Published online May 28, 2021. doi: 10.4329/wjr.v13.i5.122
Peer-review started: January 27, 2021
First decision: March 1, 2021
Revised: March 16, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: May 28, 2021
Processing time: 120 Days and 21.1 Hours
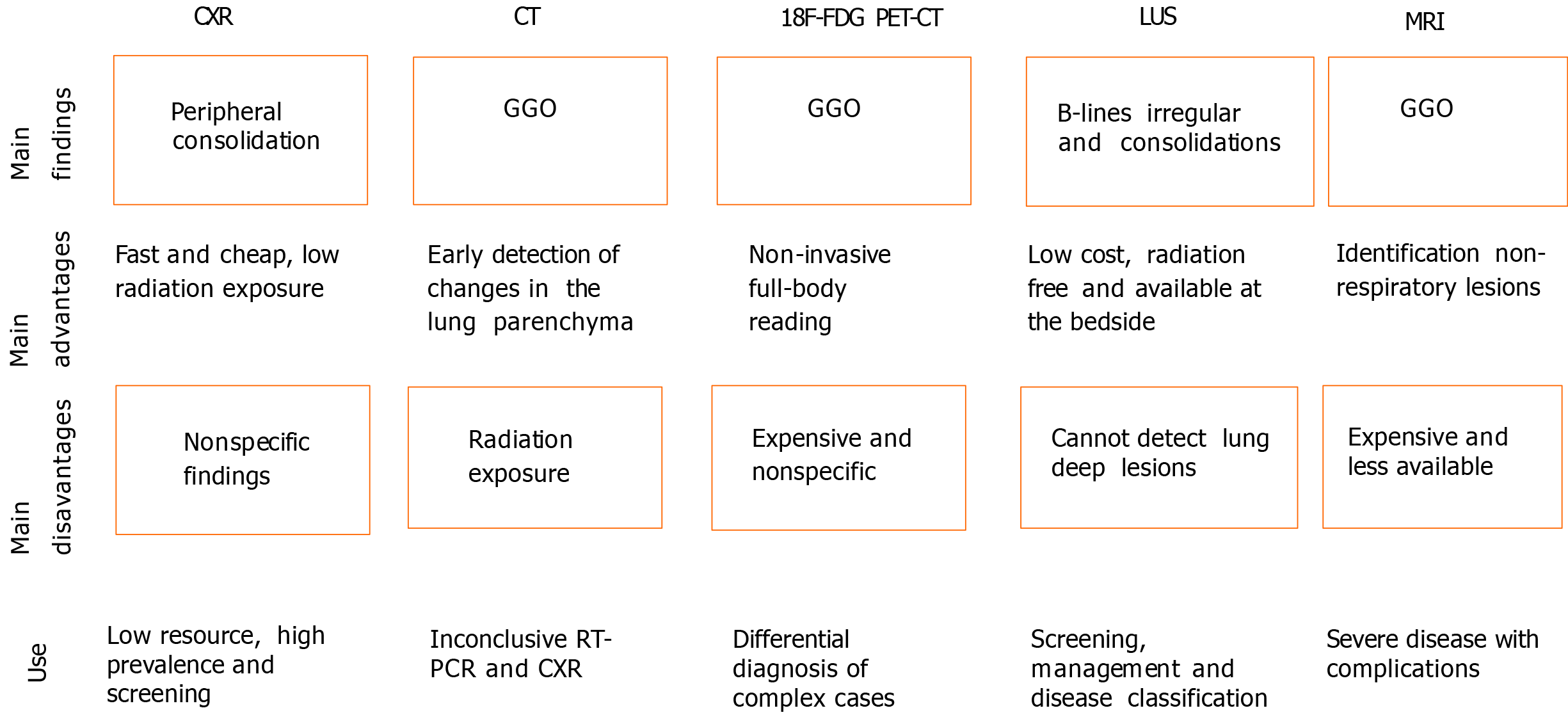
Coronavirus disease 2019 (COVID-19), a global emergency, is caused by severe acute respiratory syndrome coronavirus 2. The gold standard for its diagnosis is the reverse transcription polymerase chain reaction, but considering the high number of infected people, the low availability of this diagnostic tool in some contexts, and the limitations of the test, other tools that aid in the identification of the disease are necessary. In this scenario, imaging exams such as chest X-ray (CXR) and computed tomography (CT) have played important roles. CXR is useful for assessing disease progression because it allows the detection of extensive consolidations, besides being a fast and cheap method. On the other hand, CT is more sensitive for detecting lung changes in the early stages of the disease and is also useful for assessing disease progression. Of note, ground-glass opacities are the main COVID-19-related CT findings. Positron emission tomography combined with CT can be used to evaluate chronic and substantial damage to the lungs and other organs; however, it is an expensive test. Lung ultrasound (LUS) has been shown to be a promising technique in that context as well, being useful in the screening and monitoring of patients, disease classification, and management related to mechanical ventilation. Moreover, LUS is an inexpensive alternative available at the bedside. Finally, magnetic resonance imaging, although not usually requested, allows the detection of pulmonary, cardiovascular, and neurological abnormalities associated with COVID-19. Furthermore, it is important to consider the challenges faced in the radiology field in the adoption of control measures to prevent infection and in the follow-up of post-COVID-19 patients.
Core Tip: Imaging exams have played an important role in the current coronavirus disease 2019 pandemic. Thus, even though reverse transcription polymerase chain reaction is the gold standard method for the diagnosis, the use of computed tomography (CT) in the management of severe acute respiratory syndrome coronavirus 2-infected individuals has been highlighted. On the other hand, X-Ray, positron emission tomography combined with CT, and magnetic resonance imaging, along with ultrasound, can also assist in this process. We herein discuss the main evidence on the use of such exams and the challenges to the radiology field in that context as well.
- Citation: de Carvalho LS, da Silva Júnior RT, Oliveira BVS, de Miranda YS, Rebouças NLF, Loureiro MS, Pinheiro SLR, da Silva RS, Correia PVSLM, Silva MJS, Ribeiro SN, da Silva FAF, de Brito BB, Santos MLC, Leal RAOS, Oliveira MV, de Melo FF. Highlighting COVID-19: What the imaging exams show about the disease. World J Radiol 2021; 13(5): 122-136
- URL: https://www.wjgnet.com/1949-8470/full/v13/i5/122.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i5.122
In December 2019, several cases of a pneumonia of unknown cause with a clinical presentation compatible with conditions of viral etiology were reported in the city of Wuhan, Hubei province, China[1-4]. Later, it was found to be caused by a new type of coronavirus that was subsequently called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease came to be called coronavirus disease 2019 (COVID-19)[5,6]. Since then, the number of cases has increased, becoming a major outbreak and a global emergency[7,8]. By 19 January 2021, more than 93956883 cases and 2029084 deaths have been confirmed by the World Health Organization[9].
The SARS-CoV-2 is a β-coronavirus with spherical RNA and spike proteins that protrude on its surface[10]. It primarily infects the respiratory system but other organs such as the kidneys, heart, ileum, and spleen can also be infected[11]. The pathophysiological mechanisms involved in this process are complex, and includes virus attachment, recognition between specific cell receptors, and transmembrane Spike glycoprotein (S-protein) receptor-binding domain, along with protease cleaving by host cellular transmembrane serine protease (TMPRSS)[12]. Angiotensin-converting enzyme type 2 (ACE2) receptors are expressed in various human cells, including epithelial cells in the lungs, cardiomyocytes, neuronal and glial cells in the brain[13], glandular cells of the gastric, duodenal, and rectal epithelia, and enterocytes of the small intestine[14,15]. The main pathway by which SARS-CoV-2 enters cells is through the binding of S-protein to ACE2[14,15], and protein cleavage by enzymes, such as TMPRSS2[16].
The SARS-CoV-2 infection has variable clinical presentations, from asymptomatic to severe cases, which can lead to death[1,5]. The main symptoms involve fever, dry cough, dyspnea, and fatigue[17-20]. The gold standard diagnostic test for COVID-19 is the reverse transcription polymerase chain reaction (RT-PCR)[21,22]. However, due to the low availability of this diagnostic tool in some contexts, failures in sample collections, and the possibility of false-negative results, it has become necessary to use other methods to increase the accuracy of infection identification[23].
