Published online Oct 28, 2023. doi: 10.4329/wjr.v15.i10.281
Peer-review started: July 28, 2023
First decision: September 14, 2023
Revised: September 26, 2023
Accepted: October 11, 2023
Article in press: October 11, 2023
Published online: October 28, 2023
Processing time: 87 Days and 17.8 Hours
Ileus is a pathological condition of the abdomen that presents as a medical emergency. It is characterized by potential complications such as perforation and ischemia, which can lead to significant morbidity and mortality if not promptly addressed. The successful management of ileus relies heavily on the timely and precise identification of the condition. While conventional radiography (CR) is commonly used as the primary diagnostic tool, its accuracy in identifying obstructions ranges from 46% to 80%. Furthermore, the diagnostic accuracy of identifying the location and etiology of intestinal obstruction by CR is limited, therefore making computed tomography (CT) the ideal imaging modality in this regard.
To determine the presence of acute bowel obstruction (BO) on abdominal CT scenogram images and the accuracy of determining its possible location, taking into account the experience of the observers.
A retrospective screening was conducted on an ensemble of 46 individuals who presented to the emergency department between January 2021 and January 2022 with severe abdominal pain and were subsequently monitored for suspected ileus. The abdominal CT scans of these patients were assessed by three radiologists with varying levels of experience (1, 3, and 10 years) at different intervals (1 mo apart). The evaluation focused on determining the presence or absence of BO, as well as identifying the potential location of the obstruction (small bowel or large bowel). The study employed Kappa statistics to assess inter-observer variances, while the McNamer test was used to evaluate obstruction and segmentation discrepancies between observations. A significance level of P < 0.05 was determined to indicate statistical significance.
Out of the total sample size of 46 patients, 15 individuals (32.6%) were identified as female, while the remaining 31 individuals (67.4%) were identified as male. The ultimate diagnosis of 42 instances (91.3%) indicated ileus resulting from mechanical obstruction (MO). Among these patients, 14 (33%) experienced obstruction in the large bowel (LB), while 28 (66%) experienced obstruction in the small bowel (SB). The initial evaluation yielded sensitivity rates of 76.19%, 83.31%, and 83.33%, and diagnostic accuracy rates of 69.56%, 76.08%, and 80.43% for the detection of BO among the three observers. The initial study revealed that the average sensitivity of three observers in detecting the presence of ileus caused by MO was 80.94%, while the diagnostic accuracy was 75.35%. Based on the first evaluation, the senior observer demonstrated the highest sensitivity (85.71%), negative predictive value (92.60%), and diagnostic accuracy (80.43%) when accurately estimating the thick and thin segmentation, as per the final diagnosis. There was no statistically significant disparity observed in the sensitivities pertaining to the identification of ileus during the second assessment, as well as the precise determination of the segment level inside the LB or SB, when comparing the second and third observers. Nevertheless, although there was no statistically significant alteration in the detection rate of ileus by the first observer, there was a notable rise in the accuracy rate of segment estimating (73.91%). The senior assessor had a higher level of accuracy in assessing the existence of ileus and segmentation compared to the other evaluators in both evaluations.
The findings of our study indicate that the sensitivity and accuracy rates of abdominal CT scenogram scans in diagnosing acute MOs are similar to or greater than those of CR. Additionally, the study revealed that radiologists with more experience demonstrated a higher likelihood of accurately predicting the existence and potential localization of MO compared to their less experienced counterparts.
Core Tip: This retrospective study aims to determine the accuracy of detecting the presence and possible location of obstruction on computed tomography (CT) scenogram images of the abdomen, which can be used as the primary imaging method in the diagnosis of acute bowel obstruction, taking observer experience into account. The experienced observer had the highest sensitivity (83.33%), positive predictive value (94.59%), and diagnostic accuracy (80.43%) for detecting mechanical obstruction (MO). The diagnostic accuracy of the same observer in estimating the segmentation of a MO was 80.43%. These findings show that CT scenogram images alone can demonstrate high diagnostic accuracy and sensitivity in relation to years of experience in diagnosing ileus.
- Citation: Kadirhan O, Kızılgoz V, Aydin S, Bilici E, Bayat E, Kantarci M. Does the use of computed tomography scenogram alone enable diagnosis in cases of bowel obstruction? World J Radiol 2023; 15(10): 281-292
- URL: https://www.wjgnet.com/1949-8470/full/v15/i10/281.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i10.281
Diagnostic imaging is necessary to determine the existence, location, severity, and potential cause of bowel obstruction (BO) when it is suspected based on clinical indicators and physical examination results[1]. BO is a medical disorder that can arise from either mechanical or functional causes, impeding the regular flow of intestinal contents. The choice of therapy, whether surgical or non-surgical, and subsequent follow-up treatments, will depend on the underlying cause of the obstruction. According to existing literature, it has been reported that around 20% of surgical admissions related to acute abdominal discomfort can be attributed to BO[2]. Timely identification of this condition has significance in terms of averting potential consequences such as perforation and ischemia.
Conventional radiography (CR) is the primary imaging modality utilized for determining the existence of ileus, owing to its widespread availability and cost-effectiveness[3]. Nevertheless, CR is not typically capable of accurately displaying the precise position, extent, and etiology of BO, nor can it effectively identify secondary indications such as aberrant wall thickening, pneumatous acid, and intestinal viability. In contrast, computed tomography (CT) is widely regarded as the preferred modality for addressing these diagnostic needs[4]. The literature has demonstrated a range of 90-95% accuracy for CT in the diagnosis of high-grade intestinal obstructions[5-8]. CT scenogram images are acquired with the patient lying in the supine posture, and they offer a comprehensive overview of the region of interest. These images are obtained with minimal radiation exposure. The utilization of X-rays in both CT and CR imaging techniques results in the generation of ionizing radiation. Ionizing radiation induces heritable alterations in the genetic code via deoxyribonucleic acid damage. It has been reported that ionizing radiation can cause cataracts, skin burns, temporary or permanent infertility in the case of exposure to high doses, and various cancers in the case of intermittent exposure to low doses[9]. In a published study, 1012 patients who presented to the emergency department and simultaneously underwent chest X-ray and CT scan were included. This study demonstrated that a single imaging method was able to accurately diagnose the patients in 77.1% of the cases involving trauma and 80.4% of the cases without trauma. Consequently, the prompt referral of patients to appropriate treatment was facilitated, as there was no requirement for a second imaging method. This demonstrates the importance of minimizing the utilization of imaging techniques that include ionizing radiation, in light of the potential adverse consequences[10]. A study revealed that the utilization of CT scenogram images as a standalone diagnostic tool for BO exhibited an interobserver sensitivity ranging from 93% to 86% and a specificity ranging from 85% to 87%. These findings were similar to the outcomes reported for axial CT and the combination of axial and coronal CT[11].
