Copyright
©2014 Baishideng Publishing Group Inc.
World J Radiol. Jul 28, 2014; 6(7): 446-458
Published online Jul 28, 2014. doi: 10.4329/wjr.v6.i7.446
Published online Jul 28, 2014. doi: 10.4329/wjr.v6.i7.446
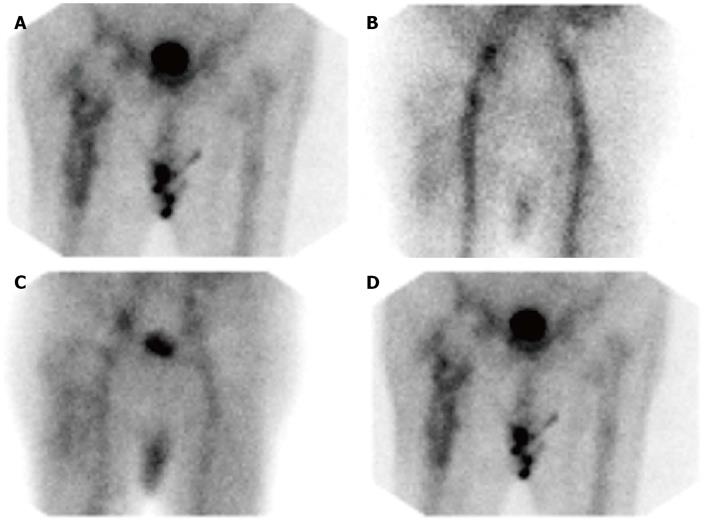
Figure 1 Aseptically loosened right hip arthroplasty.
A: X-ray reveals medial protrusion of the acetabular component of a painful 15 year old hip replacement. There is heterotopic ossification around both greater trochanters (arrows); B: On the 99mTc-methylene diphosphonate bone scan, there is focally increased radiopharmaceutical accumulation at the distal tip of the femoral component (arrow) of the right hip replacement and lateral to the femoral neck (arrowhead) corresponding to the heterotopic bone seen on the X-ray. An aseptically loosened prosthesis was revised. Focally increased radiopharmaceutical accumulation is present at the tip of the femoral component of the asymptomatic left hip arthroplasty (double arrows) which also was 15 years old.
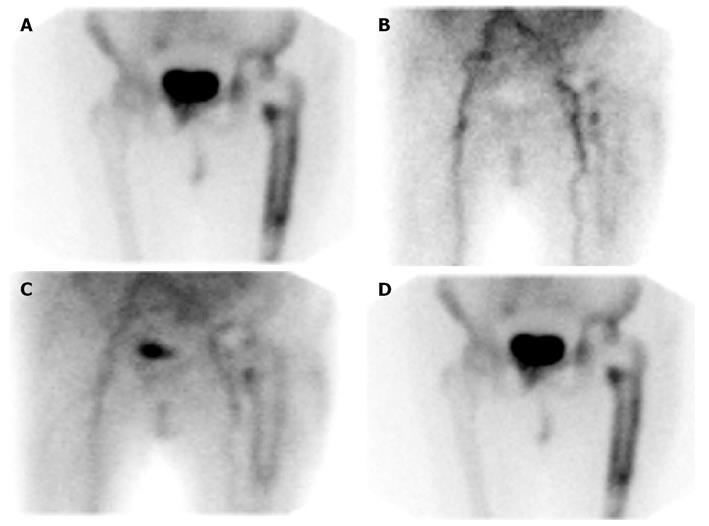
Figure 2 Infected right hip arthroplasty.
A: On the 99mTc-methylene diphosphonate bone scan, there is irregularly increased radiopharmaceutical accumulation around the entire femoral component of the 2 years old cementless (revision) prosthesis, a pattern which some investigators have reported as specific for infection; B-D: On the 99mTc-MDP bone scan, there is diffuse hyperperfusion, and hyperemia around the prosthesis on the flow and blood pool images, and diffusely increased periprosthetic radiopharmaceutical on the delayed, bone image (same patient illustrated in Figure 2A); B: Flow; C: Blood pool; D: Bone.
Figure 3 Aseptically loosened left hip replacement.
A: On the 99mTc-MDP bone scan, there is diffusely increased radiopharmaceutical accumulation around the femoral component of the cemented 2 years old prosthesis. Compare with Figure 2A; B-D: On the 99mTc-MDP bone scan, there is diffuse hyperperfusion, and hyperemia around the prosthesis on the flow and blood pool images, and diffusely increased periprosthetic radiopharmaceutical on the delayed, bone image (same patient illustrated in Figure 3A), B: Flow; C: Blood pool; D: Delayed. The scan appearance is nearly identical to that of the infected prosthesis in Figure 2B.
