Published online Nov 28, 2024. doi: 10.4329/wjr.v16.i11.638
Revised: September 19, 2024
Accepted: September 26, 2024
Published online: November 28, 2024
Processing time: 93 Days and 1 Hours
With very high mortality and disability rates, cerebrovascular diseases and intracranial tumors severely threaten the health and fighting strength of flying personnel, requiring great concern and intensive screening in clinic, early warning in an early and accurate manner and early intervention of diseases possibly resulting in inflight incapacitation are key emphases of aeromedical support in clinic.
To probe into the spectra of intracranial diseases, flight factors and medical imaging characteristics of military pilots (cadets) in the physical examination for transfer to pilot modified high performance aircraft, thus rendering theoretical references for clinical aeromedical support of pilots.
A total of 554 military pilots (cadets) undergoing physical examination for transfer to pilot modified high performance aircraft from December 2020 to April 2024 in a military medical center were enrolled in this study. Then, a retrospective study was carried out on intracranial disease spectra and head magnetic resona
Abnormal head images were found in 36 out of 554 pilots (cadets) participating in the physical examination for transfer to pilot modified high performance aircraft, including arachnoid cyst in 17 (3.1%) military pilots (cadets), suspected very small aneurysm in 11 (2.0%), cavernous hemangioma in 4 (0.7%), vascular malformation in 2 (0.4%), and pituitary tumor in 3 (0.5%, one of which developed cavernous hemangioma simultaneously). Among the 17 pilots (cadets) with arachnoid cyst, 4 were identified as unqualified for transfer to pilot modified high performance aircraft because the marginal brain tissues were compressed by the cyst > 6 cm in length and diameter. The 11 pilots (cadets) with suspected very small aneurysms identified by 3.0T MRI consisted of 6 diagnosed with conus arteriosus by digital subtraction angiography and qualified for transfer to pilot modified high performance aircraft, and 5 identified as very small intracranial aneurysms with diameter < 3 mm and unqualified for transfer to pilot modified high performance aircraft. No symptoms and signs were observed in the 4 military pilots (cadets) with cavernous hemangioma, and the results of MRI revealed bleeding. The 1 of the 4 had the lesion located in pons and developed Rathke cyst in pituitary gland at the same time, and unqualified for transfer to pilot modified high performance aircraft. The 2 of the 4 were unqualified for flying, and 2 transferred to air combat service division. The 2 pilots (cadets) with vascular malformation were identified as unqualified for transfer to pilot modified high performance aircraft. Among the 3 pilots (cadets) with pituitary tumor, one pilot cadet was identified as unqualified for flying since the tumor compressed the optic chiasma, one had cavernous hemangioma in pons in the meantime and transferred to air combat service division, and one was diagnosed with nonfunctional microadenoma and qualified for transfer to pilot modified high performance aircraft.
High-resolution head MRI examination is of great significance for screening and detecting cerebrovascular diseases and intracranial tumors in military flying personnel, and attention should be paid to its clinical application to physical examination for transfer to pilot modified high performance aircraft.
Core Tip: Cerebrovascular diseases and intracranial tumors may lead to intracranial hemorrhage, epilepsy, headache, neurological impairment and other risk factors for inflight incapacitation. High-resolution head magnetic resonance imaging examination is of great significance for screening and detecting cerebrovascular diseases and intracranial tumors in military flying personnel, and its clinical application to physical examination for transfer to pilot modified high performance aircraft should be attached with great importance. It is essential to detect and to intervene and treat cerebrovascular diseases and intracranial tumors as early as possible, thus reducing the grounding rate and maintaining flight safety.
- Citation: Zhao Y, Gao D, Liu YB, Xue JJ, Lu X, Dong JJ, Zhang Y, Zeng J. Spectra of intracranial diseases in Chinese military pilots (cadets) unqualified for transfer to pilot modified high performance aircraft. World J Radiol 2024; 16(11): 638-643
- URL: https://www.wjgnet.com/1949-8470/full/v16/i11/638.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i11.638
Early warning in an early and accurate manner and early intervention of diseases possibly resulting in inflight incapacitation are key emphases of aeromedical support in clinic[1]. With very high mortality and disability rates, cere
The 554 military pilots (cadets) who were hospitalized in a military medical center for the physical examination for transfer to pilot modified high performance aircraft from December 2020 to April 2024, and 36 pilots (cadets) had abnormal results of 3.0T head MRI examination were recruited in this study, followed by a retrospective analysis on their clinical data and appraisal conclusions.