The purpose of this study was to determine the presence and potential location of obstruction on CT scenogram images of the abdomen, which can be used as a primary imaging method in the diagnosis of acute BO, taking observer experience into consideration.
The research undertaken in this study received approval from the Erzincan University Ethics Committee (Decision no: E-21142744 804.01-128338 Date: December 7, 2021) and was carried out in compliance with the principles outlined in the Declaration of Helsinki.
The retrospective design of the study necessitated the exemption of informed consent. A retrospective investigation was conducted on a cohort of 46 patients who were brought to the emergency department between January 2021 and January 2022. These patients presented with acute abdomen and were subsequently followed up due to suspicion of BO. As part of the evaluation, multi-detector abdominal CT scans were performed. The CT scans underwent anonymization processes and were thereafter uploaded to designated workstations.
The coronal abdominal CT scenogram images of the patients enrolled in the study were assessed by three radiologists who had varying levels of experience, with one having 1 year, another having 3 years, and the third having 10 years of experience. These radiologists were blinded to the final diagnosis of the patients. The abdominal CT scenogram images were assessed at two separate time points, with a one-month interval, to determine the presence of BO (coded as 1 for presence and 0 for absence). Additionally, the localization of the potential obstruction (either in the small bowel or the large bowel) was evaluated in cases where obstruction was suspected.
The ultimate diagnosis was determined by reviewing medical records, surgical reports, and pathology results. The exclusion of BO can be achieved through the identification and treatment of an alternative illness, or by confirming that the patient has not undergone exploratory laparotomy and does not exhibit any indications of prolonged discomfort, abscess, or unexplained fever throughout their hospitalization.