In this context, some imaging exams such as lung ultrasound (LUS), chest X-Ray (CXR), magnetic resonance imaging (MRI), and especially chest computed tomography (CT) have been very useful in the diagnosis of COVID-19[24]. It is noteworthy that in places of low prevalence of the disease or in asymptomatic individuals, imaging tests may have problems with false positive or missed detection. Thus, factors such as epidemiological data, clinical condition, laboratory tests and imaging exams can contribute to the screening of COVID-19, but for the final diagnosis the identification of viral RNA using RT-PCR is necessary[25,26].
CT is able to show important findings for early detection of the infection even when negative results are obtained in the RT-PCR, such as ground-glass opacities (GGO)[27]. It is worth mentioning that CXR is more often used in the evaluation of disease progression than in the detection of the infection itself due to its lower value in the early identification of GGO compared to CT[28]. LUS is a faster and safer method than the aforementioned methods and, even though it provides images with an inferior quality than those obtained with a CT scan, it has become very useful due to its practicality, as it is possible to perform this technique at the patient's bedside, whereas the other procedures involve displacement and longer periods of time[29]. Of course, all available resources for patient care should always be taken into consideration, but when dealing with a pandemic, it is of unequal importance to thoroughly evaluate aspects related to the speed and efficiency of diagnostic methods[30].
In the initial phase of the COVID-19 outbreak, when RT-PCR tests had limited availability, countries presented divergent opinions regarding the use of imaging exams in the diagnosis of the infection worldwide. With the increase in the availability of RT-PCR kits throughout the pandemic, the criteria for the use of imaging tests began to gain consensus. But, it is worth mentioning that the national guidelines vary according to factors such CT scanner availability, personal protective equipment availability, and in vitro testing infrastructure[31]. Therefore, this review aims to describe the use of imaging exams for the detection of COVID-19, providing a broad overview on the main methods used in this context and discussing the challenges in the radiology field during the pandemic.
Although the detection of SARS-CoV-2 RNA using the RT-PCR remains the gold standard diagnostic method, the unspecific or asymptomatic initial stage of COVID-19 highlights the important role of imaging exams in assisting the early diagnosis, as well as in monitoring and identifying complications[32,29]. Figure 1 summarizes the main points regarding the imaging modalities used in COVID-19.
The reduced capacity of CXR to reveal GGO, an early finding in the disease, limits its use in COVID-19 diagnosis. However, extensive consolidations, which are visible in the CXR, are common as the disease progresses[33].
Despite the sparse data in the literature on radiography in the COVID-19 context[34], the consolidation is the most common finding in the radiographs of infected patients, being predominantly observed in peripheral areas of the lower zones[35], with a peak of severity 10-12 d after the onset of symptoms[36]. Among 9 patients in Korea, the CXR detected parenchymal abnormalities in three of them, most with peripheral consolidation that was later confirmed by CT[37]. Moreover, a severity score can be used to quantify the extent of infection, with a score assigned to each lung that ranges from 0 to 4 according to the extent of lung involvement: 0 = no involvement; 1 corresponding to less than 25%; 2 = 25%-50%; 3 = 50%-75% and 4 to more than 75%. The scores obtained for each lung are then added together to provide the final gravity points[36].
A study published in October 2020 showed that chest radiographs may be reliable in predicting results from definitive COVID-19 diagnostic methods, particularly in places with limited resources and a high number of cases[38]. Radiography is the fastest and cheapest method to evaluate COVID-19 patients and it is broadly available in clinics, emergency rooms, and hospitals worldwide[39,40]. Moreover, this method is associated with a low exposure to ionizing radiation in users. In addition, the portable X-Ray units, whose mobility and cleaning are easy, have been considered as facilitating resources in emergencies[41].
However, the CXR abnormalities observed in COVID-19 are nonspecific and may overlap with findings from other infectious diseases such as influenza[42,43]. Thus, the analysis of imaging patterns on chest radiography in SARS-CoV-2 infection is complex, time-consuming, and prone to error. This evaluation is a challenge that must be considered, mainly due to the lack of specialized radiologists[39,41]. Therefore, an artificial intelligence (AI) algorithm could be used and programmed to distinguish COVID-19 pneumonia from non-COVID-19 pneumonia through CXR images[44]. The main goal of AI, when gathering imaging data and clinical information is to read image studies accurately, preferably as a screening tool[34].
A study observed sensibility and specificity of 95% and 71%, respectively, for the association between COVID-19 pneumonia with the involvement of 4 or more zones and clinical deterioration, in both critical and non-critical patients[45]. An analysis performed to determine the CXR diagnostic precision in comparison to RT-PCR in 569 patients with suspected SARS-CoV-2 infection showed, in the initial CXR, 61% sensibility and 76% specificity in the hospital environment[46]. In November 2020, an evaluation of the CXR associated with AI support for COVID-19 detection reported an increase in the diagnostic sensibility from 47% to 61%, even though the specificity reduced from 79% to 75%. This is a promising result for the possible use of AI to enhance the accuracy of this exam[39]. In conclusion, the CXR may be indicated in situations of low resources and high prevalence of the disease.
There is a vast amount of information regarding CT findings in COVID-19 reported in different studies around the world[47]. It is known that the characteristics of the lung fields at CT scan change over time, with different presentations according to the stage and severity of the pulmonary infection[48].
The main feature found on a CT scan as a consequence of COVID-19 is the presence of GGO, with a predominantly bilateral and peripheral distribution[49]. Vascular enlargement is seen in GGO, representing interstitial peribronchovascular edema/inflammation and possible increased cardiac diameter[50].
In the initial stage of COVID-19, chest CT is characterized by single or multiple scattered patchy or agglomerated GGOs[51]. Subsequently, there may be an increase in the number and extent of lesions[52]. As far as the disease progresses, images show diffuse consolidation of the lungs, air bronchograms, and bronchial dilation. The resolution of the GGO and pulmonary consolidation occurs gradually, with some residual opacities remaining characteristic of fibrosis[53].
Chest CT may be useful for early diagnosis in cases of clinical suspicion, indefinite pulmonary abnormalities on CXR, and unavailable or negative RT-PCR test, and in the follow-up of severe cases[54].