Descriptive statistical analyses were carried out on the age, fighter type, flying time, type of diseases found in physical examination and appraisal conclusions of the 36 military pilots (cadets) with abnormal results of 3.0T head MRI examination. In addition, the disease proportion and systemic disease order were calculated. The 11 pilots (cadets) with cerebrovascular diseases unqualified for transfer to pilot modified high performance aircraft were identified and shunted.
All the 36 pilots (cadets) enrolled were male, aged 19-34 years old with a median age of 23.5 years ± 3.9 years old. The flying time was 0-1600 hours. The fighter type plus the number and age distribution is listed in Table 1.
| Fighter type (battle station) | n | Proportion | Age (years) | Median age (years) | Flying time (hours) | |
| Pilot cadet | Primary trainer cadet | 16 | 44.4 | 20-23 | 21.4 ± 1.0 | 17-200 |
| Advanced trainer cadet | 8 | 22.2 | 24-25 | 24.5 ± 0.5 | 300-370 | |
| Pilot cadet in basic education stage | 6 | 16.7 | 19-22 | 20.3 ± 1.0 | 0 | |
| Fighter pilot | 6 | 16.7 | 29-34 | 31.1 ± 1.7 | 1200-1600 | |
Totally 6 diseases were detected in the 36 military pilots (cadets), which, in the order of detection rate, were arachnoid cyst in 17 pilots (cadets), suspected cerebral aneurysm in 11, cavernous hemangioma in 4, pituitary tumor in 3 (one of which was accompanied by cavernous vascular malformation) and vascular malformation in 2. Among the 11 cases of suspected cerebral aneurysm, 6 cases were diagnosed as conus arteriosus by digital subtraction angiography (DSA), and qualified for transfer to pilot modified high performance aircraft. The 11 pilots (cadets) were definitely diagnosed with cerebrovascular diseases, including 5 cases of cerebral aneurysm, 4 cases of cavernous hemangioma and 2 cases of vascular malformation, and unqualified for transfer to pilot modified high performance aircraft (Table 2).