The investigation of inter-observer differences was conducted using Kappa statistics. The percentages of inter-observer and intra-observer agreement were determined by dividing the total number of instances with complete agreement by the overall number of instances. Cohen's Kappa statistics were employed to assess the level of agreement, accounting for the agreement that could occur by chance. Interpretation of the Kappa statistic is as follows: When the value is less than 0.00, the level of agreement is considered poor; when the value falls between 0.00 and 0.20, the agreement is categorized as mild; when the value ranges from 0.21 to 0.40, the agreement is considered fair; when the value falls between 0.41 and 0.60, the agreement is categorized as moderate; when the value ranges from 0.61 to 0.80, the agreement is categorized as considerable; and when the value falls between 0.81 and 1.00, the agreement is virtually perfect. The present study examined the inter-observer appraisal of obstruction and segmentation differences using the McNamer test. The statistical analyses were conducted using the SPSS (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, United States) 21.0 software package. Statistical significance was determined by a P value threshold of less than 0.05.
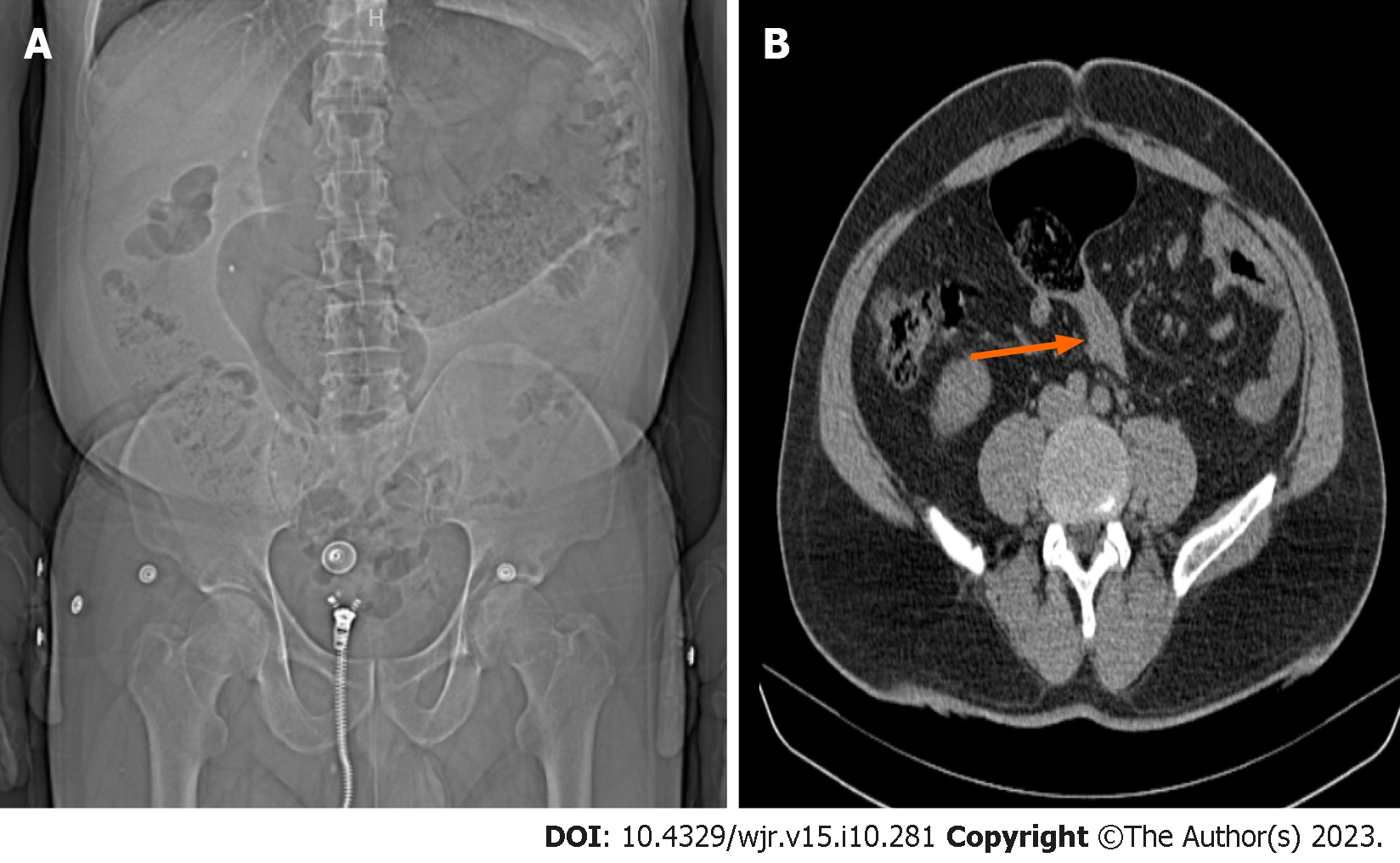
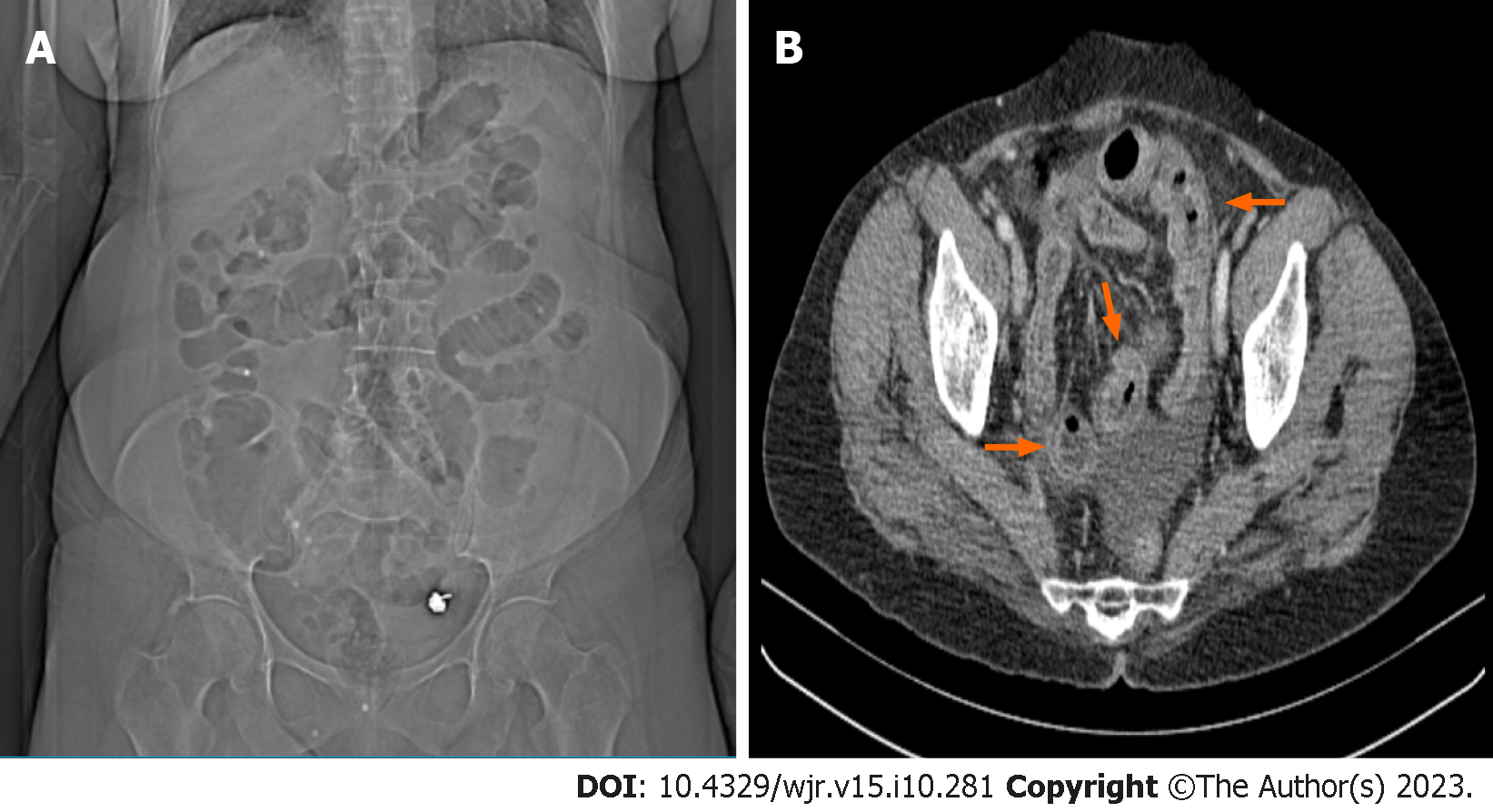
Demographic findings: Out of the total sample size of 46 patients, 15 individuals (32.6%) were identified as female, while the remaining 31 participants (67.4%) were classified as male. The ultimate diagnosis of 42 instances, accounting for 91.3% of the total, indicated ileus resulting from MO. Out of the total number of patients, 14 individuals (33%) exhibited obstruction in the large bowel (LB), whereas 28 individuals (66%) experienced obstruction in the small bowel (SB). A comprehensive breakdown of the factors contributing to obstruction is presented in Table 1. Several case studies are illustrated in Figures 1-4.
