Copyright
©2011 Baishideng Publishing Group Co.
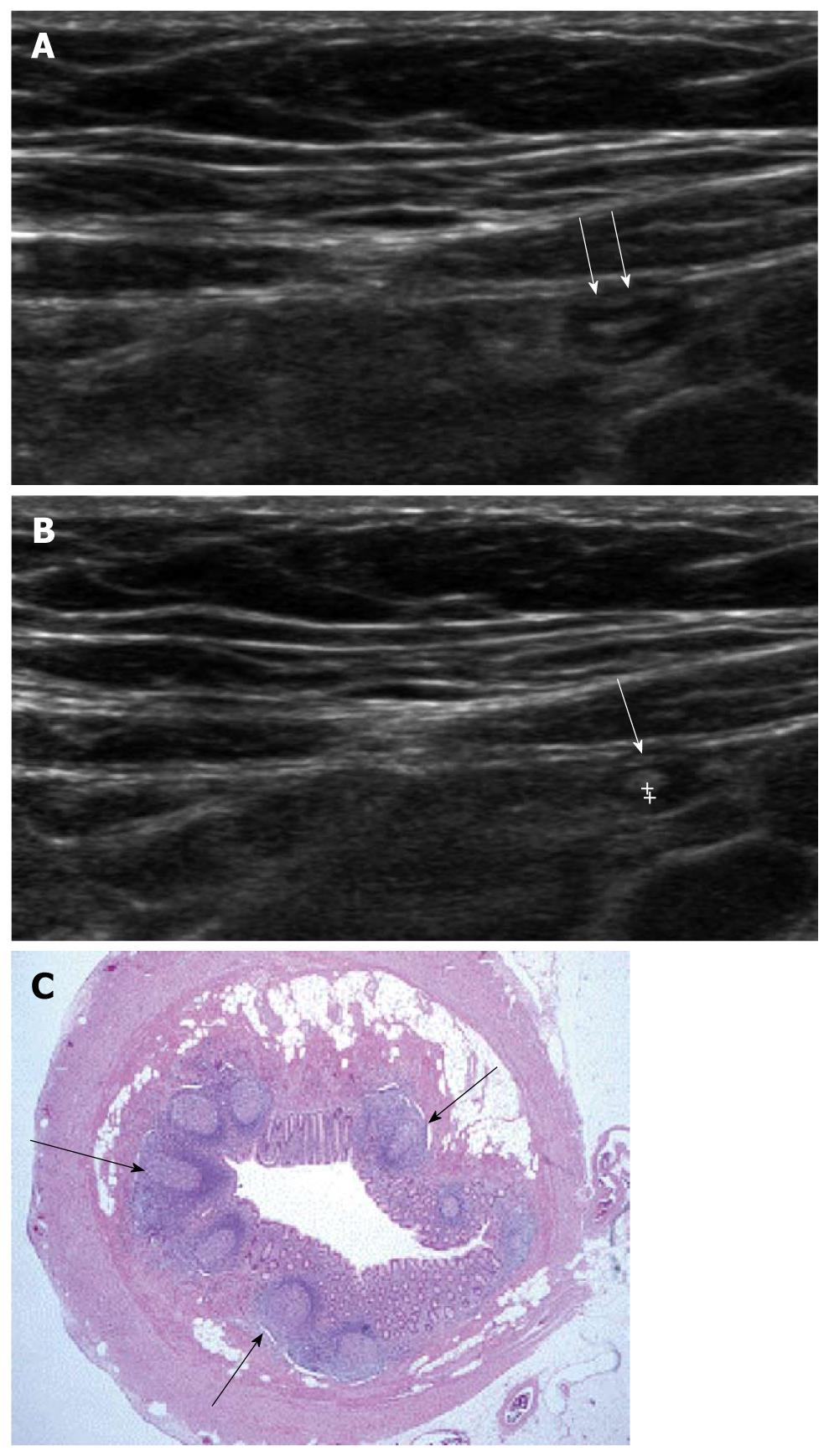
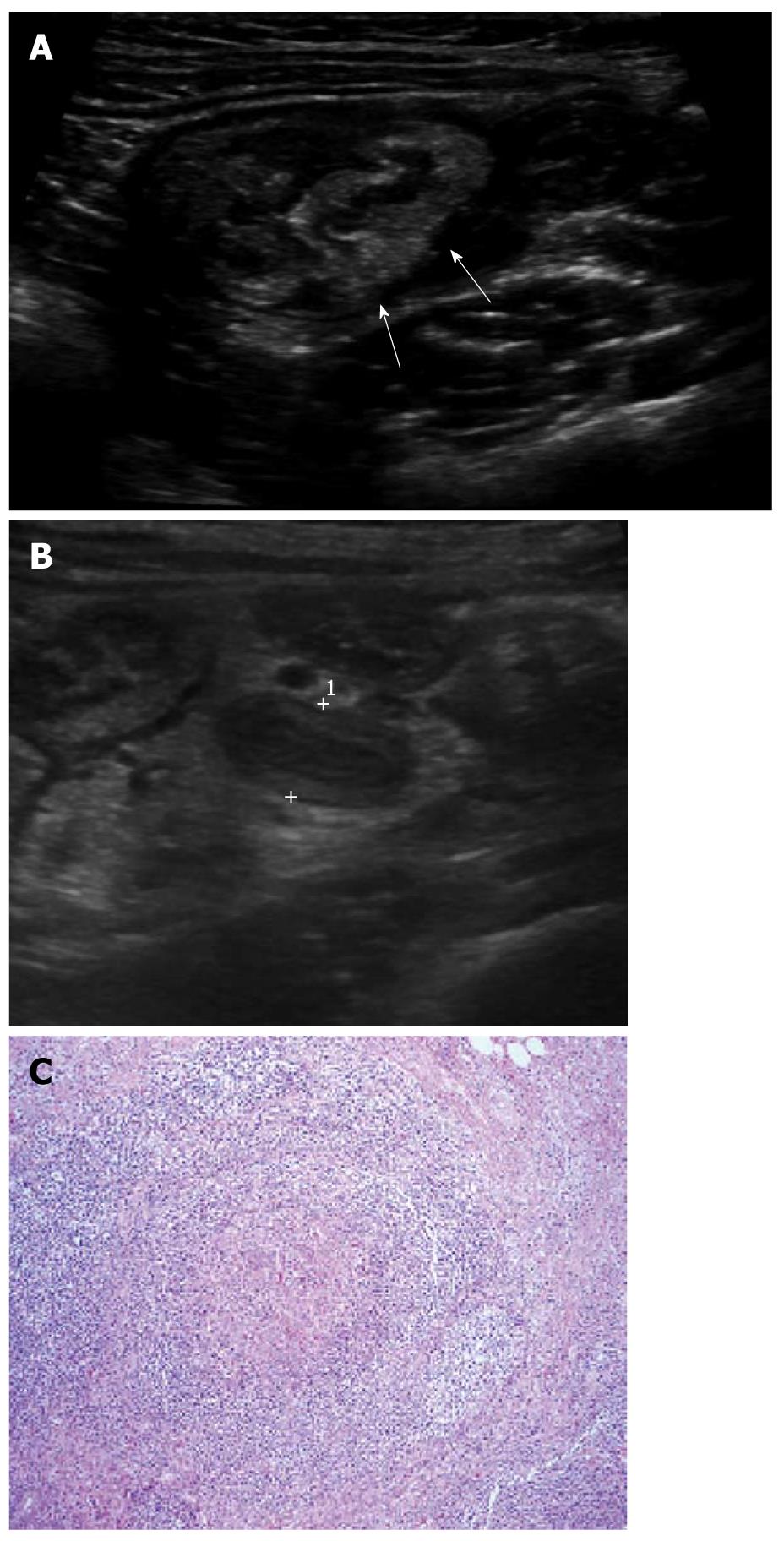
Figure 1 Ultrasonographic and histologic findings of normal appendix.
A: Normal appendix (arrows) with thin inner hypoechoic band was seen on high frequency ultrasonography; B: The thickness of the inner hypoechoic band (cursors) of appendix (arrow) was measured as 0.5 mm; C: Low-magnification view of a cross section of the appendix. The inner wall of the appendix is lined by a layer of surface epithelium. The remainder of the mucosa (crypts, surrounding lamina propria, and the inconspicuous muscularis mucosae) surrounds this surface epithelial layer. The characteristic lymphoid nodules (arrows) within the lamina propria were found (× 20, H-E stain).