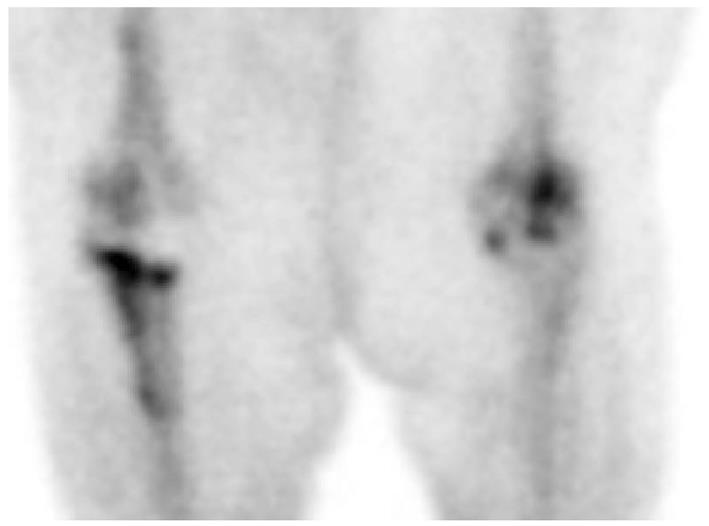
Figure 4 Asymptomatic right knee arthroplasty.
On the 99mTc-MDP bone scan, there is irregular, intense radiopharmaceutical accumulation around the long stemmed tibial component of a three year old right knee replacement. The femoral component is unremarkable. The patient had a history of breast carcinoma and bone scintigraphy was performed as part of a routine evaluation for metastatic disease.
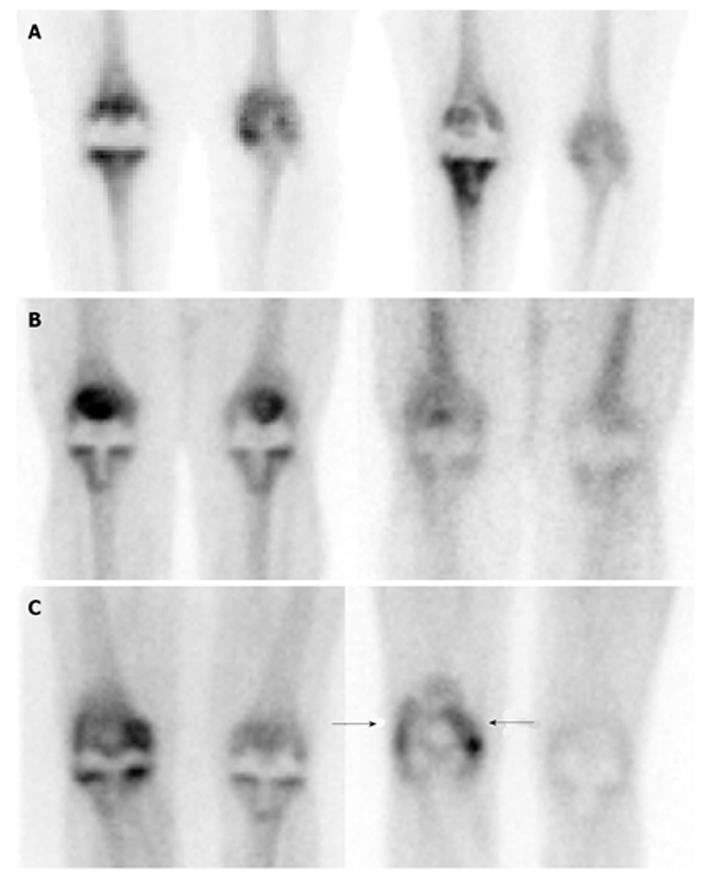
Figure 5 Aseptically loosened right knee arthroplasty.
A: On the 99mTc-methylene diphosphonate (MDP) bone scan, performed about 6 mo after implantation (left), shows mildly increased radiopharmaceutical accumulation around the femoral and tibial components. On the repeat study, performed 9 mo later (15 mo after implantation), there is intensely increased radiopharmaceutical accumulation around the tibial component, while activity around the femoral component has resolved. An aseptically loosened tibial component was revised; B: On the 99mTc-MDP bone scan (left) there is increased radiopharmaceutical accumulation around the tibial component of both the symptomatic right and asymptomatic left knee prostheses. There is normal periprosthetic distribution around both prostheses on the gallium-67 image (right), and the combined study is negative for infection; C: On the 99mTc-MDP bone scan (left) there is increased radiopharmaceutical accumulation around the tibial component of the symptomatic right and faintly increased accumulation around the tibial component of the asymptomatic left knee prosthesis. On the gallium-67 image (right), in contrast to the bone scan, there is increased radiopharmaceutical accumulation around the femoral component (arrows) of the right knee replacement, while activity around the tibial component is normal. There is normal periprosthetic gallium activity around the asymptomatic left prosthesis. The distribution of activity around the right knee prosthesis on the bone and gallium studies is spatially incongruent and the combined study is (false) positive for infection. Aseptic loosening of joint replacements often is accompanied by an intense inflammatory response and gallium cannot reliably differentiate infection from inflammation.
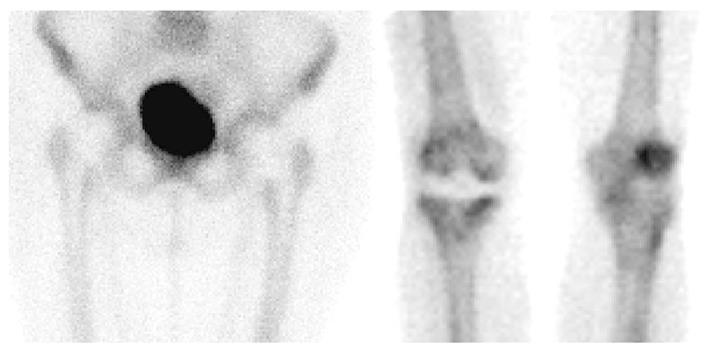
Figure 6 Normal 99mTc-methylene diphosphonate bone scans of bilateral hip (left) and right knee (right) prostheses.
A normal bone scan is defined as a scan in which periprosthetic activity is indistinguishable from adjacent, non-articular bone. The bone scan has a high negative predictive value and therefore a normal study makes it very unlikely that the patient’s symptoms are related to the prosthesis.
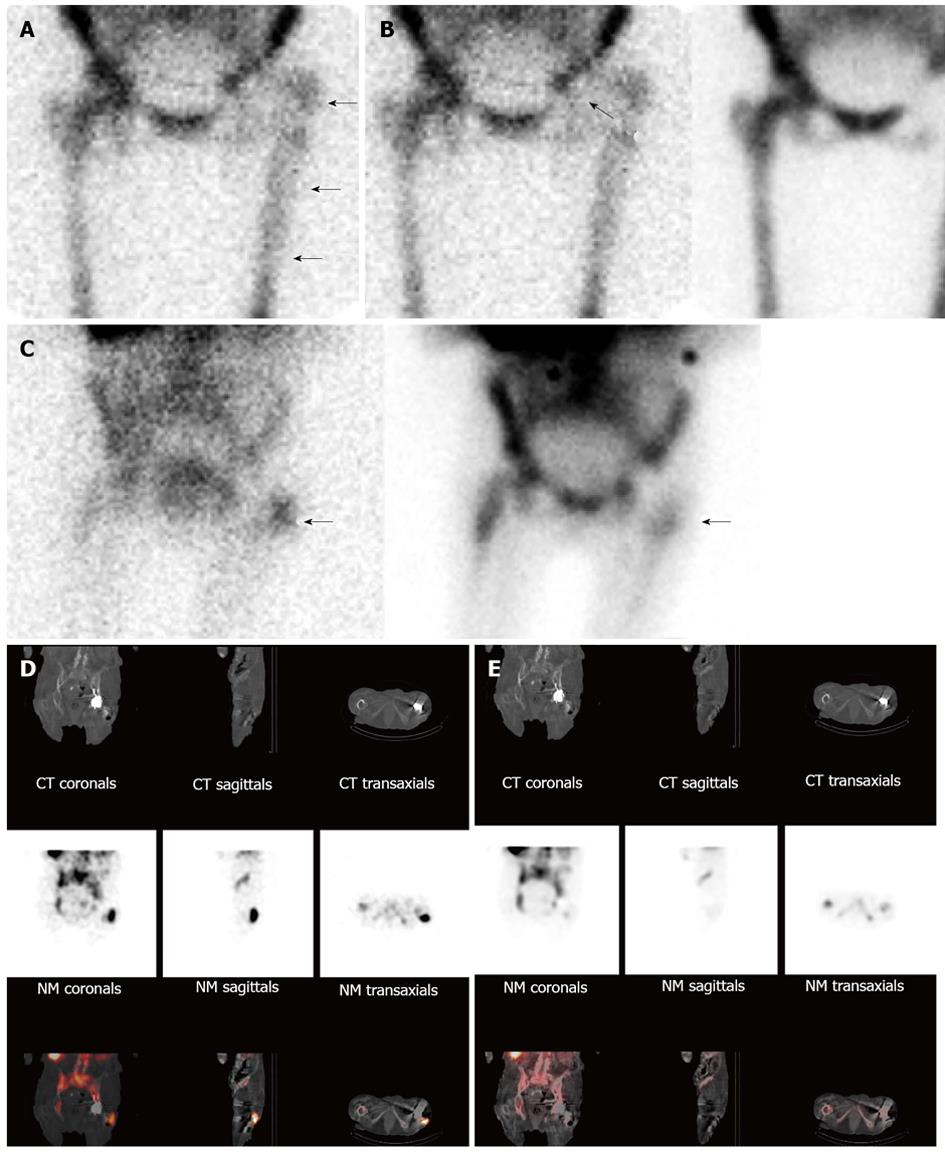
Figure 7 Infected left hip arthroplasty.
A: On this anterior image from an indium-111 labeled leukocyte study, periprosthetic activity (arrows) is similar in intensity to activity in the contralateral lower extremity and less intense than pelvic activity, areas typically used as reference points when interpreting these studies. Because studies in which the intensity of labeled leukocyte activity in the region of interest does not exceed intensity of activity in the reference point, this study could be erroneously interpreted as negative for infection; B: The distribution of periprosthetic activity on the labeled leukocyte (left, 111In-WBC) and sulfur colloid bone marrow (right, 99mTc-SC) images is spatially incongruent (arrows), i.e., there is activity in the left hip joint on the labeled leukocyte image, but not on the bone marrow image. The combined study is positive for infection. (Same patient illustrated in Figure 7A); Although the planar combined indium labeled leukocyte/bone marrow study (C, left, 111In-WBC; right, 99mTc-SC) is positive for infection (arrows), precise information about the location and extent of infection is lacking. On the fused images (bottom row) from the labeled leukocyte SPECT/CT (D) the location of the abnormal labeled leukocyte accumulation (arrows) can clearly be seen adjacent and extending to the prosthesis at the level of the greater trochanter. Note also the adjacent hypodense area in the soft tissues, consistent with abscess. Bone marrow SPECT/CT images (E) acquired simultaneously with the labeled leukocyte images in 16a confirm that the activity on the labeled leukocyte component of the examination is due to infection. Whether or not the bone marrow component of the SPECT/CT study contributes additional information beyond what planar imaging provides remains to be determined.
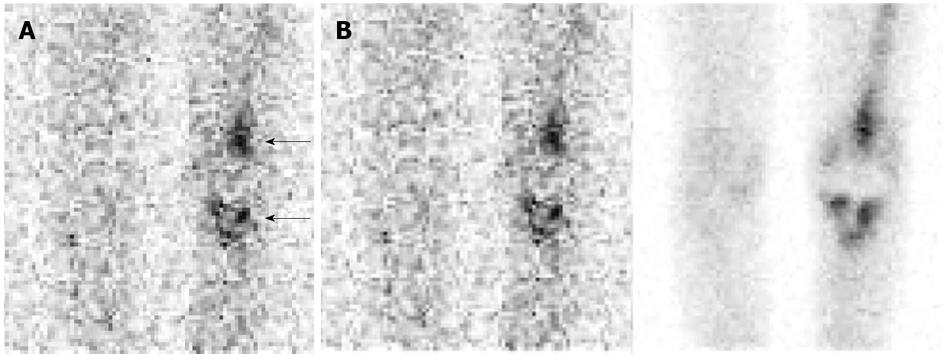
Figure 8 Aseptically loosened left knee arthroplasty.
A: On this anterior image from an indium-111 labeled leukocyte study, there is intense periprosthetic activity around both the tibial and femoral components (arrows), while there is no activity around the contralateral knee. The study could be interpreted erroneously as positive for infection. Compare the intensity of activity around this prosthesis with the intensity of activity around the infected hip arthroplasty in Figure 7A. As these two cases illustrate, the intensity of labeled leukocyte activity around a prosthetic joint is not a reliable criterion for determining the presence or absence of infection; B: The distribution of periprosthetic activity on the labeled leukocyte (left, 111In-WBC) and sulfur colloid bone marrow (right, 99mTc-SC) images is virtually identical (spatially congruent) and the combined study is negative for infection. The periprosthetic activity on the labeled leukocyte image is due to marrow, not to infection. Performing complementary bone marrow imaging eliminates the two major difficulties inherent in the interpretation of labeled leukocyte images: variable intensity of periprosthetic activity and differentiating bone marrow activity from infection. Same patient illustrated in Figure 8A.
- Citation: Palestro CJ. Nuclear medicine and the failed joint replacement: Past, present, and future. World J Radiol 2014; 6(7): 446-458
- URL: https://www.wjgnet.com/1949-8470/full/v6/i7/446.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i7.446