Revised: February 22, 2012
Accepted: March 1, 2012
Published online: March 28, 2012
AIM: To evaluate two simple angle measurements for predicting lumbosacral transitional vertebra (LSTV) in magnetic resonance imaging (MRI) studies of the spine.
METHODS: The lumbar spine MRI studies of 50 subjects with LSTV and 50 subjects with normal lumbosacral anatomy were retrospectively evaluated. In each study, the mid-sagittal T2-weighted image was used to measure the angle formed by a line parallel to the superior surface of the sacrum and a line perpendicular to the axis of the scan table (A-angle), as well as the angle formed by a line parallel to the superior endplate of the L3 vertebra and a line parallel to the superior surface of the sacrum (B-angle).
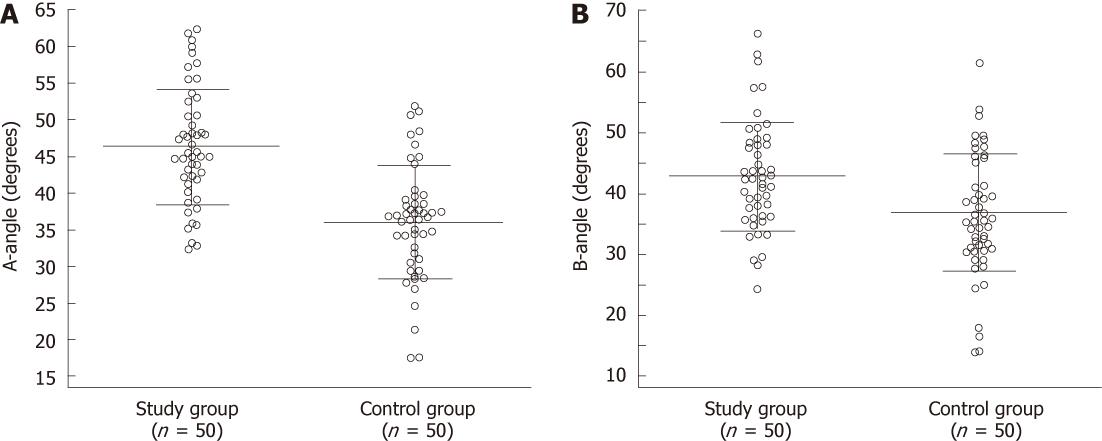
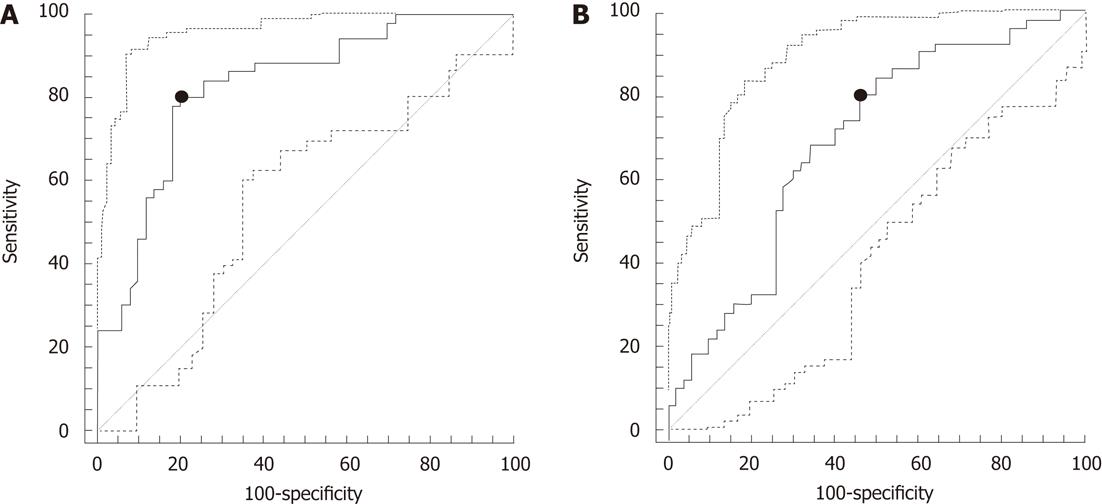
RESULTS: The total study population consisted of 100 subjects (46 males, 54 females, 51 ± 16 years old). There were no differences in age and sex between the two groups. Both A-angle and B-angle were significantly increased in subjects with LSTV compared to controls (P < 0.05). The optimal cut-off values of A-angle and B-angle for the prediction of LSTV were 39.8° (sensitivity = 80%, specificity = 80%, accuracy = 83%; 95% confidence interval = 74%-89%, P = 0.0001) and 35.9° (sensitivity = 80%, specificity = 54%, accuracy = 69%; 95% confidence interval = 59%-78%, P = 0.0005), respectively.