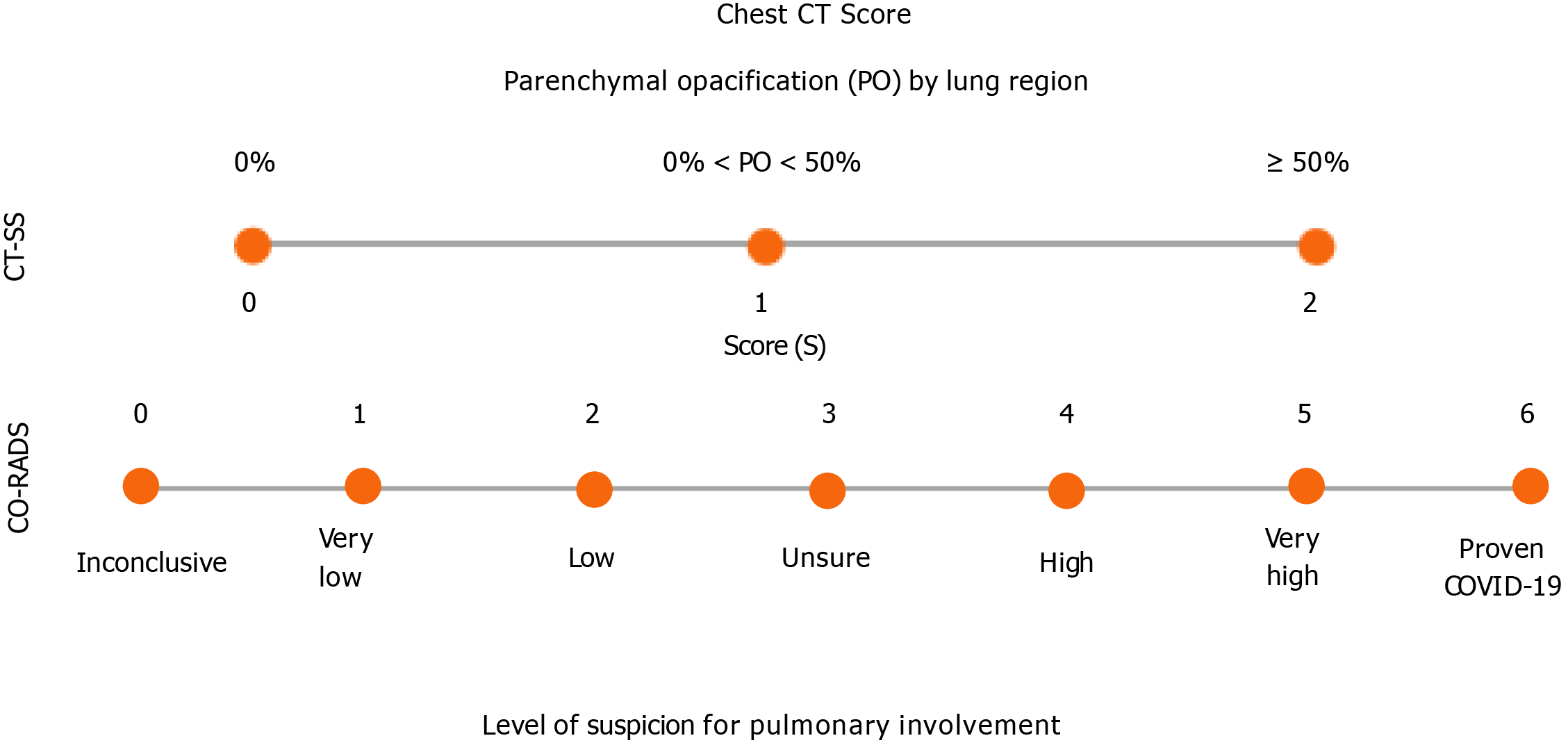
A study used a chest CT severity score (CT-SS) that is based on the sum of scores from 20 regions of the lung. Each region receives a score from 0 to 2 according to the intensity of parenchymal opacification. A CT-SS threshold value of 19.5 was identified as a reliable cut-off to detect severe COVID-19, suggesting that this method may be useful in identifying people who need hospitalization[55]. Another method that aims to facilitate and standardize the assessment of patients with moderate-to-severe symptoms of COVID-19 on CT images is the COVID-19 reporting and data system (CO-RADS), which is determined according to the level of suspicion of pulmonary involvement, varying from CO-RADS 1 (very low) to CO-RADS 5 (very high). Moreover, there are some extra classifications: CO-RADS 0 for technically insufficient tests and CO-RADS 6 for cases confirmed by RT-PCR[56]. Figure 2 summarizes the aforementioned scores.
Compared with the CXR, CT is more sensitive for detecting changes in the lung parenchyma in the early stages of the disease, besides enabling the monitoring of disease progression and possible differential diagnoses[57]. However, special attention is needed for non-infectious etiologies and other infectious causes, such as non-COVID-19 viral pneumonia, Mycoplasma pneumoniae, Pneumocystis jiroveci, and pulmonary granulomatous infections that may be similar to CT findings in COVID-19. In these cases, clinical manifestations, laboratory tests, and immunological status should also be considered to assist in the differential diagnosis[58].
Furthermore, evidence shows that some patients with a CT pattern suggestive of COVID-19 pneumonia initially have a negative RT-PCR test result, suggesting the need to repeat the diagnostic tests if there is high clinical suspicion[59]. In this sense, it is even considered that chest CT should be performed in symptomatic patients who will undergo surgery in a context that requires a quick diagnosis and RT-PCR is not available. This is important considering the high perioperative mortality of patients infected with SARS-CoV-2[60].
Despite the potential advantages of CT, factors such as the period needed to clean the imaging exam rooms, the risk of viral transmission for healthcare professionals, and radiation exposure to the patient must also be considered[61]. There is no standard for the radiation dose in cases of COVID-19, but some studies suggest single-phase, non-contrast, low-dose chest CT, which varies depending on factors such as the patient’s body habitus, in those of small and medium size, for example, volume CT dose index < 3 mGy can be sufficient[62].
Regarding diagnostic accuracy, a meta-analysis that included studies with high-risk patients for COVID-19 reported a relatively high sensitivity of chest CT ranging from 92.9% to 97%, whereas specificity was poor, varying from 25% to 71.9%[63]. It is important to emphasize that these studies are influenced by several factors such as patient selection, disease prevalence, and medical interpretation, influencing the generalization of these results[64]. A French study[65], for example, suggested that chest CT has an important role in early diagnosis in areas with a high prevalence of COVID-19. However, Kim et al[66] indicated that in low-prevalence settings, many false positives can occur with the use of chest CT. Table 1 summarizes diagnostic accuracy values of CXR and CT for COVID-19.
Although positron emission tomography combined with CT (PET/CT) and the use of 18F-fluorodeoxyglucose (18F-FDG) tracer in PET/CT are more complex than a simple chest CT, these imaging exams can provide morphological and functional information on infectious and inflammatory diseases[67]. The cells of the inflammatory process pick up 18F-FDG, which showed potential in the differential diagnosis of complex cases, as well as lung lesions caused by SARS-CoV-2[68].
18F-FDG PET/CT plays an important role in the evaluation of infectious and inflammatory lung diseases, including the detection of involved pulmonary segments, estimating the extent of the lesion, monitoring progression and responses to treatment[69]. In COVID-19, PET/CT could be used as a non-invasive full-body reading to assess chronic and substantial damage to the lungs and other organs[68]. In a previous study, 38.46% of patients submitted to 18F-FDG PET/CT were diagnosed with COVID-19 before undergoing RT-PCR. Therefore, the authors concluded that the test can possibly identify SARS-CoV-2 infection when the findings, clinical history, and epidemiological context are related[70]. Moreover, this exam should also be done to evaluate the impact of possible damage, especially in patients from groups at increased risk for severe disease who present with respiratory symptoms[71]. Previous studies have reported that the main COVID-19 imaging findings were accidentally detected in cancer patients submitted to the exam[72,73]. When these findings were correlated with clinical and epidemiological data, they strongly suggested the SARS-CoV-2 infection[70], facilitating the patient’s management.
The main imaging findings reported using 18F-FDG PET/CT in COVID-19 are the presence of GGOs with areas of focal consolidation, mainly in the peripheral regions, as well as an interlobular septal thickening in one or both lungs[74,75]. Furthermore, positive 18F-FDG lymph nodes in the mediastinal, hilar, and subclavian regions can also be observed[74]. In the early stages, COVID-19 pneumonia presents with segmental GGO and nodal involvement in the peripheral and posterior regions of the lungs, while disease progression is accompanied by an increase in the number of lesions as well as in their extension and density. In addition, a mosaic paving pattern and air bronchogram sign have also been identified[76].
The 18F-FDG PET/CT exam has important disadvantages. The test is still expensive and inaccessible for some people, especially those living in poor countries[77]. In addition, the low physical half-life, approximately 110 min, of 18F-FDG is a problem, because this limitation prevents the examination from being carried out in places distant from the producers of this tracer[78]. Another important difficulty associated with the use of this substance is that it is unable to differentiate distinct populations of immune cells and it is not specific for viral infections[72]. Thus, these limitations are very relevant when considering performing this exam.
The level of accuracy of this imaging exam in the diagnosis of COVID-19 is still uncertain. Therefore, further studies using larger cohorts are needed to understand the usefulness of this exam in COVID-19[68]. Of note, the long-term follow-up of patients is very important to identify possible chronic damage caused by COVID-19 and the role of 18F-FDG PET/CT in detecting such damage[71].
LUS has evolved over the years in the diagnosis of lung diseases, becoming in the current COVID-19 pandemic an alternative mode of first-line imaging because it is a viable and highly accurate imaging exam when used at the bedside[79]. It has the advantage of being an economical alternative, more accessible to low and middle-income countries, available at the bedside, in real time, and free of radiation risks[30,80]. LUS can also assist in the screening of symptomatic patients, classification of disease severity, monitoring of patients with pulmonary findings, management related to mechanical ventilation, and treatment allocation and evaluation[81].