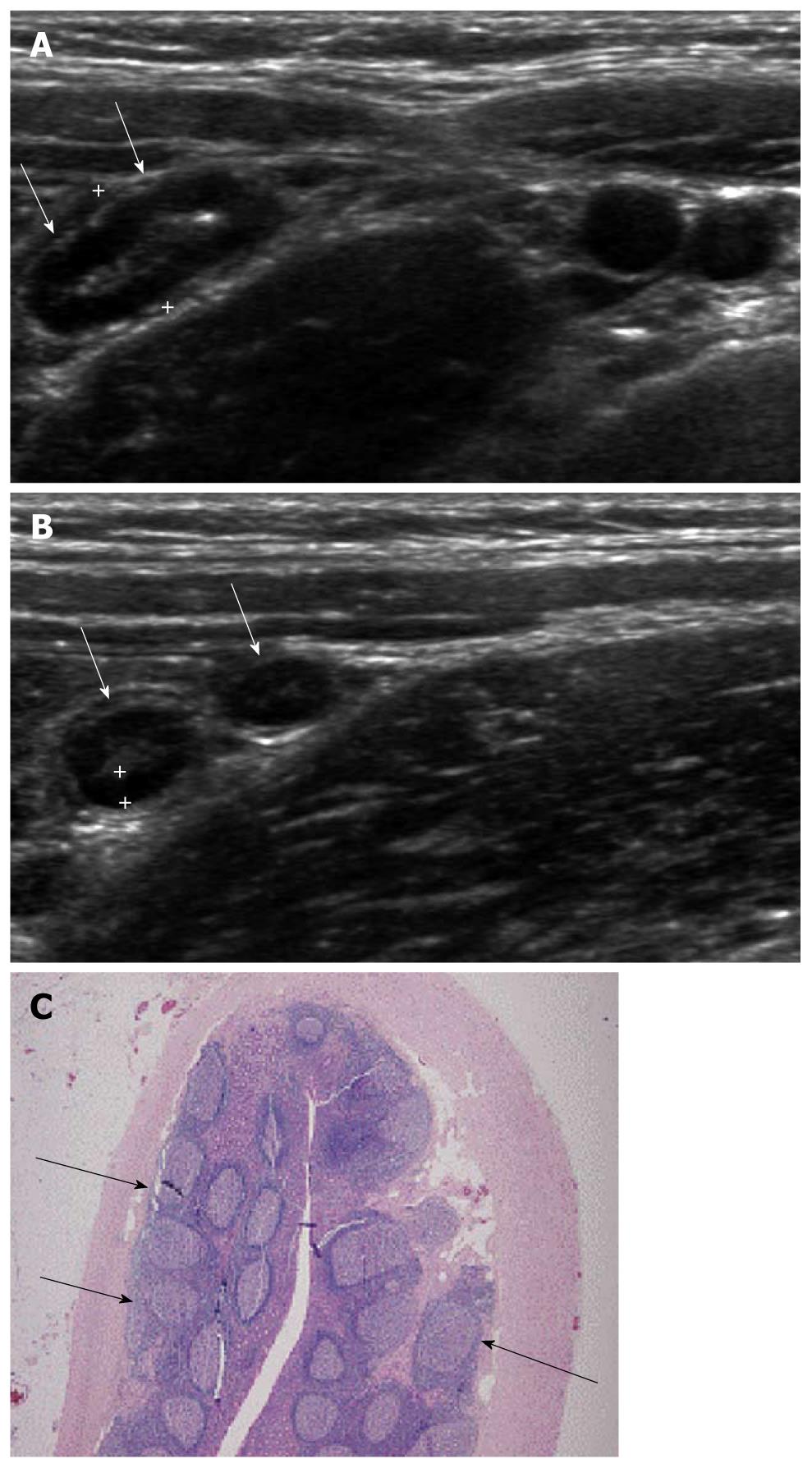
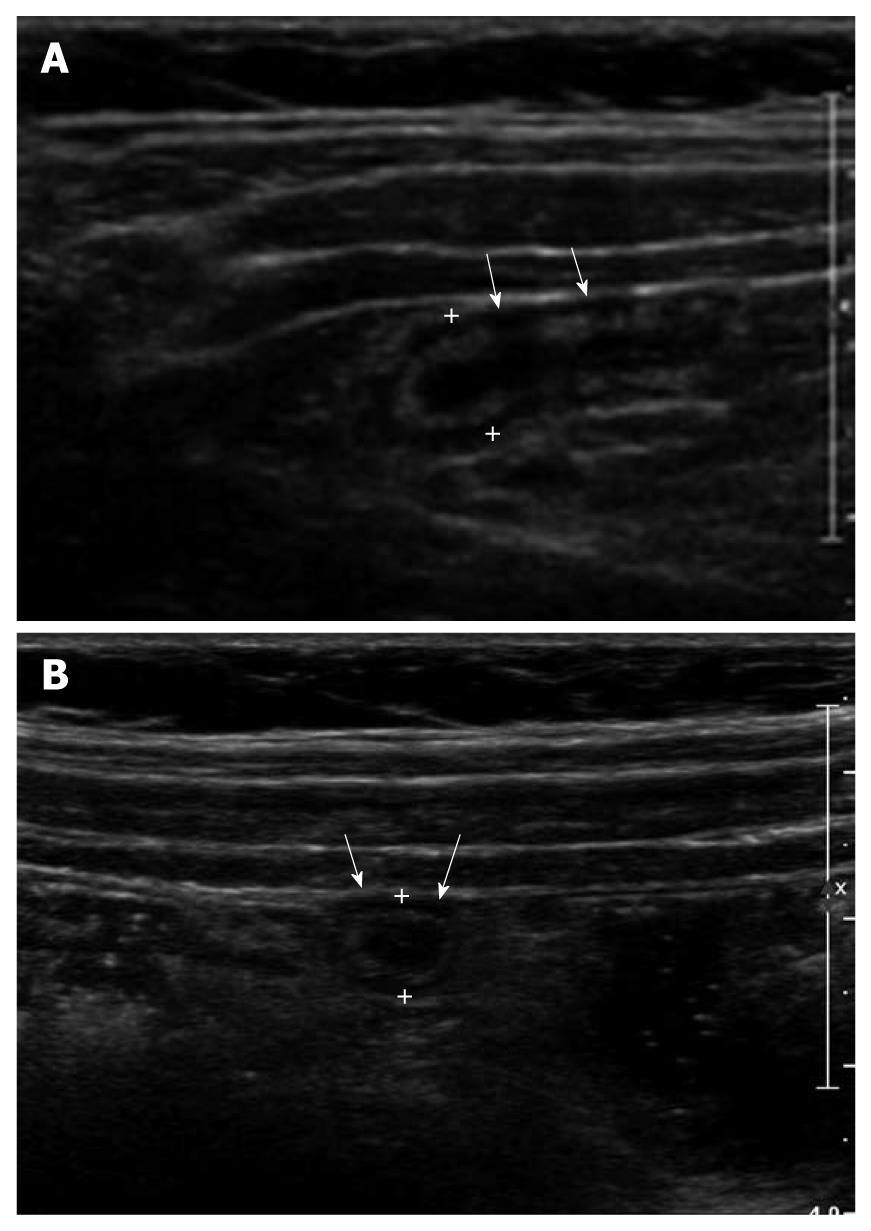
Figure 2 Ultrasonographic and histologic findings of mucosal lymphoid hyperplasia of the appendix.
A: Normal appendix with thick inner hypoechoic band was seen (arrows). The maximal outer diameter was