/v4/i7/335.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i7.335
Chondroblastomas are uncommon bone tumours of cartilaginous origin, accounting for less than 1% of all primary bone tumours. They are commonly seen in children and young adults, usually before the age of epiphyseal closure and are classically located in the epiphysis and apophysis of long bones[1]. Affected individuals usually present with pain and restriction of movement of the adjacent joint. Surgical curettage with or without bone grafting/cementing has been the treatment of choice for chondroblastomas and the risk of recurrence following surgery is high ranging from 10% to 35%[2]. Considering the epiphyseal location of the lesions, the risk of damage to articular cartilage and the growth plate with subsequent development of premature degenerative changes and limb shortening, respectively, is high[3].
Due to its minimally invasive nature and high success rates, radiofrequency (RF) ablation has become the treatment of choice for osteoid osteoma and is being increasingly used as palliative treatment for bone metastasis. It is also being evaluated in other benign bone tumours and recently, a few studies have described its effectiveness in the treatment of chondroblastomas[3-6]. In this article, we report three cases of chondroblastoma treated using the bipolar RF ablation system.
The study was approved by our institutional ethics committee. The decision to proceed with RF ablation over open surgery was taken in consensus with the orthopaedic surgeons taking into account the lesion size, location and potential surgical morbidity.
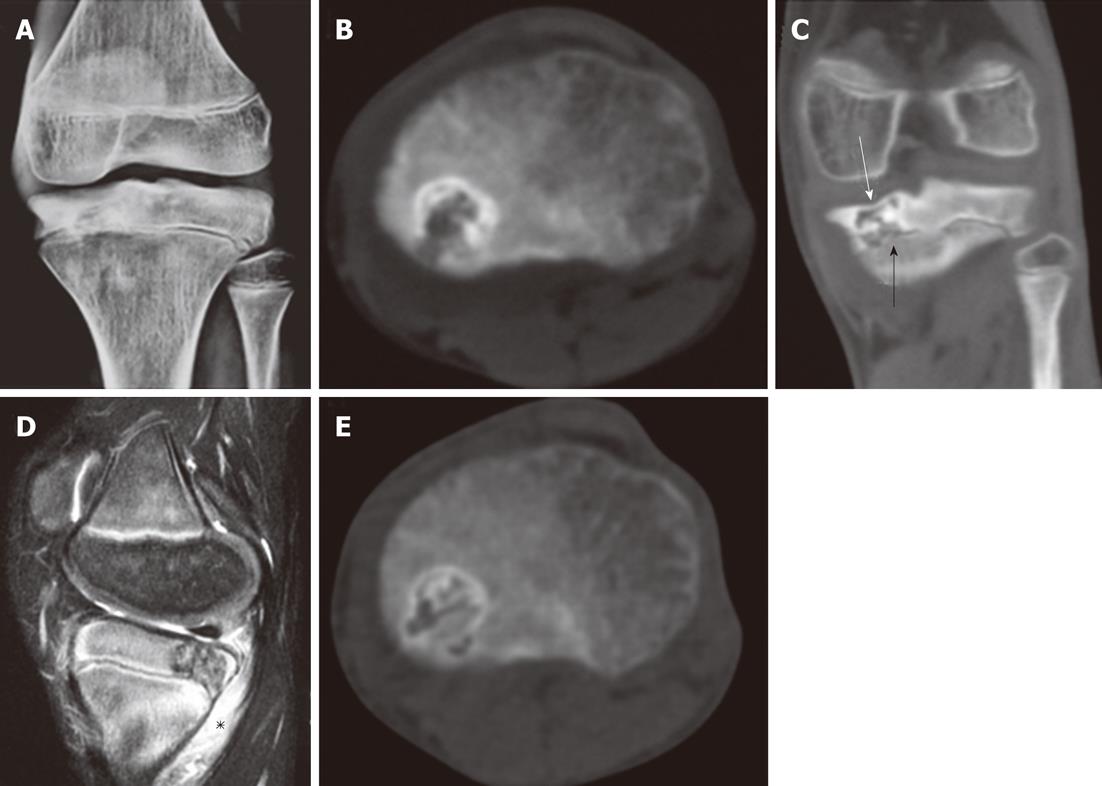
A 14-year-old male presented with pain in the left knee for the past 18 mo which was partially relieved with analgesics. The Visual Analogue Scale (VAS) score was 7. Radiograph and computed tomography (CT) images of the left knee revealed a 1.6 cm × 1.4 cm × 1.0 cm geographic lytic lesion with sclerotic margins in the left tibial epiphysis. There was associated thinning of the articular bone. The growth plate was open and the lesion was abutting the physis without breaching it. The lesion was hypointense on T1W images and heterogeneously hyperintense on T2W images with associated bone marrow oedema and mild joint effusion. A diagnosis of chondroblastoma was presumed based on the clinical profile and the characteristic location and imaging appearance of the lesion.