The challenges of using ultrasound include prolonged operator exposure and the need for scanner plates and transducers that need to be completely disinfected, in addition, another limitation of this exam is that it cannot detect deep lesions in the lung[81,82]. Although a limited number of studies have evaluated this method in COVID-19, this procedure has high sensitivity and a high level of accuracy as a diagnostic tool for pneumonia, with a sensitivity of 93% and a specificity of 95% in the evaluation of patients with the disease. Some studies have also shown high sensitivity (93%-98%) for acute respiratory distress syndrome[82]. Thus, LUS is comparable to CT, but CT shows intra-pulmonary and apical lesions more clearly and comprehensively than LUS[29]. LUS is considered advantageous for detecting smaller lesions and peripulmonary effusions as well as pleural injuries, and is a dynamic and easily accessible method[34].
The evaluation of patients with COVID-19 using LUS often shows signs that include various forms of B-lines (often separated and coalescing), an irregular or fragmented pleural line, subpleural consolidations, pleural effusions, and absence of pulmonary slippage. These findings are variable and non-pathognomonic for SARS-CoV-2 infection[34]. The specificity for this disease occurs when irregular bilateral vertical artifacts and multifocal white lung signs are present, suggesting interstitial-alveolar damage[83]. The demonstration of B-lines are described as laser-like hyperechoic artifacts that resemble a "comet tail" or "light beam" and have been commonly observed in cases of COVID-19 pneumonia; these B-lines may be associated with an interstitial syndrome and decreased aeration and when the confluents may appear as a "white lung" equivalent to the frosted glass opacities of CT. These characteristics suggest a more severe loss of lung aeration[84,29].
LUS has been a promising alternative, which can be performed very quickly, is non-invasive, can be used to identify probable COVID-19 patients in association with RT-PCR and to identify pulmonary involvement and possible complications, differentiating acute signs of respiratory failure from normal function[80,85]. These characteristics aid in the management of the patient, whether in defining the need for hospitalization, ventilation or another specific therapy, and of great importance in the current pandemic[85].
MRI is not often performed in COVID-19, unlike CT[86]. However, when requested, a thoracic MRI is obtained with the respiratory navigator during the expiratory phase, thus providing valuable information for clinical evaluation[87]. MRI allows the detection of minute and fine aspects of the pulmonary parenchyma. Moreover, it detects pleural effusion and lymphadenopathy, and is a promising diagnostic tool in the detection of pulmonary nodules[88].
The most common finding in the thoracic MRI scan is GGO, which comes up due to slight interstitial thickening, edema, and hyaline membranes in the lung and may come together to form interlobular septum consolidation. This consolidation in COVID-19 occurs when there is increased density in the alveoli, and is multifocal, segmental, irregular, subpleural or peribroncovascular[88,89].
Due to the presence of the ACE2 receptor in other systems, the affinity between SARS-CoV-2 and ACE2, as well as other systemic consequences of this infection, can lead to cardiotoxicity and cardiovascular injury or thromboembolic event[90]. For this reason, greater attention should be paid to the possibility of some myocardial involvement even in recovered patients who had cardiac symptoms[91]. Within this framework, MRI has been of great value in patients with cardiovascular conditions, such as arrhythmias, fulminant myocarditis, and acute coronary syndromes[92].
In this context, cardiovascular MRI (CMR) allows the visualization of several myocarditis characteristics, such as contractile dysfunction, inflammatory edema, pulmonary artery filling defects, and necrosis[92,93]. The main methods are conventional cine images, T2-weighted sequences, parametric T1 and T2 maps, and late gadolinium enhanced images. Thus, CMR allows an anatomical and functional evaluation, revealing the different patterns of cardiac tissue damage, whether inflammatory or ischemic[93].
Moreover, MRI has become a very efficient tool in the investigation of a possible relationship between SARS-CoV-2 and nervous system abnormalities. Some studies have already suggested a neurotropism of the virus in infected patients who present with persistent severe anosmia and dysgeusia[94]. In this context, significant differences are observed in the signal intensity emitted at MRI of the olfactory bulb in patients with anosmia, presenting a T2/FLAIR hyperintensity[95].
The olfactory bulb MRI is very enlightening as it provides visualization of anatomical details and allows monitoring of the volume reduction of the bulb and respiratory tract that is directly linked to the clinical picture and presentation of anosmia[96]. This finding may be related to an initial inflammatory reaction of the nasal mucosa by the virus, as well as in the neuroepithelium of the olfactory fissure, in patients with a total loss of smell, affecting neural smell as was noted on MRI of anosmic patients[95].
It is important to note that, despite its importance, MRI is less available and more expensive than CT. However, its use is essential in the screening and monitoring of some serious neurological complications resulting from COVID-19 such as stroke, encephalitis, encephalopathy, and Guillain Barré syndrome[97].
The main indications for MRI are cases with worsening of the disease such as in the occurrence of acute necrotizing encephalopathy, with medial portion hypersignal of the thalamus on T2-weighted MRI and FLAIR sequences as well as in the subinsular region and medial portion of the temporal lobes from gadolinium ring uptake on T1-weighted sequences[89]. Furthermore, the aforementioned radiological signals are often detected in patients seeking MRI for other reasons. Thus, the radiologist’s ability to recognize those characteristic findings is crucial to detect them even in patients without a prior COVID-19 diagnosis[86].
Radiologists, as they are among the health professionals exposed to COVID-19, must be aware of the infection control protocols, in order to prevent viral spreading among patients or between patients and healthcare professionals[31,98].
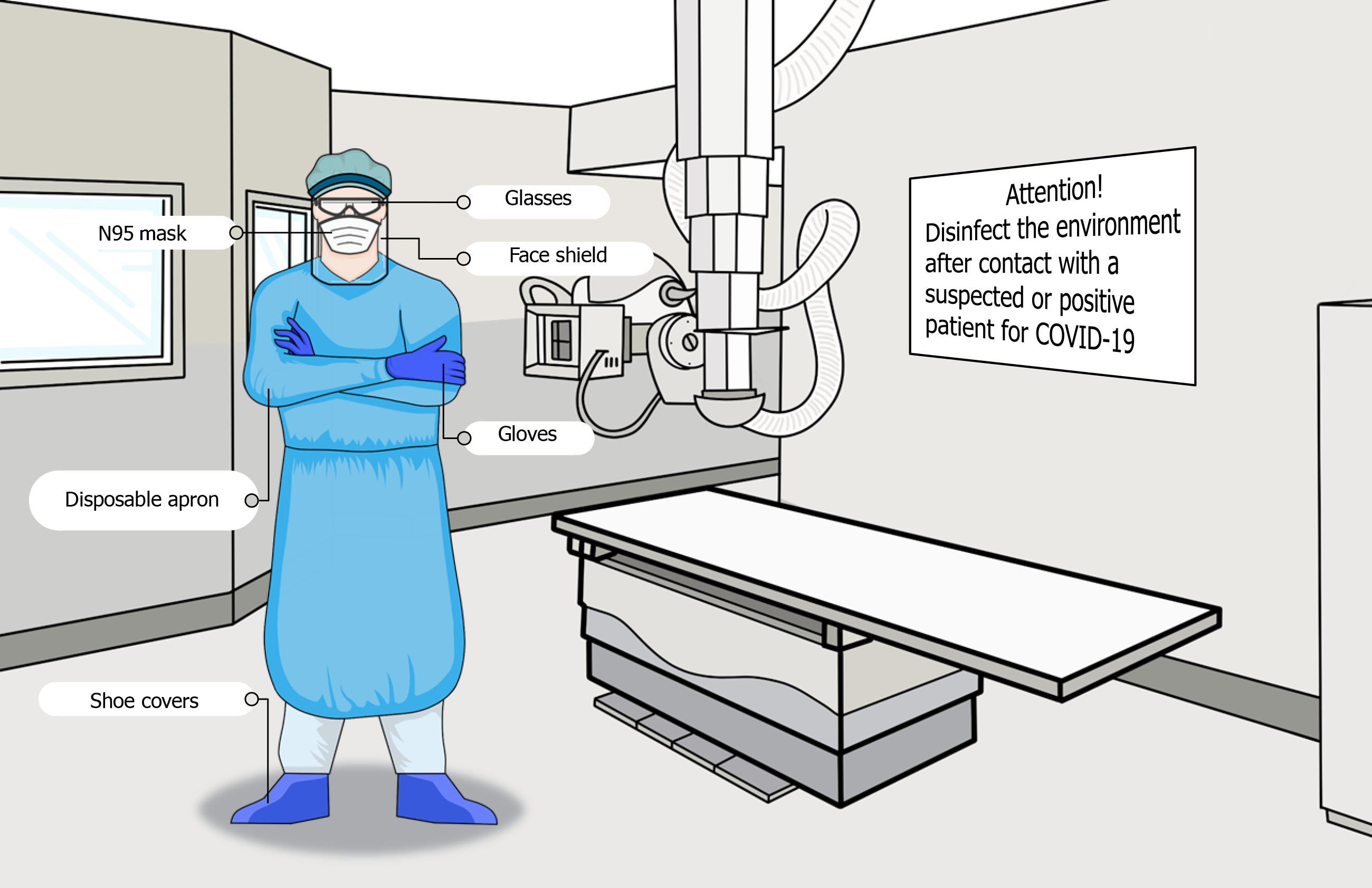
Firstly, an infection control team should be established for the radiology department[99]. It is important to use personal protection equipment (PPE), which is divided into categories according to the radiologists’ contact with patients[99]. In this sense, disposable protective caps, surgical masks, and goggles must be worn by everyone, as well as good hand hygiene[100]. For health professionals whose protection is level one, that is, people who manage registration and screening for review, disposable latex gloves and, if possible, N95 masks are recommended[100]. In levels two and three, which include those who perform diagnostic examinations such as X-Ray and CT in confirmed or suspected patients, should use the aforementioned PPE, plus a face shield as well as a disposable apron and shoe protectors[101,102]. Moreover, the people who are responsible for cleaning equipment and places, and those involved in the safe disposal of infectious medical waste, must use level two PPE[103]. Figure 3 illustrates the PPE indicated to prevent infection in the radiology room.
The removal of clothing should be carried out after contact with suspected or confirmed individuals, and new PPE is required to proceed with a new service. The patients must always wear surgical masks[101,103]. The equipment and the environment that the patient had contact with must undergo a decontamination process[82], using soap and water or a disinfectant such as alcohol and, after cleaning, it is recommended that the room be left unused for 1 h for air circulation[43,99].
Another challenge that emerges for the radiologists during the pandemic is the post-infection follow-up, i.e., to control complications and assist patients during recovery. Given the lack of concrete evidence on the long-term effects of COVID-19, the British Thoracic Society guidelines determined two follow-up algorithms[104]: (1) In patients who had the most severe COVID-19 pneumonia, it is suggested that a clinical review should be conducted between 4 to 6 wk after discharge and, if CXR still shows abnormalities, new radiography must be performed within 6-8 wk; (2) In patients who had mild or moderate COVID-19 pneumonia, it is suggested that CXR be performed 12 wk after discharge[105].
However, a study of 110 patients followed for 8 to 12 wk after admission, pointed out that CXRs are not necessary in those who did not need oxygen during infection, because they are unlikely to present any abnormalities[106].
Another study noted that point-of-care ultrasound findings, performed after hospital discharge, assist in monitoring the progress of severe COVID-19 pneumonia. During follow-up, besides LUS, chest CT was used for patients with suspected residual lung injury as well as CT pulmonary angiography and echocardiography for patients with residual thromboembolic disease[107].
The COVID-19 pandemic has brought several challenges to health care systems. Due to the high rate of viral transmission, early diagnosis is essential to monitor and isolate the patient, reducing the risk of further contamination. In the initial phase of the pandemic, with the limited availability of RT-PCR tests, imaging techniques were important tools to assist in the diagnosis of COVID-19. Even with the improved availability of RT-PCR tests, over time, imaging remains useful not only for diagnosis but also for assessing disease progression and severity. Even in countries with financial and technical difficulties, imaging exams, if well managed, can assist in the diagnosis and monitoring of patients, enabling better results and reducing health costs. As the pandemic advances, some challenges are perpetuated, such as the need to maintain control to prevent and reduce risks of contamination in the radiology department, and others arise, such as the monitoring of post-COVID-19 patients. However, different to the initial phase of the pandemic, accumulated knowledge has enabled a better understanding of the main imaging findings associated with COVID-19 and the regional guidelines provide guidance on the proper use of imaging modalities considering the reality of each location. In addition, the use of AI has contributed to a more accurate diagnosis in the radiology field.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhu CW S-Editor: Fan JR L-Editor: Webster JR P-Editor: Wang LL
| 1. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30086] [Article Influence: 6017.2] [Reference Citation Analysis (3)] |
| 2. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17619] [Article Influence: 3523.8] [Reference Citation Analysis (0)] |
| 3. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18184] [Article Influence: 3636.8] [Reference Citation Analysis (0)] |
| 4. | Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol. 2020;92:401-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1670] [Cited by in RCA: 1768] [Article Influence: 353.6] [Reference Citation Analysis (0)] |
| 5. | Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536-544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5202] [Cited by in RCA: 4629] [Article Influence: 925.8] [Reference Citation Analysis (0)] |
| 6. | Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3736] [Cited by in RCA: 3194] [Article Influence: 638.8] [Reference Citation Analysis (0)] |
| 7. | Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3213] [Cited by in RCA: 2653] [Article Influence: 530.6] [Reference Citation Analysis (0)] |
| 8. | Phelan AL, Katz R, Gostin LO. The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. JAMA. 2020;323:709-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 774] [Cited by in RCA: 744] [Article Influence: 148.8] [Reference Citation Analysis (6)] |
| 9. | World Health Organization. Geneva: 2020. Weekly operational update on COVID-19. [cited 19 January 2021]. Available from: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19---19-january-2021. |
| 10. | Ashour HM, Elkhatib WF, Rahman MM, Elshabrawy HA. Insights into the Recent 2019 Novel Coronavirus (SARS-CoV-2) in Light of Past Human Coronavirus Outbreaks. Pathogens. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 389] [Cited by in RCA: 356] [Article Influence: 71.2] [Reference Citation Analysis (1)] |
| 11. | Kabir MT, Uddin MS, Hossain MF, Abdulhakim JA, Alam MA, Ashraf GM, Bungau SG, Bin-Jumah MN, Abdel-Daim MM, Aleya L. nCOVID-19 Pandemic: From Molecular Pathogenesis to Potential Investigational Therapeutics. Front Cell Dev Biol. 2020;8:616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 12. | Gu J, Han B, Wang J. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology. 2020;158:1518-1519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 954] [Cited by in RCA: 949] [Article Influence: 189.8] [Reference Citation Analysis (1)] |
| 13. | Villapol S. Gastrointestinal symptoms associated with COVID-19: impact on the gut microbiome. Transl Res. 2020;226:57-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 217] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 14. | Wong SH, Lui RN, Sung JJ. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35:744-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 445] [Article Influence: 89.0] [Reference Citation Analysis (0)] |
| 15. | Lai CC, Ko WC, Lee PI, Jean SS, Hsueh PR. Extra-respiratory manifestations of COVID-19. Int J Antimicrob Agents. 2020;56:106024. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 204] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 16. | Stopsack KH, Mucci LA, Antonarakis ES, Nelson PS, Kantoff PW. TMPRSS2 and COVID-19: Serendipity or Opportunity for Intervention? Cancer Discov. 2020;10:779-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 287] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 17. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12966] [Article Influence: 2593.2] [Reference Citation Analysis (1)] |
| 18. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14756] [Article Influence: 2951.2] [Reference Citation Analysis (0)] |
| 19. | Zhang G, Zhang J, Wang B, Zhu X, Wang Q, Qiu S. Analysis of clinical characteristics and laboratory findings of 95 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a retrospective analysis. Respir Res. 2020;21:74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 192] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 20. | Yan Y, Shin WI, Pang YX, Meng Y, Lai J, You C, Zhao H, Lester E, Wu T, Pang CH. The First 75 Days of Novel Coronavirus (SARS-CoV-2) Outbreak: Recent Advances, Prevention, and Treatment. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 138] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 21. | Tahamtan A, Ardebili A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev Mol Diagn. 2020;20:453-454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 594] [Cited by in RCA: 702] [Article Influence: 140.4] [Reference Citation Analysis (0)] |
| 22. | Carvalho ARVS, Cezarotti Filho ML, Azevedo PCP, Silveira Filho RN, Barbosa FT, Rocha TJM, Sousa-Rodrigues CF, Ramos FWDS. Epidemiology, diagnosis, treatment, and future perspectives concerning SARS-COV-2: a review article. Rev Assoc Med Bras (1992). 2020;66:370-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Aljondi R, Alghamdi S. Diagnostic Value of Imaging Modalities for COVID-19: Scoping Review. J Med Internet Res. 2020;22:e19673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (2)] |