| Causes of mechanical obstruction | Case count |
| Postoperative adhesion | 21 |
| Hernia | 10 |
| Epigastric | 2 |
| Femoral | 2 |
| Incisional | 1 |
| Indirect inguinal | 2 |
| Umbilical | 2 |
| Obturator | 1 |
| Colon cancer | 6 |
| Ascending | 1 |
| Descending | 2 |
| Transverse | 1 |
| Sigmoid | 2 |
| Volvulus | 3 |
| Sigmoid | 3 |
| Ileitis due to Crohn's disease | 1 |
| Closed loop obstruction | 1 |
The initial assessment scenario for identifying the existence of obstruction: The initial sensitivity findings of the three observers analyzing the abdominal CT scenogram images were 76.19%, 83.31%, and 83.33%, while their diagnostic accuracy results in recognizing the existence of BO were 69.56%, 76.08%, and 80.43%, respectively. The average sensitivity estimate for all three observers in detecting ileus caused by MO during the initial examination was determined to be 80.94%, with a corresponding diagnostic accuracy of 75.35%. The third observer demonstrated the greatest sensitivity (83.33%), positive predictive value (94.59%), and diagnostic accuracy (80.43%) among all observers, as shown in Table 2.
| Mechanical obstruction by final diagnosis | Specificity, % | Sensitivity, % | PPV, % | NPV, % | Accuracy, % | |||
| Yes | None | Total | ||||||
| I Observer | ||||||||
| Yes | 32 (76.2) | 4 (100) | 36 (78.3) | 76.19 | 0 | 88.88 | 0 | 69.56 |
| None | 10 (23.8) | 0 (0) | 10 (21.7) | |||||
| II Observer | ||||||||
| Yes | 35 (83.3) | 4 (100) | 39 (84.8) | 83.31 | 0 | 89.74 | 0 | 76.08 |
| None | 7 (16.7) | 0 (0) | 7 (15.2) | |||||
| III Observer | ||||||||
| Yes | 35 (83.3) | 2 (50) | 37 (80.4) | 83.33 | 50 | 94.59 | 22.23 | 80.43 |
| None | 7 (16.7) | 2 (50) | 9 (19.6) | |||||
| Total | 42 (91.3) | 4 (8.7) | 46 (100) | |||||
Initial examination of obstruction segmentation assessment: Based on the initial evaluation's segmentation according to the final diagnosis, the three observers demonstrated accuracy rates of 54.33%, 65.22%, and 80.43% in estimating the segmentation level of the large and small bowel. Notably, these rates were observed to increase proportionally with the observers' years of experience. In addition, when comparing the results of the 3rd observer with 10 years of experience in accurately evaluating the MO segmentation level to those of the other observers (Table 3), it was seen that this observer had the highest diagnostic sensitivity (85.71%) and negative predictive value (92.60%).
| Mechanical obstruction segment by final diagnosis | Specificity, % | Sensitivity, % | PPV, % | NPV, % | Accuracy, % | |||
| Large | Small | Total | ||||||
| I Observer | ||||||||
| Large | 12 (85.7) | 19 (59.4) | 31 (67.4) | 85.70 | 40.62 | 38.67 | 86.69 | 54.33 |
| Small | 2 (14.3) | 13 (40.6) | 15 (32.6) | |||||
| II Observer | ||||||||
| Large | 8 (57.1) | 10 (31.3) | 18 (39.1) | 57.14 | 68.75 | 44.40 | 78.60 | 65.22 |
| Small | 6 (42.9) | 22 (68.8) | 28 (60.9) | |||||
| III Observer | ||||||||
| Large | 12 (85.7) | 7 (21.9) | 19 (41.3) | 85.71 | 78.12 | 63.12 | 92.60 | 80.43 |
| Small | 2 (14.3) | 25 (78.1) | 27 (58.7) | |||||
| Total | 14 (30.4) | 32 (69.6) | 46 (100) | |||||
Second assessments: There was no statistically significant distinction observed between the second and third observers in their ability to detect the existence of BO during the second repeated evaluation. Additionally, there was no significant difference in their accuracy in predicting the level of the large or small bowel segment in the presence of obstruction, as well as their sensitivity. The P value obtained was greater than 0.05. Nevertheless, although there was no statistically significant difference in the rate of detecting obstruction by the initial evaluator (P > 0.05), there was a noteworthy rise in the rate of accurately estimating segmentation (P = 0.022) (Table 4). The diagnostic accuracy for estimating the localization of obstruction segmentation by the first observer increased from 54.33% (Table 3) to 73.91% (Table 6), indicating a noticeable improvement. The accuracy of the 3rd observer in correctly predicting the presence of MO (Table 5) and identifying the potential location of segmentation (Table 6) during the second evaluation was higher compared to the other evaluators.