RF ablation was performed under general anaesthesia and CT guidance (Somatom Sensation 40 slice CT scanner, Siemens, Erlangen, Germany). Thin axial sections were acquired for precise localisation of the lesion. An 11 G bone biopsy needle set (Osteo Site, COOK Medical, Bloomington, United States) and a hammer were used to gain lesion access. An 18 G bipolar RF applicator with a 15 mm exposed tip (CelonProSurge Micro, Celon AG Medical Instruments, Teltow, Germany) and a bipolar/multipolar RF power generator (CelonLab POWER, Celon AG Medical Instruments, Teltow, Germany) were used for the ablation procedure. Since a bipolar RF system was used, grounding pads were not required for heat dispersion. As recommended by the manufacturers, pulsed RF energy was applied at a power setting of 5 W until a total energy of 0.90 KJ was deposited. As claimed by the manufacturers, the RF electrode produced an ablation zone of approximately 10 mm in diameter. Repeat ablation was performed after repositioning the needle so as to encompass the entire lesion. No immediate complications were observed. Analgesics and antibiotics were prescribed and the patient was discharged the next day. Since the lesion was located along a weight-bearing surface, the patient was instructed to restrain from strenuous/weight-bearing activities for 1-2 mo. A core biopsy specimen of the lesion obtained at the time of the procedure showed histopathological features consistent with chondroblastoma.
The patient experienced complete pain relief 1-2 d after the procedure (VAS = 0) and remained asymptomatic during the follow-up period (18 mo). Follow-up imaging (radiograph and CT) obtained at 6 mo showed increased matrix ossification with no significant change in lesion size. No delayed complications were observed. The pre-procedural, procedural and follow-up CT images of the patient are presented in Figure 1.
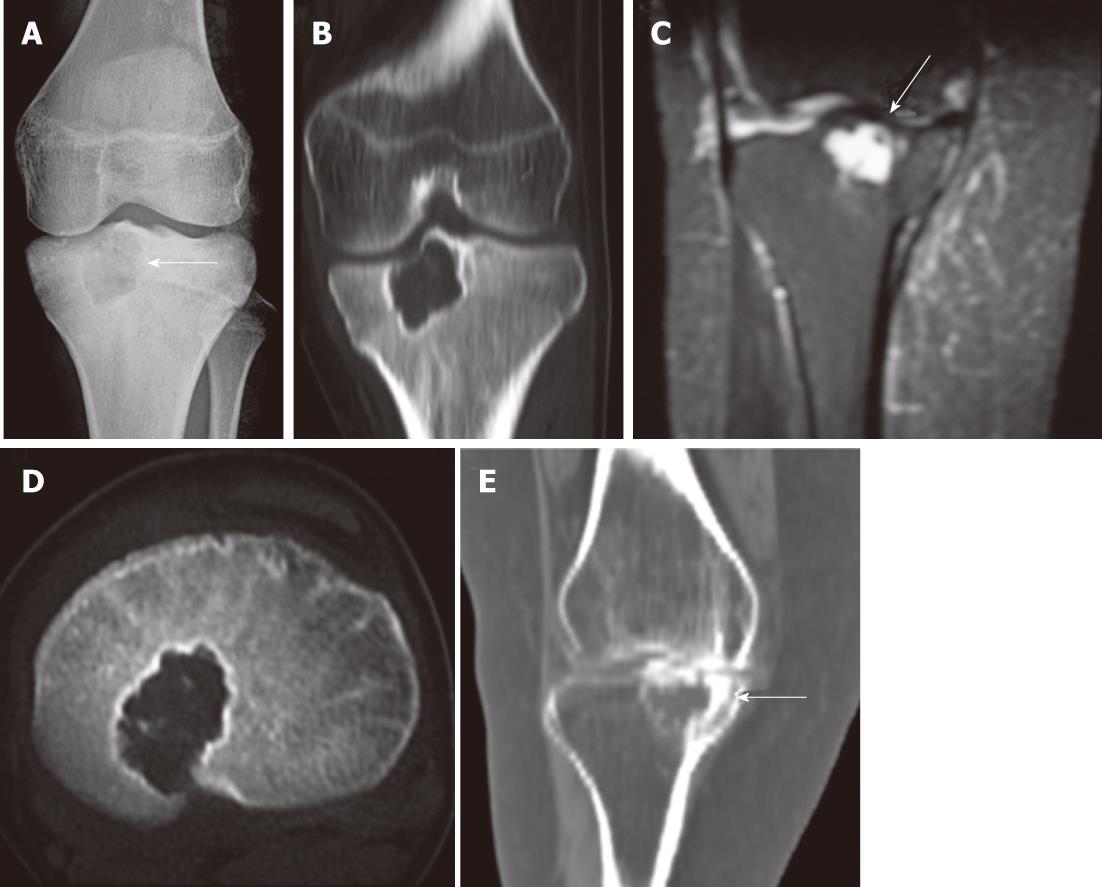