CONCLUSION: On sagittal MR images of the lumbar spine, an increased A-angle and/or B-angle should alert the radiologist to the presence of LSTV.
- Citation: Chalian M, Soldatos T, Carrino JA, Belzberg AJ, Khanna J, Chhabra A. Prediction of transitional lumbosacral anatomy on magnetic resonance imaging of the lumbar spine. World J Radiol 2012; 4(3): 97-101
- URL: https://www.wjgnet.com/1949-8470/full/v4/i3/97.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i3.97
Lumbosacral transitional vertebra (LSTV) is a developmental spinal anomaly, in which the lowest lumbar vertebra shows elongation of its transverse process and varying degrees of fusion/failure of segmentation from the sacrum[1]. LSTV has been reported to alter the biomechanics of the lumbar spine and contribute to low back pain[2-5]. However, controversy still exists regarding the actual clinical significance of this entity[6,7], which has an incidence of 4%-30% in the general population[8]. The radiologic identification and reporting of LSTV may provide the clinician with a potential cause for the patient’s symptoms and prevent erroneous numbering of the lumbar vertebrae, which may have serious implications in cases where spinal surgery is contemplated[7,8]. The anteroposterior radiograph of the lumbar spine remains the reference standard method to detect the above entity[9], but is not always available to the magnetic resonance imaging (MRI) reader. On MRI studies of the lumbar spine, LSTVs can be detected either on coronal images which highlight the transitional lumbosacral anatomy, or on axial images of the lumbosacral junction which depict the pseudoarthrosis or fusion of the last lumbar vertebra with the sacrum. However, coronal images are not usually acquired in MRI examinations of the lumbar spine, whereas the lumbosacral junction may be erroneously identified at the L4-L5 level in sagittal scout images of subjects with LSTV, resulting in incomplete axial coverage of the transitional level. As a result, LSTVs may be missed on MRI.
We hypothesized that transitional lumbosacral anatomy is associated with alterations of the lumbosacral curvature, the assessment of which could assist in detecting the entity on MRI. To validate this hypothesis, we applied two specific angle measurements in lumbar spine MRI studies of patients with and without LSTVs.
Institutional review board approval was granted and informed consent was waived for this HIPAA-compliant retrospective study. The MRI database of our institution was searched for examinations of the lumbar spine performed in adults over a period of 6 mo (from January to June 2010). Two radiologists, who were blinded to the original reports of the MRI studies, consecutively evaluated examinations from newer to older on a picture archiving and communication system workstation (Ultravisual, Emageon, AL, United States), in order to enroll 50 subjects with LSTV (study group) and 50 subjects without LSTV (control group). In each examination, a vertebra was defined as LSTV when (1) on sagittal images, it was separated from the sacrum by disc material; and (2) on axial images, it exhibited uni- or bilateral pseudoarthrosis or fusion with the sacral ala[6,9-11]. Subjects with scoliosis, listhesis greater than grade 1, and/or history or MRI findings of spinal trauma, tumor, surgery or infection were excluded. After the selection of the study sample, a software-based goniometer tool was used on the mid-sagittal T2-weighted image of each MRI study in order to measure: (1) the angle formed by a line parallel to the superior surface of the sacrum and a line perpendicular to the axis of the scan table (A-angle); and (2) the angle formed by a line parallel to the superior endplate of the L3 vertebra and a line parallel to the superior surface of the sacrum (B-angle) (Figure 1).
The patient’s age and sex, angle measurements of the respective MRI study and side(s) of pseudoarthrosis were registered for each case. In subjects with LSTV, the side(s) of the pseudoarthrosis/fusion was additionally recorded. Differences in age, A-angle and B-angle between the study and control groups were evaluated using Student’s t-test for independent samples, and difference in sex using χ2. Receiver operating characteristic (ROC) curves were computed to determine the optimal cut-off values of A-angle and B-angle for the prediction of transitional lumbosacral anatomy. A probability level of 0.05 was considered statistically significant. All data were stored on a spreadsheet (Excel 2010, Microsoft, Seattle, WA, United States), and analyses were performed using a commercially available statistical package (MedCalc 8.0, MedCalc Software, Mariakerke, Belgium).
The total study population consisted of 100 subjects (46 males, 54 females, 51 ± 16 years old). Table 1 summarizes the demographics of the two groups, along with the angle measurements of the respective MRI examinations. A graphic representation of the results obtained during angle measurements in subjects of the study and control groups is demonstrated in Figure 2. There were no differences in age and sex between the two groups. Both A-angle and B-angle were significantly increased in subjects with LSTV as compared to controls (P < 0.05, Figure 3). In the study group, the pseudoarthrosis/fusion was located on the left side in 19 (38%) cases, on the right side in 6 cases (12%) cases, and bilaterally in 25 (50%) cases. Based on the ROC curves, the optimal cut-off values of A-angle and B-angle for the prediction of LSTV were 39.8° (sensitivity = 80%, specificity = 80%, area under the ROC curve = 0.825; 95% confidence interval = 0.737-0.894, P = 0.0001), and 35.9° degrees (sensitivity = 80%, specificity = 54%, area under the ROC curve = 0.687; 95% confidence interval = 0.586-0.776, P = 0.0005), respectively (Figure 4).
| Feature | Study group | Control group | P value |
| Age (yr) | 53 ± 17 | 48 ± 14 | 0.1465 |
| Sex (males/females) | 22/28 | 24/26 | 0.4205 |
| A-angle (degrees) | 46.3 ± 7.8 | 35.9 ± 7.7 | < 0.0001 |
| B-angle (degrees) | 46.7 ± 8.4 | 41.6 ± 10.0 | 0.0035 |
Since the first reported association between LSTVs and low back pain by Bertolotti et al[12] in 1917, there has been considerable debate and controversy among authors regarding the clinical relevance of the above entity. It has been suggested that articulation between a LSTV and the sacrum protects the intervening intervertebral disc by limiting motion across the pseudoarthrosis and transmitting stress to superior lumbar segments, thereby resulting in its early degeneration. In subjects with LSTV, low back pain can originate from the pseudoarthrosis, resultant instability and degeneration of the level cephalad to the LSTV, compression of the nerve root from hypertrophied transverse process, and the contralateral facet joint, when the articulation is unilateral[8]. Clinicians who consider LSTV as a cause of low back pain and physicians who are involved with interventional procedures on the lumbar spine would benefit from MRI reports which describe the presence of this anatomical variation and provide accurate numbering of the lumbar vertebrae. MRI of the lumbar spine lacks the panoramic perspective of radiography and the spatial resolution of computed tomography, and unless the radiologist actively interrogates for this entity, the detection of LSTV may be missed.
In our experience, subjects with LSTV frequently demonstrate exaggerated lumbar lordotic curvature and lack of sharp angulations at the lumbosacral junction on the mid-sagittal MR image. Hence, we employed two simple angle measurements, the A-angle and the B-angle, which quantify the lumbosacral angulation and sacral inclination on sagittal MRI images, respectively. The A-angle is identical in measurement to the lumbosacral angle measured on lateral radiographs of the spine, increased values of which have been previously reported to be associated with low back pain[13]. The B-angle was defined by the superior sacral surface and the superior endplate of L3 vertebra, as we have observed that, in most cases, the main curvature of the lumbar spine extends along the above levels.
In agreement with our observations, both angles were significantly increased in subjects with LSTV as compared to controls (Figure 2). The two angles exhibited similar levels of sensitivity; however, the A-angle demonstrated higher specificity. Since most radiologists start the evaluation of lumbar spine MRIs from the sagittal images, it is suggested that a measurement of the A-angle or B-angle or at least a gross assessment of the sacral inclination and lumbar lordosis should be performed before proceeding to the detailed study assessment. An A-angle of greater than 40°, a B-angle of greater than 36°, a large inclination of the sacrum grossly with respect to axis of the scan table, or an exaggerated lumbar lordosis should alert the radiologist for the possible presence of an LSTV. Compared to the A-angle, the B-angle may be more difficult to measure (e.g., the forming lines may intersect out of the image) and is also harder to assess grossly by visual inspection. Of course, exaggerated lumbar lordosis may also result from significant degenerative disc disease, age or larger degrees of listhesis. The results of this study suggest that this finding should be carefully scrutinized in young subjects to avoid missing an LSTV.
Previous studies have reported several predictive similar signs which can suggest the presence of LSTV in lumbar spine MRIs. O’Driscoll et al[11] described two types of intervertebral discs, which present at the lumbosacral junction in subjects with LSTV. The “type I” disc is smaller than the superior one, maintains its high T2 signal intensity, has no intranuclear cleft, and extends along the entire anteroposterior space without any fusion between the adjacent endplates, and has been considered indicative of an LSTV. However, the specificity of the above findings is questionable, as in cases of pseudoarthrosis the transitional disc may appear normal. A “type II” disc is a rudimentary disc which is smaller than the transitional one, maintains its signal intensity, has no intranuclear cleft, and is associated with fusion of the anterior endplates, both of which appear concave[11]. Again, these signs are non-specific since a residual disc may exist at the S1-S2 level in up to 58% of cases, leading to over-diagnosis of LSTV[1]. On axial images, the identification of the iliolumbar ligaments, arising from the L5 vertebra, enables precise detection of LSTV and accurate numbering of the lumbar vertebrae[9]; however, in cases with segmentation anomalies of the thoracolumbar spine, the recognition of L5 vertebra may be incorrect[8]. Another study demonstrated that LSTVs commonly assume a “squared” appearance in lateral radiographs, with the ratio of the anteroposterior diameter of the superior endplate to the inferior endplate being less than 1.37[14].
By design, retrospective case-control studies are susceptible to selection bias; therefore a limitation of our study is that the studied material is not representative of the general population. Another limitation is the absence of correlation with radiographic findings, and the identification of the transitional anatomy being exclusively based on MRI. As a result, from the four classical types of LSTVs described by Castelvi et al[6], we were able to identify the LSTVs which exhibited pseudoarthrosis or fusion with the sacrum (types II , III and IV), but not those with dysplastic transverse processes, measuring at 19 mm in craniocaudal dimension (type I). Therefore, we cannot exclude the possibility that one or more cases were erroneously included in the study or the control group. However, the intent of the study was to predict LSTV on MR imaging alone, as these simple measurements may help MRI readers in their routine practice when radiographs have not been performed, or are not available at the time of read out. Future prospective studies in larger populations may re-evaluate the predictive values of the angles we present in this paper.
Lumbosacral transitional vertebra (LSTV) has been reported to alter the biomechanics of the lumbar spine and has been postulated to be an important contributor to low back pain. On magnetic resonance imaging (MRI), the detection of LSTVs is not always straightforward, and an unknown number of cases are missed. Sagittal MRI images constitute the initial search front for the readers to detect abnormalities of curvature and vertebral numbering. If the LSTV is not suspected on the sagittal image, it is easy to overlook the transitional vertebra on the axial image and lose the normal count. A simple means to detect LSTV on sagittal MRI studies of the lumbar spine may assist radiologists in providing more accurate reports.
This paper describes two simple angle measurements used on sagittal MRI images of the lumbar spine to predict LSTV.
Previous authors have described angle measurements which can be used to predict LSTV on radiographs, but there have been no respective reports on MRI. This is a novel and important paper, which describes easy and accurate means of predicting LSTV on MRI studies of the lumbar spine.
The angle measurements described are helpful for detecting LSTV, particularly in cases where radiographs have not been performed, or are not available at the time of read out.
LSTV is a developmental spinal anomaly, in which the lowest lumbar vertebra shows elongation of its transverse process and varying degrees of fusion/failure of segmentation from the sacrum.
The authors present simple but useful research describing an easy and intuitive sign that may give a hint to the radiologist regarding the presence of a transitional lumbosacral vertebral body. The A-angle is quite easy to assess at gross visual inspection and may alert radiologists looking for other morphologic signs which should be regarded as the only real definite evidence of transitional vertebral anatomy.
Peer reviewers: Shigeru Ehara, MD, Professor, Chair, Iwate Medical University School of Medicine, Morioka 020-8505, Japan; Tommaso Bartalena, MD, PhD, Radiology, S. Orsola University Hospital, Via Massarenti 9, 40138 Bologna, Italy
S- Editor Cheng JX L- Editor A E- Editor Zheng XM
| 1. | Hughes RJ, Saifuddin A. Imaging of lumbosacral transitional vertebrae. Clin Radiol. 2004;59:984-991. [PubMed] |
| 2. | Avimadje M, Goupille P, Jeannou J, Gouthière C, Valat JP. Can an anomalous lumbo-sacral or lumbo-iliac articulation cause low back pain? A retrospective study of 12 cases. Rev Rhum Engl Ed. 1999;66:35-39. [PubMed] |
| 3. | Brault JS, Smith J, Currier BL. Partial lumbosacral transitional vertebra resection for contralateral facetogenic pain. Spine (Phila Pa 1976). 2001;26:226-229. [PubMed] |
| 4. | Jonsson B, Stromqvist B, Egund N. Anomalous lumbosacral articulations and low-back pain. Evaluation and treatment. Spine. 1989;14:831-834. [PubMed] |
| 5. | Santavirta S, Tallroth K, Ylinen P, Suoranta H. Surgical treatment of Bertolotti's syndrome. Follow-up of 16 patients. Arch Orthop Trauma Surg. 1993;112:82-87. [PubMed] |
| 6. | Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984;9:493-495. [PubMed] |
| 7. | Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007;73:687-695. [PubMed] |
| 8. | Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010;31:1778-1786. [PubMed] |
| 9. | Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol. 2006;187:W59-W65. [PubMed] |
| 10. | Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976). 2004;29:200-205. [PubMed] |
| 11. | O'Driscoll CM, Irwin A, Saifuddin A. Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol. 1996;25:225-230. [PubMed] |
| 12. | Bertolloti M. Contribute alla conoscenza dei vizi di differenzazione del rachide con speciale reguardo all assimilazione sacrale della v lombare. La Radiologia Medica. 1917;4:113-144. |
| 13. | Hellems HK, Keats TE. Measurement of the normal lumbosacral angle. Am J Roentgenol Radium Ther Nucl Med. 1971;113:642-645. [PubMed] |
| 14. | Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976). 1980;5:215-222. [PubMed] |