| 24. | Güneyli S, Atçeken Z, Doğan H, Altınmakas E, Atasoy KÇ. Radiological approach to COVID-19 pneumonia with an emphasis on chest CT. Diagn Interv Radiol. 2020;26:323-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 25. | Meng X, Liu Y. Chest Imaging Tests versus RT-PCR Testing for COVID-19 Pneumonia: There Is No Best, Only a Better Fit. Radiology. 2020;297:E345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Akl EA, Blažić I, Yaacoub S, Frija G, Chou R, Appiah JA, Fatehi M, Flor N, Hitti E, Jafri H, Jin ZY, Kauczor HU, Kawooya M, Kazerooni EA, Ko JP, Mahfouz R, Muglia V, Nyabanda R, Sanchez M, Shete PB, Ulla M, Zheng C, van Deventer E, Perez MDR. Use of Chest Imaging in the Diagnosis and Management of COVID-19: A WHO Rapid Advice Guide. Radiology. 2021;298:E63-E69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 113] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 27. | Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for Typical Coronavirus Disease 2019 (COVID-19) Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020;296:E41-E45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1213] [Cited by in RCA: 1209] [Article Influence: 241.8] [Reference Citation Analysis (1)] |
| 28. | Pascarella G, Strumia A, Piliego C, Bruno F, Del Buono R, Costa F, Scarlata S, Agrò FE. COVID-19 diagnosis and management: a comprehensive review. J Intern Med. 2020;288:192-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 702] [Cited by in RCA: 732] [Article Influence: 146.4] [Reference Citation Analysis (0)] |
| 29. | Gandhi D, Ahuja K, Grover H, Sharma P, Solanki S, Gupta N, Patel L. Review of X-ray and computed tomography scan findings with a promising role of point of care ultrasound in COVID-19 pandemic. World J Radiol. 2020;12:195-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Aquino EML, Silveira IH, Pescarini JM, Aquino R, Souza-Filho JA, Rocha AS, Ferreira A, Victor A, Teixeira C, Machado DB, Paixão E, Alves FJO, Pilecco F, Menezes G, Gabrielli L, Leite L, Almeida MCC, Ortelan N, Fernandes QHRF, Ortiz RJF, Palmeira RN, Junior EPP, Aragão E, Souza LEPF, Netto MB, Teixeira MG, Barreto ML, Ichihara MY, Lima RTRS. Social distancing measures to control the COVID-19 pandemic: potential impacts and challenges in Brazil. Cien Saude Colet. 2020;25:2423-2446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 272] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 31. | Tan BS, Dunnick NR, Gangi A, Goergen S, Jin ZY, Neri E, Nomura CH, Pitcher RD, Yee J, Mahmood U. RSNA International Trends: A Global Perspective on the COVID-19 Pandemic and Radiology in Late 2020. Radiology. 2021;299:E193-E203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Bhat R, Hamid A, Kunin JR, Saboo SS, Batra K, Baruah D, Bhat AP. Chest Imaging in Patients Hospitalized With COVID-19 Infection - A Case Series. Curr Probl Diagn Radiol. 2020;49:294-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 33. | Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, Zhang LJ. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020;296:E15-E25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1106] [Cited by in RCA: 950] [Article Influence: 190.0] [Reference Citation Analysis (1)] |
| 34. | Kaufman AE, Naidu S, Ramachandran S, Kaufman DS, Fayad ZA, Mani V. Review of radiographic findings in COVID-19. World J Radiol. 2020;12:142-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 35. | Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, Lui MM, Lo CS, Leung B, Khong PL, Hui CK, Yuen KY, Kuo MD. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol Cardiothorac Imaging. 2020;2:e200034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 604] [Cited by in RCA: 474] [Article Influence: 94.8] [Reference Citation Analysis (0)] |
| 36. | Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72-E78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 832] [Cited by in RCA: 825] [Article Influence: 165.0] [Reference Citation Analysis (1)] |
| 37. | Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, Park CM, Kim YH. Chest Radiographic and CT Findings of the 2019 Novel Coronavirus Disease (COVID-19): Analysis of Nine Patients Treated in Korea. Korean J Radiol. 2020;21:494-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 431] [Cited by in RCA: 374] [Article Influence: 74.8] [Reference Citation Analysis (0)] |
| 38. | Cellina M, Panzeri M, Oliva G. Chest Radiography Features Help to Predict a Favorable Outcome in Patients with Coronavirus Disease 2019. Radiology. 2020;297:E238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 39. | Dorr F, Chaves H, Serra MM, Ramirez A, Costa ME, Seia J, Cejas C, Castro M, Eyheremendy E, Fernández Slezak D, Farez MF; Study Collaborators. COVID-19 pneumonia accurately detected on chest radiographs with artificial intelligence. Intell Based Med. 2020;3:100014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Zhang R, Tie X, Qi Z, Bevins NB, Zhang C, Griner D, Song TK, Nadig JD, Schiebler ML, Garrett JW, Li K, Reeder SB, Chen GH. Diagnosis of Coronavirus Disease 2019 Pneumonia by Using Chest Radiography: Value of Artificial Intelligence. Radiology. 2021;298:E88-E97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 73] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 41. | Gianchandani N, Jaiswal A, Singh D, Kumar V, Kaur M. Rapid COVID-19 diagnosis using ensemble deep transfer learning models from chest radiographic images. J Ambient Intell Humaniz Comput. 2020;1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 42. | Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK; Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4155] [Cited by in RCA: 3820] [Article Influence: 764.0] [Reference Citation Analysis (1)] |
| 43. | Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 272] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 44. | Kerpel A, Apter S, Nissan N, Houri-Levi E, Klug M, Amit S, Konen E, Marom EM. Diagnostic and Prognostic Value of Chest Radiographs for COVID-19 at Presentation. West J Emerg Med. 2020;21:1067-1075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 45. | Al-Smadi AS, Bhatnagar A, Ali R, Lewis N, Johnson S. Correlation of chest radiography findings with the severity and progression of COVID-19 pneumonia. Clin Imaging. 2021;71:17-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 46. | Tsakok M, Shaw R, Murchison A, Ather S, Xie C, Watson R, Brent A, Andersson M, Benamore R, MacLeod F, Gleeson F. Diagnostic accuracy of initial chest radiograph compared to SARS-CoV-2 PCR in patients with suspected COVID-19. BJR Open. 2020;2:20200034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 47. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 858] [Article Influence: 171.6] [Reference Citation Analysis (0)] |
| 48. | Hani C, Trieu NH, Saab I, Dangeard S, Bennani S, Chassagnon G, Revel MP. COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101:263-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 49. | Parekh M, Donuru A, Balasubramanya R, Kapur S. Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era. Radiology. 2020;297:E289-E302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 50. | Plesner LL, Dyrberg E, Hansen IV, Abild A, Andersen MB. [Diagnostic imaging findings in COVID-19]. Ugeskr Laeger. 2020;182. [PubMed] |
| 51. | Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, Huang Q, Han Y, Hu B, Hu F, Li BH, Li YR, Liang K, Lin LK, Luo LS, Ma J, Ma LL, Peng ZY, Pan YB, Pan ZY, Ren XQ, Sun HM, Wang Y, Wang YY, Weng H, Wei CJ, Wu DF, Xia J, Xiong Y, Xu HB, Yao XM, Yuan YF, Ye TS, Zhang XC, Zhang YW, Zhang YG, Zhang HM, Zhao Y, Zhao MJ, Zi H, Zeng XT, Wang XH; ; for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team; Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 881] [Cited by in RCA: 1136] [Article Influence: 227.2] [Reference Citation Analysis (0)] |