A 12-year-old female presented with severe pain in the left knee for the past year (VAS = 8) which was partially relieved with analgesics. Plain radiograph and CT images of the left knee showed a geographic lytic lesion with sclerotic margins of approximately 2.5 cm × 2.1 cm × 2.0 cm in size in the proximal epiphysis of the left tibia. The growth plate was open and breached and the lesion extended into the metaphysis. The overlying subchondral bone was significantly thinned. A diagnosis of chondroblastoma was presumed considering the clinical and imaging presentation which was confirmed histopathologically from the core biopsy specimen obtained during the procedure. RF ablation was performed in a similar manner to that in case 1 under general anaesthesia using an18G RF probe with a 15 mm active tip. A total of 3 ablations were performed at different needle positions to ensure adequate lesion coverage. The patient experienced complete pain relief (VAS = 0) 1-2 d after the procedure and remained asymptomatic during follow-up (17 mo). No further analgesic intake was required. No complications were observed. Pre-procedural and procedural images of the patient are shown in Figure 2.
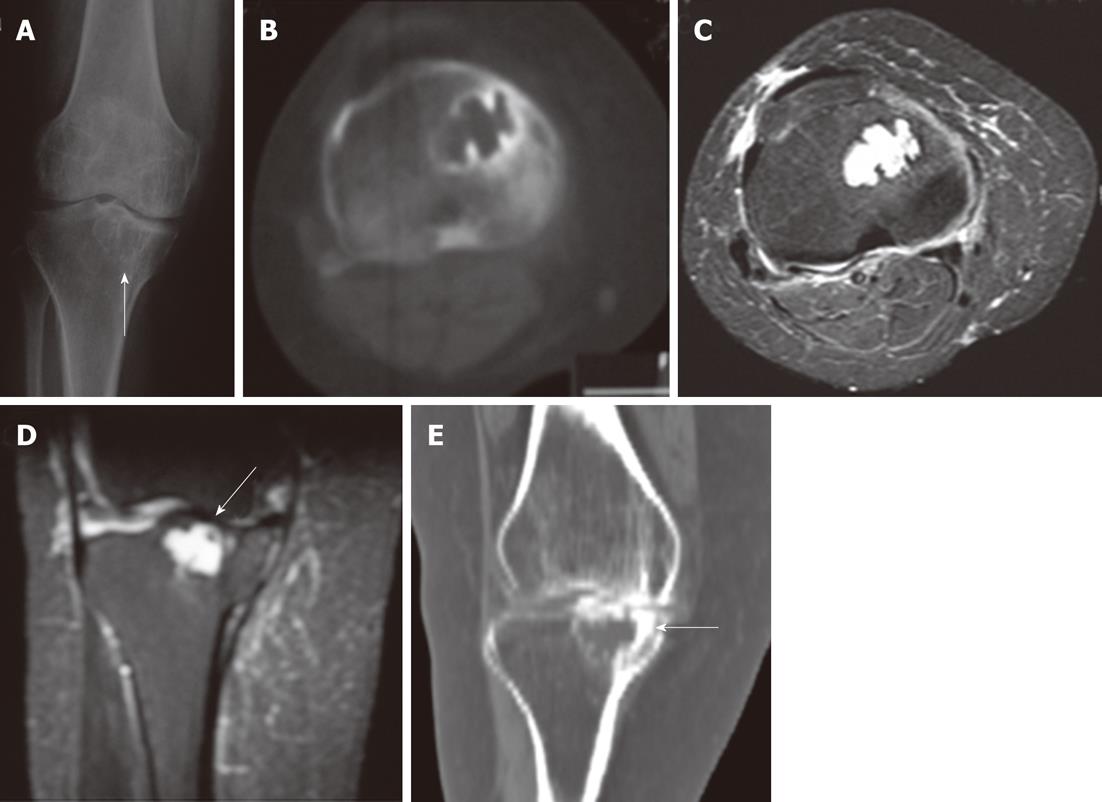
A 55-year-old female presented with severe pain and restriction of movement of the right knee joint for the past 2 years. The pain was increasing in severity over time and the VAS score at the time of presentation was 8. Radiograph and CT images of the right knee showed a 2.5 cm× 1.5 cm × 1.8 cm geographic lytic lesion with sclerotic margins in the proximal epiphysis of the right tibia. The lesion was hypointense on T1W images, homogeneously hyperintense on T2W images with associated mild joint effusion. There was thinning of the overlying subchondral bone. Although the age of the patient was atypical for chondroblastoma, the epiphyseal location of the lesion and its typical CT appearance favoured a diagnosis of chondroblastoma over other bone pathologies occurring in this location and RF ablation was chosen as the treatment option.