| Observer | Positive predict rate (large) | Negative predict rate (small) | P valuea | |
| Obstruction | I | 36 (100) | 8 (80) | 0.500 |
| II | 35 (89.7) | 6 (85.7) | 0.375 | |
| III | 36 (97.3) | 8 (88.9) | 0.999 | |
| Segmentation | I | 20 (64.5) | 13 (86.7) | 0.022 |
| II | 16 (88.9) | 23 (82.1) | 0.453 | |
| III | 18 (94.7) | 26 (96.3) | 0.999 |
| Mechanical obstruction by final diagnosis | Specificity, % | Sensitivity, % | PPV, % | NPV, % | Accuracy, % | |||
| Yes | None | Total | ||||||
| I Observer | ||||||||
| Yes | 34 (81) | 4 (100) | 38 (82.6) | 81 | 0 | 88.47 | 0 | 73.91 |
| None | 8 (19) | 0 (0) | 8 (17.4) | |||||
| II Observer | ||||||||
| Yes | 32 (76.2) | 4 (100) | 36 (78.3) | 76.19 | 0 | 88.88 | 0 | 69.56 |
| None | 10 (23.8) | 0 (0) | 10 (21.7) | |||||
| III Observer | ||||||||
| Yes | 35 (83.3) | 2 (50) | 37 (80.4) | 83.33 | 50 | 94.59 | 22.23 | 80.43 |
| None | 7 (16.7) | 2 (50) | 9 (19.6) | |||||
| Total | 42 (91.3) | 4 (8.7) | 46 (100) | |||||
| Mechanical obstruction segment by final diagnosis | Specificity, % | Sensitivity, % | PPV, % | NPV, % | Accuracy, % | |||
| Large | Small | Total | ||||||
| I Observer | ||||||||
| Large | 12 (85.7) | 10 (31.3) | 22 (47.8) | 85.71 | 68.75 | 54.50 | 91.68 | 73.91 |
| Small | 2 (14.3) | 22 (68.8) | 24 (52.2) | |||||
| II Observer | ||||||||
| Large | 9 (64.3) | 12 (37.5) | 21 (45.7) | 64.29 | 62.50 | 42.82 | 80.03 | 63.04 |
| Small | 5 (35.7) | 20 (62.5) | 25 (54.3) | |||||
| III Observer | ||||||||
| Large | 13 (92.9) | 6 (18.8) | 19 (41.3) | 92.86 | 81.25 | 68.39 | 96.30 | 84.78 |
| Small | 1 (7.1) | 26 (81.3) | 27 (58.7) | |||||
| Total | 14 (30.4) | 32 (69.6) | 46 (100) | |||||
Intra-rater compliance: Upon evaluation of the Cohen Kappa coefficients pertaining to intra-observer agreement in the diagnosis of MO, it was shown that a moderate level of agreement existed between the first and second observers. Similarly, there was moderate agreement in the diagnosis of obstruction between observers I-III and II-III. The study analyzed Cohen Kappa coefficients to assess the level of agreement among evaluators in diagnosing the potential segmentation location of MO. The results indicated a moderate level of agreement between evaluators I-III and evaluators II-III (P < 0.05). Nevertheless, it was noted that there existed a limited level of concordance between I and II (indicating poor agreement), and it was found that there was no statistically significant evidence of agreement (P = 0.228) (Table 7).
| Observer | Positive predict rate | Negative predict rate | κ (95%CI) | P value | |
| Obstruction | I vs II | 34 (94.4) | 5 (50) | 0.498 (0.336-0.660) | 0.001 |
| I vs III | 33 (91.7) | 6 (60) | 0.536 (0.382-0.690) | < 0.001 | |
| II vs III | 35 (95.5) | 5 (55.6) | 0.548 (0.386-0.710) | < 0.001 | |
| Segmentation | I vs II | 14 (45.2) | 11 (73.3) | 0.151 (0.03-0.272) | 0.228 |
| I vs III | 18 (58.1) | 14 (93.3) | 0.426 (0.314-0.538) | 0.001 | |
| II vs III | 13 (68.4) | 22 (81.5) | 0.503 (0.373-0.633) | 0.001 |
BO is a frequently observed clinical condition within the field of general surgery. Failure to urgently diagnose this condition can lead to serious complications, including perforation and ischemia. Therefore, it is of utmost importance to promptly identify and refer patients with suspected small or large BO to the appropriate medical specialty. According to available reports, it has been shown that roughly 75% of mechanical obstructions affecting the gastrointestinal tract are specifically localized within the SB[12,13]. In our study, consistent with the literature, there was a predominance of small bowel obstruction (SBO), with a prevalence rate of 66%.
The causes of a MO at the level of the SB can be adhesions, internal and external hernias, primary or extraintestinal neoplasia, stricture due to Crohn's disease, malrotation, duplication cysts, hematoma, ischemic stricture, invagination, endometriosis, and foreign body[14]. Adhesions are commonly identified as the primary cause of MO in western countries, whereas hernias and malignancies are also recognized as significant contributors to this condition[3,15-17]. The total frequency of the aforementioned three etiologies exceeds 80%[18]. In our research, the underlying causes of obstruction occurring in the SB were primarily attributed to surgical adhesions, with external hernias being the second most prevalent factor.
The causes of MO at the level of the LB include colorectal cancer, diverticulitis, volvulus, stricture owing to Crohn's disease, non-colorectal malignancy, endometriosis, ischemic stenosis, hernia, adhesions, fecal impaction, and foreign body[13,19]. Over 60% of cases of colonic obstruction are caused by colon malignancies[2,20], with the sigmoid colon and splenic flexure being the most prevalent locations[21]. In our study, the most common cause among the etiologies of colon involvement was colon cancer, and the most common location was the sigmoid colon. Volvulus is the second most common (10%-15%) cause of LBO. The second most frequent (10%–15%) cause of obstruction of the LB is volvulus. Volvulus is observed at low frequencies (< 1%) at the transverse colon and splenic flexure levels, but at high rates in the colon at the sigmoid (60%-75%) and cecum (25%-33%) levels[2,5]. According to our study, volvulus, which is localized at the sigmoid colon level, is the second most frequent cause of MO in the LB.
Anamnesis and physical exam results by themselves are insufficient for diagnosis and appropriate guidance; in cases of suspected BO, evaluation in conjunction with imaging techniques is crucial. However, depending on the extent of BO, diagnosis might be challenging even with advancements in abdominal imaging[22]. BO can be diagnosed using a variety of radiological modalities, including barium exams, enteroclysis, CT, ultrasound, and CR.
In patients presenting with abdominal pain and suspected BO, the primary objective of imaging is to detect possible obstruction, and CR is the first preferred imaging modality due to its low cost and low radiation exposure. The literature reports the diagnostic accuracy of CR for detecting BO to range from 46%-80%[3] and its sensitivity has been shown to range from 19%-86%[3,16,23]. The observed proportional difference may be attributed to variations in the severity of obstruction among the patients included in the studies.
CT is indicated for patients presenting with suspected BO in cases where the patient's clinical symptoms and initial CR findings are inconclusive. In order to effectively manage early treatment in cases of ileus, it is crucial to accurately determine the localization, etiology, severity of obstruction, transition point, and the presence of additional findings such as abnormal wall thickening, pneumatosis, strangulation, and pneumoperitoneum within the affected intestinal segment. Therefore, the utilization of a CT scan is imperative in order to validate the diagnosis and ascertain supplementary observations in contrast to CR[4]. CT has been documented to have a high diagnostic sensitivity (94%-100%) and diagnostic accuracy (90%-95%) for determining the presence and severity of complete or high-grade BO[24]. The diagnostic precision of CT is diminished when there is incomplete low-grade or intermittent obstruction. In such instances, enteroclysis and CT enteroclysis are the preferred approaches for assessing the existence and severity of BO[7].
In addition to established imaging techniques employed in CT, localizer radiographs, also referred to as scout, topogram, or scenogram images, and are acquired to facilitate identification of the initial and final positions of the scanning range. These radiographs rely on the anatomical landmarks of the patients to accurately determine the desired scan area[25]. CT scenogram images are a valuable contemporary implementation of conventional abdominal radiography. They serve the purpose of identifying supplementary information that aids in making a direct diagnosis of specific pathologies or narrowing down the differential diagnosis. This is achieved by examining findings both within and outside the scanned field of view. CT scenogram images can be utilized to assess many entities, including foreign substances (such as those that are undesirable, characterized by devices, or localized within the body), air-related findings (such as bowel gas pattern, pneumoperitoneum, and pneumatosis), calcifications, trauma/bone-related concerns, as well as soft tissues[26,27]. However, there have been reports indicating that scenogram images are eliminated from CT scanning examinations at a frequency of up to 75%, or alternatively, they are disregarded by a majority of radiologists when interpreting CT examinations[28-30]. In this study, the presence and possible location of the obstruction on abdominal CT scenograms, which can be used as the primary imaging modality in the diagnosis of acute BO, were contrasted with the final diagnosis, taking the observer's experience into account. There is only one study in the literature that examines the diagnostic accuracy of CT scenogram images in BO by different observers, taking into account the periods of experience. The diagnostic sensitivity reported in this study varies from 93% to 86%, with an average of 88%. These findings demonstrate a similarity to the results obtained for axial and axial plus coronal CT within the same investigation[11]. In our study, the evaluators' ability to accurately detect the existence of MO through the assessment of CT scenogram images exhibited a range of sensitivity values, spanning from 76.19% to 83.33%. The average sensitivity for diagnostic purposes was determined to be 80.94%.
The CT scenogram images can be classified into two categories based on the patterns of intestinal gas: Obstructive patterns and non-obstructive patterns. Imaging modalities of mechanical BO typically indicate decompressed loops in the distal region of the obstruction, as well as abnormally expanded bowel loops in the proximal region of the obstruction. Similar, imaging findings are present at levels showing distension on CT scenogram images. Supine CR images have characteristic findings expected in BO. The expected findings in an obstruction at the level of SB segments are enlarged air- or liquid-filled intestine with a diameter greater than 2.5-3 cm, colorectal gas deficiency, enlarged stomach, gasless abdomen, stretch sign, SB enlargement disproportionate to the colon, pseudotumor sign, etc. LBO is characterized by enlarged air- or liquid-filled bowel segments greater than 9 cm in the cecum and 6 cm in other levels of the colon, rectal gas deficiency, and SB dilatation, which may sometimes be accompanied by check valve system disorder[18]. These characteristic findings can also be identified in CT scenogram images.
Closed loop obstructions arise as a result of many factors such as adhesions, internal hernias, congenital malformations, or iatrogenic mesenteric deformities. These obstructions specifically affect a distinct segment and involve nearby sites of obstruction. In these instances, there exists a potential hazard of ischemia and necrosis resulting from total occlusion. While CT scenogram images may exhibit distinctive indicators of SBOs, similar to CRs, the proximal segment typically displays less tension and the closed loop segment tends to contain fluid, resulting in a normal or "non-specific" appearance on imaging[31].
Sigmoid volvulus refers to an abnormal bending of the sigmoid colon along its mesenteric axis, being the predominant type of colonic volvulus with a prevalence ranging from 60%-75% of cases[32]. In CT scenogram images, the characteristic inverted U-shaped swollen sigmoid colon pointing to the right upper quadrant seen on CRs, disproportionate sigmoid distension, proximal colon dilatation, absence of rectal gas or dilated sigmoid colon cephalo extension above the transverse colon (northern exposure), and sigmoid findings such as the 'coffee bean' sign describing the distandual segment with central coated walls can be identified[33,34]. It has been reported that an inverted U-shape can be seen in 86%-94% of cases[33,35] and the "coffee bean" sign can be seen in 76% of cases[33] in CT scenogram images.
Abdominal CT scans are frequently employed in the evaluation of patients who present with abdominal pain and are thought to have BO. These scans are commonly used to identify specific abnormalities, such as pneumoperitoneum and pneumatosis, which serve as indicators of the existence of severe or extensive obstruction. The evaluation of pneumoperitoneum presents challenges when using supine radiographs. In cases where there is suspicion, chest radiographs are primarily employed as they have the capability to detect even small amounts of intraperitoneal gas, as little as 1 mL[36]. The assessment of pneumoperitoneum is more challenging when using supine radiographs. However, several subtle features have been documented that could potentially indicate the existence of pneumoperitoneum. These findings are typically observed on CT scenogram images. These findings are: Rigler sign, right upper quadrant gas sign, falciform ligament sign, football sign, and inverted V sign[37,38]. Pneumatosis intestinalis is the presence of gas in the intestinal wall, and it is a warning sign for ischemia and impending perforation in the event of BO[32]. Pneumatosis typically appears as gas accumulation in the lower part of the intestine, whereas pseudopneumatosis refers to the entrapment of gas inside the stool's wall. This condition can provide a resemblance to genuine pneumatosis when observed using abdominal radiography or CT scenogram images. However, distinguishing between pseudopneumatosis and actual pneumatosis is more effectively achieved through the use of CT scans[39]. Portal venous gas is an additional indication of possible ischemia resulting from BO, which can be shown on CRs in situations of significant severity[40]. In our study, there were no cases with perforation-pneumoperiteneum, ischemia-pneumatosis findings secondary to severe MO.