measured as 7.3 mm; B: The thickness of the inner hypoechoic band (cursors) of the appendix (arrows) was measured as 1.4 mm; C: Prominent lymphoid follicles (arrows) were found (× 20, H-E stain).
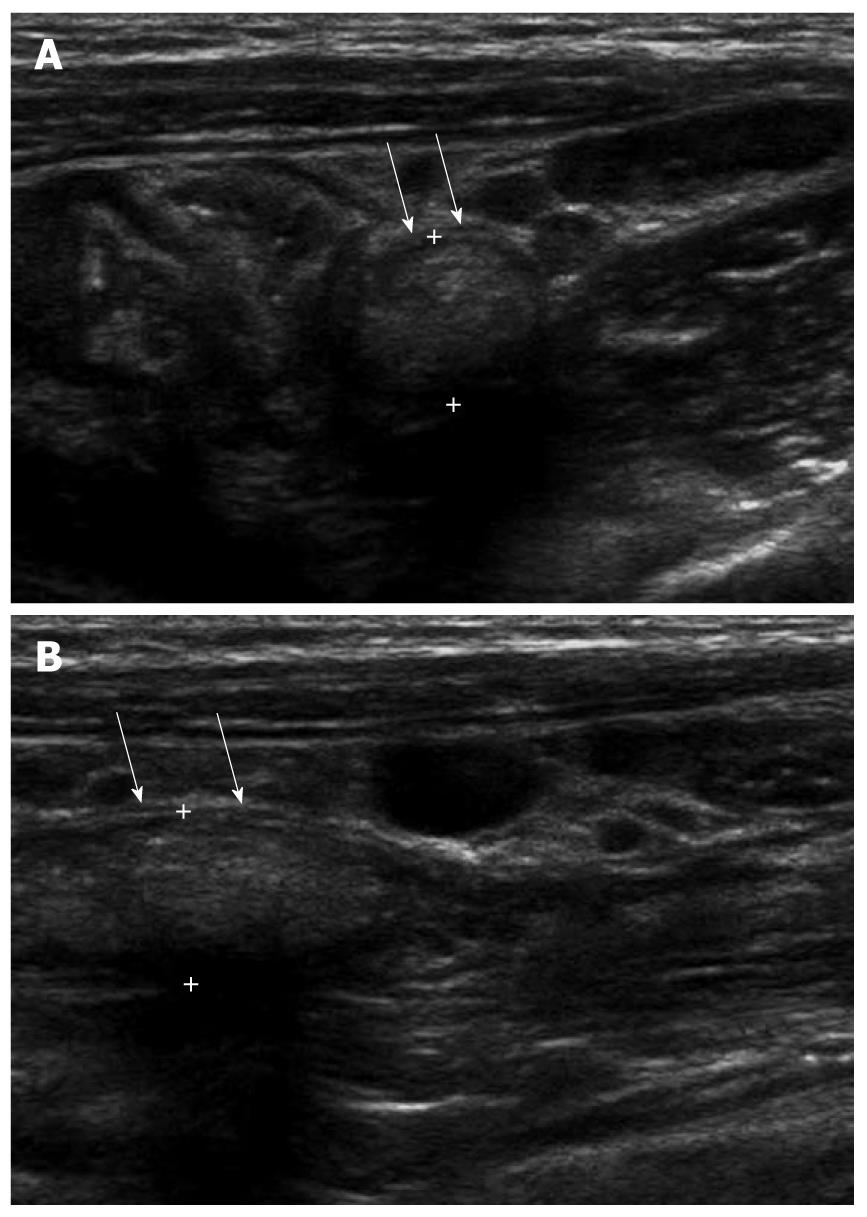
Figure 3 A 5-year-old male with acute abdominal pain.
A: Fecal distended appendix (arrows) with thinned maximal mural thickness (0.6 mm) and preservation of wall layers were seen on axial image; B: The maximal outer diameter of fecal distended appendix (arrows) was measured as 8.5 mm.
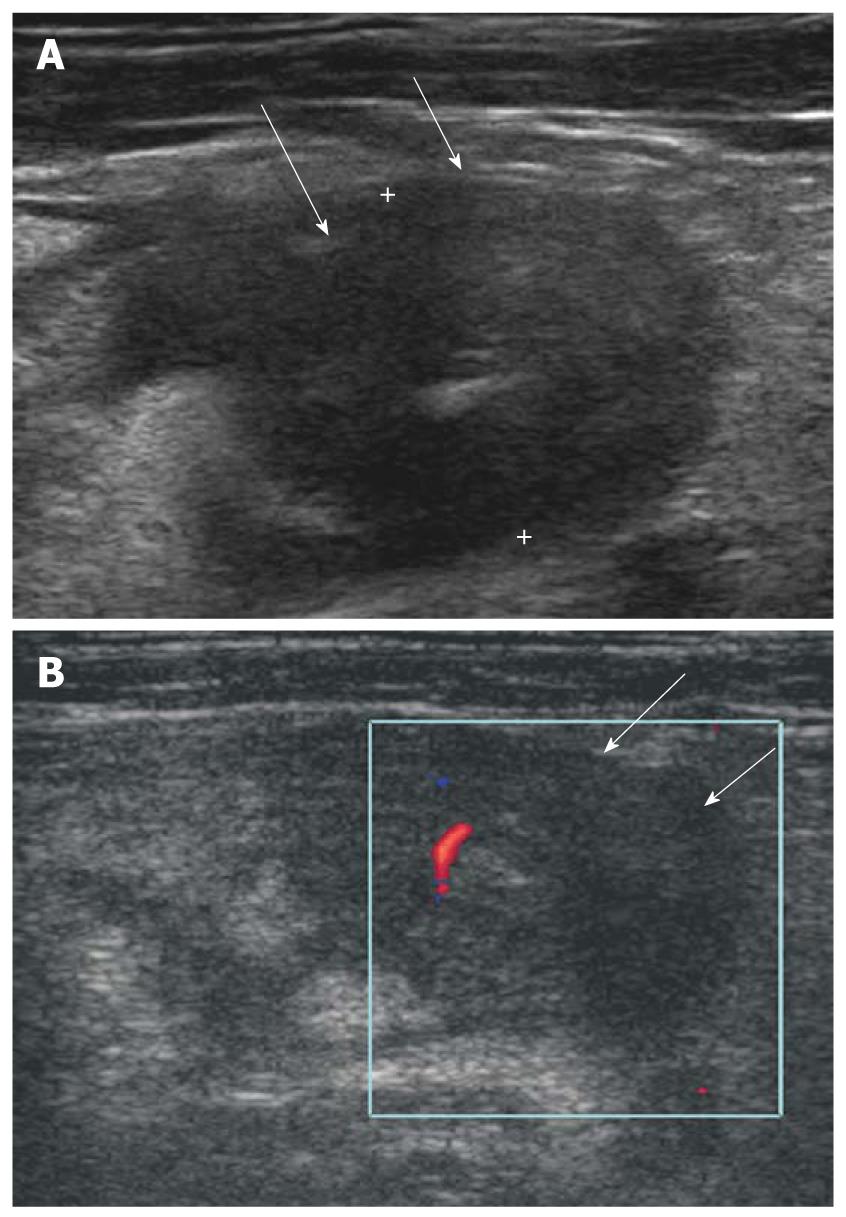
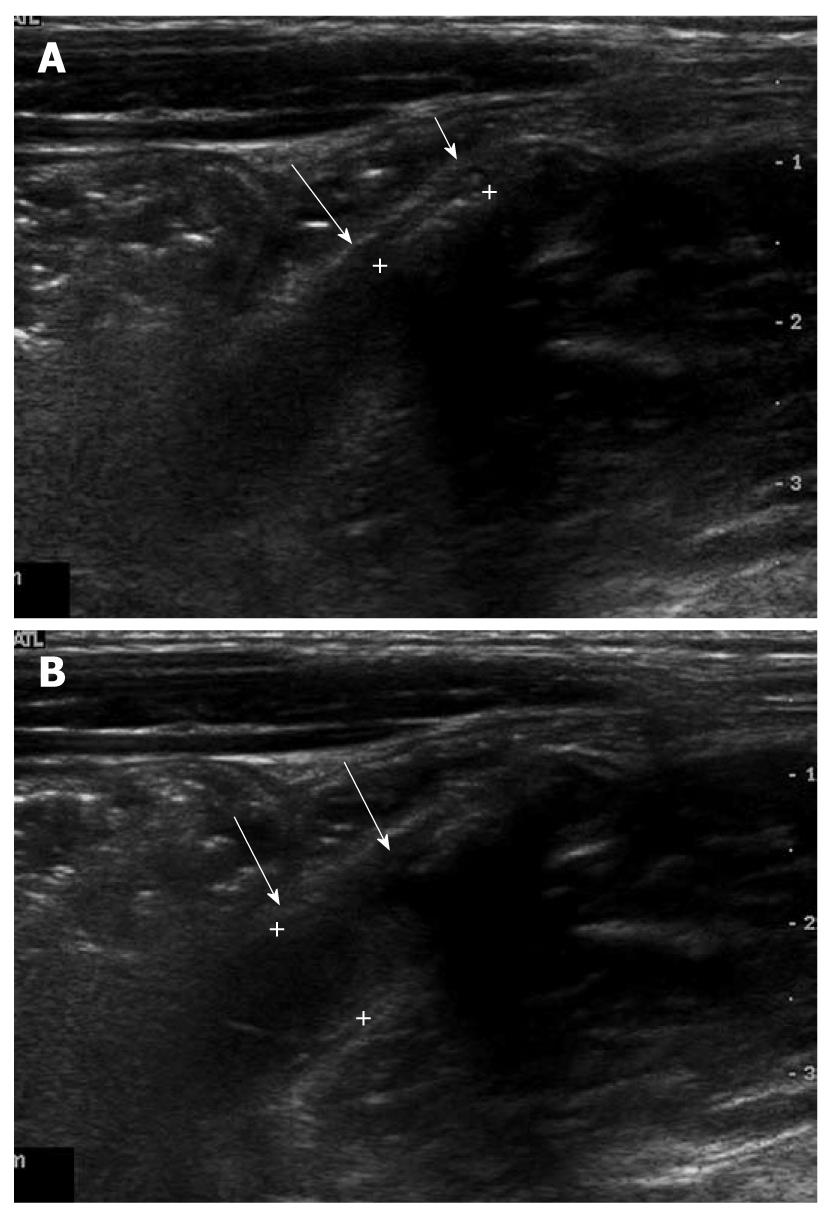
Figure 4 Isolated Crohn’s appendicitis.
A: Marked thickening with transmural hypoechoic echo-alteration of appendiceal wall (arrows); B: Mild increased blood flow in thickened appendiceal wall (arrows) was seen on color Doppler study.
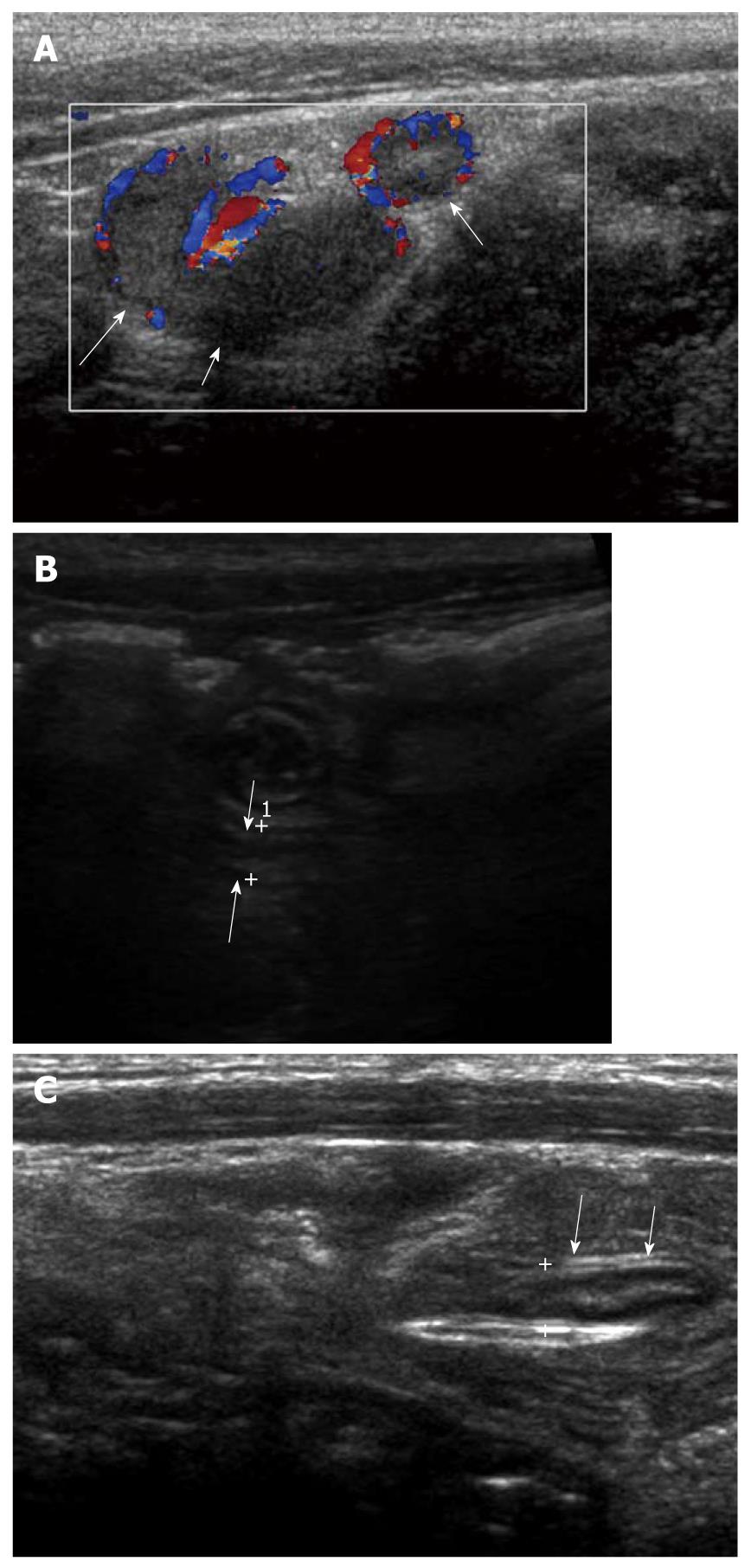
Figure 5 A 4-year-old female with acute colitis.
A: Diffuse thickening of the colonic wall including cecum (arrows) was seen; B: Appendix (cursors) was also swollen with a maximal outer diameter of 7.8 mm and mildly increased echogenicity of periappendiceal mesenteric fat, which led to the misdiagnosis of acute appendicitis; C: The lymphoid follicles within the Peyer’s patches show granulomas with microabscesses (× 100, H-E stain), suggestive of yersiniosis.
Figure 6 A 10-year-old male with a non-obstructive acute appendicitis.
A: Thickening of appendiceal wall (arrows) with a maximal outer diameter (MOD) of 3 mm and some irregularity of the submucosal echogenic layer. However, no evidence of luminal distention and intraluminal appendicolith was found; B: MOD of inflamed appendix (arrows) was measured as 7.1 mm.
Figure 7 A 7-year-old female with an obstructive acute appendicitis.
A: Luminal distention of appendix (arrows) was seen. The maximal outer diameter was measured as approximately 7.9 mm; B: Proximal intraluminal appendicolith (cursors) of appendix (arrows) was identified.
Figure 8 A 6-year-old male with acute appendicitis and fever.
A: Distended appendix with dirty intraluminal fluid and hyperemia of appendiceal wall on color Doppler study (arrows). Periappendiceal mesenteric fat infiltration was identified; B: Because of lobar pneumonia, surgery was delayed and antibiotic therapy given. On follow-up ultrasonography 3 d later, the maximal outer diameter of appendix (arrows) was decreased to 4 mm with disappearance of intraluminal content; C: On follow-up after 6 d, the wall layers of the appendix (arrows) had recovered significantly. Periappendiceal mesenteric fat change had almost resolved.