| Disease | n | Proportion | Detection rate | Fighter pilot | Advanced trainer cadet | Primary trainer cadet | Pilot cadet in basic education stage | Qualified for transfer to pilot modified high performance aircraft | Unqualified for transfer to pilot modified high performance aircraft | Qualified for flying | Transfer to pilot fighter | Transfer to pilot transport plane | Transfer to pilot helicopter | Transfer to air combat service division |
| Arachnoid cyst | 17 | 47.2 | 3.1 | 1 | 4 | 9 | 3 | 7 | 10 (58.8) | 4 | 7 | 6 | 0 | 0 |
| Cerebral conus arteriosus | 6 | 16.7 | 1.1 | 2 | 1 | 3 | 0 | 6 | 0 (0) | 0 | 6 | 0 | 0 | 0 |
| Cerebral aneurysm | 5 | 13.9 | 0.9 | 2 | 2 | 1 | 0 | 0 | 5 (100) | 0 | 2 (two-seat) | 2 | 1 | |
| Cavernous hemangioma | 4 | 11.1 | 0.7 | 0 | 2 | 1 | 1 | 0 | 4 (100) | 3 | 0 | 0 | 0 | 1 |
| Pituitary tumor | 3 | 8.3 | 0.5 | 1 | 1 | 0 | 1 | 1 | 2 (66.7) | 1 | 1 | 0 | 0 | 1 |
| Vascular malformation | 2 | 5.6 | 0.4 | 0 | 0 | 2 | 0 | 0 | 2 (100) | 0 | 0 | 0 | 2 | 2 |
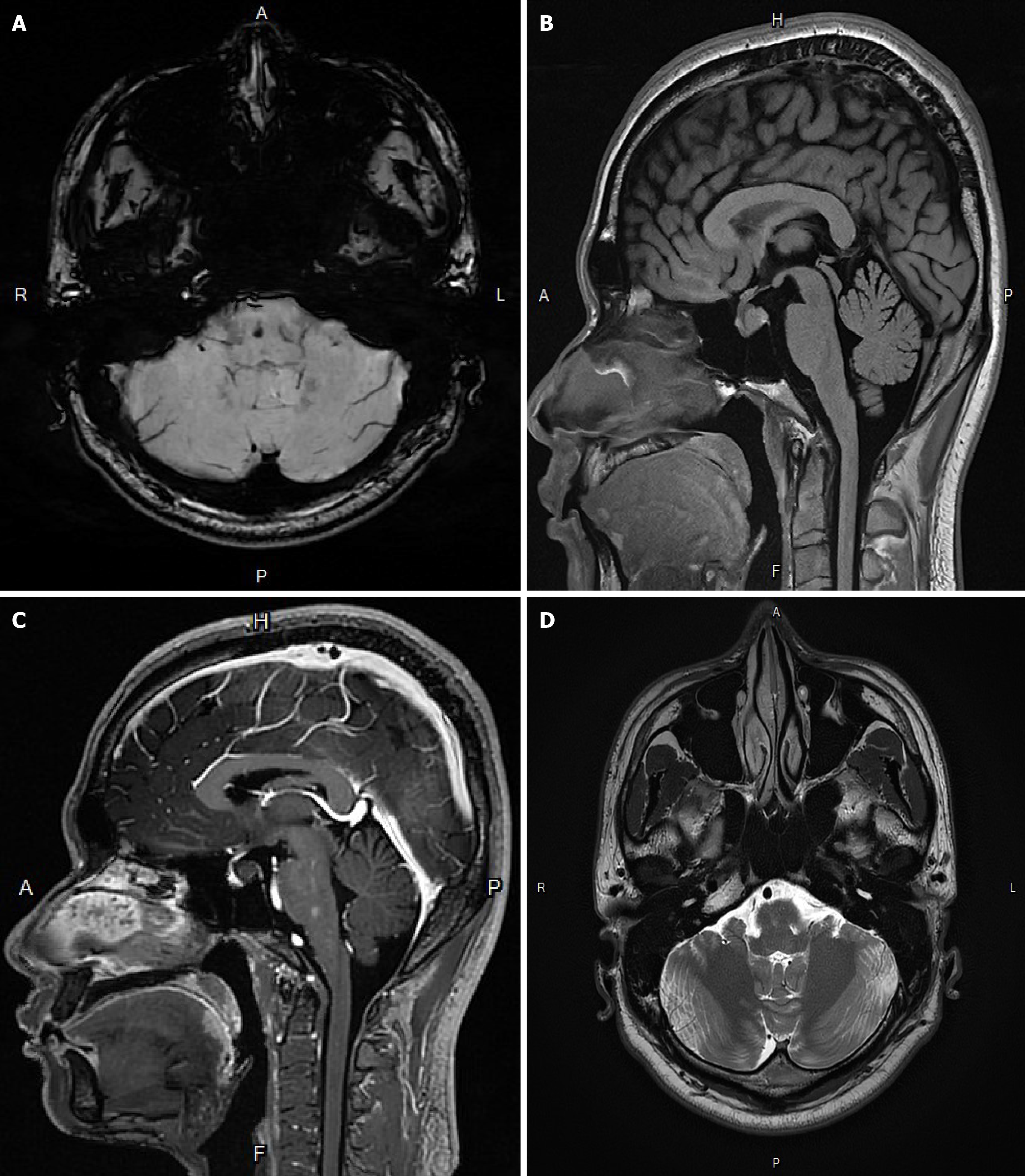
According to head MRI images, the sella turcica was slightly enlarged, and a quasi-circular 14 cm long focus showing slightly short T1 and long T2 signals was found in the pituitary gland. This focus showed slightly hyperintense signal on diffusion-weighted image (DWI), iso-intense signal on T1-weighted image (T1WI), and hyperintense signal on T2-weighted image (T2WI) and T2 fluid attenuated inversion recovery (T2FLAIR). Such a focus had a clear boundary, without enhancement after enhancement. Besides, the pituitary stalk moved forward slightly under pressure. In addition, there was a 5 mm quasi-circular focus in pons, with clear boundary and showing hyperintense signal on MRI, hypo-intense signal on DWI and SWI, slightly hypo-intense signal on T1WI, and normal signal on T2WI and T2FLAIR, and this focus had moderate enhancement after enhancement. Imaging diagnosis: Abnormal enhanced focus was found in pons, possibly suggesting cavernous hemangioma. No enhanced cystic focus was found in the sella, possibly suggesting Rathke cyst (Figure 1).
