Copyright
©2014 Baishideng Publishing Group Inc.
World J Radiol. Jun 28, 2014; 6(6): 344-354
Published online Jun 28, 2014. doi: 10.4329/wjr.v6.i6.344
Published online Jun 28, 2014. doi: 10.4329/wjr.v6.i6.344
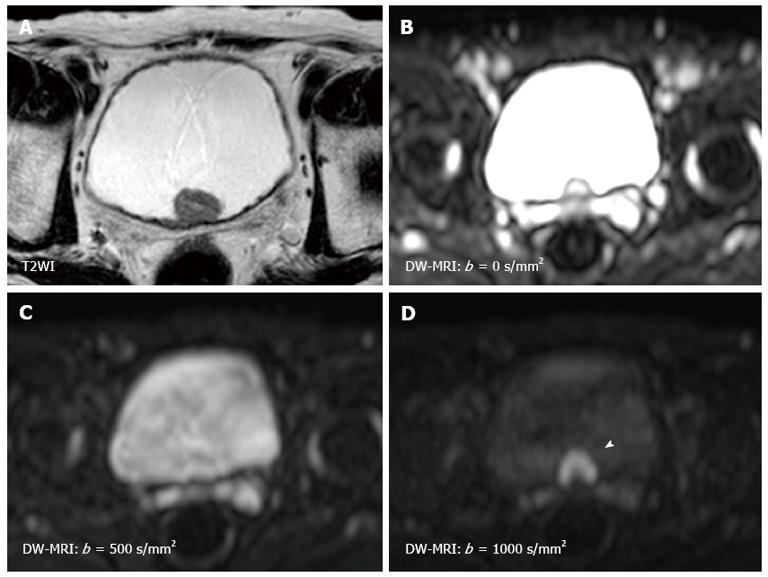
Figure 1 Magnetic resonance images of a 79-year-old man with non-muscle invasive bladder cancer (urothelial cancer, stage pTa, grade 2 > 3).
A: T2WI shows a hypointense tumor at the trigone; B: The signal intensity of diffusion-weighted magnetic resonance imaging depends on both water diffusion and the T2 relaxation time; C: Due to the very long T2 relaxation time of urine, the signal of the urine in the bladder remains high on the diffusion-weighted magnetic resonance imaging with a b-value of 500 s/mm2. This is known as the “T2 shine-through effect”; D: Using a b-value of 1000 s/mm2 decreases the signal of the urine, as well as those of the seminal vesicles, while the bladder cancer (arrow head) shows little signal attenuation with the increased b-value.
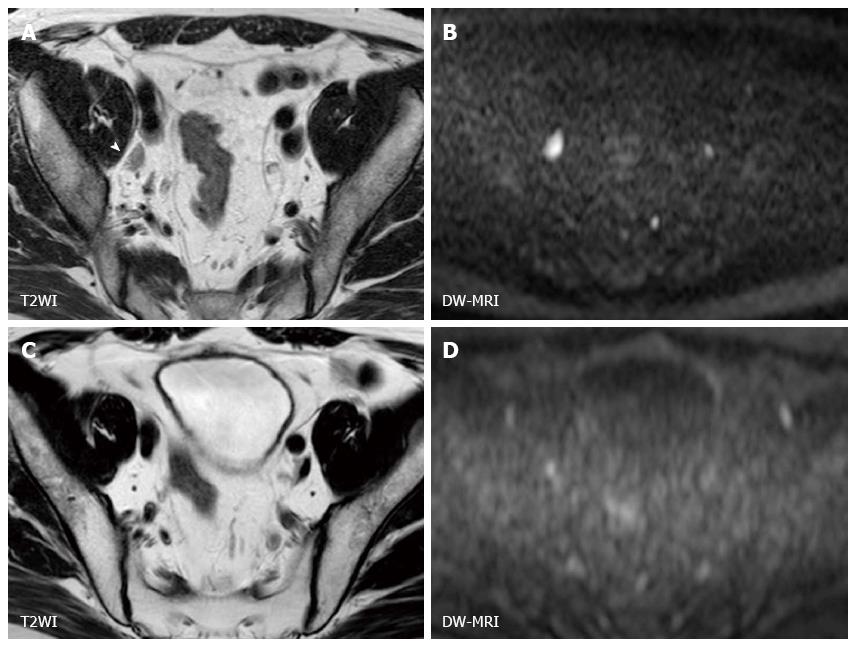
Figure 2 Magnetic resonance images of a 45-year-old man with muscle-invasive bladder cancer (urothelial cancer, stage cT3N1) before and after chemoradiotherapy.
A: Before CRT, an enlarged right external iliac lymph node (arrow head) is visible on T2WI; B: The lymph node on the corresponding DW-MRI shows a hyperintense signal; C and D: After CRT, size reduction on T2WI (C) and signal attenuation on DW-MRI (D) in lymph node is evident, consistent with the expected treatment response. CRT: Chemoradiotherapy; DW-MRI: Diffusion-weighted magnetic resonance imaging.
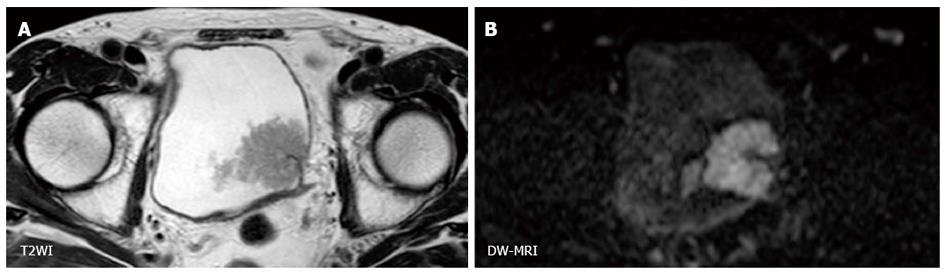
Figure 3 Magnetic resonance images of a 63-year-old man with non-muscle-invasive bladder cancer (urothelial cancer, stage pT1, grade 2 > 3).
A: T2WI shows a large papillary tumor on the left bladder wall; B: DW-MRI displays a C-shaped high-signal tumor with a low-signal-intensity stalk connecting to the bladder wall. This C-shaped high signal is known as an “inchworm sign”, which is a criterion for T staging in non-muscle-invasive bladder cancer (stage cT1 or less). DW-MRI: Diffusion-weighted magnetic resonance imaging.
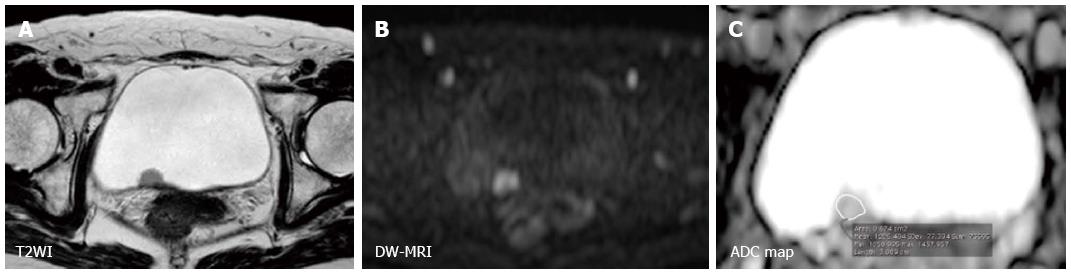
Figure 4 Magnetic resonance images of a 52-year-old woman with non-muscle-invasive bladder cancer (urothelial cancer, pTa, grade 2).
A: T2WI shows a hypointense tumor at the posterior wall; B: DW-MRI displays the tumor as a high-signal mass; C: The corresponding ADC map demonstrates a lesser degree of restricted diffusion. The mean ADC value with the ROI positioned not extending over the tumor is 1.21 x 10-3 s/mm2. DW-MRI: Diffusion-weighted magnetic resonance imaging; ADC: Apparent diffusion coefficient.
Figure 5 Magnetic resonance images of a 75-year-old man with muscle-invasive bladder cancer (urothelial cancer, stage cT4, grade 3).
A and B: T2WI shows a large hypointense tumor at the bladder neck, invading the prostate; C: DW-MRI displays the tumor as a high-signal mass; D: The corresponding ADC map demonstrates restricted diffusion. The mean ADC value of the tumor is 0.63 x 10-3 mm2/s. DW-MRI: Diffusion-weighted magnetic resonance imaging; ADC: Apparent diffusion coefficient.
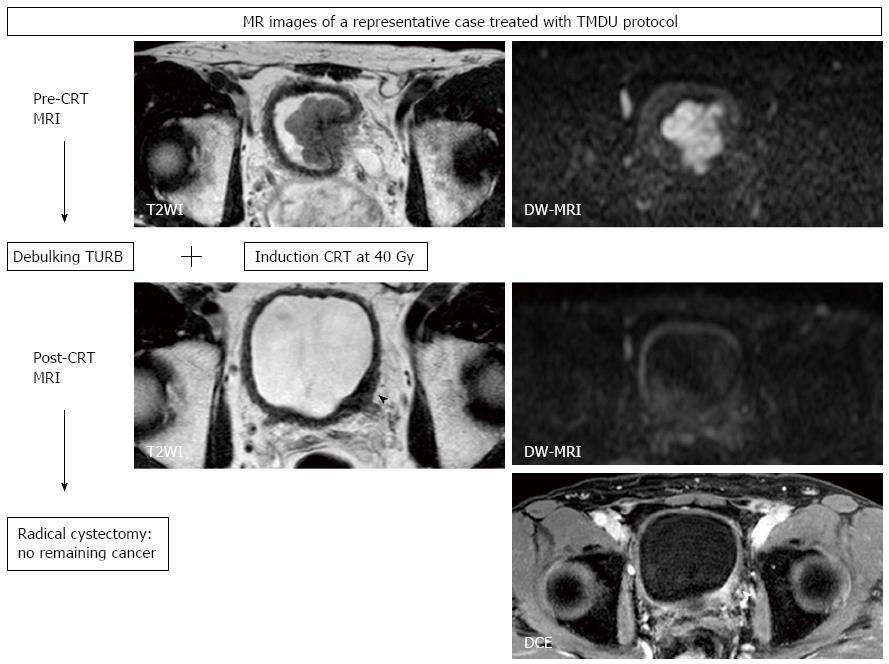
Figure 6 Magnetic resonance images of a 61-year-old man with muscle-invasive bladder cancer (urothelial cancer, stage cT3, grade 3) treated with the Tokyo Medical and Dental University protocol consisting of transurethral resection of bladder tumor and induction chemoradiotherapy (CRT) followed by radical or partial cystectomy.
T2WI shows a large hypointense tumor at the bladder neck, invading the prostate. At the diagnosis, DW-MRI with a b-value of 1000 s/mm2 displays a hyperintense lobulated mass. After TURBT and CRT, this lesion shows wall thickening (arrow head) on T2WI and enhancement on DCE, while the abnormal signal on DW-MRI is diminished to normal signal intensity. Histopathologic examination of the cystectomized sample reveals no remaining bladder cancer, revealing the findings of post-CRT T2WI and DCE to be false-positive findings reflecting post-treatment changes in bladder tissues. TURBT: Transurethral resection of bladder tumor; CRT: Chemoradiotherapy; DW-MRI: Diffusion-weighted magnetic resonance imaging; DCE: Dynamic contrast-enhanced.
- Citation: Yoshida S, Koga F, Kobayashi S, Tanaka H, Satoh S, Fujii Y, Kihara K. Diffusion-weighted magnetic resonance imaging in management of bladder cancer, particularly with multimodal bladder-sparing strategy. World J Radiol 2014; 6(6): 344-354
- URL: https://www.wjgnet.com/1949-8470/full/v6/i6/344.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i6.344