RF ablation was performed in a similar manner to that in the previous cases under general anaesthesia using the 18 G RF probe with a 15 mm exposed tip, and a total of 3 ablations were performed to adequately cover the lesion. Core biopsy of the lesion performed during the procedure confirmed the diagnosis of chondroblastoma. The patient continued to experience similar pain of reduced intensity (VAS 4-6) following the procedure. Follow-up CT imaging showed no obvious change in lesion appearance or the development of complications related to the procedure. A diagnosis of residual disease was made, and repeat RFA was carried out. A second RF ablation was performed 3 mo after the first procedure in a similar manner under general anaesthesia using an18 G RF probe with a 15 mm active tip. A total of 3 ablations were performed at different needle positions. The patient experienced complete pain relief (VAS 0) following the procedure. No complications were observed during follow-up (21 mo). Follow-up imaging (radiograph and CT) performed after the second RF procedure showed increased peripheral sclerosis of the lesion with no obvious change in lesion size. Procedural and follow-up images of the patient are shown in Figure 3.
Patient and procedure details are summarised in Table 1.
| S.No | Parameter | Patient 1 | Patient 2 | Patient 3 |
| 1 | Age/sex | 14/M | 12/F | 55/F |
| 2 | Pre-procedure VAS score | 7 | 8 | 8 |
| 3 | Location | Proximal tibia-Lt | Proximal tibia-Lt | Proximal tibia-Rt |
| 4 | Lesion dimension | 1.6 cm x 1.4 cm x 1.0 cm | 2.5 cm x 2.1 cm x 2.0 cm | 2.5 cm x 1.5 cm x 1.8 cm |
| 5 | Sub-chondral bone thinning | Present | Present | Present |
| 6 | Growth plate | Open-lesion abutting physis | Open-breached | Closed |
| 7 | Number of procedures | 1 | 1 | 2 |
| 8 | Number of ablations per procedure | 2 | 3 | 3 |
| 9 | Follow-up period | 18 mo | 17 mo | 21 mo |
| 10 | Complications | None | None | Recurrence |
| 11 | Post procedure VAS 1 wk, 1 mo, 3 mo | 2,0,0 | 0,0,0 | 4,6,0 |
| 12 | Post procedure analgesic intake | None | None | None |
Chondroblastomas are rare benign cartilaginous tumours commonlyoccurring in children and young adults between 10 and 20 years of age. They characteristically involve the epiphysis and apophysis of long bones with the proximal femur, proximal tibia and proximal humerus being the most commonly affected sites[7]. They are highly prone to recurrence following surgery due to difficult anatomical locations, inadequate tumour removal, or tumour aggressiveness[8]. Surgery is also associated with a risk of damage to articular cartilage and physeal plate leading to premature degenerative changes and limb length discrepancies,respectively[3,9].
RF ablation is a focal form of thermal ablation in which the deposited energy causes ionic oscillation, frictional heating and coagulation necrosis of the tissues[10]. In the musculoskeletal system, RF ablation is widely used in benign bone lesions such as osteoid osteoma and in bone metastasis due to high success rates, reduced surgical risks and early postoperative recovery[11,12]. A few recent studies have proved the effectiveness of RF ablation in the treatment of selected cases of chondroblastomas and have shown high success rates and minimal associated complications[3-6]. To the best of our knowledge, RF ablation of chondroblastomas using bipolar RF applicators has not been reported previously.
The bipolar RF system is considered a safer form of treatment compared to the monopolar system, since placement of grounding pads is eliminated, precluding the risk of skin burns. Additionally, the applied RF energy is confined to the treatment area in the bipolar system in contrast to the monopolarsystem where the energy streams out through the body in all directions, increasing the body temperature by 1-2 °C. For the same reason, metallic implants are a contraindication to the use of the monopolar system since they may be included in the electrical circuit leading to undesirable effects[13]. The bipolar system is also considered a more efficient form of treatment than the monopolar system. Since current flow is restricted to the probe tip, the bipolar system allows the use of higher current densities resulting in more uniform heating of tissues and the production of larger volumes of ablation[14]. Burdío et al[15] and several other authors[14,16] have established the precise and uniform nature of ablation produced by the bipolar system in vivo/animal studies. This may offer an additional advantage in the management of chondroblastomas, considering their critical location close to articular cartilage and joints.
The average size of the three lesions in the present study was 2.2 cm (longest dimension). All three lesions were located in weight-bearing surfaces (proximal tibial epiphysis) and there was associated thinning of the subchondral bone in all three patients. Considering the critical location of the lesions and the associated subchondral bone thinning, there was a risk of mechanical failure and articular surface damage following the procedure. We did not experience any complications regarding articular surface damage (collapse, osteonecrosis or chondrolysis) in the follow-up period. Intact cortical bone is a thermal and electrical insulator. Therefore, small chondroblastomas with an intact surrounding shell of bone carry a reduced risk of collateral thermal damage[4]. However, in large lesions, such as those treated in our study with expansion and cortical thinning, the insulating properties are greatly reduced with a substantial risk for articular cartilage damage. We believe that a restricted and precise zone of ablation produced by the bipolar system reduced the risk of collateral damage to surrounding structures. However, a larger study with a longer follow-up is required to confirm this. In the study by Rybak et al[3], the largest lesion in the study developed articular collapse which they attributed to the presence of a residual viable tumour. In the study by Tins et al[4], two of the four cases developed articular collapse. This was attributed to the use of multi-tined expandable electrodes which produced larger volumes of coagulation and carried an increased risk of damage to the surrounding structures. Large lesion size with thinning/breach of subchondral bone, location along a weight-bearing surface and the use of probes which produce larger coagulation zones increase the risk of articular surface damage following RF treatment[3].
Petsas et al[5] performed RF ablation of two large femoral head chondroblastomas (average size 2.7 cm) using multi-tined probes followed by apposition of bone grafts. Neither of the patients developed articular failure since the procedures were coupled with bone augmentation procedures. Both patients experienced clinical success.
Since chondroblastomas are epiphyseal tumours occurring in the younger population, there is risk of damage to the physis both during surgery and RF ablation. In fact, RF ablation is being evaluated in animal models as a method of producing epiphysiodesis for the treatment of limb length discrepancy and angular deformity[17]. Two patients (patients 1 and 2) in our study had an open growth plate and one of them had a physeal breach with extension of the lesion into the metaphysis. We did not observe any limb length discrepancy (on physical examination) during follow-up in either patient (17 and 18 mo). However, longer periods of follow-up are required to assess the occurrence of growth plate damage and limb length discrepancy, if any. The presence of a rim of bone between the lesion and the physis reduces the risk of damage to the physis[3].
One of our patients (patient 3) experienced residual pain following the procedure which was likely due to incomplete tumour ablation. Repeat RF ablation was performed after which she was asymptomatic at follow-up. Chondroblastomas have a high recurrence rate ranging from 10% to 35% following surgery,and cases have been reported to recura decade aftersurgery[18]. Hence, a larger study with a longer follow-up would be required to assess the risk of recurrence following RF ablation.
The average VAS score of the patients before the RF procedure was 7.7 (range: 7-8). All three patients experienced complete pain relief (VAS 0) in the initial few days following successful RF treatment requiring no further analgesic intake.
To conclude, RF ablation allows successful treatment of small chondroblastomas. Larger lesions carry a risk of damage to articular cartilage/growth plate and mechanical failure following RF treatment. The bipolar system may allow treatment of larger lesions with a relatively reduced risk of damage to surrounding structures compared to the monopolar system. However, a larger study with longer follow-up is required to establish the long-term outcome of this treatment.