| 52. | Carotti M, Salaffi F, Sarzi-Puttini P, Agostini A, Borgheresi A, Minorati D, Galli M, Marotto D, Giovagnoni A. Chest CT features of coronavirus disease 2019 (COVID-19) pneumonia: key points for radiologists. Radiol Med. 2020;125:636-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 165] [Cited by in RCA: 128] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 53. | Yang W, Sirajuddin A, Zhang X, Liu G, Teng Z, Zhao S, Lu M. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol. 2020;30:4874-4882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 193] [Cited by in RCA: 177] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 54. | Floridi C, Fogante M, Agostini A, Borgheresi A, Cellina M, Natella R, Bruno F, Cozzi D, Maggialetti N, Palumbo P, Miele V, Carotti M, Giovagnoni A. Radiological diagnosis of Coronavirus Disease 2019 (COVID-19): a Practical Guide. Acta Biomed. 2020;91:51-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 55. | Yang R, Li X, Liu H, Zhen Y, Zhang X, Xiong Q, Luo Y, Gao C, Zeng W. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiol Cardiothorac Imaging. 2020;2:e200047. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 344] [Cited by in RCA: 345] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 56. | Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L, Geurts B, Gietema H, Krdzalic J, Schaefer-Prokop C, van Ginneken B, Brink M; COVID-19 Standardized Reporting Working Group of the Dutch Radiological Society. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020;296:E97-E104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 646] [Cited by in RCA: 589] [Article Influence: 117.8] [Reference Citation Analysis (0)] |
| 57. | Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, Schluger NW, Volpi A, Yim JJ, Martin IBK, Anderson DJ, Kong C, Altes T, Bush A, Desai SR, Goldin O, Goo JM, Humbert M, Inoue Y, Kauczor HU, Luo F, Mazzone PJ, Prokop M, Remy-Jardin M, Richeldi L, Schaefer-Prokop CM, Tomiyama N, Wells AU, Leung AN. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology. 2020;296:172-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 665] [Cited by in RCA: 604] [Article Influence: 120.8] [Reference Citation Analysis (0)] |
| 58. | Hochhegger B, Zanon M, Altmayer S, Mandelli NS, Stüker G, Mohammed TL, Verma N, Meirelles GSP, Marchiori E. COVID-19 mimics on chest CT: a pictorial review and radiologic guide. Br J Radiol. 2021;94:20200703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 59. | Cartocci G, Colaiacomo MC, Lanciotti S, Andreoli C, De Cicco ML, Brachetti G, Pugliese S, Capoccia L, Tortora A, Scala A, Valentini C, Almberger M, D'Aprile MR, Avventurieri G, Giura R, Kharrub Z, Leonardi A, Boccia M, Catalano C, Ricci P. Correction to: Chest CT for early detection and management of coronavirus disease (COVID-19): a report of 314 patients admitted to Emergency Department with suspected pneumonia. Radiol Med. 2021;126:642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 60. | Shao JM, Ayuso SA, Deerenberg EB, Elhage SA, Augenstein VA, Heniford BT. A systematic review of CT chest in COVID-19 diagnosis and its potential application in a surgical setting. Colorectal Dis. 2020;22:993-1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 61. | Koo HJ, Choi SH, Sung H, Choe J, Do KH. RadioGraphics Update: Radiographic and CT Features of Viral Pneumonia. Radiographics. 2020;40:E8-E15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 62. | Kalra MK, Homayounieh F, Arru C, Holmberg O, Vassileva J. Chest CT practice and protocols for COVID-19 from radiation dose management perspective. Eur Radiol. 2020;30:6554-6560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 63. | Adams HJA, Kwee TC, Yakar D, Hope MD, Kwee RM. Systematic Review and Meta-Analysis on the Value of Chest CT in the Diagnosis of Coronavirus Disease (COVID-19): Sol Scientiae, Illustra Nos. AJR Am J Roentgenol. 2020;215:1342-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 64. | Suchá D, van Hamersvelt RW, van den Hoven AF, de Jong PA, Verkooijen HM. Suboptimal Quality and High Risk of Bias in Diagnostic Test Accuracy Studies on Chest Radiography and Computed Tomography in the Acute Setting of the COVID-19 Pandemic: A Systematic Review. Radiol Cardiothorac Imaging. 2020;2:e200342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 65. | Herpe G, Lederlin M, Naudin M, Ohana M, Chaumoitre K, Gregory J, Vilgrain V, Freitag CA, De Margerie-Mellon C, Flory V, Ludwig M, Mondot L, Fitton I, Jacquier ARR, Ardilouze P, Petit I, Gervaise A, Bayle O, Crombe A, Mekuko Sokeng M, Thomas C, Henry G, Bliah V, Le Tat T, Guillot MS, Gendrin P, Garetier M, Bertolle E, Montagne C, Langlet B, Kalaaji A, Kayayan H, Desmots F, Dhaene B, Saulnier PJ, Guillevin R, Bartoli JM, Beregi JP, Tasu JP. Efficacy of Chest CT for COVID-19 Pneumonia Diagnosis in France. Radiology. 2021;298:E81-E87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 66. | Kim H, Hong H, Yoon SH. Diagnostic Performance of CT and Reverse Transcriptase Polymerase Chain Reaction for Coronavirus Disease 2019: A Meta-Analysis. Radiology. 2020;296:E145-E155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 354] [Cited by in RCA: 365] [Article Influence: 73.0] [Reference Citation Analysis (0)] |
| 67. | Treglia G. Diagnostic Performance of 18F-FDG PET/CT in Infectious and Inflammatory Diseases according to Published Meta-Analyses. Contrast Media Mol Imaging. 2019;2019:3018349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 68. | Lütje S, Marinova M, Kütting D, Attenberger U, Essler M, Bundschuh RA. Nuclear medicine in SARS-CoV-2 pandemia: 18F-FDG-PET/CT to visualize COVID-19. Nuklearmedizin. 2020;59:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 69. | Capitanio S, Nordin AJ, Noraini AR, Rossetti C. PET/CT in nononcological lung diseases: current applications and future perspectives. Eur Respir Rev. 2016;25:247-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 70. | Setti L, Kirienko M, Dalto SC, Bonacina M, Bombardieri E. FDG-PET/CT findings highly suspicious for COVID-19 in an Italian case series of asymptomatic patients. Eur J Nucl Med Mol Imaging. 2020;47:1649-1656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 71. | Deng Y, Lei L, Chen Y, Zhang W. The potential added value of FDG PET/CT for COVID-19 pneumonia. Eur J Nucl Med Mol Imaging. 2020;47:1634-1635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 72. | Olivari L, Riccardi N, Rodari P, Buonfrate D, Diodato S, Formenti F, Angheben A, Salgarello M. Accidental diagnosis of COVID-19 pneumonia after 18F FDG PET/CT: a case series. Clin Transl Imaging. 2020;1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 73. | Habouzit V, Sanchez A, Dehbi S, Prevot N, Bonnefoy PB. Incidental Finding of COVID-19 Lung Infection in 18F-FDG PET/CT: What Should We Do? Clin Nucl Med. 2020;45:649-651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 74. | Qin C, Liu F, Yen TC, Lan X. 18F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. Eur J Nucl Med Mol Imaging. 2020;47:1281-1286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 205] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 75. | Jajodia A, Ebner L, Heidinger B, Chaturvedi A, Prosch H. Imaging in corona virus disease 2019 (COVID-19)-A Scoping review. Eur J Radiol Open. 2020;7:100237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 76. | Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. AJR Am J Roentgenol. 2020;215:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 219] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 77. | Caetano R, Schluckebier L, Bastos C, Silva R, Carneiro M, Silva J, Biz AN. Análise dos custos do procedimento PET-TC com 18F-FDG na perspectiva do SUS provedor: estudo em uma unidade pública de saúde do Rio de Janeiro, Brasil. Cad Saúde Pública. 2014;30:379-392. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 78. | Ducharme J, Goertzen AL, Patterson J, Demeter S. Practical Aspects of 18F-FDG PET When Receiving 18F-FDG from a Distant Supplier. J Nucl Med Technol. 2009;37:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 79. | Volpicelli G, Lamorte A, Villén T. What's new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med. 2020;46:1445-1448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 177] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 80. | Kulkarni S, Down B, Jha S. Point-of-care lung ultrasound in intensive care during the COVID-19 pandemic. Clin Radiol 2020; 75: 710.e1-710. e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 81. | Sultan LR, Sehgal CM. A Review of Early Experience in Lung Ultrasound in the Diagnosis and Management of COVID-19. Ultrasound Med Biol. 2020;46:2530-2545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 82. | Stogiannos N, Fotopoulos D, Woznitza N, Malamateniou C. COVID-19 in the radiology department: What radiographers need to know. Radiography (Lond). 