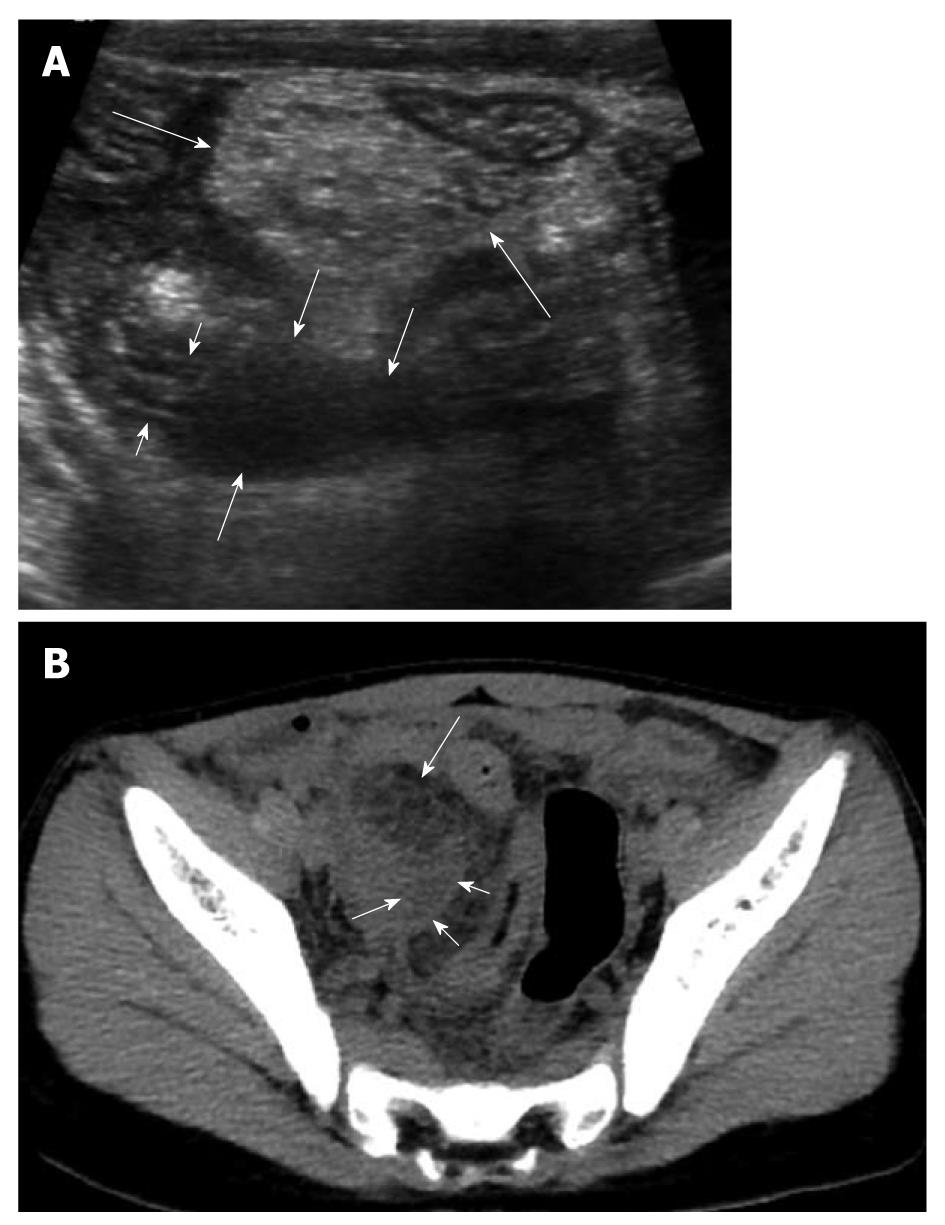
Figure 9 An 8-year-old male with perforated appendicitis.
A: Initial US showed a collapsed appendix with distal wall defect (short arrows) and periappendiceal fluid collection (medium sized arrows) in the deep right lower abdomen. In addition, marked mesenteric inflammatory change (long arrows) was seen; B: Subsequent axial CT scan revealed loculated fluid (short arrows) corresponding to the periappendiceal fluid collection on US and marked mesenteric fat change (long arrow) in the right lower abdomen.
- Citation: Park NH, Oh HE, Park HJ, Park JY. Ultrasonography of normal and abnormal appendix in children. World J Radiol 2011; 3(4): 85-91
- URL: https://www.wjgnet.com/1949-8470/full/v3/i4/85.htm
- DOI: https://dx.doi.org/10.4329/wjr.v3.i4.85