Peer reviewers: Adnan Kabaalioglu, MD, Professor, Department of Radiology, Akdeniz University Hospital, Antalya 07059, Turkey; John L Nosher, MD, Clinical Professor, Chairman, Department of Radiology, University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School, 1 Robert Wood Johnson Place, PO Box 19, Medical Education Bldg., Room 404, New Brunswick, NJ 08903-0019, United States
S- Editor Cheng JX L- Editor Webster JR E- Editor Xiong L
| 1. | Yochum TR, Rowe LJ. Essentials of Skeletal Radiology. 3rd ed. Hagerstown, MD: Lippincott Williams and Wilkins 2005; 1280-1283. |
| 2. | Ramappa AJ, Lee FY, Tang P, Carlson JR, Gebhardt MC, Mankin HJ. Chondroblastoma of bone. J Bone Joint Surg Am. 2000;82-A:1140-1145. [PubMed] |
| 3. | Rybak LD, Rosenthal DI, Wittig JC. Chondroblastoma: radiofrequency ablation--alternative to surgical resection in selected cases. Radiology. 2009;251:599-604. [PubMed] |
| 4. | Tins B, Cassar-Pullicino V, McCall I, Cool P, Williams D, Mangham D. Radiofrequency ablation of chondroblastoma using a multi-tined expandable electrode system: initial results. Eur Radiol. 2006;16:804-810. [PubMed] |
| 5. | Petsas T, Megas P, Papathanassiou Z. Radiofrequency ablation of two femoral head chondroblastomas. Eur J Radiol. 2007;63:63-67. [PubMed] |
| 6. | Christie-Large M, Evans N, Davies AM, James SL. Radiofrequency ablation of chondroblastoma: procedure technique, clinical and MR imaging follow up of four cases. Skeletal Radiol. 2008;37:1011-1017. [PubMed] |
| 7. | Sepah YJ, Umer M, Minhas K, Hafeez K. Chondroblastoma of the cuboid with an associated aneurysmal bone cyst: a case report. J Med Case Rep. 2007;1:135. [PubMed] |
| 8. | Garin IE, Wang EH. Chondroblastoma. J Orthop Surg (Hong Kong). 2008;16:84-87. [PubMed] |
| 9. | Masui F, Ushigome S, Kamitani K, Asanuma K, Fujii K. Chondroblastoma: a study of 11 cases. Eur J Surg Oncol. 2002;28:869-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001;13:129-147. [PubMed] |
| 11. | Rosenthal DI, Hornicek FJ, Torriani M, Gebhardt MC, Mankin HJ. Osteoid osteoma: percutaneous treatment with radiofrequency energy. Radiology. 2003;229:171-175. [PubMed] |
| 12. | Callstrom MR, Charboneau JW, Goetz MP, Rubin J, Wong GY, Sloan JA, Novotny PJ, Lewis BD, Welch TJ, Farrell MA. Painful metastases involving bone: feasibility of percutaneous CT- and US-guided radio-frequency ablation. Radiology. 2002;224:87-97. [PubMed] |
| 13. | Mahnken AH, Tacke JA, Wildberger JE, Günther RW. Radiofrequency ablation of osteoid osteoma: initial results with a bipolar ablation device. J Vasc Interv Radiol. 2006;17:1465-1470. [PubMed] |
| 14. | Nakada SY, Jerde TJ, Warner TF, Wright AS, Haemmerich D, Mahvi DM, Lee FT. Bipolar radiofrequency ablation of the kidney: comparison with monopolar radiofrequency ablation. J Endourol. 2003;17:927-933. [PubMed] |
| 15. | Burdío F, Güemes A, Burdío JM, Navarro A, Sousa R, Castiella T, Cruz I, Burzaco O, Guirao X, Lozano R. Large hepatic ablation with bipolar saline-enhanced radiofrequency: an experimental study in in vivo porcine liver with a novel approach. J Surg Res. 2003;110:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Yi B, Somasundar P, Espat NJ. Novel laparoscopic bipolar radiofrequency energy technology for expedited hepatic tumour ablation. HPB (Oxford). 2009;11:135-139. [PubMed] |
| 17. | KUNKEL MG, DAHLIN DC, YOUNG HH. Benign chondroblastoma. J Bone Joint Surg Am. 1956;38-A:817-826. [PubMed] |
| 18. | Ghanem I, El Hage S, Diab M, Saliba E, Khazzaka A, Aftimos G, Dagher F, Kharrat K. Radiofrequency application to the growth plate in the rabbit: a new potential approach to epiphysiodesis. J Pediatr Orthop. 2009;29:629-635. [PubMed] |