2020;26:254-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 83. | Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J Ultrasound Med. 2020;39:1459-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 311] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 84. | Vetrugno L, Bove T, Orso D, Barbariol F, Bassi F, Boero E, Ferrari G, Kong R. Our Italian experience using lung ultrasound for identification, grading and serial follow-up of severity of lung involvement for management of patients with COVID-19. Echocardiography. 2020;37:625-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 85. | Sorlini C, Femia M, Nattino G, Bellone P, Gesu E, Francione P, Paternò M, Grillo P, Ruffino A, Bertolini G, Cariati M, Cortellaro F; Fenice Network (Italian Group for Clinical Research in Emergency Medicine). The role of lung ultrasound as a frontline diagnostic tool in the era of COVID-19 outbreak. Intern Emerg Med. 2021;16:749-756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 86. | Garcia JVR, Fonseca EKUN, Chate RC, Strabelli DG, Farias LPG, Loureiro BMC, Ferreira LC, Sawamura MVY. COVID-19 on resonance magnetic: an incidental but important finding in times of pandemic. Einstein (Sao Paulo). 2020;18:eAI5891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 87. | Torkian P, Rajebi H, Zamani T, Ramezani N, Kiani P, Akhlaghpoor S. Magnetic resonance imaging features of coronavirus disease 2019 (COVID-19) pneumonia: The first preliminary case series. Clin Imaging. 2021;69:261-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 88. | Ates OF, Taydas O, Dheir H. Thorax Magnetic Resonance Imaging Findings in Patients with Coronavirus Disease (COVID-19). Acad Radiol. 2020;27:1373-1378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 89. | Meirelles GSP. COVID-19: a brief update for radiologists. Radiol Bras. 2020;53:320-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 90. | Caballeros Lam M, de la Fuente Villena A, Hernández Hernández A, García de Yébenes M, Bastarrika Alemañ G. Cardiac magnetic resonance characterization of COVID-19 myocarditis. Rev Esp Cardiol (Engl Ed). 2020;73:863-864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 91. | Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265-1273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1240] [Cited by in RCA: 1464] [Article Influence: 292.8] [Reference Citation Analysis (0)] |
| 92. | Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging. 2020;13:2330-2339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 389] [Cited by in RCA: 393] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 93. | Galea N, Catapano F, Marchitelli L, Cundari G, Maestrini V, Panebianco V, Mancone M, Fedele F, Catalano C, Francone M. How to perform a cardio-thoracic magnetic resonance imaging in COVID-19: comprehensive assessment of heart, pulmonary arteries, and lung parenchyma. Eur Heart J Cardiovasc Imaging. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 94. | Politi LS, Salsano E, Grimaldi M. Magnetic Resonance Imaging Alteration of the Brain in a Patient With Coronavirus Disease 2019 (COVID-19) and Anosmia. JAMA Neurol. 2020;77:1028-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 95. | Chetrit A, Lechien JR, Ammar A, Chekkoury-Idrissi Y, Distinguin L, Circiu M, Saussez S, Ballester MC, Vasse M, Berradja N, Hans S, Carlier R, Edjlali M. Magnetic resonance imaging of COVID-19 anosmic patients reveals abnormalities of the olfactory bulb: Preliminary prospective study. J Infect. 2020;81:816-846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 96. | Galougahi MK, Ghorbani J, Bakhshayeshkaram M, Naeini AS, Haseli S. Olfactory Bulb Magnetic Resonance Imaging in SARS-CoV-2-Induced Anosmia: The First Report. Acad Radiol. 2020;27:892-893. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 97. | Garg RK, Paliwal VK, Gupta A. Encephalopathy in patients with COVID-19: A review. J Med Virol. 2021;93:206-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 140] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 98. | Nakajima K, Kato H, Yamashiro T, Izumi T, Takeuchi I, Nakajima H, Utsunomiya D. COVID-19 pneumonia: infection control protocol inside computed tomography suites. Jpn J Radiol. 2020;38:391-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 99. | Chen Q, Zu ZY, Jiang MD, Lu L, Lu GM, Zhang LJ. Infection Control and Management Strategy for COVID-19 in the Radiology Department: Focusing on Experiences from China. Korean J Radiol. 2020;21:851-858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 100. | Niu Y, Xian J, Lei Z, Liu X, Sun Q. Management of infection control and radiological protection in diagnostic radiology examination of COVID-19 cases. Radiat Med Prot. 2020;1:75-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 101. | European Centre for Disease Prevention and Control. Guidance for wearing and removing personal protective equipment in healthcare settings for the care of patients with suspected or confirmed COVID-19. Stockholm: ECDC; 2020. [cited 19 January 2021]. Available from: https://www. ecdc.europa.eu/sites/default/files/documents/COVID-19-guidance-wearingand-removing-personal-protective-equipment-healthcare-settings-updated. pdf. |
| 102. | Zhang HW, Yu J, Xu HJ, Lei Y, Pu ZH, Dai WC, Lin F, Wang YL, Wu XL, Liu LH, Li M, Mo YQ, Zhang H, Luo SP, Chen H, Lyu GW, Zhou ZG, Liu WM, Liu XL, Song HY, Chen FZ, Zeng L, Zhong H, Guo TT, Hu YQ, Yang XX, Liu PN, Li DF. Corona Virus International Public Health Emergencies: Implications for Radiology Management. Acad Radiol. 2020;27:463-467. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 103. | Ding J, Fu H, Liu Y, Gao J, Li Z, Zhao X, Zheng J, Sun W, Ni H, Ma X, Feng J, Wu A, Liu J, Wang Y, Geng P, Chen Y. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020;30:3603-3608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 104. | George PM, Barratt SL, Condliffe R, Desai SR, Devaraj A, Forrest I, Gibbons MA, Hart N, Jenkins RG, McAuley DF, Patel BV, Thwaite E, Spencer LG. Respiratory follow-up of patients with COVID-19 pneumonia. Thorax. 2020;75:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 223] [Cited by in RCA: 224] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 105. | McStay R, Johnstone A, Hare SS, Jacob J, Nair A, Rodrigues JCL, Edey A, Robinson G. COVID-19: looking beyond the peak. Challenges and tips for radiologists in follow-up of a novel patient cohort. Clin Radiol 2021; 76: 74.e1-74. e14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 106. | Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, Noel A, Gunning S, Hatrick J, Hamilton S, Elvers KT, Hyams C, Bibby A, Moran E, Adamali HI, Dodd JW, Maskell NA, Barratt SL. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 385] [Article Influence: 77.0] [Reference Citation Analysis (0)] |
| 107. | Alharthy A, Abuhamdah M, Balhamar A, Faqihi F, Nasim N, Ahmad S, Noor A, Tamim H, Alqahtani SA, Abdulaziz Al Saud AAASB, Kutsogiannis DJ, Brindley PG, Memish ZA, Karakitsos D, Blaivas M. Residual Lung Injury in Patients Recovering From COVID-19 Critical Illness: A Prospective Longitudinal Point-of-Care Lung Ultrasound Study. J Ultrasound Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 108. | Stephanie S, Shum T, Cleveland H, Challa SR, Herring A, Jacobson FL, Hatabu H, Byrne SC, Shashi K, Araki T, Hernandez JA, White CS, Hossain R, Hunsaker AR, Hammer MM. Determinants of Chest X-Ray Sensitivity for COVID- 19: A Multi-Institutional Study in the United States. Radiol Cardiothorac Imaging. 2020;2:e200337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 109. | Wen Z, Chi Y, Zhang L, Liu H, Du K, Li Z, Chen J, Cheng L, Wang D. Coronavirus Disease 2019: Initial Detection on Chest CT in a Retrospective Multicenter Study of 103 Chinese Patients. Radiol Cardiothorac Imaging. 2020;2:e200092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 110. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3283] [Article Influence: 656.6] [Reference Citation Analysis (0)] |