The scarcity of research in the existing body of literature regarding the diagnosis of BO and the determination of the potential obstructed segment using CT scenogram images is evident. The insufficient attention provided by radiologists to these factors, together with their correlation to seniority level, underscores the significance of this research.
The retrospective nature of this study, the small number of patients, and the fact that, despite the high diagnostic accuracy of the results reported by the observers, they failed to provide clear indications of the criteria upon which they based their estimates constituted limitations. Other limitations of CT scenogram images include limited resolution, supine positioning, and two-dimensional planar presentation of complex three-dimensional anatomy. In addition, the fact that the female/male ratio is not suitable statistically for the comparison of parameters between genders is another limitation of this study. As the symptom and anamnesis information of most of the cases included in the study was not accessible, the evaluation was carried out mainly and only on radiological images. Incorporating clinical information into the evaluation process may alter study data.
This study revealed that the sensitivity and accuracy rates for detecting the presence and segmentation of MO on abdominal CT scenogram images were comparable to or greater than those observed in CR, particularly in relation to the radiologist's level of experience. While scenogram images are typically not given much attention during CT scans and are often disregarded by radiologists during interpretation, it is crucial to examine and incorporate any relevant data from CT scenogram images into the diagnostic report.
The effective management of ileus is heavily reliant on prompt and precise diagnosis, as a failure to achieve this may lead to adverse health outcomes and potential loss of life. While conventional radiography (CR) is commonly used as the primary imaging modality for patients with a preliminary diagnosis of ileus, its diagnostic accuracy in identifying the specific site and underlying cause of bowel obstruction (BO) is limited. Due to this constraint, computed tomography (CT) has emerged as the most suitable imaging modality in this particular situation.
CT scenogram images have the potential to assess several entities, encompassing air-related observations such as intestinal gas pattern, pneumoperitoneum, and pneumatosis. However, there are reports showing that scenogram images are omitted from CT scan examinations up to 75% of the time, or alternatively, ignored by the majority of radiologists when interpreting CT examinations. There exists a singular study within the literature that investigates the diagnostic sensitivity of CT scans in detecting BO, specifically considering the varying levels of expertise among different observers. Our intention was to make a scholarly contribution within this particular field of study.
This study aims to determine the presence of acute BO on abdominal CT scenogram images and the accuracy with which its possible location can be determined, taking into account the experience of the observers.
A retrospective screening was performed on a group of 46 people who arrived at the emergency room with acute abdominal pain between January 2021 and January 2022 and were subsequently evaluated for suspected ileus. The patients' abdominal CT images were evaluated at different intervals (1 mo apart) by three radiologists with varying degrees of expertise (1, 3, and 10 years). The assessment focused on establishing the presence or absence of BO as well as the likely location of the obstruction (small bowel or large bowel).
In the first evaluation by 3 radiologists to detect the presence of BO, the rate of detecting the presence of ileus due to mechanical obstruction (MO) was 80.94% and the diagnostic accuracy was 75.35%. Among all observers, the third observer had the highest sensitivity (83.33%), positive predictive value (94.59%), and diagnostic accuracy (80.43%). Considering the segmentation according to the final diagnosis at the first evaluation, the sensitivity (85.71%) and diagnostic accuracy (80.43%) values were highest in the senior observer's correct estimation of the large and small bowel segmentation. In the second evaluation, the senior observer's prediction of the presence of ileus and segmentation was more accurate than the other observers. Compared to the second evaluation, while there was no significant change in the rate of the first observer detecting the presence of ileus, there was an increase in the rate of correctly predicting the segmentation (73.91%). No significant change was detected in the other observers' estimates of the presence of MO and possible localization at different periods.
Our results show that the sensitivity and accuracy of abdominal CT scenogram images in detecting the presence and segmentation of acute MO in relation to seniority is similar to or higher than CR.
Considering the possible contribution of CT scenogram images to the diagnosis of some pathologies such as ileus, more studies are needed to diagnose these and similar pathologies and to narrow down the differential diagnosis.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine & medical imaging
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ciarambino T, Italy S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Herlinger H, Rubesin SE, Morris JB. Small bowel obstruction. In: Gore RM, Levine MS, editors. Textbook of gastrointestinal radiology. 2nd ed. Philadelphia, Pa: Saunders; 2000; 815–837. [DOI] [Full Text] |
| 2. | Welch JP. Bowel obstruction: differential diagnosis and clinical management. 1987. [DOI] [Full Text] |
| 3. | Maglinte DD, Reyes BL, Harmon BH, Kelvin FM, Turner WW Jr, Hage JE, Ng AC, Chua GT, Gage SN. Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol. 1996;167:1451-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 151] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Liu P, Zhu H, Zhang X, Feng A, Zhu X, Sun Y. Predicting Survival for Hepatic Arterial Infusion Chemotherapy of Unresectable Colorectal Liver Metastases: Radiomics Analysis of Pretreatment Computed Tomography. J Transl Int Med. 2022;10:56-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Gore RM, Miller FH, Pereles FS, Yaghmai V, Berlin JW. Helical CT in the evaluation of the acute abdomen. AJR Am J Roentgenol. 2000;174:901-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Maglinte DD, Heitkamp DE, Howard TJ, Kelvin FM, Lappas JC. Current concepts in imaging of small bowel obstruction. Radiol Clin North Am. 2003;41:263-283, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 95] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Suri S, Gupta S, Sudhakar PJ, Venkataramu NK, Sood B, Wig JD. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 127] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Balthazar EJ. George W. Holmes Lecture. CT of small-bowel obstruction. AJR Am J Roentgenol. 1994;162:255-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 146] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Karavas E, Ece B, Aydın S, Kocak M, Cosgun Z, Bostanci IE, Kantarci M. Are we aware of radiation: A study about necessity of diagnostic X-ray exposure. World J Methodol. 2022;12:264-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (8)] |
| 10. | Fatihoglu E, Aydin S, Gokharman FD, Ece B, Kosar PN. X-ray Use in Chest Imaging in Emergency Department on the Basis of Cost and Effectiveness. Acad Radiol. 2016;23:1239-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Jaffe TA, Martin LC, Thomas J, Adamson AR, DeLong DM, Paulson EK. Small-bowel obstruction: coronal reformations from isotropic voxels at 16-section multi-detector row CT. Radiology. 2006;238:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Markogiannakis H, Messaris E, Dardamanis D, Pararas N, Tzertzemelis D, Giannopoulos P, Larentzakis A, Lagoudianakis E, Manouras A, Bramis I. Acute mechanical bowel obstruction: clinical presentation, etiology, management and outcome. World J Gastroenterol. 2007;13:432-437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 158] [Cited by in RCA: 152] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Drożdż W, Budzyński P. Change in mechanical bowel obstruction demographic and etiological patterns during the past century: observations from one health care institution. Arch Surg. 2012;147:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Sabiston DC, Townsend CM, Beauchamp R, Evers BM, Mattox KL. Sabiston textbook of surgery: the biological basis of modern surgical practice: Wb Saunders Philadelphia; 2001. [DOI] [Full Text] |
| 15. | Jeffrey RB. Small bowel obstruction. In: Federle MP, Jeffrey RB, Woodward PJ, Borhani AA, eds. Diagnostic imaging: abdomen, 2nd ed. Salt Lake City, Utah: Amirsys, 2010; 44–47. [RCA] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 66] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Frager DH, Baer JW. Role of CT in evaluating patients with small-bowel obstruction. Semin Ultrasound CT MR. 1995;16:127-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Miller G, Boman J, Shrier I, Gordon PH. Etiology of small bowel obstruction. Am J Surg. 2000;180:33-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 276] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 18. | Paulson EK, Thompson WM. Review of small-bowel obstruction: the diagnosis and when to worry. Radiology. 2015;275:332-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 147] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 19. | Cappell MS, Batke M. Mechanical obstruction of the small bowel and colon. Med Clin North Am. 2008;92:575-597, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Biondo S, Parés D, Frago R, Martí-Ragué J, Kreisler E, De Oca J, Jaurrieta E. Large bowel obstruction: predictive factors for postoperative mortality. Dis Colon Rectum. 2004;47:1889-1897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 139] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Garcia-Valdecasas JC, Llovera JM, deLacy AM, Reverter JC, Grande L, Fuster J, Cugat E, Visa J, Pera C. Obstructing colorectal carcinomas. Prospective study. Dis Colon Rectum. 1991;34:759-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Matrawy KA, El-Shazly MJAJom. Intestinal obstruction: role of multi-slice CT in emergency department. 2014; 50: 171-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Shrake PD, Rex DK, Lappas JC, Maglinte DD. Radiographic evaluation of suspected small bowel obstruction. 1991; 86. [DOI] [Full Text] |
| 24. | Boudiaf M, Soyer P, Terem C, Pelage JP, Maissiat E, Rymer R. Ct evaluation of small bowel obstruction. Radiographics. 2001;21:613-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 90] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | American Association of Physicists in Medicine. AAPM CT Lexicon version 1.3. 2012. |
| 26. | Lee MH, Lubner MG, Mellnick VM, Menias CO, Bhalla S, Pickhardt PJ. The CT scout view: complementary value added to abdominal CT interpretation. Abdom Radiol (NY). 2021;46:5021-5036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Bian Y, Jiang H, Zheng J, Shao C, Lu J. Basic Pancreatic Lesions: Radiologic-pathologic Correlation. J Transl Int Med. 2022;10:18-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 28. | Daffner RH. Reviewing CT Scout Images: Observations of an Expert Witness. AJR Am J Roentgenol. 2015;205:589-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Berlin L. Reviewing the CT scout view: medicolegal and ethical considerations. AJR Am J Roentgenol. 2014;202:1264-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Berlin L. Medicolegal--malpractice and ethical issues in radiology. CT scout views and standard of care. AJR Am J Roentgenol. 2014;203:W741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Balthazar EJ, Birnbaum BA, Megibow AJ, Gordon RB, Whelan CA, Hulnick DH. Closed-loop and strangulating intestinal obstruction: CT signs. Radiology. 1992;185:769-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 168] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Jaffe T, Thompson WM. Large-Bowel Obstruction in the Adult: Classic Radiographic and CT Findings, Etiology, and Mimics. Radiology. 2015;275:651-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 107] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 33. | Levsky JM, Den EI, DuBrow RA, Wolf EL, Rozenblit AM. CT findings of sigmoid volvulus. AJR Am J Roentgenol. 2010;194:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 34. | Javors BR, Baker SR, Miller JA. The northern exposure sign: a newly described finding in sigmoid volvulus. AJR Am J Roentgenol. 1999;173:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Burrell HC, Baker DM, Wardrop P, Evans AJ. Significant plain film findings in sigmoid volvulus. Clin Radiol. 1994;49:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | James B, Kelly B. The abdominal radiograph. Ulster Med J. 2013;82:179-187. [PubMed] |
| 37. | Menuck L, Siemers PT. Pneumoperitoneum: importance of right upper quadrant features. AJR Am J Roentgenol. 1976;127:753-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 38. | Levine MS, Scheiner JD, Rubesin SE, Laufer I, Herlinger H. Diagnosis of pneumoperitoneum on supine abdominal radiographs. AJR Am J Roentgenol. 1991;156:731-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 78] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Wang JH, Furlan A, Kaya D, Goshima S, Tublin M, Bae KT. Pneumatosis intestinalis versus pseudo-pneumatosis: review of CT findings and differentiation. Insights Imaging. 2011;2:85-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Liebman PR, Patten MT, Manny J, Benfield JR, Hechtman HB. Hepatic--portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg. 1978;187:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 314] [Article Influence: 6.7] [Reference Citation Analysis (0)] |