Due to influences of flying height, flight load and other factors, fighter pilots have increased psychological and physiological stress response intensity, together with greatly fluctuated blood pressure and heart rate in combat and training flight. Moreover, acceleration change can also cause changes in intracranial pressure and blood supply to the brain of fighter pilots. In the case of cerebrovascular diseases and intracranial tumors, cerebral hemorrhage, seizures, neurological symptoms and the like may be induced in pilots, resulting in inflight incapacitation, which is a severe threat to flight safety[4-6]. Head MRI examination is not included in the existing pilot physical examination and annual physical examination. In this study, the pilots with intracranial diseases did not suffer neurological symptoms or focal neu
With the popularization of high-resolution nuclear magnetic resonance and the progress of imaging artificial inte
In China, the prevailing criteria for flying personnel appraisal are central nervous system diseases and their sequelae, as well as disqualification for flying. In aeromedical appraisal, risk factors endangering flight safety such as epilepsy, intracranial hemorrhage, and focal neurological dysfunction should be evaluated, and then a comprehensive and accurate evaluation should be made in combination with the fighter type and flight experience of military flying personnel. Due to greatly fluctuated heart rate and blood pressure of fighter pilots in an air combat flight, intracranial pressure and intracranial blood supply can be changed by a high-load flight, easily leading to cerebrovascular disease/hemorrhage and other risk factors for inflight incapacitation[11-13]. Therefore, it is suggested to make strict requirements for the selection of pilot cadets and the pilots of single-seat high performance aircraft with disqualification for flying. Flying personnel with no symptoms and a low probability of hemorrhage are allowed to pilot multi-seat high performance aircraft with a small load, relevant head nuclear magnetic resonance examinations should be implemented frequently during follow-up, and risk factors (such as blood pressure, blood lipid, smoking and drinking) and flight intensity should also be controlled.
Cerebrovascular diseases and intracranial tumors may lead to intracranial hemorrhage, epilepsy, headache, neurological impairment and other risk factors for inflight incapacitation. High-resolution head MRI examination is of great significance for screening and detecting cerebrovascular diseases and intracranial tumors in flying personnel, and its clinical application to physical examination for transfer to pilot modified high performance aircraft should be attached with great importance. It is essential to detect and to intervene and treat cerebrovascular diseases and intracranial tumors as early as possible, thus reducing the grounding rate and maintaining flight safety.
| 1. | DeJohn CA, Mills WD, Hathaway W, Larcher J. Cardiac Inflight Incapacitations of U.S. Airline Pilots: 1995-2015. Aerosp Med Hum Perform. 2018;89:837-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Chen H, Khunte M, Colasurdo M, Malhotra A, Gandhi D. Thrombectomy vs Medical Management for Posterior Cerebral Artery Stroke: Systematic Review, Meta-Analysis, and Real-World Data. Neurology. 2024;102:e209315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 3. | Liu X, Cheng LC, Gao TY, Luo J, Zhang C. The burden of brain and central nervous system cancers in Asia from 1990 to 2019 and its predicted level in the next twenty-five years : Burden and prediction model of CNS cancers in Asia. BMC Public Health. 2023;23:2522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 4. | Biriukbaeva GN, Bogomolova MA. [Some peculiar traits of cerebrovascular diseases of aviation personnel]. Aviakosm Ekolog Med. 2012;46:50-54. [PubMed] |
| 5. | Evans S, Radcliffe SA. The annual incapacitation rate of commercial pilots. Aviat Space Environ Med. 2012;83:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Khurana VG, Jithoo R, Barnett M. Aerospace Implications of Key Neurological Conditions. Aerosp Med Hum Perform. 2021;92:113-119. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Lehnen NC, Schievelkamp AH, Gronemann C, Haase R, Krause I, Gansen M, Fleckenstein T, Dorn F, Radbruch A, Paech D. Impact of an AI software on the diagnostic performance and reading time for the detection of cerebral aneurysms on time of flight MR-angiography. Neuroradiology. 2024;66:1153-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Kwak Y, Son W, Kim YS, Park J, Kang DH. Discrepancy between MRA and DSA in identifying the shape of small intracranial aneurysms. J Neurosurg. 2021;134:1887-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Zyck S, Davidson CL, Sampath R. Arteriovenous Malformations of the Central Nervous System. 2024 Mar 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] |
| 10. | Jagathesan T, OBrien M. Aeromedical Implications of Cerebral Cavernomas. Aerosp Med Hum Perform. 2021;92:120-123. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 11. | Copeland K, Whinnery JE. Cerebral Blood Flow Based Computer Modeling of G(z)-Induced Effects. Aerosp Med Hum Perform. 2023;94:409-414. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Gunduz SH, Metin S. Medical reasons for permanent and temporary disqualification of Turkish civil aviation pilots. Arch Environ Occup Health. 2024;79:113-120. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Simons R, Maire R, Van Drongelen A, Valk P. Grounding of Pilots: Medical Reasons and Recommendations for Prevention. Aerosp Med Hum Perform. 2021;92:950-955. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |